Abstract
Orthopaedics has been left behind in the worldwide drive towards diversity and inclusion. In the UK, only 7% of orthopaedic consultants are female. There is growing evidence that diversity increases innovation as well as patient outcomes. This paper has reviewed the literature to identify some of the common issues affecting female surgeons in orthopaedics, and ways in which we can address them: there is a wealth of evidence documenting the differences in the journey of men and women towards a consultant role. We also look at lessons learned from research in the business sector and the military. The ‘Hidden Curriculum’ is out of date and needs to enter the 21st century: microaggressions in the workplace must be challenged; we need to consider more flexible training options and support trainees who wish to become pregnant; mentors, both male and female, are imperative to provide support for trainees. The world has changed, and we need to consider how we can improve diversity to stay relevant and effective.
Cite this article: Bone Jt Open 2021;2-10:893–899.
Keywords: Orthopaedics, Gender, Bias, Pregnancy, Leadership, Female, Microaggressions, Hidden Curriculum, Sterotype, Flexible training, orthopaedic surgeons, orthopaedic surgery, British Orthopaedic Association, postoperative complication, polymethyl methacrylate, ophthalmology, cohort study, depression, strength’, suturing
Introduction
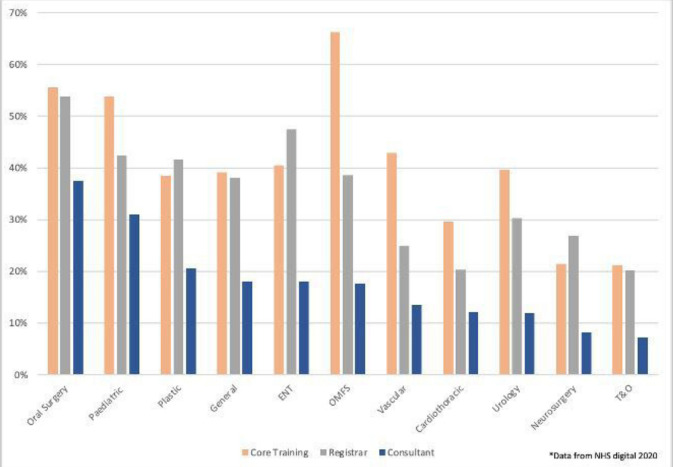
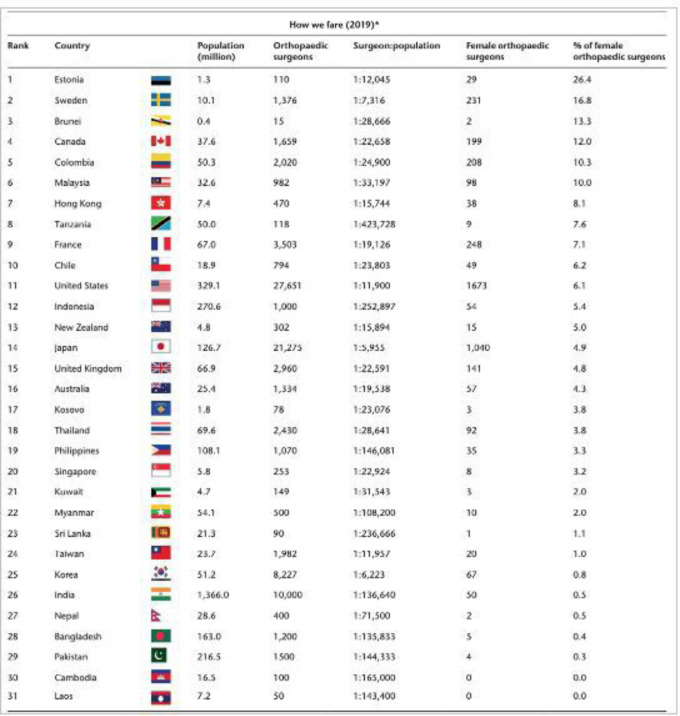
Each year the number of female applicants applying to UK medical schools increases. In 2020, 55% of the intake were female,1 but less than 30% continued to higher surgical training in the UK.2 In the USA, over 57% of medical residents were women, but less than 50% applied to surgical residency,3 and only 14% were in an orthopaedic residency programme.4 The total application rate to orthopaedic training programmes across both sexes has fallen,5 from 10 applicants per place in 2012,6 to 3.11 in 2019.7 We need to ensure that orthopaedics is attractive to all trainees to ensure we are getting the best possible candidates. Although the proportion of female surgeons has increased over the years, in 2020 women made up less than 25% of UK orthopaedic trainees, and only 7% of orthopaedic consultants (Figure 1).8 This rate of change is insufficient to match the demographic changes seen in our medical schools. Globally, the International Orthopaedic Diversity Alliance (IODA) ranked the UK 15th out of 31 countries for the proportion of female orthopaedic surgeons in 2019 (Figure 2).9 Although the number of female consultants is gradually increasing, there is no denying that orthopaedics remains a male-dominated speciality. In 2020, sing the USA National Registry, Acuña et al10 calculated that “without major changes, sex parity in orthopaedic surgery will take more than 200 years”.
Fig. 1.
Percentage of female consultants and trainees in surgical specialties.
Fig. 2.
Reproduced with the permission from the International Orthopaedic Diversity Alliance: Green JA, Chye VPC, Hiemstra LA, et al.9 *Data collected from each nation’s orthopaedic association.
Research has shown that companies with > 20% of women in corporate positions create more innovative ideas, leading to increased success.11 Diversity in orthopaedics brings a return on investment in both the quality of patient care and surgically related outcomes,12 and maximizes the abilities of its surgeons across all genders, allowing for the development of a more supportive community.12,13 To ensure we are attracting the best possible candidates, we must look carefully at why the proportion of women in orthopaedics is so low and how we can improve this. A literature search was performed looking at papers on women and gender in surgery and orthopaedics. Qualitative analysis identified the important themes and directed further literature searches, as seen below. Expanding our literature search into the corporate world and military has added breadth and weight to the recurring themes seen by women in leadership positions.
The Hidden Curriculum
The ‘Hidden Curriculum’ describes the unofficial story of what it means to be an orthopaedic surgeon,14-16 with the old-fashioned stereotype of an ‘unintelligent, strong, sexist man’.17 These unconscious biases can deter excellent candidates from orthopaedics and influence decision-making. Across the UK, ‘Hidden Curriculum’ depicts orthopaedics as a rugby “boys club”.9 Ajaz et al18 reported more than 80% of medical students heard negative comments from medical professionals about other specialties including orthopaedics.19 These myths are often reinforced by other specialties who have no recent experience of modern orthopaedics. This perceived status quo leads to false assumptions that these ‘hidden’ attitudes do not require change, even if they contribute to inappropriate behaviour.18
In 2018, a UK study assessing the effects of the ‘Hidden Curriculum’ across 13 medical schools discovered that 66% of students had heard negative comments about surgery and 27% altered their career plans as a result.19 Furthermore, Whitaker et al20 reported 95% of female medical students perceived orthopaedics to be a ‘male dominated speciality’, and 60% felt orthopaedics ‘requires physical strength’. Although orthopaedics is more physically demanding than specialities such as ophthalmology, modern-day techniques and technology have made it easier for women to operate. Such stereotypes can have a negative impact on trainees. A large study established that female surgical residents (p = 0.002) with a higher degree of stereotype perception have poorer psychological health than males (p = 0.78) and non-surgical trainees (p = 0.92).21 These perceptions hinder women’s career aspirations and increase attrition. Providing medical students and trainees with career advice and positive role models may counteract the negative propaganda and support them in choosing their specialty.9 The Royal College of Surgeons of England (RCSEng) recognizes this, and has free e-learning modules on unconscious bias.22 Diversifying our organization can help identify healthcare inequalities.
Microaggressions
The term ‘microaggression’ is used to describe subtle and/or unintentional discrimination against minorities. These can be small, apparently harmless comments, building up and putting undue stress on the person affected. The physical and psychological impact of microaggressions leads to developments of defence mechanisms, and has been linked to depression and anxiety.23 It also affects academic performance and increases the risk of medical errors.24
A study conducted by Samora et al25 found 74% of female orthopaedic surgeons had experienced a form of microaggression, mostly from patients, families, and male surgeons, during their training. At a large USA institution, Barnes et al26 discovered that female trainees in male-dominated specialties encountered higher rates of microaggression (p < 0.001). The most common domains of microaggression were ‘Leaving Gender at the Door’ where women felt compelled to act more like men, and ‘Inferiority’, where women were presumed less able due to gender.26 Others felt their capabilities were dismissed by men (p = 0.024) and difficult tasks were commonly “assigned to male colleagues” (p = 0.022).26 In another study, a participant reported that “sexist jokes were widely seen to be acceptable, and you were considered overly sensitive if you thought otherwise”.26 A cohort study conducted by Barnes et al24 found that 58% of female surgeons were mistaken for a nurse or another medical/non-medical professional, and 47% felt that they were treated more negatively by nurses. Similarly, a 2020 Australian study illustrated that although implicit gender assumptions may seem harmless, they can ‘become burdensome’, leading women to make unconscious changes in their practice. This includes altering their introductions, thus reducing the instance of ‘mistaken identity’, and establishing methods to gain patient’s trust, such as longer appointment schedules.27 This appears to be a vicious cycle, as the majority of these biases are unintentional. In order to educate the patient population, methods employed in the previous study become important to raise awareness.
Confronting microaggressions is an unnerving task. Warner and Njathi-Ori28 developed a ‘method to address microaggressions in a non-accusatory manner’ with the mnemonic ‘GRIT: Gather your thoughts, Restate, Inquire, Talk it out’. This allows both sides to reflect and respond to the microaggression in a calm manner. ‘Gender blindness’ in some male surgeons has further heightened these issues and the true extent of gender inequality is likely to be underestimated.29 Departmental strategies, such as team case-based discussion and training in implicit bias, can be employed to create a culture that is responsive to microaggression.30 Creating a culture of ‘microaffirmations’ develops a sense of belonging.
Flexible training
A study in the USA found that one of the most common reasons for women not choosing orthopaedics as a speciality was the ‘inability to have a good work-life balance’ (182 of 2,332 (78%)).31 Singh et al32 conducted a global review between 1998 and 2018, and described concerns that women had voiced about “heavy burden managing a home and a career”. Further studies have shown that surgery is not a ‘career welcoming women’ due to inflexible training infrastructure and difficulty in maintaining relationships.33,34 Liang et al35 described all these factors as a “tower of blocks”; female surgeons are more likely to already have two or three blocks before adding in further stressors. The final block to topple the pile could be a relatively minor concern, which could have been prevented by a small intervention.35 The NHS recognizes such difficulties: Supported Return to Training (SuppoRTT) is an individually tailored programme run by Health Education England, providing trainees with professional mentoring, coaching, and enhanced supervision. It is also important for supervisors to recognize when a trainee is struggling, and suggest options of flexible training before it is too late. RCSEng offers clear guidance on flexible training and also has confidential support groups.
Pregnancy
There is a perception that pregnancy during orthopaedic training will hinder training, although there is no documentation in the literature about the frequency of such views. Orthopaedics has unique health and safety risks, including exposure to radiation and teratogenic chemicals. Currently, there is little reported evidence of risk to a foetus from the polymethyl methacrylate (PMMA) vapours,36 and reported radiation exposure when wearing lead gowns is minimal at < 1 mSv over nine months.36 Using appropriate safety measures such as surgical hoods and lead gowns have been shown to minimize exposure.9 RCSEng and the Joint Committee on Surgical Training (JCST) have clear guidance for pregnant trainees on radiation and chemical exposure.37 Each hospital has a Radiation Protection Committee with safety policies for surgeons.38 In summary, there is no medical reason why an orthopaedic surgeon should not get pregnant if they wish.39
In 2020, the British Orthopaedic Association (BOA) reported that 75% of females felt there was a ‘significant compromise in training during pregnancy’ due to intense workload (55%), inappropriate cases out of hours (25%), and difficult on-calls (59%).40 Post-pregnancy, more than half of trainees had taken at least six months to regain their confidence and technical skills, which is unsurprising after an extended period of leave. Unfortunately, 25% felt they were treated “differently” by their colleagues.40 A large USA survey found that 48.4% of female orthopaedic residents deferred having children due to training, and that 59.5% experienced bias against pregnancy from co-residents.41 Female surgeons who had familial duties were perceived to be “less committed by their seniors”, especially when working part-time.29 These attitudes are likely to have an effect on the number of women entering orthopaedics. Deaneries across the UK are more active in ensuring that pregnant trainees are not disadvantaged, and attitudes are changing slowly. Pregnancy during training is not associated with an increased risk of attrition and does not affect case numbers (p = 0.93) or pass rate for exams (p = 0.50).33,42,43 Therefore, female surgeons should not be discouraged from getting pregnant while in training.39
Competence
A female surgeon’s abilities have been described using positive assumptions and credibility deficits.27 Hutchison27 reported that female surgeons were perceived to have less knowledge and ‘technically less proficient’ but were assumed to have neater suturing skills. These biases have been shown to have harmful effects on both surgeon and institution.27 Furthermore, a meta-analysis showed that men rated themselves as significantly more effective than women rated themselves, despite scores from others depicting women more effective than men.44 It is important to highlight that female orthopaedic surgeons are just as competent as males, with studies showing reduced postoperative complication rates and mortality in patients operated on by female orthopaedic surgeons.45,46 Many corporate organizations raise awareness of implicit bias through training modules. We can adopt a similar approach to better educate surgeons.
Leadership
Women are under-represented in leadership roles across all professions. In 2020, only 7.9% of CEOs in the European Union were female.47 This problem is historical and as societal attitudes are changing towards gender inequality, this is reflected in job roles undertaken by women. The presumption that men are better leaders than women is a longstanding perception with no real basis.48 Research demonstrates that female orthopaedic surgeons in leadership roles are just as academically productive as males.48 During the 2018 “Grit in Leadership” American Orthopaedic Symposium, 60.7% of female attendees and 35.9% of male attendees had reported observing negative biases towards women or minorities at least once a month during their practice.49 A study in 2017 found that only 9% of editors for three major orthopaedic journals were women and there were no female editors-in-chief.50 In the UK, from 2014 to 2018, less than 5% of sessions at BOA annual conference were delivered by female orthopaedic surgeons.51 The shortage of female leaders in orthopaedics is due to both lower total numbers and likely attrition.52 Fortunately, NHS England has leadership fellowships that prepare trainees for leadership roles within their organizations.
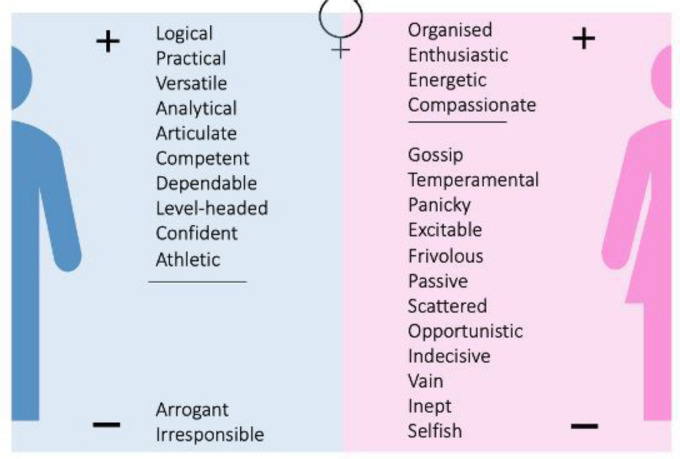
The military has similar issues regarding gender discrimination. A study assessing the language used to subjectively describe military leaders discovered that women received a statistically significantly greater number of negative attributes (p < 0.0001) than men.53 Although these leaders were matched on seniority and competence, there is a clear distinction in the terms used to describe male and female leaders.53 The only negative words used to describe male leaders were ‘arrogant’ and ‘irresponsible’,53 whereas female leaders were most commonly described as ‘inept’ and ‘selfish’ (p < 0.001) (Figure 3).53
Fig. 3.
Statistically significant words used to describe male and female leaders.49
Role models and mentors
Studies have determined a number of important factors leading to female trainees leaving surgery including difficulty in approving leave, poor psychological health, lack of female role models, fear of repercussion, and lack of support pathways.36 Orthopaedic institutions with a large cohort of female faculty have a greater percentage of female trainees.9 A recent study has shown that 83% of female students felt there was inadequate representation of female orthopaedic faculty members, and that achieving a leadership role as a woman was unattainable.35 While more visible female orthopaedic mentors are required, men can be equally efficient role models and can bridge the gap by supporting female students and trainees in orthopaedics.
Lack of female orthopaedic mentors appears to be a factor affecting which subspecialities female orthopaedic surgeons enter. Bratescu et al54 reported that hand (24%) and paediatrics (22.6%) were the most common subspecialties among women. The main reasons for this were personal interests and lack of strong mentorship in other subspecialties.54 In the UK, orthopaedic societies such as the BOA are actively investigating ways to increase “diversity and mentorship for female members”,55 and upcoming female leaders of such societies are championing for more female leaders across all grades in orthopaedics.
The future
The time has come for us to recognize that orthopaedics has been left behind in the worldwide drive to improve diversity. We cannot develop as a profession unless women are completely included, not just in numbers, but also in respect and authority. Factors affecting the uptake of females include unconscious bias, inflexible training, and lack of female role models. To achieve a diverse workforce, the UK ‘30% club’ outlines a 30% representation of minorities as the diversity goal in every organization, with studies showing an improvement in corporate performance.56 In the UK, 14.7% of orthopaedic speciality trainees were female in 2012, which increased to 18.6% in 2019.8 At this rate of ‘improvement’, 30% of female orthopaedic speciality trainees and consultants will be achieved in 2042 and 2069, respectively. To attain this goal sooner, measures are being put in place.
Successful programmes across the UK have made substantial strides in representing women. Women in Surgery (WinS) and International Orthopaedic Diversity Alliance (@OrthoDiversity) are fast-growing networks dedicated to improving diversity.57 RCSEng Diversity Report has highlighted sex discrimination across surgery and created strategies to increase the number of visible female role models in leadership positions.58 A new nternational collaborative, Women in Orthopaedics Worldwide (@orthoWOW), has been created to share experience and support. There are also informal support groups on Facebook (W.ORTH – Women in Orthopaedics) and twitter (@OrthoWomen). Social media now enables people to support each other across the world via Twitter hashtags such as #ILookLikeaSurgeon and #speakuportho.
We must generate a cultural and structural change within our departments and medical schools by allowing early exposure of orthopaedics and providing mentors. The ‘Hidden Curriculum’ should not be an accepted “part of professional socialisation”.59 Research has established that USA ‘pipeline programs’ such as ‘Perry Initiative’ and ‘Nth Dimensions’ are successful at addressing implicit biases and in enlisting female students into orthopaedics.60
In our daily practice, we must acknowledge our inherent biases and set ground rules for inappropriate behaviours. Both men and women must speak out and challenge biases and microaggressions. This is difficult to accomplish, but the more we dissuade such behaviour, the more likely we are to eliminate gender bias. We must consider how we wish to portray our speciality and support our trainees, so that we attract and retain the best colleagues, to better serve our patients.
Take home message
- Orthopaedics must recognize the various factors affecting uptake of women to the specialty in order to increase diversity.
- A cultural and structural change in our departments and medical universities will help improve diversity in orthopaedics.
Acknowledgements
The authors would like to thank Caroline Hing and the International Orthopaedic Diversity Association for their support.
Footnotes
Author contributions: M. Ahmed: Investigation, Writing – original draft.
L. C. Hamilton: Investigation, Writing – original draft.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Open access funding: The authors confirm that they received no open access funding from any third parties for this article.
Twitter: Follow L. C Hamilton @OrthoWomen
Contributor Information
Maryam Ahmed, Email: Maryam.ahmed7@nhs.net.
Laura C. Hamilton, Email: laurahamilton21@hotmail.com.
References
- 1. No authors listed . 2020 entry UCAS Undergraduate reports by sex, area background, and ethnic group. https://www.ucas.com/data-and-analysis/undergraduate-statistics-and-reports/ucas-undergraduate-end-cycle-data-resources-2020/2020-entry-ucas-undergraduate-reports-sex-area-background-and-ethnic-group (date last accessed 10 April 2021).
- 2. Moberly T. A fifth of surgeons in England are female. BMJ. 2018;363:k4530. [DOI] [PubMed] [Google Scholar]
- 3. Sing C, Loseth C, et al. Women in surgery: a systematic review of 25 years. BMJ Leader. 2020. [Google Scholar]
- 4. Mulcahey MK, Van Heest AE, Weber K, et al. Women in Orthopaedics: How Understanding Implicit Bias Can Help Your Practice. Instr Course Lect. 2020;69:245–254. [PubMed] [Google Scholar]
- 5. Green R, Steven R, Haddow K, Royal College of Surgeons . Declining applications to surgical specialist training: an ENT perspective on when we should start to worry. 2017. https://publishing.rcseng.ac.uk/doi/pdf/10.1308/rcsbull.2017.141
- 6. Kahane S, Palan J, Stammers J, Baird EJ, Cottam HL, Briggs TWR. Competition for trauma and orthopaedic training numbers. BMJ. 2012;344:e1490. [Google Scholar]
- 7. No authors listed . Competition Ratios. NHS Health Education England. https://specialtytraining.hee.nhs.uk/Competition-Ratios (date last accessed 10 April 2021).
- 8. Holye A, Walsh A, Chatterji S, McNeill H, Davis N. https://www.boa.ac.uk/resources/mentorship-for-female-orthopaedic-surgeons-are-we-behind-the-curve.html (date last accessed 1 September 2021).
- 9. Green JA, Chye VPC, Hiemstra LA, et al. Diversity: Women in orthopaedic surgery – a perspective from the International Orthopaedic Diversity Alliance. Journal of Trauma and Orthopaedics. 8:44–51. [Google Scholar]
- 10. Acuña AJ, Sato EH, Jella TK, et al. How long will it take to reach gender parity in orthopaedic surgery in the United States? An analysis of the National Provider Identifier Registry. Clin Orthop Relat Res. 2021;479(6):1179–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Day MA, Owens JM, Caldwell LS, et al. Breaking Barriers: A Brief Overview of Diversity in Orthopedic Surgery. Iowa Orthop J. 2019;39(1):1–5. [PMC free article] [PubMed] [Google Scholar]
- 12. Cooke DT, Olive J. The importance of a Diverse Specialty: Introducing the STS workforce on diversity. Ann Thorac Surg. 2019;108(4):1000–1005. [DOI] [PubMed] [Google Scholar]
- 13. Bruce AN, Battista A, Plankey MW, Johnson LB, Marshall MB. Perceptions of gender-based discrimination during surgical training and practice. Med Educ Online. 2015;20(1):25923:3492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hill EJR, Bowman KA, Stalmeijer RE, Solomon Y, Dornan T. Can I cut it? Medical students’ perceptions of surgeons and surgical careers. Am J Surg. 2014;208(5):860–867. [DOI] [PubMed] [Google Scholar]
- 15. Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students’ perceptions of teaching. BMJ. 2004;329(7469):770–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Oxtoby K. Do the classic specialty stereotypes still hold true for today’s doctors? BMJ. 2013;347:f7454. [Google Scholar]
- 17. Curlewis K, Thornhill C, et al. The effects of sex, race and the hidden curriculum on medical students’ career choices: lessons for orthopaedics. Bull Royal Coll Surg Engl. 2020;102(6):e7:11. [Google Scholar]
- 18. Ajaz A, David R, Brown D, Smuk M, Korszun A, et al. Bash: Badmouthing, attitudes and stigmatisation in healthcare as experienced by medical students. BJPsych Bull. 2016;40(2):97–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Howleson W, Cloke D, Royal College of Surgeons . The hidden curriculum and its implications for surgical specialties. 2019. https://publishing.rcseng.ac.uk/doi/pdfplus/10.1308/rcsbull.2019.282 (date last accessed 12 August 2021).
- 20. Whitaker J, Hartley B, Zamora R, Duvall D, Wolf V. Residency selection preferences and orthopaedic career perceptions: A notable mismatch. Clin Orthop Relat Res. 2020;478(7):1515–1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Salles A, Mueller CM, Cohen GL. Exploring the Relationship Between Stereotype Perception and Residents’ Well-Being. J Am Coll Surg. 2016;222(1):52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. No authors listed . Avoiding unconscious bias. Royal College of Surgeons. https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/avoiding-unconscious-bias/ (date last accessed 10 June 2021).
- 23. Torres MB, Salles A, Cochran A. Recognizing and reacting to microaggressions in medicine and surgery. JAMA Surg. 2019;154(9):868–872. [DOI] [PubMed] [Google Scholar]
- 24. Barnes KL, Dunivan G, Sussman AL, McGuire L, McKee R. Behind the Mask: An Exploratory Assessment of Female Surgeons’ Experiences of Gender Bias. Acad Med. 2020;95(10):1529–1538. [DOI] [PubMed] [Google Scholar]
- 25. Samora JB, Denning J, Haralabatos S, Luong M, Poon S. Do women experience microaggressions in orthopaedic surgery? Current state and future directions from a survey of women orthopaedists. Current Orthopaedic Practice. 2020;31(5):503–507. [Google Scholar]
- 26. Barnes KL, McGuire L, Dunivan G, Sussman AL, McKee R. Gender bias experiences of female surgical trainees. J Surg Educ. 2019;76(6):e1–e14. [DOI] [PubMed] [Google Scholar]
- 27. Hutchison K. Four types of gender bias affecting women surgeons and their cumulative impact. J Med Ethics. 2020;46(4):236–241. [DOI] [PubMed] [Google Scholar]
- 28. Warner NS, Njathi-Ori CW. The GRIT (Gather, Restate, Inquire,Talk It Out) Framework for Addressing Microaggressions. JAMA Surg. 2020;155(2):178–179. [DOI] [PubMed] [Google Scholar]
- 29. Lim WH, Wong C. The unspoken reality of gender bias in surgery: A qualitative systematic review. PLoS One. 2021;16(2):e0246420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Luo EM, Molina RL. “Are you doing my surgery?”: Addressing microaggressions in surgery. May 16, 2019. https://blog.womensurgeons.org/professionalism/microaggressions/ (date last accessed 12 August 2021).
- 31. Rohde RS, Wolf JM. Where are the women in orthopaedic surgery? Clin Orthop Relat Res. 2016;474(9):1950–1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Singh C, Loseth C, Shoqirat N, et al. Women in surgery: a systematic review of 25 years. BMJ Leader. 2020;41:leader-2019-000199–8. [Google Scholar]
- 33. Arnold-Forster A. Sexism in surgery – little has changed. https://Blogs.Bmj.Com/Bmj/2019/01/24/Agnes-Arnold-Forster-Sexism-in-Surgery-Little-Has-Changed (date last accessed 10 April 2021).
- 34. Fitzgerald JE, Tang SW. Gender-related perceptions of careers in surgery among new medical graduates: results of a cross-sectional study. Am J Surg. 2013;206(1):112–119. [DOI] [PubMed] [Google Scholar]
- 35. Liang R, Dornan T, Nestel D, et al. Why do women leave surgical training? A qualitative and feminist study. Lancet. 2019;393(10171):541–549. [DOI] [PubMed] [Google Scholar]
- 36. No authors listed . Women in surgery. Orthnorth Teaching & Education Association. https://orthnorth.org.uk/experience/women-in-surgery (date last accessed 10 April 2021).
- 37. No authors listed . Surgery, pregnancy and parenthood. Royal College of Surgeons. https://www.rcseng.ac.uk/careers-in-surgery/women-in-surgery/parenthood-with-a-surgical-career/ (date last accessed 10 June 2021).
- 38. Health and Safety Executive . Working safely with ionising radiation. https://www.hse.gov.uk/pubns/indg334.pdf (date last accessed 10 June 2021).
- 39. Hamilton LC. The lesser-spotted pregnant surgeon. June 2018. (date last accessed 13 August 2021). [DOI] [PubMed]
- 40. Dorman S, Shelton J, Wharton D. Inequality, discrimination and regulatory failure in surgical training during pregnancy. https://www.boa.ac.uk/resources/knowledge-hub/inequality-discrimination-and-regulatory-failure-in-surgical-training.html (date last accessed 13 August 2021).
- 41. Hamilton AR, Tyson MD, Braga JA, Lerner LB, et al. Childbearing and pregnancy characteristics of female orthopaedic surgeons. J Bone Joint Surg Am. 2012;94-A(11):e77:11. [DOI] [PubMed] [Google Scholar]
- 42. Rangel EL, Smink DS. Pregnancy and Motherhood During Surgical Training. JAMA Surg. 2018;153(7):644–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Brown EG, Galante JM. Pregnancy-related attrition in general surgery. JAMA Surg. 2014;149(9):893–897. [DOI] [PubMed] [Google Scholar]
- 44. Paustian-Underdahl SC, Walker LS, Woehr DJ. Gender and perceptions of leadership effectiveness: A meta-analysis of contextual moderators. J Appl Psychol. 2014;99(6):1129–1145. [DOI] [PubMed] [Google Scholar]
- 45. No authors listed . Orthopaedic surgeon gender: no bearing on patient outcomes. Brigham and Women’s Hospital. https://www.brighamhealthonamission.org/2020/11/16/orthopaedic-surgeon-gender-no-bearing-on-patient-outcomes (date last accessed 18 April 2021).
- 46. Wallis CJD, Ravi B. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;359:J4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Paustian-Underdahl SC, Walker LS, Woehr DJ, et al. Gender and perceptions of leadership effectiveness: A meta-analysis of contextual moderators. J Appl Psychol. 2014;99(6):1129–1145. [DOI] [PubMed] [Google Scholar]
- 48. Hoof MA, Sommie C, et al. Gender related differences in research productivity. J Am Acad Orthop Surg. 2020;28(21):893–899. [DOI] [PubMed] [Google Scholar]
- 49. Halim UA, Elbayouk A. The prevalence and impact of gender bias and sexual discrimination in orthopaedics, and mitigating strategies. Bone Joint J. 2020;102-B(11):1446–1456. [DOI] [PubMed] [Google Scholar]
- 50. Rynecki ND, Krell ES, Potter JS, Ranpura A, Beebe KS, et al. How well represented are women orthopaedic surgeons and residents on major orthopaedic editorial boards and publications? Clin Orthop Relat Res. 2020;478(7):1563–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Krahelski O, Gallivan S, Hing CB, Royal College of Surgeons . How well are women represented at orthopaedic conferences? November 2020. https://publishing.rcseng.ac.uk/doi/full/10.1308/rcsbull.2020.206 (date last accessed 13 August 2021).
- 52. Emamaulee JA, Lyons MV, et al. Women leaders in surgery: Past, present, and future. Bull Am Coll Surg. 2012;97(8):24–29. [PubMed] [Google Scholar]
- 53. Smith DG, Rosenstein JE, Nikolov MC, Chaney DA. The power of language: gender, status, and agency in performance evaluations. Sex Roles. 2018;80(2):1–13. [Google Scholar]
- 54. Bratescu RA, Gardner SS, Jones JM, et al. Which subspecialties do female orthopaedic surgeons choose and why? JAAOS: Global Research and Reviews. 2020;4(1):e19.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. No authors listed . Diversity and inclusion. British Orthopaedic Association. https://www.boa.ac.uk/about-us/diversity-and-inclusion.html (date last accessed 18 April 2021).
- 56. No authors listed . 30% Club. https://30percentclub.org/ (date last accessed 10 June 2021).
- 57. No authors listed . Women in surgery. Royal College of Surgeons. https://www.rcseng.ac.uk/careers-in-surgery/women-in-surgery/ (date last accessed 18 April 2021).
- 58. No authors listed . Diversity review report launch: we will put diversity at the heart of our strategy. https://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/diversity-review-report-launch (date last accessed 18 April 2021).
- 59. Brown MEL, Coker O, Heybourne A, Finn GM. Exploring the hidden curriculum’s impact on medical students: Professionalism, identity formation and the need for transparency. Med Sci Educ. 2020;30(3):1107–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Van Heest A, Heest AV. Gender diversity in orthopedic surgery: we all know it’s lacking, but why? Iowa Orthop J. 2020;40(1):1–4. [PMC free article] [PubMed] [Google Scholar]