Abstract
Aims
The effect of pelvic tilt (PT) and sagittal balance in hips with pincer-type femoroacetabular impingement (FAI) with acetabular retroversion (AR) is controversial. It is unclear if patients with AR have a rotational abnormality of the iliac wing. Therefore, we asked: are parameters for sagittal balance, and is rotation of the iliac wing, different in patients with AR compared to a control group?; and is there a correlation between iliac rotation and acetabular version?
Methods
A retrospective, review board-approved, controlled study was performed including 120 hips in 86 consecutive patients with symptomatic FAI or hip dysplasia. Pelvic CT scans were reviewed to calculate parameters for sagittal balance (pelvic incidence (PI), PT, and sacral slope), anterior pelvic plane angle, pelvic inclination, and external rotation of the iliac wing and were compared to a control group (48 hips). The 120 hips were allocated to the following groups: AR (41 hips), hip dysplasia (47 hips) and cam FAI with normal acetabular morphology (32 hips). Subgroups of total AR (15 hips) and high acetabular anteversion (20 hips) were analyzed. Statistical analysis was performed using analysis of variance with Bonferroni correction.
Results
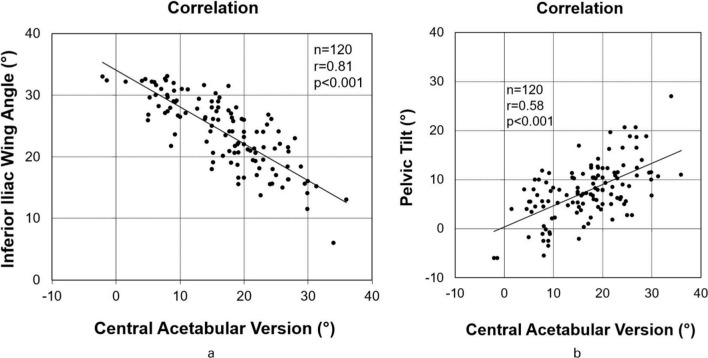
PI and PT were significantly decreased comparing AR (PI 42° (SD 10°), PT 4° (SD 5°)) with dysplastic hips (PI 55° (SD 12°), PT 10° (SD 6°)) and with the control group (PI 51° (SD 9°) and PT 13° (SD 7°)) (p < 0.001). External rotation of the iliac wing was significantly increased comparing AR (29° (SD 4°)) with dysplastic hips (20°(SD 5°)) and with the control group (25° (SD 5°)) (p < 0.001). Correlation between external rotation of the iliac wing and acetabular version was significant and strong (r = 0.81; p < 0.001). Correlation between PT and acetabular version was significant and moderate (r = 0.58; p < 0.001).
Conclusion
These findings could contribute to a better understanding of hip pain in a sitting position and extra-articular subspine FAI of patients with AR. These patients have increased iliac external rotation, a rotational abnormality of the iliac wing. This has implications for surgical therapy with hip arthroscopy and acetabular rim trimming or anteverting periacetabular osteotomy (PAO).
Cite this article: Bone Jt Open 2021;2(10):813–824.
Keywords: Hip, Hip dysplasia, Femoroacetabular impingement, FAI, Acetabular retroversion, Pelvic incidence, Pelvic tilt
Keywords: pelvic incidence, dysplastic hips, pelvic tilting, femoroacetabular impingement, hips, CT scans, hip pain, acetabular rim, cam-type FAI
Introduction
Pincer-type femoroacetabular impingement (FAI) is associated with anterior hip pain and osteoarthritis in young and active patients.1-3 The pathomechanism was described as an early osseous conflict of a prominent acetabular rim with the proximal femur.1-3 Acetabular retroversion (AR) was initially described as a prominent overgrowth of the anterior acetabular wall,4 but there is increasing evidence that AR could be a rotational abnormality of the iliac wing or the hemipelvis (Figure 1, Supplementary Figure a).5-7 Surgical therapy for these hips is controversial:8,9 some authors reported good midterm results with advanced hip arthroscopy,8 and others reported good surgical outcome after an anteverting periacetabular osteotomy (PAO).9 The common surgical treatment is acetabular rim trimming during hip arthroscopy.4 Even if the clinical results of hips with AR treated with acetabular rim trimming are favourable,10 excessive rim trimming can theoretically lead to iatrogenic hip dysplasia.11 A MRI-based 3D investigation found that the size of the lunate surface is normal without focal overgrowth in these hips.11 Comparing rim trimming and anteverting PAO, the latter showed a higher survivorship at midterm follow-up,10 supporting anteverting PAO as a therapy for these hips, but few studies with long-term results after this procedure have been published.10
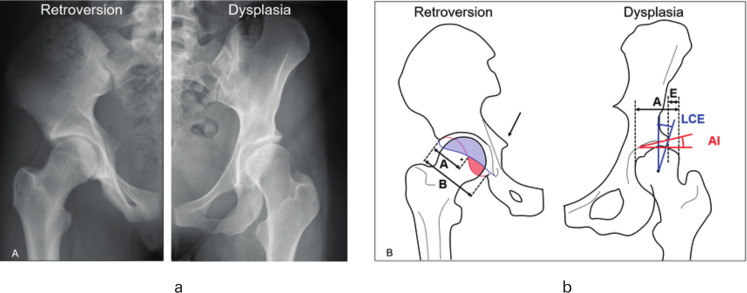
Fig. 1.
a) Radiological and b) schematic views of young patients with hip pain due to acetabular retroversion (left) and hip dysplasia (right). b) Three radiological signs of acetabular retroversion are shown (positive ischial spine sign, posterior wall sign and crossover sign with retroversion index of >50%) . AI, acetabular index; LCE, lateral-centre edge.
In the initial description of FAI, abnormal pelvic tilt (PT) has been proposed as possible explanation for AR.12 More recently, sagittal balance and pelvic incidence (PI) have been investigated in hips with pincer-type FAI due to AR.13,14 PI is a fundamental static parameter15 that determines lumbar lordosis and the adaptation of sacral slope (SS) from standing to sitting position. Several studies have investigated the correlation between PI and spinal pathologies, such as vertebral fractures16 and spondylolisthesis.17 More recently, a possible link between the spinopelvic parameters and the acetabular morphology was suggested by other authors.18 However, there is conflicting evidence whether or not PI is decreased in patients with FAI.13,14 This could be due to different definitions for diagnosis of AR in pincer-type FAI.13,14
The diagnosis of AR is based on several radiological signs on anteroposterior (AP) radiographs (Figure 1 and Figure 2) that can be influenced by tilt and rotation during patient positioning.5,6,19-21 There are no objective radiological diagnostic signs independent of patient positioning on AP radiographs.20 PT varies between standing and supine position in patients with hip dysplasia.22,23 Furthermore, pelvic inclination is another parameter for PT and should theoretically be increased in hips with AR according to orthopaedic literature.12 The effect of pelvic inclination and sagittal balance is unclear in hips with FAI due to AR.10 We intended to compare sagittal balance in a patient series of symptomatic patients with subtypes of FAI or hip dysplasia.
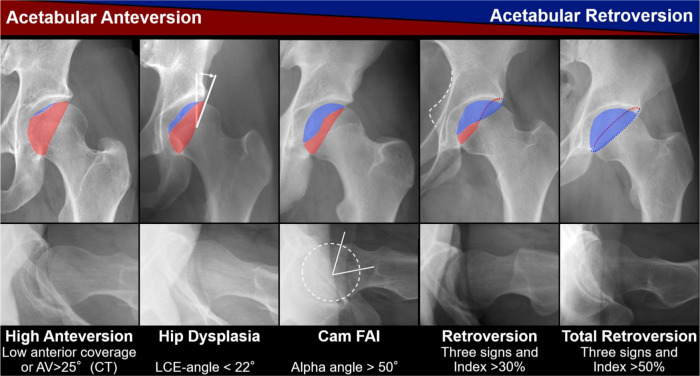
Fig. 2.
Radiological definitions of the five study groups are shown. AV, anteversion; FAI, femoroacetabular impingement; LCE, lateral-centre edge.
Therefore, we posed the following questions: are parameters for sagittal balance (PI, PT, and SS), and is external rotation of the iliac wing, different in patients with AR compared to controls?; and is there a correlation between external rotation of the iliac wing and central acetabular version?
Methods
We performed a retrospective, review board-approved, controlled radiological study evaluating 120 hips in symptomatic patients with FAI or hip dysplasia. They were reviewed in the outpatient clinic of the author’s institution (Inselspital Bern, Bern, Switzerland). All patients presented with hip pain at time of image acquisition and a history, physical exam, and imaging that were consistent with anterior hip impingement or hip dysplasia. Mean age of the total study group was 28 years (standard deviation (SD) 8; 16 to 50) and 63% were female (n = 54) (Table I). AP and lateral radiographs and pelvic CT scans were available for all patients. Institutitonal review board approval was obtained for this study.
Table I.
Demographic and radiological data of the five study groups.
| Parameter | Total | Cam FAI | Acetabular retroversion | Hip dysplasia | Total acetabular retroversion | High acetabular anteversion | Control group | p-value |
|---|---|---|---|---|---|---|---|---|
| Hips (patients) | 120 (86) | 32 (24) | 41 (33) | 47 (29) | 15 (9) | 20 (17) | 48 (27) | |
| Mean age, yrs (SD; range) | 28 (8; 16 to 50) | 28 (9; 18 to 46) | 28 (8; 17 to 44) | 29 (9; 16 to 50) | 31 (7; 16 to 42) | 31 (10; 16 to 50) | 63 (11; 36 to 79)* | 0.003† |
| Female, % | 63 | 38 | 63 | 81 | 53 | 95 | 81 | < 0.001‡ |
| Left side, % | 43 | 50 | 41 | 40 | 53 | 25 | 52 | 0.188‡ |
| Mean height, cm (SD; range) | 172 (6; 158 to 188) | 176 (6; 162 to 181) | 171 (6; 160 to 181) | 170 (7; 158 to 188) | 171 (4; 165 to 175) | 170 (9; 158 to 188) | N/A | 0.009† |
| Mean weight, kg (SD; range) | 72 (14; 44 to 100) | 75 (11; 60 to 99) | 69 (14; 44 to 98) | 71 (14; 50 to 100) | 74 (21; 44 to 98) | 76 (16; 50 to 100) | N/A | 0.467† |
| Mean BMI, kg/m2 (SD; range) | 24 (6; 16 to 35) | 24 (4; 19 to 34) | 24 (4; 16 to 33) | 25 (5; 18 to 35) | 25 (7; 16 to 33) | 27 (5; 20 to 35) | N/A | 0.641† |
| Mean LCE, ° (SD; range) | 26 (10; 4 to 52) | 28 (3; 23 to 33) | 35 (7; 22 to 52) | 16 (5; 4 to 21) | 39 (7; 28 to 52) | 14 (4; 4 to 20) | 35 (4; 24 to 40) | < 0.001† |
| Mean AI, ° (SD; range) | 6 (7; -11 to 27) | 4 (6; -9 to 15) | 1 (5; -11 to 9) | 12 (6; 2 to 27) | 0 (5; -11 to 9) | 15 (6; 3 to 25) | 2 (3; -6 to 7) | < 0.001† |
| Mean EI, ° (SD; range) | 24 (9; 0 to 46) | 21 (4; 12 to 29) | 16 (7; 0 to 29) | 32 (6; 14 to 46) | 11 (6; 0 to 23) | 36 (4; 30 to 46) | N/A | < 0.001† |
| Mean total coverage, % (SD; range) | 74 (12; 32 to 100) | 78 (7; 67 to 92) | 82 (9; 64 to 100) | 64 (9; 32 to 78) | 86 (9; 71 to 100) | 61 (10; 32 to 71) | N/A | < 0.001† |
| Mean anterior coverage, % (SD; range) | 23 (10; 1 to 54) | 21 (5; 10 to 30) | 34 (8; 19 to 54) | 15 (6; 1 to 27) | 40 (6; 28 to 50) | 10 (4; 1 to 14) | N/A | < 0.001† |
| Mean posterior coverage, % (SD; range) | 39 (8; 18 to 61) | 44 (9; 24 to 61) | 34 (7; 20 to 46) | 39 (6; 18 to 50) | 31 (8; 20 to 45) | 40 (6; 30 to 50) | N/A | < 0.001† |
| Crossover sign, % | 58 | 53 | 100 | 23 | 100 | 15 | N/A | < 0.001‡ |
| Mean retroversion index, % (SD; range) | 21 (25; 0 to 100) | 8 (10; 0 to 29) | 51 (21; 30 to 100) | 5 (7; 0 to 25) | 73 (19; 50 to 100) | 3 (7; 0 to 13) | N/A | < 0.001† |
| Posterior wall sign, % | 69 | 41 | 100 | 64 | 100 | 70 | N/A | < 0.001‡ |
| Ischial spine sign, % | 53 | 31 | 100 | 28 | 100 | 10 | N/A | < 0.001‡ |
| Mean α angle, ° (SD; range) | 59 (12; 34 to 87) | 66 (10; 51 to 85) | 59 (14; 41 to 87) | 55 (11; 34 to 85) | 61 (10; 45 to 72) | 41 (6; 33 to 49) | N/A | < 0.001† |
| Mean neck-shaft angle, ° (SD; range) | 133 (7; 110 to 159) | 130 (4; 120 to 137) | 131 (7; 110 to 142) | 137 (8; 124 to 159) | 128 (5; 116 to 135) | 139 (9; 126 to 159) | 130 (5; 122 to 139) | < 0.001† |
| Mean symphysis sacrococcygeal distance, ° (SD; range) | 54 (16; 23 to 92) | 50 (18; 23 to 88) | 58 (17; 33 to 92) | 53 (12; 34 to 84) | 64 (13; 47 to 80) | 54 (10; 41 to 75) | N/A | 0.079† |
| Mean sacrofemoral pubic angle, ° (SD; range) | 69 (6; 58 to 85) | 68 (6; 60 to 82) | 72 (5; 65 to 85) | 67 (5; 58 to 75)* | 74 (6; 66 to 85) | 66 (5; 59 to 74) | N/A | 0.135† |
Significant difference compared to acetabular retroversion group.
Analysis of variance.
Chi-squared test.
AI, acetabular index; EI, extrusion index; FAI, femoroacetabular impingement; LCE, lateral centre edge angle; SD, standard deviation.
Description of study group
Inclusion criteria were the availability of a pelvic CT scan including the endplate of S1 in skeletal mature patients with symptomatic anterior FAI or hip dysplasia. Exclusion criteria was hip osteoarthritis > Grade 2 according to Tönnis.24 Out of 410 hips with a pelvic CT scan between January 2010 and August 2016 used for another study,25 we excluded 74 hips with previous hip or spine operations or with a history of hip disease in childhood (slipped capital femoral epiphysis (SCFE)26 or Perthes’ disease,27 26 skeletally immature hips, 71 hips with post-traumatic conditions, 20 hips with mixed FAI, 33 hips with no obvious pathomorphology on the AP radiograph, 21 hips with overcoverage, 22 hips with severe overcoverage, 18 hips with valgus morphology, and five hips with avascular necrosis of the femoral head (Table II). This resulted in a total study group of 120 hips of consecutive patients with symptomatic anterior FAI or hip dysplasia and a complete radiological dataset. The definition of pincer-type FAI attributed to overcoverage (LCE angle 35° to 39°) and to severe overcoverage (LCE angle > 39°) was based on previously published reference values (Table II).28 Mixed-type FAI was defined as combined overcoverage (LCE angle 35° to 39°) with a cam-type deformity.
Table II.
Definition of study groups with the used in- and exclusion criteria are shown. The allocation to a specific group was performed based on the morphological analysis of the conventional anteroposterior pelvic radiograph and the cross-table lateral radiographs of the hip.
| Criteria | Definition | Hips (patients) |
|---|---|---|
| Inclusion | ||
| Hip dysplasia | LCE angle < 22°28 and/or anterior coverage < 14%28 independent of the neck-shaft-angle | 47 (29) |
| Acetabular retroversion | Positive crossover sign29 positive ischial spine sign6 positive posterior wall sign29 and retroversion index > 30%30 independent from alpha angle | 41 (33) |
| Cam-type FAI | alpha angle > 50°31 with neck-shaft angle of 120° to 140° and with normal acetabulum (LCE 23° to 33°)28 not all retroversion signs positive | 32 (24) |
| Total acetabular retroversion* | Positive crossover sign29 positive ischial spine sign6 positive posterior wall sign29 and retroversion index > 50%30 independent from α angle | 15 (9) |
| High acetabular anteversion† | Central acetabular anteversion > 25°32on CT scan and/or anterior coverage < 14%28 | 20 (17) |
| Exclusion | ||
| No obvious pathomorphology | No obvious acetabular and femoral deformities, normal LCE angle (22° to 34°), normal alpha angle (< 50°), normal femoral head coverage, symptomatic hip | 33 (33) |
| Severe overcoverage | LCE angle > 39°32 and/or protrusio acetabuli (defined as femoral head touching or crossing the ilioischial line), and/or total femoral coverage > 93%28 not all retroversion signs positive | 22 (14) |
| Overcoverage | LCE angle 34° to 39°28 with alpha angle < 50°, not all retroversion signs positive | 21 (11) |
| Mixed-type FAI | Mixed-type FAI was defined as combined overcoverage (LCE angle 35° to 39°) with an alpha angle > 50°, not all retroversion signs positive | 20 (20) |
| Valgus hips | Neck-shaft-angle > 139° | 18 (18) |
| Avascular necrosis | Avascular necrosis of the femoral head | 5 (5) |
| Control group | Patients with whole body CT scans for nonorthopaedic reasons (mostly multiple myeloma patients) | 48 (27) |
This group is a subgroup of the patients with acetabular retroversion.
This group is a subgroup of the patients with hip dysplasia .
FAI, femoroacetabular impingement; LCE, lateral centre edge angle.
Group allocation
These 120 hips were allocated to three primary groups: AR (41 hips), hip dysplasia (47 hips), and hips with cam FAI with normal acetabular morphology (32 hips). Two subgroups were analyzed: one subgroup with total AR (15 hips) and another with high acetabular anteversion (20 hips) were analyzed. The 15 hips of the subgroup with total AR were also included in the group with AR (41 hips). The 20 hips with high acetabular anteversion were also included in the group with hip dysplasia (47 hips). The study groups were defined using the previously validated software Hip2Norm33 (University of Bern, Switzerland) for calculation of radiological parameters for description of the acetabular morphology (Figure 1 and Figure 2, Supplementary Video a). Based on the analysis of the conventional radiographs, the inclusion criteria for the three primary groups and the two subgroups were: hip dysplasia (lateral centre edge (LCE) angle < 22°);28 anterior FAI attributed to AR (positive crossover sign,29 positive ischial spine sign,6 positive posterior wall sign,29 and retroversion index > 30%30 ); high acetabular anteversion (> 25°32 on CT scan or reduced anterior coverage < 14%);25 anterior FAI attributed to total AR (positive crossover sign,29 positive ischial spine sign,6 positive posterior wall sign),29 and retroversion index > 50%; cam-type FAI was defined as alpha-angle > 50°31 in the presence of neither hip dysplasia34,35 nor pincer-type morphology (LCE angle 23° to 33°). The allocation to each group was based on previously published reference values for acetabular28 and femoral31 morphology (Table II).
Control group
A control group of 48 hips of a previous study25 with whole body CT scans was used for comparison of sagittal parameters. Exclusion criteria for the control group were patients with LCE angle < 25° or > 39°, neck-shaft angle < 120 or > 139°, and α angle > 55°, as in the previous study.25
Clinical evaluation
As part of the routine workup, all patients were clinically evaluated in the outpatient clinic for hip preservation surgery. This included a thorough acquisition of the patient history, a goniometric measurement of the hip range of motion in prone and supine position, the evaluation of the anterior and posterior impingement tests,2 and the assessment of hip instability (based on the apprehension/flexion, abduction, and external rotation tests), abductor strength, and general joint laxity using the Beighton score.36 The posterior impingement test was used as a potential indicator for anterior hip instability.2
Radiological assessment
Standardized AP and cross-table lateral radiographs were performed in a standardized manner2 and served for calculation of the radiological parameters of Hip2Norm. This software allows accurate and reliable measurement of eight radiological parameters of the hip, including the assessment of femoral head coverage. No correction of PT and rotation was performed with Hip2Norm because the lateral pelvic radiograph was not available for all patients. The α angle was measured as a measure of femoral asphericity on the axial cross-table radiograph (Figure 2). The symphysis to sacrococcygeal distance and the sacrofemoral pubic angle was measured for all hips on the AP radiograph. All radiological measurements were performed by two independent observers (TDL, AB). Additional projections or functional views were acquired if needed for diagnosis or surgical planning.
CT protocol included the entire pelvis, the endplate of S1, and the distal femoral condyles in all hips37 . The CT scans were performed according to a previously described protocol37 for calculation of femoral and acetabular version25 and for preoperative planning. A slice thickness of 2 mm and an interval of reconstruction of 1.7 mm were chosen.
Acetabular version was calculated on the CT scans.32 Central acetabular version was measured according to Tönnis and Heinecke,32 and was defined as the angle between a sagittal line and a line connecting the anterior and posterior acetabular rim, with correction for malpositioning of the patient in the CT scanner. By drawing a line that connects both femoral head centre, the sagittal line was drawn perpendicular (90°) to this line. A normal central acetabular version was defined from 10° to 25°.32 Increased acetabular version was defined > 25°. The anterior pelvic plane (APP) angle was measured according to the method described in a previous study by Tachibana et al.23
Outcome parameters
PI was defined as the angle between the line perpendicular to the middle of the cranial sacral endplate to the centre of the bicoxofemoral axis38 (Supplementary Figure b). PT was defined as the angle between the vertical line and the line connecting the middle of the sacral endplate and the centre of the bicoxofemoral axis.38 SS was defined as the angle between the horizontal line and the cranial sacral endplate tangent.38 In addition, pelvic inclination was defined as the angle formed by the line connecting the promontory of the sacrum and the upper border of the symphysis with the horizontal plane.12
External rotation of the iliac wing was measured using the inferior iliac wing angle, as previously described.39,40 This angle was measured on axial CT slices on the level of the anterior-inferior iliac spine (AIIS). An angle drawn by a line through the tip of the AIIS and a vertical line was calculated (Figure 3).39,40 The vertical line was reconstructed by connection of bilateral iliosacral joints to take into account pelvic positioning. Standardization of pelvic position was made for measurement of the iliac wing angle in relation to the iliosacral joint on the axial CT scan. By drawing a line that connects both anterior iliosacral joints, the sagittal line was drawn perpendicular to this line (Supplementary Figure c). The lower the angle, the more the iliac wing was internally rotated.
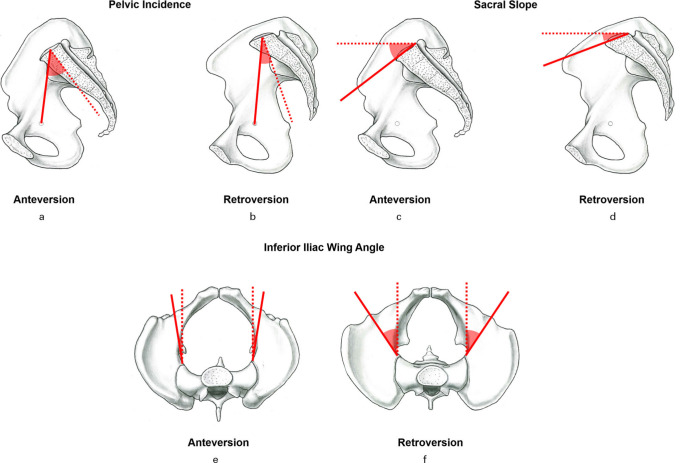
Fig. 3.
a) and b) Sagittal profiles of a pelvic bone of a patient with a) and c) high acetabular anteversion, and b) and d) a patient with acetabular retroversion (AR). e) Hips with AR have more external rotation of the iliac wing compared to f) hip dysplasia.
Two observers (TDL, IAST) independently measured the study variables on a random sample of 30 hips taken from our patient cohort at two timepoints. A good agreement (defined as intraclass correlation coefficient (ICC) > 0.8)41 was found for both reproducibility and reliability of PI and SS (ICC ranging from 0.8 to 0.95) and a substantial agreement (defined as ICC > 0.6) was found for reproducibility and reliability of PT (ICC ranging from 0.72 to 0.8; Table III).
Table III.
Reliability and reproducibility of the evaluated study variables. Values are expressed as mean intraclass correlation coefficient with 95% confidence intervals.
| Parameter | ICC intraobserver 1 | ICC intraobserver 2 | ICC interobserver |
|---|---|---|---|
| Pelvic incidence | 0.91 (0.85 to 0.95) | 0.95 (0.91 to 0.97) | 0.92 (0.89 to 0.95) |
| Pelvic tilt | 0.80 (0.65 to 0.89) | 0.77 (0.61 to 0.88) | 0.72 (0.63 to 0.81) |
| Sacral slope | 0.85 (0.73 to 0.91) | 0.81 (0.66 to 0.89) | 0.82 (0.66 to 0.9) |
| APP angle | 0.89 (0.85 to 0.95) | 0.91 (0.81 to 0.97) | 0.85 (0.79 to 0.95) |
APP, anterior pelvic plane; ICC, intraclass correlation coefficient.
Statistical analysis
Statistical analysis was performed using Winstat software (R. Fitch Software, Germany). Normal distribution was tested using the Kolmogorov-Smirnov test. Differences among the five groups for demographic data, radiological data, pelvic inclination, and parameters for sagittal balance were determined using analysis of variance (ANOVA) for continuous data and the chi-squared test for binominal data. If differences existed, pairwise comparison was performed using the independent-samples t-test for continuous data and the Fisher’s exact test for binominal data. To correct for multiple comparisons within the outcomes the Bonferroni correction was applied. This is a conservative method to minimize false positive results, however some true positive might have been missed. The level of significance was adjusted for six groups to p = 0.008. Pearson’s correlation coefficient was used because the data were normally distributed.
Results
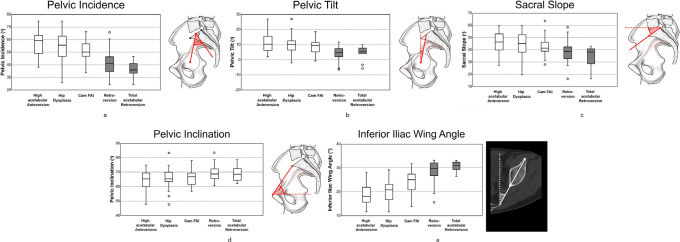
PI, PT, and SS differed significantly among the five study groups (p < 0.001, ANOVA; Table IV, Supplementary Figure c). PI was significantly decreased in hips with AR (42° (SD 10°)) compared to dysplastic hips (55° (SD 12°)) and hips with cam FAI (51° (SD 7°); p < 0.001, ANOVA, Figure 4) (Supplementary Video b). PI and PT were significantly decreased in hips with total AR (37° (SD 7°) and 4° (SD 5°)) compared to hips with high acetabular anteversion (57° (SD 11°) and 11° (SD 7°); p < 0.001, ANOVA, Figure 4).
Table IV.
The CT-based measurements and outcome parameters of the five study groups and of the control group. Level of significance was adjusted using the Bonferroni correction for six groups (0.05/6 = 0.008).
| Parameter | Cam FAI | Acetabular retroversion | Hip dysplasia | Total acetabular retroversion | High acetabular anteversion | Control group | p-value* |
|---|---|---|---|---|---|---|---|
| Hips, n (patients) | 32 (24) | 41 (33) | 47 (29) | 15 (9) | 20 (17) | 48 (27) | |
| Mean pelvic incidence, ° (SD; range) | 51 (7; 34 to 66)† ‡ | 42 (10; 24 to 67) | 55 (12; 25 to 75)† ‡ | 37 (7; 24 to 46) | 57 (11; 38 to 75)† ‡ | 51 (9; 32 to 72)† ‡ | < 0.001 |
| Mean pelvic tilt, ° (SD; range) | 8 (5; -1 to 19)† | 4 (5; -6 to 12) | 10 (6; -2 to 27)† ‡ | 4 (5; -6 to 10) | 11 (7; 2 to 27)† ‡ | 13 (7; 4 to 27)† ‡ | < 0.001 |
| Mean sacral slope, ° (SD; range) | 42 (7; 28 to 64) | 38 (9 ;16 to 58) | 44 (9; 19 to 60)† ‡ | 34 (9; 16 to 43) | 46 (8; 27 to 60)† ‡ | 38 (7; 26 to 54) | < 0.001 |
| Mean external iliac rotation, inferior iliac wing angle, ° (SD; range) | 24 (5; 14 to 32)† ‡ | 29 (4; 16 to 33) | 20 (5; 6 to 29)† ‡ | 31 (2; 26 to 33) | 19 (5; 6 to 28)† ‡ | 25 (5; 15 to 33)† ‡ | < 0.001 |
| Mean pelvic inclination, ° (SD; range) | 66 (5; 57 to 78) | 69 (5; 61 to 83) | 65 (7; 48 to 83) | 68 (5; 62 to 78) | 64 (7; 48 to 75) | 59 (7; 46 to 70)† ‡ | 0.038 |
| Mean acetabular version, ° (SD; range) | 18 (6; 8 to 30) | 10 (6; -2 to 25) | 22 (5; 9 to 36)† ‡ | 5 (4; -2 to 14) | 25 (5; 15 to 36)† ‡ | 18 (5; 8 to 26)† ‡ | < 0.001 |
| Mean APP angle, ° (SD; range) | 5 (5; -7 to 17) | 8 (5; -1 to 24) | 7 (6; -6 to 20) | 8 (6; -1 to 15) | 7 (7; -4 to 20) | 1 (7; -10 to 15) | 0.703 |
Analysis of variance.
Significant difference compared to hips with acetabular retroversion.
Significant difference compared to hips with total acetabular retroversion.
APP, anterior pelvic plane; FAI, femoroacetabular impingement; SD, standard deviation.
Fig. 4.
Boxplots for a) pelvic incidence, b) pelvic tilt (PT), c) sacral slope (SS), d) pelvic inclination, and e) the inferior iliac wing angle. We found a significantly decreased PI, PT and SS for acetabular retroversion (AR) compared to hip dysplasia. In addition, we found a significantly increased inferior iliac wing angle for AR compared to hip dysplasia. The level of significance was adjusted for 6 groups (0.05/6 = 0.008). Dark boxes signify significant difference compared to hip dysplasia. FAI, femoroacetabular impingement.
PI and PT were significantly decreased in hips with total AR compared to the control group. PT was significantly decreased in hips with AR (4° (SD 5°)) compared to hip dysplasia (10° (SD 6°)) and hips with cam FAI (8° (5°)) (p < 0.001, ANOVA). SS was significantly decreased in hips with total AR (34° (SD 9°)) compared to hips with high acetabular anteversion (46° (SD 8°); Supplementary Figure c). SS was significantly decreased in hips with AR (38° (SD 9°)) compared to hip dysplasia (44° (SD 9°); p < 0.001, ANOVA; Supplementary Figure c). Pelvic inclination was not significantly different among the five study groups (p = 0.038, ANOVA; Supplementary Figure c).
External rotation of the iliac wing was significantly (p < 0.001, Figure 4) increased in hips with AR (29° (SD 4°)) compared to hip dysplasia (20° (SD 5°); p < 0.001, ANOVA; Figure 3, Supplementary Video c, Supplementary Figure c). External rotation of the iliac wing was significantly (p < 0.001) increased in hips with AR (31° (SD 2°)) compared to hips with high acetabular anteversion (19° (SD 5°)) and compared to the control group (25° (SD 5°); p < 0.001, ANOVA) (Supplementary Figure c).
Interestingly, the anterior pelvic plane (APP) angle was not significantly different and the distance between the symphysis and the sacrococcygeal joint was not significantly different between hips with total AR and hip with increased acetabular anteversion (Table I). Overall, there was no significant difference of the sacrofemoral pubic angle between all groups. The sacrofemoral pubic angle was significantly increased in patients with AR (72° (SD 5°)) compared to hip dysplasia (67° (SD 5°); p < 0.001, ANOVA).
We found a significant and strong correlation (r = 0.81; p < 0.001, Pearson’s correlation coefficient) between external rotation of the iliac wing (inferior iliac wing angle) and central acetabular version (Figure 5a). Correlation between central acetabular version and PT (Figure 5b) was also significant (r = 0.58; p < 0.001, Pearson's correlation coefficient) but with moderate correlation coefficient (Figure 5).
Fig. 5.
a) Correlation between central acetabular version and the inferior iliac wing angle. b) Correlation between central acetabular version and pelvic tilt.
Discussion
We intended to determine sagittal balance in a large patient series of symptomatic patients with FAI due to AR or hip dysplasia. Therefore, the aim of this study was to investigate PI, PT, SS, and pelvic inclination in these two groups in comparison to control hips and patients with cam-type morphology with a normal acetabular coverage. Most importantly, we found that hips with AR have significantly decreased PI, PT, and SS (p < 0.001, ANOVA). Interestingly, we found a significantly increased iliac external rotation (p < 0.001, ANOVA) and a strong correlation between external rotation of the iliac wing and central acetabular version. We found no significant difference for pelvic inclination among the six groups.
The current study represents a large study investigating the radiological association between hip morphologies and sagittal balance. Previous studies involving symptomatic FAI patients had a lower sample size and included no control group.13,14 Other morphological studies were based on asymptomatic volunteers18 or cadaveric investigations42-44 and their results are difficult to translate into clinical practice, since it is difficult to judge the radiological findings without clinical examinations.45 Another strength of the current study is that the definitions used in the current study for FAI patients are based on previously published radiological reference values for acetabular under- and overcoverage28 measured on the AP pelvic radiograph. We used three radiological signs for definition of AR and this is different compared to other investigations for pincer-type morphologies.13,42 Other studies used solely the crossover sign for the diagnosis of AR,12,18,19 which could overestimate AR. In a recent systematic review, a high prevalence of signs for AR in asymptomatic volunteers was described.46 In addition, in a population-based cohort of 2,081 healthy young adults, a positive crossover sign was prevalent in 51% of male and in 46% of female asymptomatic volunteers.47
We used the combination of the crossover sign, the ischial spine sign, the posterior wall sign, and the retroversion index > 30%34 for the diagnosis of AR, with > 50% for total AR. These three diagnostic signs were used to ensure reproducibility and to avoid false-positive diagnosis. The third strength of this study is the use of CT scans for assessment of sagittal balance. Other studies used lateral radiographs13 for the calculation of PI. We found a good reproducibility for the four outcome parameters using pelvic CT scans.
We compared our results for PI with the literature. The reported values for PI for patients with cam-type FAI range from 49°13 to 51°14 and are in line with the results of the current study (51° (SD 7°)). Comparing our results of hips with hip dysplasia and high acetabular anteversion with another study investigating hip dysplasia patients, we found a comparable value.48 In contrast, PI varied between 45°13 and 51°14 in other studies that investigated hips with AR and this is higher compared to our results (42° (SD 10°)). A lower PI of 38° was reported in a recent study for FAI patients with a deep socket13 (defined as LCE angle > 39°).13 This could be due to their definition of a deep socket that was based solely on the LCE angle but did not evaluate the three radiological signs for AR that we used. Our definition of AR is based on three radiological signs and minimum retroversion index of 30%. Recent studies13,14 used axial CT slices and defined retroversion as anteversion < 15°. We think that this CT-based definition of AR is questionable, because others reported normal values for acetabular version between 10° and 25°.32
PI is a static parameter that determines lumbar lordosis. PI is age-independent in adults, increases during childhood, and stabilizes at ten years of age.49 Normal values range from 51° to 55° and have been described by several authors;15,38,43,50-52 these are summarized in Supplementary Table i. According to current spine literature, with a higher PI, lumbar lordosis is increased and the range of adaptation of the SS may be greater.53 In case of a lower PI, lumbar lordosis is decreased and the range of adaptation of the SS is more limited. Theoretically, patients with AR should have less lumbar lordosis and a weaker capacity to adapt to sagittal imbalance.53 This could aggravate anterior hip impingement in sitting position because less posterior pelvic tilting is possible.
PT differed significantly (p < 0.001) among the study groups (p < 0.001, ANOVA). Comparing our results of the hips with AR to others, they described higher values for PT ranging from 10°15 to 13°38 for asymptomatic volunteers. We found comparable values for hips with high acetabular anteversion (11° (SD 7°)), while we found decreased values for hips with total AR (4° (SD 5°)). Others investigated PT of patients with AR before and after anteverting PAO surgery.54 They reported comparable values for PT, SS, PI, and the APP angle compared to the results of hips with AR in the current study. Comparing our results of hips with hip dysplasia and high acetabular anteversion with another study investigating hip dysplasia patients, we found a comparable value of PT.48 A small decrease of PT was described after bilateral PAO for treatment of hip dysplasia.55
This is important, because increased posterior PT is often associated with postural imbalance to compensate for forward tilt of the entire trunk. This can lead to a posterior hip impingement in standing position.56-58 In contrary, excessive anterior PT in a sitting position can lead to anterior hip impingement.53 Some authors have proposed that in patients with hip osteoarthritis and decreased PI, the pelvis attempts to maintain normal lumbar lordosis by increasing anterior PT.59
SS was significantly different among the study groups (p = 0.001, ANOVA). For asymptomatic volunteers, SS ranged between 38°15 and 43°.43 Compared to our results, we found lower SS for hips with total AR (34° (SD 9°)) and higher SS for hips with high acetabular anteversion (46° (SD 8°)). This is interesting because SS determines lumbar lordosis and is higher in standing position compared to sitting position.53 In sitting position, posterior PT with verticalization of the sacrum and decrease of the SS was described.53 Sitting position has clinical relevance for patients with FAI, because many patients experience hip pain in this position.2,60 Our findings contribute to a better understanding of anterior hip pain experienced in sitting position.
External rotation of the iliac wing was increased in patients with total AR compared to hip dysplasia. For hip dysplasia, an increased internal rotation of the iliac wing has been described previously.39,40 This is even more increased in hip dysplasia with a coxa profunda sign.40 Comparing the results for external iliac rotation to the orthopaedic literature, we found only one study investigating the rotation of the iliac wing in hips with AR.7 Their results are in line with the results of the current study, but theirs was performed with measurements performed on AP radiographs,7 which are difficult to compare to our results of the 3D-CTs.
Pelvic inclination was not significantly different among the five study groups (p = 0.038, ANOVA). Previous investigations described comparable values for pelvic inclination ranging from 59° to 66°.12 Evaluation of pelvic inclination24 was initially performed to decrease measurement errors in assessment of acetabular orientation and femoral head coverage for planning of reorientation procedures.12 Signs for AR were found at lower PT angles12 in male pelves compared to female pelves in a cadaver study including four pelves.12 Therefore, it could be hypothesized that pelvic inclination should theoretically be increased in hips with AR according to previous literature.12 We were surprised that pelvic inclination was not significantly different in hips with AR compared to hip dysplasia.
This study has clinical implications. Our findings suggest that patients with pincer-type FAI due to AR should present with increased iliac external rotation. Theoretically, if these patients are treated with anteverting PAO30,34 to rotate the anterior-inferior iliac spine (AIIS) internally, the recently described extra-articular subspine FAI37 could potentially be reduced. Patients with pincer-type FAI due to AR showed decreased PI, PT, and SS. Consequently, these patients should present with decreased lumbar lordosis. We were surprised, because we suspected increased SS and increased lumbar lordosis. Based on the increased iliac external rotation, a rotational deformity of the iliac wing is possible in patients with AR. This study has implications for diagnosis of AR on AP radiographs. Diagnosis based on the symphysis to sacrococcygeal distance21 seems to be difficult for hips with total AR. We found a significantly increased sacrofemoral pubic angle in patients with AR compared to hip dysplasia. This parameter could help to identify patients with AR on AP radiographs.
In case of a low PI, patients with AR could have less compensation with posterior pelvic tilting because they could have less lumbar lordosis. This finding has implications for non-surgical treatment, such as posterior PT taping.61,62 This implies little effect of posterior PT on decrease of anterior hip pain and hip impingement, as suggested by others.63 Treatment of AR should focus on deformity correction rather than trying to modify the functional pelvic position.54 According to the literature, in case of a lower PI, the range of adaptation of the SS is limited53 and can theoretically lead to a functional anterior impingement conflict in sitting position because posterior pelvic tilting is impossible. This could be a possible explanation for the anterior hip pain in sitting positions in patients with pincer-type FAI due to AR.2,60 We recommend asking all patients presenting with AR if they experience hip pain in sitting position.
This study has limitations. First, these radiological parameters are parameters for sagittal balance and were measured on pelvic CT scans that were acquired in supine position, without taking into account functional parameters in sitting or squatting positions. We do not report on parameters for the lumbar or thoracic spine because these were not visible on the pelvic CT scans. In addition, we do not report 3D impingement simulation37 or clinical outcome because this was beyond the scope of this study. Second, we had a low number of hips with total AR and with high acetabular anteversion. Total AR is a relatively rare hip morphology and the 15 hips in our study represent the total number available with a CT scan and a complete radiological dataset. Third, we did not report clinical outcomes of these patients. This was not the aim of this study. In addition, femoral head coverage was assessed with a previously validated software based on 2D AP radiographs, without correction of PT or pelvic rotation. This is a relevant parameter for surgical therapy decision-making (acetabular rim trimming vs acetabular reorientation). The 3D assessment of the femoral head coverage could be part of further studies. In addition, measurement of the iliac wing angle was not adapted to the APP. However, because the APP angle was not significantly different between hips with AR and hip dysplasia, we believe that no adaptation/normalization is needed. Last, we investigated patients that presented in a university hospital, which could lead to a potential selection bias of complex patients. This bias was reduced with analysis of a consecutive patient cohort and standardized evaluation. Compared to other studies,13 we included more female patients, which is probably due to the higher prevalence of pincer-type FAI and hip dysplasia in women.1,2
In summary, this study investigated sagittal balance in symptomatic FAI patients with AR. We found a lower PT and lower PI and an increased external rotation of the iliac wing in patients with AR compared to hip dysplasia. Patients with AR have a rotational abnormality of the iliac wing. This could contribute to a better understanding of hip pain in sitting position and extra-articular subspine FAI of these patients37 . This study has implications for surgical treatment with hip arthroscopy or with anteverting PAO. Theoretically, external rotation of the iliac wing could be corrected with anteverting PAO because the AIIS is rotated internally during this operation. AR seems to affect the sagittal balance and lumbar lordosis. Non-surgical treatment of total AR attempting to modify the functional pelvic position could be difficult due to low PI.
Take home message
- Pelvic incidence and pelvic tilt were low in hips with acetabular retroversion (AR).
- We found an increased external rotation of the iliac wing in hips with AR; this could be a rotational abnormality of the iliac wing.
- These findings have implications for surgical treatment with hip arthroscopy with acetabular rim trimming or with anteverting periacetabular osteotomy and for non-surgical treatment (posterior pelvic tilt taping).
Acknowledgements
T. D. Lerch, F. Schmaranzer, and M. Tannast received research funding from the Swiss National Science Foundation.
Footnotes
Author contributions: T. D. Lerch: Formal analysis, Visualization, Writing – original draft, Writing – review & editing.
A. Boschung: Investigation.
F. Schmaranzer: Writing – review & editing.
I. A. S. Todorski: Investigation.
J. Van Lommel: Writing – original draft.
K. A. Siebenrock: Supervision.
S. D. Steppacher: Supervision, Conceptualization, Formal analysis, Visualization.
M. Tannast: Supervision, Conceptualization, Formal analysis, Visualization, Writing – review & editing.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. The open access fee was funded by Inselspital Bern, Bern University Hospital, University of Bern, Bern, Switzerland.
Ethical review statement: Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Supplementary material: Supplemental material contains figures for description of the methods and a literature table for comparison of the results.
Contributor Information
Till Dominic Lerch, Email: till.lerch@insel.ch.
Adam Boschung, Email: boschunga@gmail.com.
Florian Schmaranzer, Email: florian.schmaranzer@insel.ch.
Inga A. S. Todorski, Email: inga.todorski@insel.ch.
Jan Vanlommel, Email: janvanlommel@hotmail.com.
Klaus A. Siebenrock, Email: klaus.siebenrock@insel.ch.
Simon D. Steppacher, Email: simon.steppacher@gmail.com.
Moritz Tannast, Email: moritz.tannast@unifr.ch.
References
- 1. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 2. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188(6):1540–1552. [DOI] [PubMed] [Google Scholar]
- 3. Schmaranzer F, Hanke M, Lerch T, Steppacher S, Siebenrock K, Tannast M. Impingement of the hip. Radiologe. 2016;56(9):825–838. [DOI] [PubMed] [Google Scholar]
- 4. Byrd JWT, Jones KS. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39(Suppl:7S–13S). [DOI] [PubMed] [Google Scholar]
- 5. Kakaty DK, Fischer AF, Hosalkar HS, Siebenrock KA, Tannast M. The ischial spine sign: does pelvic tilt and rotation matter? Clin Orthop Relat Res. 2010;468(3):769–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466(3):677–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tannast M, Pfannebecker P, Schwab JM, Albers CE, Siebenrock KA, Büchler L. Pelvic morphology differs in rotation and obliquity between developmental dysplasia of the hip and retroversion. Clin Orthop Relat Res. 2012;470(12):3297–3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maldonado DR, Chen JW, Kyin C, et al. Hips with acetabular retroversion can be safely treated with advanced arthroscopic techniques without anteverting periacetabular osteotomy: Midterm outcomes with propensity-matched control group. Am J Sports Med. 2020;48(7):1636–1646. [DOI] [PubMed] [Google Scholar]
- 9. Parry JA, Swann RP, Erickson JA, Peters CL, Trousdale RT, Sierra RJ. Midterm outcomes of reverse (anteverting) periacetabular osteotomy in patients with hip impingement secondary to acetabular retroversion. Am J Sports Med. 2016;44(3):672–676. [DOI] [PubMed] [Google Scholar]
- 10. Zurmühle CA, Anwander H, Albers CE, et al. Periacetabular osteotomy provides higher survivorship than rim trimming for acetabular retroversion. Clin Orthop Relat Res. 2017;475(4):1138–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Steppacher SD, Lerch TD, Gharanizadeh K, Liechti EF, Werlen SF, Puls M. Size and shape of the lunate surface in different types of pincer impingement: theoretical implications for surgical therapy. Osteoarthritis Cartilage. 2014;22(7):951–958. [DOI] [PubMed] [Google Scholar]
- 12. Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. [DOI] [PubMed] [Google Scholar]
- 13. Hellman MD, Haughom BD, Brown NM, Fillingham YA, Philippon MJ, Nho SJ. Femoroacetabular impingement and pelvic incidence: Radiographic comparison to an asymptomatic control. Arthroscopy. 2017;33(3):545–550. [DOI] [PubMed] [Google Scholar]
- 14. Weinberg DS, Gebhart JJ, Liu RW, Salata MJ. Radiographic signs of femoroacetabular impingement are associated with decreased pelvic incidence. Arthroscopy. 2016;32(5):806–813. [DOI] [PubMed] [Google Scholar]
- 15. Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dai J, Yu X, Huang S, Fan L, Zhu G, Sun H. Relationship between sagittal spinal alignment and the incidence of vertebral fracture in menopausal women with osteoporosis: a multicenter longitudinal follow-up study. Eur Spine J. 2015;24(4):737–743. [DOI] [PubMed] [Google Scholar]
- 17. Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine. 2002;27(18):2026–2029. [DOI] [PubMed] [Google Scholar]
- 18. Tiziani S, Gautier L, Farei-Campagna J, Osterhoff G, Jentzsch T, Nguyen-Kim TDL. Correlation of pelvic incidence with radiographical parameters for acetabular retroversion: a retrospective radiological study. BMC Med Imaging. 2015;15:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the ‘cross-over-sign. J Orthop Res. 2007;25(6):758–765. [DOI] [PubMed] [Google Scholar]
- 20. Tannast M, Fritsch S, Zheng G, Siebenrock KA, Steppacher SD. Which radiographic hip parameters do not have to be corrected for pelvic rotation and tilt? Clin Orthop Relat Res. 2015;473(4):1255–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tannast M, Murphy SB, Langlotz F, Anderson SE, Siebenrock KA. Estimation of pelvic tilt on anteroposterior X-rays--a comparison of six parameters. Skeletal Radiol. 2006;35(3):149–155. [DOI] [PubMed] [Google Scholar]
- 22. Tani T, Takao M, Uemura K, et al. Posterior pelvic tilt from supine to standing in patients with symptomatic developmental dysplasia of the hip. J Orthop Res. 2020;38(3):578–587. [DOI] [PubMed] [Google Scholar]
- 23. Tachibana T, Fujii M, Kitamura K, Nakamura T, Nakashima Y. Does acetabular coverage vary between the supine and standing positions in patients with hip dysplasia? Clin Orthop Relat Res. 2019;477(11):2455–2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tönnis D. General radiography of the hip joint. : Congenital Dysplasia and Dislocation of the Hip in Children and Adults. New York, New York, USA: Springer. 1987: 100–142. [Google Scholar]
- 25. Lerch TD, Todorski IAS, Steppacher SD, et al. Prevalence of femoral and acetabular version abnormalities in patients with symptomatic hip disease: A controlled study of 538 hips. Am J Sports Med. 2018;46(1):122–134. [DOI] [PubMed] [Google Scholar]
- 26. Lerch TD, Vuilleumier S, Schmaranzer F, Ziebarth K, Steppacher SD, Tannast M. Patients with severe slipped capital femoral epiphysis treated by the modified Dunn procedure have low rates of avascular necrosis, good outcomes, and little osteoarthritis at long-term follow-up. Bone Joint J. 2019;101–B(4):403–414. [DOI] [PubMed] [Google Scholar]
- 27. Tannast M, Macintyre N, Steppacher SD, Hosalkar HS, Ganz R, Siebenrock KA. A systematic approach to analyse the sequelae of LCPD. Hip Int. 2013;23(Suppl 9):S61-70. [DOI] [PubMed] [Google Scholar]
- 28. Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res. 2015;473(4):1234–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81-B(2):281–288. [DOI] [PubMed] [Google Scholar]
- 30. Siebenrock KA, Schaller C, Tannast M, Keel M, Büchler L. Anteverting periacetabular osteotomy for symptomatic acetabular retroversion: results at ten years. J Bone Joint Surg Am. 2014;96-A(21):1785–1792. [DOI] [PubMed] [Google Scholar]
- 31. Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84-B(4):556–560. [DOI] [PubMed] [Google Scholar]
- 32. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81-A(12):1747–1770. [DOI] [PubMed] [Google Scholar]
- 33. Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26(9):1199–1205. [DOI] [PubMed] [Google Scholar]
- 34. Lerch TD, Steppacher SD, Liechti EF, Siebenrock KA, Tannast M. Bernese periacetabular osteotomy: Indications, technique and results 30 years after the first description. Orthopade. 2016;45(8):687–694. [DOI] [PubMed] [Google Scholar]
- 35. Lerch TD, Steppacher SD, Liechti EF, Tannast M, Siebenrock KA. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res. 2017;475(4):1154–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Naal FD, Hatzung G, Müller A, Impellizzeri F, Leunig M. Validation of a self-reported Beighton score to assess hypermobility in patients with femoroacetabular impingement. Int Orthop. 2014;38(11):2245–2250. [DOI] [PubMed] [Google Scholar]
- 37. Lerch TD, Siegfried M, Schmaranzer F, et al. Location of intra- and extra-articular hip impingement is different in patients with pincer-type and mixed-type femoroacetabular impingement due to acetabular retroversion or protrusio acetabuli on 3d CT-based impingement simulation. Am J Sports Med. 2020;48(3):661–672. [DOI] [PubMed] [Google Scholar]
- 38. Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87-A(2):260–267. [DOI] [PubMed] [Google Scholar]
- 39. Fujii M, Nakashima Y, Sato T, Akiyama M, Iwamoto Y. Pelvic deformity influences acetabular version and coverage in hip dysplasia. Clin Orthop Relat Res. 2011;469(6):1735–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fujii M, Nakamura T, Hara T, Nakashima Y, Iwamoto Y. Does radiographic coxa profunda indicate increased acetabular coverage or depth in hip dysplasia. Clin Orthop Relat Res. 2015;473(6):2056–2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Montgomery AA, Graham A, Evans PH, Fahey T. Inter-rater agreement in the scoring of abstracts submitted to a primary care research conference. BMC Health Serv Res. 2002;2(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gebhart JJ, Streit JJ, Bedi A, Bush-Joseph CA, Nho SJ, Salata MJ. Correlation of pelvic incidence with cam and pincer lesions. Am J Sports Med. 2014;42(11):2649–2653. [DOI] [PubMed] [Google Scholar]
- 43. Legaye J, Duval-Beaupere G, Barrau A, et al. Relationship between sacral pelvic incidence and acetabular orientation. Hip Int. 2011;21(1):87–97. [DOI] [PubMed] [Google Scholar]
- 44. Weinberg DS, Morris WZ, Gebhart JJ, Liu RW. Pelvic incidence: an anatomic investigation of 880 cadaveric specimens. Eur Spine J. 2016;25(11):3589–3595. [DOI] [PubMed] [Google Scholar]
- 45. Griffin DR, Dickenson EJ, O’Donnell J, Agricola R, Awan T, Beck M. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169–1176. [DOI] [PubMed] [Google Scholar]
- 46. Mascarenhas VV, Rego P, Dantas P, Morais F, McWilliams J, Collado D. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: A systematic review. Eur J Radiol. 2016;85(1):73–95. [DOI] [PubMed] [Google Scholar]
- 47. Laborie LB, Lehmann TG, IØ E, Eastwood DM, Engesæter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260(2):494–502. [DOI] [PubMed] [Google Scholar]
- 48. Okuzu Y, Goto K, Okutani Y, Kuroda Y, Kawai T, Matsuda S. Hip-spine syndrome: Acetabular anteversion angle is associated with anterior pelvic tilt and lumbar hyperlordosis in patients with acetabular dysplasia: A retrospective study. JB JS Open Access. 2019;4(1):e0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mangione P, Gomez D, Senegas J. Study of the course of the incidence angle during growth. Eur Spine J. 1997;6(3):163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15(4):415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Sagittal parameters of global spinal balance: Normative values from a prospective cohort of seven hundred nine caucasian asymptomatic adults. Spine (Phila Pa 1976). 2010;35(22):E1193-1198. [DOI] [PubMed] [Google Scholar]
- 52. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30(3):346–353. [DOI] [PubMed] [Google Scholar]
- 53. Lazennec JY, Brusson A, Rousseau MA. Hip-spine relations and sagittal balance clinical consequences. Eur Spine J. 2011;20(Suppl 5):686–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Grammatopoulos G, Salih S, Beaule PE, Witt J. Spinopelvic characteristics in acetabular retroversion: Does pelvic tilt change after periacetabular osteotomy? Am J Sports Med. 2020;48(1):181–187. [DOI] [PubMed] [Google Scholar]
- 55. Daley E, Nahm N, Koueiter D, Zaltz I. Does compensatory anterior pelvic tilt decrease after bilateral periacetabular osteotomy? Clin Orthop Relat Res. 2019;477(5):1168–1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord Tech. 2003;16(1):44–50. [DOI] [PubMed] [Google Scholar]
- 57. Itoi E. Roentgenographic analysis of posture in spinal osteoporotics. Spine. 1991;16(7):750–756. [DOI] [PubMed] [Google Scholar]
- 58. Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34(17):E599-606. [DOI] [PubMed] [Google Scholar]
- 59. Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine. 2005;30(14):1650–1657. [DOI] [PubMed] [Google Scholar]
- 60. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lee KS, Yoo WG, Kim MH, Oh J-S, Lee K-S, Han JT. Effect of posterior pelvic tilt taping in women with sacroiliac joint pain during active straight leg raising who habitually wore high-heeled shoes: A preliminary study. J Manipulative Physiol Ther. 2014;37(4):260–268. [DOI] [PubMed] [Google Scholar]
- 62. Falk Brekke A, Overgaard S, Hróbjartsson A, Holsgaard-Larsen A. Non-surgical interventions for excessive anterior pelvic tilt in symptomatic and non-symptomatic adults: a systematic review. EFORT Open Rev. 2020;5(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Patel RV, Han S, Lenherr C, Harris JD, Noble PC. Pelvic tilt and range of motion in hips with femoroacetabular impingement syndrome. J Am Acad Orthop Surg. 2020;28(10):e432–e427. [DOI] [PubMed] [Google Scholar]