Abstract
Aims
The aim of this meta-analysis is to assess the association between exchange of modular parts in debridement, antibiotics, and implant retention (DAIR) procedure and outcomes for hip and knee periprosthetic joint infection (PJI).
Methods
We conducted a systematic search on PubMed, Embase, Web of Science, and Cochrane library from inception until May 2021. Random effects meta-analyses and meta-regression was used to estimate, on a study level, the success rate of DAIR related to component exchange. Risk of bias was appraised using the (AQUILA) checklist.
Results
We included 65 studies comprising 6,630 patients. The pooled overall success after DAIR for PJI was 67% (95% confidence interval (CI) 63% to 70%). This was 70% (95% CI 65% to 75%) for DAIR for hip PJI and 63% (95% CI 58% to 69%) for knee PJI. In studies before 2004 (n = 27), our meta-regression analysis showed a 3.5% increase in success rates for each 10% increase in component exchange in DAIR for hip PJI and a 3.1% increase for each 10% increase in component exchange for knee PJI. When restricted to studies after 2004 (n = 37), this association changed: for DAIR for hip PJI a decrease in successful outcome by 0.5% for each 10% increase in component exchange and for DAIR for knee PJI this was a 0.01% increase in successful outcome for each 10% increase in component exchange.
Conclusion
This systematic review and meta-regression found no benefit of modular component exchange on reduction of PJI failure. This limited effect should be weighed against the risks for the patient and cost on a case-by-case basis. The association between exchange of modular components and outcome changed before and after 2004. This suggests the effect seen after 2004 may reflect a more rigorous, evidence-based, approach to the infected implant compared to the years before.
Level of Evidence: Level III
Cite this article: Bone Jt Open 2021;2(10):806–812.
Keywords: Periprosthetic joint infection; DAIR; Modular component exchange; Total joint replacement; debridement, antibiotics, and implant retention; hips; knee periprosthetic joint infection; Periprosthetic joint infection (PJI); knees; regression analysis; revision arthroplasties; randomized controlled trials; debridement; lower limb arthroplasties
Introduction
Periprosthetic joint infection (PJI) is a devastating complication for patients following total joint replacement, often leading to multiple surgical procedures, prolonged antibiotic treatment, substantial patient morbidity, and increased mortality.1,2 At present, debridement, antibiotics, and implant retention (DAIR) is considered the best treatment modality for patients presenting with early PJI.3 The advantage of a DAIR procedure for a patient is that the well-fixed implant remains, with lower morbidity and costs.4 As for late presentation of PJI, success rates are less favourable, which is explained by the presence of a more mature biofilm, often requiring removal of the implant.5 DAIR procedure can be performed with and without exchange of modular components (i.e. liners and heads). Exchange of modular components is advocated to provide the most optimal surgical access to the implant, in order to decrease bacterial load and disrupt the biofilm, and thereby increase efficacy of debridement.6 However, controversy exists whether exchange of modular components does reduce PJI recurrence rates.7 Furthermore, removal of modular components may require considerable force, which may jeopardize the cement-implant or bone-implant fixation, leading to immediate or potential late loosening of components. Some recent studies have achieved success rates of more than 80% without exchange of component, but no well-designed randomized controlled trials (RCTs) exist.7,8 These high success rates of DAIR procedures for PJI without modular component exchange challenge the practice of routine liner exchange.
In light of this equipoise, our study aimed to perform a meta-analysis and systematic review on whether the success rate after DAIR is related to modular component exchange, while taking into account possible effect modifiers such as study year and risk of bias items.
Methods
The reporting of this systematic review and meta-regression is in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and a protocol was produced before the start of the study.9
The population of interest consisted of patients with PJI in total hip or knee arthroplasty who were treated with DAIR. The outcome of interest was success rate after a DAIR, defined as eradication of infection, in terms of absence of recurrence (as defined in each paper), absence of long-term antibiotic suppression, and absence of subsequent resection (one- or two-stage procedure) during follow-up of the prosthetic joint replacement. Hemiarthroplasties and hip resurfacing procedures were not included. All observational studies (i.e. case control, cohort, or case series) were considered eligible for inclusion. Studies including both primary and revision arthroplasties were included and subjected to later sensitivity analyses. Studies with all follow-up duration were considered. We used meta-regression to determine, at a study level, the association between percentage of exchange of modular components (i.e. liners and/or heads) and success rate.10 Studies were excluded when it was unclear whether the components were actually exchanged. The hypothesis was that, on average, studies with high percentages of component exchange would produce higher success rates than studies with low percentages of component exchange. This hypothesis was further tested by classifying the included studies into three treatment strategies based on the percentage of component exchange (high-intermediate-low). Pooled success rates were determined for each group. We defined these three groups as follows: high component exchange (75% to 100% component exchange), intermediate component exchange (26% to 74% component exchange), and low component exchange (0% to 25% component exchange).
Data sources and search strategy
The literature search was designed and conducted by the first reviewer (MG) and an experienced librarian (JS). The following databases were searched from their inception up to and including 14 May 2021: PubMed, Embase, Web of Science, and the Cochrane Library. Articles in languages spoken by the review team were considered: English, German, French, Spanish, and Dutch. Bibliographies of relevant articles were cross-checked for references missing in the original search. No restrictions regarding patient background and year of publication applied. Further details regarding the search strategy are presented in Supplementary Material.
Study selection
Two reviewers (MG, AK) independently screened the titles and abstracts of studies identified by the search strategy. Both reviewers recorded their findings in an electronic database that was designed before the start of the screening. These databases were compared and any disagreement was resolved by consensus or by consulting a referee (BP). The studies remained eligible when the information in the abstract did not suffice or if any doubt remained.
The same reviewers also independently evaluated the full-text papers of eligible studies against the inclusion and exclusion criteria. Any disagreement was resolved by consensus or by consulting the referee. We included cohort studies reporting outcome of patients with hip and/or knee PJI after DAIR if the outcome could be related to the exchange of modular components. We excluded: studies with fewer than 20 patients; non-original data publications such as editorials and reviews; studies not available in full text (e.g. conference proceedings); and prosthetic implants not concerning a joint, i.e. osteosynthesis implants, arthrodesis.
Data extraction and quality assessment
The two reviewers independently extracted data and appraised the risk of bias from included studies regarding the outcome of interest, patient demographic details, and study characteristics in a predefined electronic datasheet. Results for total knee arthroplasty (TKA) and total hip arthroplasty (THA) were extracted separately to allow for a separate analysis on TKA and THA. When there were multiple publications or overlapping publications on the same patient cohort, the most comprehensive publication was included.
Quality assessment was scored and assessed independently by two authors (MG, AK). Risk of bias was appraised using the Assessment of Quality In Lower limb Arthroplasty (AQUILA) tool.11 AQUILA is specifically designed to assess the methodological quality of observational studies on lower limb arthroplasties.11,12
Statistical analysis
For the meta-analysis, a random-effects model was used to pool the success rates of individual studies in order to estimate an overall success rate and 95% confidence intervals (CIs) for each predefined level/stratum of modular component exchange. The three treatment categories were based on the percentage of component exchange: high component exchange (75% to 100%), intermediate component exchange (26% to 74%), and low component exchange (0% to 25%).
Statistical heterogeneity between studies was assessed by calculating I2 statistics.13 The I2 statistic estimates the extent to which the total variability in the effect size estimates is due to heterogeneity among the true effects. In the presence of heterogeneity, a random-effects meta-regression on the predefined factors (study-level covariates) rate of component exchange, study year, mix of primary and revision arthroplasties, and risk of bias items was performed. To account for the increasing success rate of DAIR during the studied time period, a subgroup analysis on studies before and after the year 2000 and 2004 was performed.14,15 For determination of the time of the study cohort, the median of the study period was used.
All analyses were performed using the metafor package in R statistics (the Netherlands).16 In line with recent recommendations, estimates and corresponding CIs are reported, while p-values are not reported.17
Results
Study selection and study characteristics
Our literature search revealed 2,106 papers, of which 1,322 were unique (no double entries for different databases). After abstract selection, based on inclusion criteria 65 studies, encompassing 6,630 patients, were included (Figure 1 and Supplementary Material).
Fig. 1.
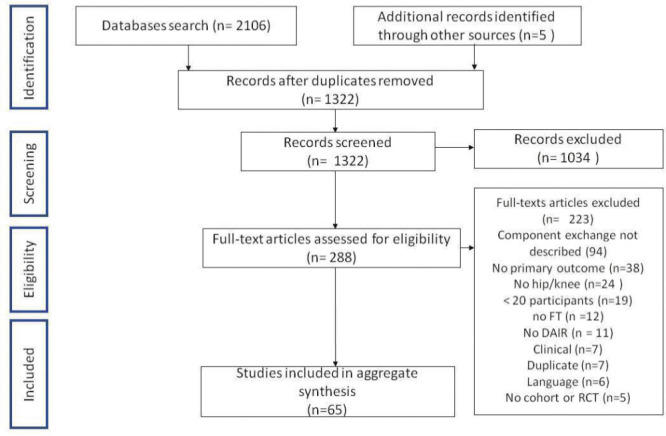
Flowchart of literature selection.
From the included studies, 23 were from the USA, eight from Spain, five from the UK, five from South Korea, four from Sweden, three from Germany, two from Switzerland, two from Norway, three from China, two from Finland, one from Denmark, one from the Netherlands, one from Belgium, one from Canada, one from Japan, one from New Zealand, and two from a consortium of West European countries. The mean age at point of DAIR procedure was 69 years (58 to 81), and 52% (21% to 83%) were female. All patients had a DAIR procedure for PJI (mean number of performed DAIRs: 1.1 (1 to 1.45)). Mean follow-up was 44 months (2 to 84) for all included cohorts. Overall, study level data were available for 3,071 patients with hip PJI and 3,559 patients with knee PJI, with a mean study size of 104 (24 to 1,174) patients per study. A total of 20 studies were mixed cohorts consisting of both hip and knee PJI.
Treatment success and exchange of modular parts
The overall pooled success rate of all included studies was 67% (95% CI 63% to 70%), with substantial heterogeneity (I2 = 95%). DAIR in hips appeared to be more successful than DAIR in knees but the CIs overlapped: the success rate for hips was 70% (95% CI 65% to 75%), and for knees 63% (95% CI 58% to 69%).
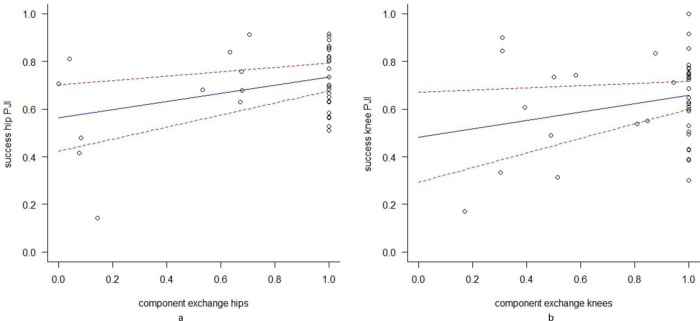
The overall meta-regression model showed that the success rate after DAIR for hip PJI increased by 1.7% (95% CI 0.1% to 3.3%) for each 10% increase in component exchange and that the success rate after DAIR for knee PJI increased by 1.8% (95% CI 0.04% to 3.9%) for each 10% increase in component exchange (Figures 2a and 2b).
Fig. 2.
a) Scatterplot showing the association between exchange of modular components and successful outcome of debridement, antibiotics, and implant retention (DAIR) for hip periprosthetic joint infection (PJI). The results from the meta-regression are presented as a blue line with red 95% confidence interval (CI). Both variables are presented as proportions of all included hips in the study cohort. b) Scatterplot showing the association between exchange of modular components and successful outcome of DAIR for knee PJI. The results from the meta-regression are presented as a blue line with red 95% CI. Both variables are presented as proportions of all included knees in the study cohort.
The success rates per category of exchange of modular parts (subgroup analysis) are presented in Table I and Table II. The pooled success rate for DAIR for hip PJI in the intermediate component exchange (26% to 74% exchange) group was 78% (95% CI 68% to 88%), which was similar to the success rate of the high component exchange (75% to 100%) group, which was 72% (95% CI 67% to 77%) (Table I).
Table I.
Pooled success rate for debridement, antibiotics, and implant retention for hip periprosthetic joint infection per category (low/medium/high) of exchange of modular parts for included cohorts.
| Component exchange | Studies, n | DAIR for hip PJI, n | Treatment success, % (95% CI) |
|---|---|---|---|
| Low (0% to 25%) | 5 | 252 | 51 (28 to 75) |
| Intermediate (26% to 74%) | 6 | 1,397 | 78 (68 to 88) |
| High (75% to 100%) | 28 | 1,422 | 72 (67 to 77) |
| Overall | 29 | 3,071 | 70 (65 to 75) |
CI, confidence interval; DAIR, debridement, antibiotics, and implant retention; PJI, periprosthetic joint infection.
Table II.
Pooled success rate per treatment strategy for debridement, antibiotics, and implant retention for knee periprosthetic joint infection per category (low/medium/high) of exchange of modular parts for included cohorts.
| Component exchange | Studies, n | DAIR for knee PJI | Treatment success, % (95% CI) |
|---|---|---|---|
| Low (0% to 25%) | 1 | 35 | 17 (4.7 to 30) |
| Intermediate (26% to 74%) | 8 | 881 | 61 (47 to 75) |
| High (75% to 100%) | 37 | 643 | 65 (60 to 70) |
| Overall | 46 | 3,559 | 63 (58 to 69) |
CI, confidence interval; DAIR, debridement, antibiotics, and implant retention; PJI, periprosthetic joint infection.
For DAIR for knee PJI the success rate in the intermediate component exchange group was 61% (95% CI 47% to 75%), which is similar to the success rate of the high component exchange group, which was 65% (95% CI 60% to 70%) (Table II). The low component exchange (0% to 25%) group for both hip and knee PJI showed low pooled success rates (respectively 51% and 17%). However, both of these estimated success rates are based on a low number of studies (five studies and one study, respectively) and the confidence intervals were wide (Table I and Table II).
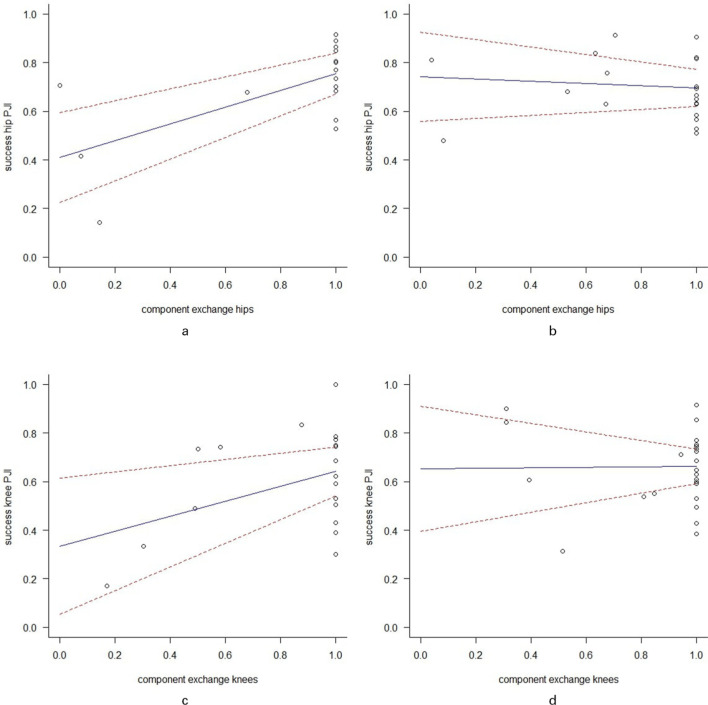
Sensitivity analyses
Our analysis suggested an overall improvement in DAIR for hip and knee PJI outcome over time: for every ten years the success rate increased by 3.8% (95% CI -4.2% to 2%) for hip PJI and 7.0% for knee PJI (95% CI -1.8% to 16%). To account for the increasing success rate of DAIR during the studied time period, we performed a subgroup analysis on studies before and after the year 2000 and 2004 (Table III and Table IV). In studies before 2004 (27 studies), our meta-regression analysis showed a 3.5% increase in success rates for each 10% increase in component exchange in DAIR for hip PJI and a 3.1% increase for each 10% increase in component exchange in DAIR for knee PJI (Figures 3a and 3c). When limiting the meta-analysis to studies performed after 2004 (37 studies), this association changed: for DAIR for hip PJI a decrease in successful outcome by 0.5% for each 10% increase in component exchange and for DAIR for knee PJI this was a 0.01% increase in successful outcome for each 10% increase in component exchange (Figures 3b and 3d). In 28 studies, DAIR procedures were performed in a mix of primary and revision arthroplasties. Therefore, a sensitivity analysis was performed. In the meta-regression model, the mix of primary and revision arthroplasties was not an effect modifier on the association between rate of component exchange and success rate of DAIR procedure. Follow-up duration did not affect the success rate for knee PJI and hip PJI. Rate of resistant pathogens did not affect the success rate for knee PJI and hip PJI.
Table III.
Regression analysis for component exchange per time period.
| Component exchange | Hip success* | Knee success* |
|---|---|---|
| Coefficient, % (SE; 95% CI) | Coefficient, % (SE; 95% CI) | |
| Pre-2000 | 1.9 (2.5; -3.0 to 6.8) | 3.3 (2.6; -1.8 to 8.4) |
| Post-2000 | 1.0 (0.9; -0.0 to 2.7) | 0.2 (1.2; -2.1 to 2.6) |
For each 10% increase in component exchange.
CI, confidence interval; SE, standard error.
Table IV.
Regression analysis for component exchange per time period.
| Component exchange | Hip success* | Knee success* |
|---|---|---|
| Coefficient, % (SE; 95% CI) | Coefficient, % (SE; 95% CI) | |
| Pre-2004 | 3.5 (1.1; 1.4 to 5.5) | 3.1 (1.6; 0.0 to 6.2) |
| Post-2004 | -0.0 (1.1; -2.6 to 1.7) | 0.0 (1.4; -2.7 to 2.9) |
For each 10% increase in component exchange.
CI, confidence interval; SE, standard error.
Fig. 3.
Scatterplot showing the association between exchange of modular components and successful outcome of hips after debridement, antibiotics, and implant retention (DAIR) procedure. The results from the meta-regression is presented as a blue line with red 95% confidence interval (CI). Both variables are presented as proportions of all included hips in the study cohort. a) represents studies starting cohort inclusion before the year 2004. b) represents studies starting cohort inclusion after the year 2004. Scatterplot showing the association between exchange of modular components and successful outcome of knees after DAIR procedure. The results from the meta-regression is presented as a blue line with red 95% CI. Both variables are presented as proportions of all included knees in the study cohort. c) represents studies starting cohort inclusion before the year 2004. d) represents studies starting cohort inclusion after the year 2004.
Risk of bias
The mean AQUILA methodological quality score was 7.5 points out of a maximum of 11 points (3 to 10) and was not an effect modifier on the association between rate of component exchange and success rate of DAIR procedure. The main methodological flaw concerned outcome at follow-up. Two out of 65 studies did not include a comprehensive primary research question. These studies both analyzed patient outcome (clinical series) and developed an algorithm for treatment outcome (prognostic).18,19 In 20 out of 65 studies the follow-up was pre-defined. In 38 out of 65 studies the follow-up was performed when patients had complaints or chart review (of non-predefined follow-up) and in seven out of 65 studies it was unclear how the follow-up was performed. Table V displays the methodological score for each item.
Table V.
Assessment of Quality In Lower Limb Arthroplasty score for included articles.
| AQUILA methodological quality items | Studies, n |
|---|---|
| 1. Is there a clear primary research question/hypothesis? | Yes: 64 of 65 |
|
2. How were the cohorts constructed?
A: Consecutively B: Non-consecutively C: Unknown |
A: 44 of 65 B: 20 of 65 C: 1 of 65 |
|
3. How adequate was the follow-up?
A: Fully completed follow-up B: ≤ 5% lost-to-follow-up or follow-up quotient is ≤ 1 C: > 5% lost-to-follow-up or follow-up quotient is > 1 D: Unknown |
A: 29 of 65 B: 8 of 65 C: 11 of 65 D: 17 of 65 |
|
4. How was the follow-up performed?
A: Predefined (e.g. yearly) B: When the patient had complaints or follow-up C: Unknown |
A: 20 of 65 B: 38 of 65 C: 7 of 65 |
|
5. How many arthroplasties are at risk at the follow-up of interest?
A: ≥ 20 B: < 20 C: Unknown |
A: 60 of 65 B: 2 of 65 C: 3 of 65 |
| 6. Has a worst-case analysis or competing risk analysis for competing endpoints been performed? | Yes: 1 of 65 |
AQUILA, Assessment of Quality In Lower Limb Arthroplasty.
Discussion
Summary of evidence
In this systematic review and meta-regression we evaluated the association between rate of modular component exchange and success rate of hip and knee PJI after DAIR. Our results showed that the success rate for hip DAIRs increased by 2.6% for each 10% increase in component exchange and that the success rate for knee DAIRs increased by 2.0% for each 10% increase in component exchange. These results suggest that modular component exchange could be beneficial in reducing PJI recurrence rate. However, when restricted to studies after the year 2004, to reflect more modern PJI treatment protocols,14,15,20 there was no effect of the rate of component exchange on success rate of the studies.
Additionally, we observed no difference in pooled success rates between studies performing high (75% to 100%) and intermediate component exchange (26% to 74%) in DAIR for both hip and knee PJI, suggesting increase of component exchange does not alter outcome. Further research, preferably well-designed RCTs, are needed to evaluate the effect of modular component exchange on PJI recurrence rate. We are not aware of any other meta-regressions on this subject, however some observational studies suggest a beneficial effect of component exchange.21,22 These studies are of observational design and are susceptible to confounding and bias. Therefore there is clinical equipoise and RCTs are needed.
The purpose of effective debridement is reducing the bacterial load and disruption of the biofilm.6 In this, exchange of modular parts was advocated to effectively reduce the surface adhering bacterial load on modular parts and allow more effective debridement due to better surgical exposure, and therefore improve outcome. However, biofilm on bone-anchored parts (e.g. hip stem) is not removed with modular component exchange alone, so it may well be that modular component exchange is a proxy for early adaptation of now widespread treatment protocols in studies before 2004.
Two recent systematic reviews by Tsang et al14 and Kunutsor et al15 have shown that the success rate of DAIRs has improved in the last decades and they suggested that possible explanations for this improvement could be enhanced surgical techniques, newer and more effective antibiotic therapies, and timing of DAIR after the onset of symptoms. Similarly, improved awareness, more effective surgery technique, development of specialized surgery tools, standardized diagnostic criteria, and multidisciplinary treatment teams consisting of orthopaedic surgeons, microbiologists, and infectious disease specialists are likely to have an increasing influence on improved outcome.8,23,24 Consequently, the absolute influence of exchange on outcome after DAIR could have faded, and therefore shown no effect of exchange of modular parts in our analyses. This complexity and interaction between these different factors are potential confounders for the association between modular component exchange and PJI recurrence rate, and may explain the observed lack of effectiveness of modular component exchange in studies after 2004.
Some limitations exist: first, all included studies were observational and subject to bias and confounding. Nevertheless, we included a relatively large number of 65 studies with a total of 6,630 patients. This large number of included studies allowed for a meta-regression analysis showing a relatively small effect of modular component exchange, and this effect was no longer present in subsequent sensitivity analyses. Statistical analyses were limited by the small number of studies, with low rate of component exchange among those included.
Reporting on the extent of modular component exchange was not always adequate. As a result, it was not always clear which modular components were exchanged, e.g. the femoral head with or without the acetabular insert. Improved reporting would thus be beneficial in the future. Additionally, the methodological quality of the included studies was moderate as measured with the AQUILA score. Therefore, future studies could benefit from improved methodological quality by adding a competing risk analysis with death as a competing risk and by pre-defining patient follow-up. However, the results of the meta-regression were not influenced by the methodological quality.
Our review has the following strengths: it was the first in investigating the effect of exchange of modular parts in a large number of studies in combination with correction for important confounders (at a study level). All phases of the review were performed independently by two reviewers (MG, AK) and checked with a referee (BP) if needed.25 Furthermore, the lack of effect of modular component exchange remained after rigorous sensitivity analyses.
In conclusion, this systematic review and meta-regression on 6,630 patients found no clear benefit of modular component exchange on improved outcome after DAIR for PJI, suggesting that this possibly limited effect of component exchange should be weighed against the risks and cost on an individual patient basis. In light of this clinical equipoise, well-designed RCTs are needed.
Take home message
- This study showed no overall beneficial effect of component exchange based on included data (study level).
- Between 2000 and 2014, we found no effect of modular component exchange on debridement, antibiotics, and implant retention (DAIR) treatment outcome for hip and knee periprosthetic joint infection (PJI).
- The pooled overall success after DAIR was 70% for DAIR for hip PJI and 63% for knee PJI.
Footnotes
Author contributions: M. Gerritsen: Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Writing – original draft, Writing – review & editing.
A. Khawar: Data curation.
H. Scheper: Writing – review & editing.
R. van der Wal: Writing – review & editing.
J. Schoones: Resources, Writing – review & editing.
M. de Boer: Writing – review & editing.
R. Nelissen: Resources, Supervision, Writing – review & editing.
B. Pijls: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Supervision, Writing – review & editing.
Funding statement: Although none of the authors has received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but will be directed solely to a research fund, foundation, educational institution, or other non-profit organization with which one or more of the authors are associated.
ICMJE COI statement: B. Pijls reports government funding from ZonMw (09150161810084; 451001003), unrelated to this study. B. Pijls and R. Nelissen are listed as co-inventors on a provisional patent application from the Leiden University Medical Center (WO2020/067898) regarding induction heating of infected prosthetic joint replacements - no payments have been made - and provide unpaid advice to "Implant Preservation Devices (IPD)" as part of a licence agreement of the LUMC with IPD. R. Nelissen reports an institutional grant from VENI/NWO, related to the study, and from NWA/NWO DartBac, unrelated to the study.
Open access funding: The authors confirm that the open access fee for this study was self-funded.
Supplementary material: The search strategy and the references of the included studies.
Contributor Information
Maxime Gerritsen, Email: l.m.gerritsen@lumc.nl.
Abdullah Khawar, Email: A.A.J.Khawar@lumc.nl.
Henk Scheper, Email: H.Scheper@lumc.nl.
Robert van der Wal, Email: r.j.p.van_der_wal@lumc.nl.
Jan Schoones, Email: J.W.Schoones@lumc.nl.
Mark de Boer, Email: M.G.J.de_Boer@lumc.nl.
Rob Nelissen, Email: R.G.H.H.Nelissen@lumc.nl.
Bart Pijls, Email: b.g.c.w.pijls@lumc.nl.
References
- 1. Zmistowski B, Karam JA, Durinka JB, Casper DS, Parvizi J. Periprosthetic joint infection increases the risk of one-year mortality. J Bone Joint Surg Am. 2013;95-A(24):2177–2184. [DOI] [PubMed] [Google Scholar]
- 2. Shahi A, Tan TL, Chen AF, Maltenfort MG, Parvizi J. In-hospital mortality in patients with periprosthetic joint infection. J Arthroplasty. 2017;32(3):948–952. [DOI] [PubMed] [Google Scholar]
- 3. Osmon DR, Berbari EF, Berendt AR, et al. Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(1):1–10. [DOI] [PubMed] [Google Scholar]
- 4. Sherrell JC, Fehring TK, Odum S, et al. The Chitranjan Ranawat Award: fate of two-stage reimplantation after failed irrigation and débridement for periprosthetic knee infection. Clin Orthop Relat Res. 2011;469(1):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lebeaux D, Ghigo JM, Beloin C. Biofilm-related infections: bridging the gap between clinical management and fundamental aspects of recalcitrance toward antibiotics. Microbiol Mol Biol Rev. 2014;78(3):510–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zimmerli W, Moser C. Pathogenesis and treatment concepts of orthopaedic biofilm infections. FEMS Immunol Med Microbiol. 2012;65(2):158–168. [DOI] [PubMed] [Google Scholar]
- 7. Argenson JN, Arndt M, Babis G, et al. Hip and Knee Section, Treatment, Debridement and Retention of Implant: Proceedings of International Consensus on Orthopedic Infections. J Arthroplasty. 2019;34(2S):S399–S419. [DOI] [PubMed] [Google Scholar]
- 8. Deijkers RL, van Elzakker EPM, Pijls BG. Debridement, antibiotics, and implant retention with the direct anterior approach for acute periprosthetic joint infection following primary THA. JB JS Open Access. 2020;5(2):e0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Colditz GA, Brewer TF, Berkey CS, et al. Efficacy of BCG vaccine in the prevention of tuberculosis. Meta-analysis of the published literature. JAMA. 1994;271(9):698–702. [PubMed] [Google Scholar]
- 11. Pijls BG, Dekkers OM, Middeldorp S, et al. AQUILA: assessment of quality in lower limb arthroplasty. An expert Delphi consensus for total knee and total hip arthroplasty. BMC Musculoskelet Disord. 2011;12:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cowan JB, Mlynarek RA, Nelissen RGHH, Pijls BGCW, Gagnier JJ. Evaluation of quality of lower limb arthroplasty observational studies using the Assessment of Quality In Lower limb Arthroplasty (AQUILA). J Arthroplasty. 2015;30(9):1513–1517. [DOI] [PubMed] [Google Scholar]
- 13. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 14. Tsang SJ, Ting J, Simpson AHRW, Gaston P. Outcomes following debridement, antibiotics and implant retention in the management of periprosthetic infections of the hip: a review of cohort studies. Bone Joint J. 2017;99-B(11):1458–1466. [DOI] [PubMed] [Google Scholar]
- 15. Kunutsor SK, Beswick AD, Whitehouse MR, Wylde V, Blom AW. Debridement, antibiotics and implant retention for periprosthetic joint infections: A systematic review and meta-analysis of treatment outcomes. J Infect. 2018;77(6):479–488. [DOI] [PubMed] [Google Scholar]
- 16. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3). [Google Scholar]
- 17. Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature. 2019;567(7748):305–307. [DOI] [PubMed] [Google Scholar]
- 18. Faschingbauer M, Kappe T, Trubrich A, Bieger R, Reichel H. Retention of the prosthesis in early periprosthetic infection after total hip arthroplasty. Z Orthop Unfall. 2015;153(2):192–197. [Article in German]. [DOI] [PubMed] [Google Scholar]
- 19. Morcillo D, Detrembleur C, Poilvache H, Van Cauter M, Cyr Yombi J, Cornu O. Debridement, antibiotics, irrigation and retention in prosthetic joint infection : predictive tools of failure. Acta Orthop Belg. 2020;86(4):636–643. [PubMed] [Google Scholar]
- 20. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351(16):1645–1654. [DOI] [PubMed] [Google Scholar]
- 21. Grammatopoulos G, Bolduc M-E, Atkins BL, et al. Functional outcome of debridement, antibiotics and implant retention in periprosthetic joint infection involving the hip: a case-control study. Bone Joint J. 2017;99-B(5):614–622. [DOI] [PubMed] [Google Scholar]
- 22. Kim JG, Bae JH, Lee SY, Cho WT, Lim HC. The parameters affecting the success of irrigation and debridement with component retention in the treatment of acutely infected total knee arthroplasty. Clin Orthop Surg. 2015;7(1):69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014;27(2):302–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469(11):2992–2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]