Abstract
Dipeptidyl peptidase (DPP)-4 inhibitors are oral anti-diabetic medications that block the activity of the ubiquitous enzyme DPP-4. Inhibition of this enzyme increases the level of circulating active glucagon-like peptide (GLP)-1 secreted from L-cells in the small intestine. GLP-1 increases the glucose level, dependent on insulin secretion from pancreatic β-cells; it also decreases the abnormally increased level of glucagon, eventually decreasing the blood glucose level in patients with type 2 diabetes. DPP-4 is involved in many physiological processes other than the degradation of GLP-1. Therefore, the inhibition of DPP-4 may have numerous effects beyond glucose control. In this article, we review the pleiotropic effects of DPP-4 inhibitors beyond glucose control, including their strong beneficial effects on the stress induced accelerated senescence of vascular cells, and the possible clinical implications of these effects.
Keywords: DPP-4 inhibitors, pleiotropic effects, senescence, vascular cell
Introduction
The incidence of type 2 diabetes mellitus (T2DM) is increasing worldwide because of obesity, a sedentary lifestyle, and widespread senescence. 1 T2DM is associated with various chronic complications (eg, neuropathy, nephropathy, and retinopathy), and macrovascular complications (eg, cardiovascular heart disease, stroke, and peripheral artery disease), all of which increase mortality. 2
Various classes of antidiabetic drugs have been developed to treat T2DM. Most of the researches thus far have been focused on the development of incretin-based therapies, which have become widely used treatment options in clinical practice. The 2 types of incretin-based therapies are glucagon-like peptide (GLP)-1 receptor agonists, and inhibitors of the incretin-degrading enzyme dipeptidyl peptidase-4 (DPP-4). 3
Since the first DPP-4 inhibitor was approved to treat T2DM in 2006, 10 types of DPP4 inhibitors have become available worldwide. 4 DPP-4 inhibitors lower blood glucose levels by blocking the degradation of active GLP-1 secreted from intestinal L cells and enhancing meal-stimulated insulin secretion from pancreatic β-cells.5,6 DPP-4 inhibitors also have various non-glycemic actions because of their ubiquitous distribution and numerous substrates/ligands.7,8 In particular, recent studies have revealed the protective effect of DPP-4 inhibitors against vascular senescence.9-11 In this article, we review the non-glycemic systemic actions of DPP-4 inhibitors beyond glycemic homeostasis, including and anti-aging effect on vascular endothelial cells, and discuss future clinical implications of these actions.
Dipeptidyl Peptidase-4
DPP-4, also known as T-cell activation antigen cluster of differentiation (CD)-26, or as the adenosine deaminase (ADA)-binding protein was first discovered in 1966.12-15 This unique aminopeptidase is a member of the serine peptidase/prolyl oligopeptidase gene family subclassified by structure and function into membrane-bound peptidase, fibroblast activation protein/seprase (DPP-8 and DPP-9), nonenzymatic members (DPP-6 and DPP-10), and prolyl endopeptidase. 16 DPP-4 is a 100-kDa transmembrane peptidase that cleaves the N-terminus of peptides containing proline or alanine at the penultimate position with high selectivity. 17 DPP-4 is present soluble form in plasma, seminal fluid, cerebrospinal fluid, bile, and synovial fluid; it is present in membrane-bound form in the kidneys, intestinal mucosa, hepatocytes, and vascular endothelial cells. 18 DPP-4 is expressed on T-cells, B-cells, natural killer cells, subsets of macrophages, and hematopoietic progenitor cells; it also acts as a modulator of T-cell proliferation. 19
DPP-4 Inhibitors and GLP-1 Degradation
The rapid degradation of native GLP-1 by DPP-4 is inhibited when a DPP-4 inhibitor is administered, thereby increasing the plasma level of active GLP-1. Active GLP-1 is secreted from L-cells in the distal portion of the intestine and circulates as GLP-1(7-37) and GLP-1(7-36)NH2; these peptides are cleaved by DPP-4 within minutes to generate GLP-1(9-37) and GLP-1(9-36)NH2, respectively. 20 GLP-1(9-36)NH2 is the predominate circulating form of DPP-4-cleaved GLP-1 and dose not perform typical actions of intact GLP-1, such as enhancing glucose-stimulated insulin secretion and suppressing glucagon secretion, appetite, and gastric emptying.21,22 Rather, GLP-1 (9-36) and GLP-1 (28-36) are cleaved from GLP-1 by DPP-4; they exert beneficial cardiovascular functions, such as improving left ventricular function, vasodilation, and improving intrahepatic lipid metabolism.23-25 Thus, the inhibition of DPP-4 cancels the positive effects of the GLP-1 degradation products, and the actual effect of inhibiting DPP-4 on the beneficial effects of GLP-1 degradation products on the cardiovascular system is unknown.
The plasma level of intact GLP-1 increases in DPP4−/− mice. In contrast to control group, genetic inactivation of DPP-4 leads to reduced N-terminal degradation of GLP-1 and increased plasma level of intact GLP-1, increased levels of insulin, and improved glucose tolerance in DPP4−/− mice group in vivo study. 26 Furthermore, circulating plasma DPP-4 levels in patients with T2DM are significantly higher (approximately 33%) than in controls, and the inhibition of circulating DPP-4 leads to increases in the concentration of active GLP-1 and decreases glycated hemoglobin in patients with T2DM.27,28 These gliptins are orally available; neutral or minimally active with respect to body weight, blood pressure, and lipid profile; and are well tolerated with a low risk of hypoglycemia.29,30
The Pleiotropism of DPP-4 Inhibitors
Numerous endocrine peptides, chemokines, and neuropeptides contain an alanine or proline at the N-terminus start site and can be DPP-4 substrates. Therefore, many biological actions of DPP-4 are not related to the control of glucose homeostasis because of variety of substrates and widespread expression of DPP-4. 31 This article focuses on the pleiotropic actions of DPP-4 inhibitors, including their strong beneficial effects against stress induced accelerated senescence (SIAS) of vascular endothelial cells, and the possible clinical implications.
DPP-4 inhibition and stromal cell-derived factor (SDF)-1α, brain natriuresis protein (BNP), Neuropeptide Y (NPY), and peptide YY (PYY)
SDF-1α, which is alternately derived from SDF-1β by a single SDF-1 gene, is widely expressed in numerous cell types and tissue 32,33; its expression and secretion are often induced by cellular damage. 34 SDF-1α is cleaved by soluble or transmembrane DPP-4 into SDF-1α (3-67), thus inactivating its antiviral and chemotactic properties.35,36 Because the main role of SDF-1α and its receptor CXCR4 is to enhance migration of hematopoietic stem cells, bone marrow-derived endothelial progenitor cells are mobilized from the bone marrow into the blood stream in response to SDF-1α, which is released from damaged tissue.37,38 Therefore, the inhibition of DPP-4 activity reduces degradation of SDF-1α and potentiates the SDF-1α/CXCR4 signaling pathway, resulting in greater hematopoietic progenitor cell mobilization to the ischemic injury site. 37 In addition, administration of granulocyte colony-stimulating factor (G-CSF) increases enzymatic cleavage of SDF-1α by DPP-4 in the bone marrow and generates a circulation/bone marrow SDF-1α gradient, which mobilizes stem cells into circulation.39,40 The combined strategy of G-CSF and a DPP-4 inhibitor ameliorates vascular remodeling and wound healing after myocardial infarction via direct antiapoptotic effects on ischemic myocardium and indirect effects on enhancement of mobilizing stem cells from bone merrow which circulate to the damaged heart, where they homing via SDF-1α/CXCR4 signaling pathway.37,41,42 Moreover, the DPP-4 inhibitor vildagliptin enhanced the wound closure rate over 12 weeks in patients with T2DM and complicated peripheral artery disease, compared with controls. 43 In another retrospective analysis, DPP-4 inhibitor users exhibited a lower risk of peripheral arterial disease and lower extremity amputation, compared with nonusers. 44 Furthermore, the SDF-1α/CXCR4 signaling pathway plays an important role in protecting kidney function by decreasing oxidative stress, ischemia, and fibrotic processes.45-47 Recently, Zhu et al 48 revealed that DPP-4 inhibition by DPP-4 inhibitor anagliptin enhances bone marrow-derived hematopoietic stem cell activation and inflammatory cell production via an Adrβ3 (β3-adrenergic receptor)/CXCL12 (C-X-C motif chemokine 12) signal dependent mechanism in mice under chronic restrain stress.
Secretion of BNP increases in patients with heart failure, thus promoting natriuresis. BNP is synthesized as a 134-amino acid precursor protein (preproBNP) that is subsequently processed into proBNP, active BNP (1-32), and NT-proBNP (1-76). 49 All of these forms have a proline in the second N-terminal position; therefore, they can be DPP-4 substrates. Low levels of BNP are observed in patients with obesity, insulin resistance, and diabetes, which may contribute to the increased cardiovascular risk in these populations. 50 However, no significant changes in BNP or NT-proBNP levels are observed after treatment with linagliptin or sitagliptin in patients with T2DM or healthy subjects, respectively.51,52 Further studies are needed to evaluate the effects of inhibiting DPP-4 and lowering BNP on subsequent cardiovascular protection.
NPY and PYY are a members of the pancreatic polypeptide family that exert opposing actions on the control of food intake. 53 Inhibition of DPP-4 activity results in changes in receptor affinities of DPP-4-cleaved NPY (3-36) and PYY (3-36) from the Y1 receptor to the Y2 and Y5 receptors.54,55 Although the effects of inhibiting DPP-4 on NPY and PYY have been extensively studied in experimental models, integrated in vivo responses to these peptides after DPP-4 inhibitor therapy are not fully evaluated and further studies are needed.
DPP-4 inhibition and immune system
DPP-4 has been associated with the control of lymphocytes and immune function, cell migration, viral entry, cancer metastasis, and inflammatory reactions. 56 Two mechanisms used by DPP-4/CD26 to exert its effects on the immune system: one is the enzymatic activity of DPP-4, which degrades a targeted substrate into inactive and active fragments with subsequent actions on the immune system; the other is DPP-4/CD26, which acts as a potent co-stimulatory factor of T-cell proliferation and signal transduction. 57
DPP-4 degrades and regulates the activities of many cytokines, such as fibroblast growth factor 2, interleukin-3, GM-CSF, G-CSF, and erythropoietin. These cytokines are truncated by DPP-4, which reduces their activity and function.58-60 Inhibition of DPP-4 activity is associated with changes in tumor growth, enhanced metastasis, and invasive behavior.61,62 The interaction between DPP-4 and adenosine deaminase (ADA) is regulated in a more complex manner by factors/immune cells, rather than direct degradation. The ADA/DPP-4 interaction is a co-stimulatory signal during T-cell receptor signaling, which results in enhanced secretion of interferon-γ and tumor necrosis factor-α. However, the functional importance of the ADA/DPP-4 interaction remains incompletely understood.
DPP-4 inhibition and stroke
DPP-4 inhibitors reduce brain damage and improve functional parameters after stroke in various animal models via several mechanisms including reduction of inflammation, endothelial leakage and excitotoxicity, oxidative stress, and apoptosis and neuronal damage, independent of their control of glucose homeostasis.63-66 Although the effects of DPP-4 inhibitors on the development of cardiovascular disease (including stroke) and death are neutral, 67 the efficacies of DPP-4 inhibitors on functional outcomes after stroke have not been fully studied. 68 The DPP-4 substrate, SDF-1α, is an important factor during neovascular remodeling after stroke in the brain.69-72 Chiazza et al 73 showed that administrating the DPP-4 inhibitor linagliptin specifically increases active SDF-1α (but not GIP or GLP-1) in the brain, and linagliptin improves functional outcomes of stroke in a manner dependent on the SDF-1α/CXCL4 signaling pathway. Further studies are needed determine the mode of action of DPP-4 inhibitors in the brain and the effects of DPP-4 on functional recovery after stroke.
Results of cardiovascular outcome trials (CVOT) and other clinical trials
DPP-4 inhibitors truncate numerous substrates, which are cardioprotective and immunoprotective. Thus, DPP-4 inhibitor treatment may have a favorable effect preventing and recovering cardiovascular damage after ischemic insult through glycemic control and direct regulation of the cardiovascular system. However, large CVOTs of the DPP-4 inhibitors saxagliptin, alogliptin, sitagliptin, and linagliptin have failed to show an association between DPP-4 inhibitor use and reduced risk of major adverse cardiovascular events (MACEs).
The Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus-Thrombolysis in Myocardial Infarction (SAVOR-TIMI 53) study recruited 16,492 patients with T2DM who had a history of or were at risk for cardiovascular events. The study was designed to detect the superiority of saxagliptin over placebo for mean interval of 2.1 years. 74 Although the rate of the composite primary endpoint was not different (73% and 72% of patients taking saxagliptin and placebo, respectively), saxagliptin was associated with a significant increase in the hospitalization rate for heart failure.
The Examination of Cardiovascular Outcomes with Alogliptin versus Standard of Care (EXAMINE) trial included 5,380 patients with T2DM who had experienced recent acute coronary syndrome requiring hospitalization within 15 to 90 days; it compared the effect of alogliptin with placebo. 75 During a median 18-month follow-up period, alogliptin did not increase the MACE rate, suggesting safety and non-inferiority over placebo.
The Trial Evaluation Cardiovascular Outcomes with Sitagliptin (TECOS) study was designed to investigate the superiority of sitagliptin, compared with placebo; it included 14,671 patients with T2DM who had cardiovascular disease. 76 Sitagliptin did not appear to increase the risk of MACE or hospitalization for heart failure during a median follow-up interval of 3.0 years. However, the study only demonstrated the noninferiority of sitagliptin.
No significant difference in the risk of cardiovascular events between a DPP-4 inhibitor and placebo or comparator groups—was observed in a large meta-analysis of 69 trials. 77 Another meta-analysis showed a similar safety profile of DPP-4 inhibitors, compared with placebo, except for weak evidence indicating an increased risk of heart failure. 78
The Cardiovascular and Renal Microvascular Outcome Study with Linagliptin in Patients with Type 2 Diabetes Mellitus (CARMELINA) trial was a randomized, double-blind, placebo-controlled study that compared linagliptin with placebo in patients with T2DM who had high cardiovascular risk or existing chronic kidney disease. 79 This study was the only CVOT designed to demonstrate cardioprotection focused on patients with diabetes who had increased CV risk; however, linagliptin proved only to be non-inferior to placebo.
The Cardiovascular Outcome Study of Linagliptin Versus Glimepiride in Patients with Type 2 Diabetes (CAROLINA) study was designed to evaluate the cardiovascular superiority of the DPP-4 inhibitor linagliptin compared with the sulfonylurea glimepiride.80-82 Although, sulfonylurea was associated with an increased risk for hypoglycemia, no significant difference in cardiovascular outcomes was observed during this head-to-head active comparative study.
No CVOT has been performed for vildagliptin, but the Vildagliptin in Ventricular Dysfunction Diabetes (VIVID) trial was designed to determine the effect of vildagliptin on left ventricular ejection fraction in patients with T2DM who had heart failure. 83 No significant change in left ventricular ejection fraction was observed during 1 year of treatment.
Although the results of pooled analyses and meta-analyses of previous, smaller trials using DPP-4 inhibitors have suggested a reduction in the risk of MACEs with DPP-4 inhibitor treatment, the results of major CVOTs did not reveal increased cardiovascular safety. This discrepancy may be related to differences in study design (CV outcome vs CV safety trials) and patient characteristics (selected for high CV risk, typically older with longer duration of diabetes, greater impairment of renal function, higher comorbidity). 84 In addition, longer duration of CV safety trial increases the risk for missing data and loss of beneficial effect of DPP4 inhibitors.85-87
Protective effects of DPP-4 inhibitors against vascular disease in SIAS
Cellular senescence is classically characterized as irreversible cell cycle arrest. Cells alter gene expression, resulting in the production of proinflammatory, and matrix-degrading molecules known as the senescent-associated secretory phenotype (SASP).88,89 Cells can exhibit SIAS because of DNA damage, oxidative stress, oncogenic insults, and chemotherapeutic-induced toxicity. 90 The potential involvement of cellular senescence in aging and age-related disorders has been supported, such as in cardiovascular diseases.91,92 Senescent vascular endothelial cells accelerate the formation and progression of plaque, and vascular disease development through chronic inflammation and tissue remodeling.93,94 Thus, senolytics (ie, bioactive compounds that selectively target and eliminate senescent cells) are emerging as a new treatment modality for cardiovascular disease.95,96
DPP-4 inhibitors have direct cardiovascular effects, such as the capacity to attenuate vascular inflammation, improve lipid metabolism and endothelial function, and reduce of oxidative stress.8,97-99 We found that inhibition of DPP-4 by anagliptin reduces the SIAS of human vascular endothelial cells (HUVECs) under oxidative or glucolipotoxic stress by reducing endoplasmic reticulum stress, reactive oxygen species generation, and nucleotide-binding oligomerization domain-like receptor protein 3 (NLRP3) inflammasome signal transduction. 100 Treatment of Zucker diabetic fatty rats with vildagliptin reduces reactive oxygen species-induced senescence and DNA damage through the cAMP/protein kinase A (PKA) signaling pathway. 101 In other studies, inhibition of DPP-4 has been shown to prevent vascular aging in mice under chronic psychological stress by modulating oxidative stress and inflammation. 102 Chen et al 10 revealed that the inhibition of DPP-4 improves endothelial senescence by activating the AMP-activated protein kinase/NDA-dependent deacetylase sirtuin-1(SIRT-1)/nuclear factor erythroid-2-related factor 2 (Nrf2) signaling pathway. A study in apo E-deficient mice under chronic stress condition, DPP-4 inhibition attenuated vascular aging mediated by increased GLP-1 and adiponectin. 103 In immobilized mice, DPP-4 inhibition improved FeCl3-induced thrombosis of carotid artery via the improvement of ADAMTS13 and oxidative stress. 104 DPP-4 inhibitor gemigliptin attenuates the proliferation and migration of vascular smooth muscle cells VSMCs via p62–Keap1–Nrf2 pathway in mouse carotid arteries which enhanced neointimal hyperplasia induced by ligation injury. 105 In a study of adenosine-induced chronic kidney disease model mice, DPP-4 inhibitor gemigliptin attenuated vascular calcification and osteogenic trans-differentiation in vascular smooth muscle cells through various mechanisms including downregulation of PiT-1 expression and suppression of reactive oxygen species generation, phospho-PI3K/AKT, and the Wnt signaling pathway. 106 Novel DPP-4 inhibitor, evogliptin attenuates vascular calcification by preventing the insulin-like growth factor-1 (IGF-1) inactivation and potentiating IGF-1 receptor-dependent signaling pathway. 107 In a study of calcific aortic valve disease (CAVD) animal model, evogliptin attenuated valvular calcification and CAVD progression via inhibiting inflammatory cytokine expression, fibrosis, and calcification. 108 Taken together, the findings thus far indicate that DPP-4 inhibitors can be used novel therapeutic target or treatment strategies for stress-related vascular disorders, although further studies are needed for clinical application.
DPP-4 Inhibitors and COVID-19
It is known that underlying diabetes, especially T2DM is recognized as a risk factor for developing the more severe form of coronavirus disease 2019 (COVID-19) and worse disease outcomes, including high mortality.109-111 Recently, it raised the possibility that the DPP-4 is recognized as coronavirus receptor protein to intracellular entry of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), although angiotensin-converting enzyme 2 (ACE2) is recognized as the main receptor.111-113 In a study using human bronchial epithelial cells, there was no blocking effect on the entry of coronavirus into cells with DPP-4 inhibitors sitagliptin, vildagliptin, or saxagliptin. 114
As mentioned above, DPP-4 has not only an important role in glucose homeostasis, but also central role in the immune system as a marker of activated T lymphocytes and regulator of numerous chemokines. Furthermore, DPP-4 inhibitors have anti-inflammatory properties and vascular protective effects though various mechanisms such as reducing oxidative stress and endoplasmic reticulum stress. These finding indicates a possibility of DPP-4 as a potential treatment strategy of SARS-CoV-2 infection. 115 However, there have been no clear-cut conclusions about the role of DPP-4 inhibitors on the clinical outcomes associated with SARS-CoV-2 infection. 116 In a multicenter, retrospective, case-control study in Northern Italy hospitals including 338 patients with COVID-19 underlying T2DM, sitagliptin treatment during hospitalization was associated with reduced mortality and improved clinical outcomes. 117 In another single center, case series involving COVID-19 patients revealed the association between DPP-4 inhibitor and lower risk of mortality. 118 On the other hand, DPP-4 inhibitor treatment was associated with worse outcome in 27 patients with T2DM treated with DPP-4 inhibitors than in 49 treated with other anti-diabetic agents. 119 Thus, prospective randomized clinical trials (RCTs) are necessary, and currently at least 3 parallel-group RCTs investigating the potential survival benefits of DPP-4 inhibitors diverse populations with T2DM and COVID-19.
Conclusions and Future Perspectives
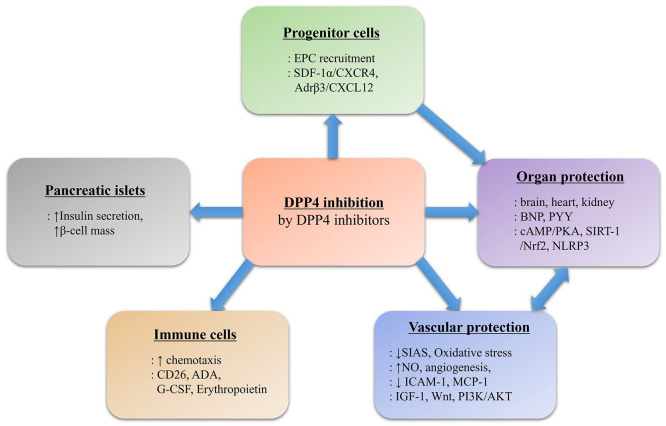
We schematically summarized the endocrine pathways that change during DPP4 inhibition in response to selective DPP4 inhibitors in Figure 1. DPP-4 inhibitors have been widely used to treat T2DM because they have good safety and tolerability profiles with low incidences of adverse events, such as hypoglycemia. However, evidence from recent CVOTs has produced a paradigm shift in the guidelines and recommendations. The published ADA/EASD 2019 Consensus Report Update 98 emphasized the importance of treating patients with T2DM and high risk of atherosclerosis with a GLP-1 receptor agonist or a sodium-glucose cotransporter 2 inhibitor. Nevertheless, DPP-4 inhibitors remain important in diabetes treatment because of their safety and pleiotropic effects unrelated to glycemic control. We wish to further elucidate the mechanisms of the pleiotropic effects of DPP-4 inhibitors and demonstrate whether the actions confirmed in preclinical studies can be reproduced in clinical practice. In particular, additional research is needed regarding the development and utilization of DPP-4 inhibitors as therapeutic target or modality against SIAS.
Figure 1.
Schematic illustration of endocrine pathways and possible molecular mechanism altered during DPP4 inhibition. Selective inhibition of DPP-4 protease activity by DPP-4 inhibitors produce various biological actions in peripheral tissues and target organs.
Abbreviations: ADA, adenosine deaminase; Adrβ3, β3-adrenergic receptor; BNP, brain natriuretic peptide; cAMP, cyclic adenosine monophosphate; CXCL, C-X-C motif ligand; EPC, endothelial progenitor cell; G-CSF, granulocyte colony-stimulating factor; GLP-1, glucagon-like peptide-1; ICAM-1, intercellular adhesion molecule-1; IGF-1, insulin-like growth factor-1; MCP-1, monocyte chemoattractant protein-1; NLRP, nucleotide-binding oligomerization domain, leucine rich repeat and pyrin domain containing proteins; NO, nitric oxidase; Nrf2, nuclear factor erythroid 2-related factor 2; PI3K, phosphoinositide 3-kinase; PKA, protein kinase A; SDF-1α, stromal cell-derived factor 1α, SIRT1, NAD-dependent deacetylase sirtuin-1.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: SM Kang and JH Park wrote and edit this review.
ORCID iD: Seon Mee Kang  https://orcid.org/0000-0002-4056-7525
https://orcid.org/0000-0002-4056-7525
Data Availability Statement: Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1. Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34:1249-1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO multinational study of vascular disease in Diabetes. Diabetologia. 2001;44 Suppl 2:S14-S21. [DOI] [PubMed] [Google Scholar]
- 3. Boer GA, Holst JJ. Incretin hormones and type 2 diabetes-mechanistic insights and therapeutic approaches. Biology. 2020;9:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nathan DM. Finding new treatments for diabetes–how many, how fast . . . How good? N Engl J Med. 2007;356:437-440. [DOI] [PubMed] [Google Scholar]
- 5. Russell S. Incretin-based therapies for type 2 diabetes mellitus: a review of direct comparisons of efficacy, safety and patient satisfaction. Int J Clin Pharm. 2013;35:159-172. [DOI] [PubMed] [Google Scholar]
- 6. Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696-1705. [DOI] [PubMed] [Google Scholar]
- 7. Aroor AR, Sowers JR, Jia G, DeMarco VG. Pleiotropic effects of the dipeptidylpeptidase-4 inhibitors on the cardiovascular system. Am J Physiol Heart Circ Physiol. 2014;307:H477-H492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fadini GP, Avogaro A. Cardiovascular effects of DPP-4 inhibition: beyond GLP-1. Vasc Pharmacol. 2011;55:10-16. [DOI] [PubMed] [Google Scholar]
- 9. Hasegawa Y, Hayashi K, Takemoto Y, et al. DPP-4 inhibition with linagliptin ameliorates the progression of premature aging in klotho-/- mice. Cardiovasc Diabetol. 2017;16:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen Z, Yu J, Fu M, et al. Dipeptidyl peptidase-4 inhibition improves endothelial senescence by activating AMPK/SIRT1/Nrf2 signaling pathway. Biochem Pharmacol. 2020;177:113951. [DOI] [PubMed] [Google Scholar]
- 11. Xin M, Jin X, Cui X, et al. Dipeptidyl peptidase-4 inhibition prevents vascular aging in mice under chronic stress: modulation of oxidative stress and inflammation. Chem Biol Interact. 2019;314:108842. [DOI] [PubMed] [Google Scholar]
- 12. Hopsu-Havu VK, Glenner GG. A new dipeptide naphthylamidase hydrolyzing glycyl-prolyl-beta-naphthylamide. Histochemie. 1966;7:197-201. [DOI] [PubMed] [Google Scholar]
- 13. McCaughan GW, Wickson JE, Creswick PF, Gorrell MD. Identification of the bile canalicular cell surface molecule GP110 as the ectopeptidase dipeptidyl peptidase IV: an analysis by tissue distribution, purification and N-terminal amino acid sequence. Hepatology. 1990;11:534-544. [DOI] [PubMed] [Google Scholar]
- 14. Ulmer AJ, Mattern T, Feller AC, Heymann E, Flad HD. CD26 antigen is a surface dipeptidyl peptidase IV (DPPIV) as characterized by monoclonal antibodies clone TII-19-4-7 and 4EL1C7. Scand J Immunol. 1990;31:429-435. [DOI] [PubMed] [Google Scholar]
- 15. Vivier I, Marguet D, Naquet P, et al. Evidence that thymocyte-activating molecule is mouse CD26 (dipeptidyl peptidase IV). J Immunol. 1991;147:447-454. [PubMed] [Google Scholar]
- 16. Drucker DJ. Dipeptidyl peptidase-4 inhibition and the treatment of type 2 diabetes: preclinical biology and mechanisms of action. Diabetes Care. 2007;30:1335-1343. [DOI] [PubMed] [Google Scholar]
- 17. Kirby M, Yu DM, O’Connor S, Gorrell MD. Inhibitor selectivity in the clinical application of dipeptidyl peptidase-4 inhibition. Clin Sci. 2009;118:31-41. [DOI] [PubMed] [Google Scholar]
- 18. Lambeir AM, Durinx C, Scharpé S, De Meester I. Dipeptidyl-peptidase IV from bench to bedside: an update on structural properties, functions, and clinical aspects of the enzyme DPP IV. Crit Rev Clin Lab Sci. 2003;40:209-294. [DOI] [PubMed] [Google Scholar]
- 19. Gorrell MD, Gysbers V, McCaughan GW. CD26: a multifunctional integral membrane and secreted protein of activated lymphocytes. Scand J Immunol. 2001;54:249-264. [DOI] [PubMed] [Google Scholar]
- 20. Deacon CF, Johnsen AH, Holst JJ. Degradation of glucagon-like peptide-1 by human plasma in vitro yields an N-terminally truncated peptide that is a major endogenous metabolite in vivo. J Clin Endocrinol Metab. 1995;80:952-957. [DOI] [PubMed] [Google Scholar]
- 21. Deacon CF. Circulation and degradation of GIP and GLP-1. Horm Metab Res. 2004;36:761-765. [DOI] [PubMed] [Google Scholar]
- 22. Campbell JE, Drucker DJ. Pharmacology, physiology, and mechanisms of incretin hormone action. Cell Metab. 2013;17:819-837. [DOI] [PubMed] [Google Scholar]
- 23. Nikolaidis LA, Elahi D, Shen YT, Shannon RP. Active metabolite of GLP-1 mediates myocardial glucose uptake and improves left ventricular performance in conscious dogs with dilated cardiomyopathy. Am J Physiol Heart Circ Physiol. 2005;289:H2401-H2408. [DOI] [PubMed] [Google Scholar]
- 24. Ban K, Noyan-Ashraf MH, Hoefer J, Bolz SS, Drucker DJ, Husain M. Cardioprotective and vasodilatory actions of glucagon-like peptide 1 receptor are mediated through both glucagon-like peptide 1 receptor-dependent and -independent pathways. Circulation. 2008;117:2340-2350. [DOI] [PubMed] [Google Scholar]
- 25. Tomas E, Wood JA, Stanojevic V, Habener JF. Glucagon-like peptide-1(9-36)amide metabolite inhibits weight gain and attenuates diabetes and hepatic steatosis in diet-induced obese mice. Diabetes Obes Metab. 2011;13:26-33. [DOI] [PubMed] [Google Scholar]
- 26. Marguet D, Baggio L, Kobayashi T, et al. Enhanced insulin secretion and improved glucose tolerance in mice lacking CD26. Proc Natl Acad Sci USA. 2000;97:6874-6879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Karagiannis T, Paschos P, Paletas K, Matthews DR, Tsapas A. Dipeptidyl peptidase-4 inhibitors for treatment of type 2 diabetes mellitus in the clinical setting: systematic review and meta-analysis. BMJ. 2012;344:e1369. [DOI] [PubMed] [Google Scholar]
- 28. Fadini GP, Albiero M, Menegazzo L, de Kreutzenberg SV, Avogaro A. The increased dipeptidyl peptidase-4 activity is not counteracted by optimized glucose control in type 2 diabetes, but is lower in metformin-treated patients. Diabetes Obes Metab. 2012;14:518-522. [DOI] [PubMed] [Google Scholar]
- 29. Patel BD, Ghate MD. Recent approaches to medicinal chemistry and therapeutic potential of dipeptidyl peptidase-4 (DPP-4) inhibitors. Eur J Med Chem. 2014;74:574-605. [DOI] [PubMed] [Google Scholar]
- 30. Kim SH, Yoo JH, Lee WJ, Park CY. Gemigliptin: an update of its clinical use in the management of type 2 Diabetes mellitus. Diabetes Metab J. 2016;40:339-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mulvihill EE, Drucker DJ. Pharmacology, physiology, and mechanisms of action of dipeptidyl peptidase-4 inhibitors. Endocr Rev. 2014;35:992-1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nagasawa T. A chemokine, SDF-1/PBSF, and its receptor, CXC chemokine receptor 4, as mediators of hematopoiesis. Int J Hematol. 2000;72:408-411. [PubMed] [Google Scholar]
- 33. Iwata S, Yamaguchi N, Munakata Y, et al. CD26/dipeptidyl peptidase IV differentially regulates the chemotaxis of T cells and monocytes toward RANTES: possible mechanism for the switch from innate to acquired immune response. Int Immunol. 1999;11:417-426. [DOI] [PubMed] [Google Scholar]
- 34. Matheeussen V, Waumans Y, Martinet W, et al. Dipeptidyl peptidases in atherosclerosis: expression and role in macrophage differentiation, activation and apoptosis. Basic Res Cardiol. 2013;108:350. [DOI] [PubMed] [Google Scholar]
- 35. Christopherson Kw, 2nd, Hangoc G, Broxmeyer HE. Cell surface peptidase CD26/dipeptidylpeptidase IV regulates CXCL12/stromal cell-derived factor-1 alpha-mediated chemotaxis of human cord blood CD34+ progenitor cells. J Immunol. 2002;169:7000-7008. [DOI] [PubMed] [Google Scholar]
- 36. Shioda T, Kato H, Ohnishi Y, et al. Anti-HIV-1 and chemotactic activities of human stromal cell-derived factor 1alpha (SDF-1alpha) and SDF-1beta are abolished by CD26/dipeptidyl peptidase IV-mediated cleavage. Proc Natl Acad Sci USA. 1998;95:6331-6336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zaruba MM, Theiss HD, Vallaster M, et al. Synergy between CD26/DPP-IV inhibition and G-CSF improves cardiac function after acute myocardial infarction. Cell Stem Cell. 2009;4:313-323. [DOI] [PubMed] [Google Scholar]
- 38. Lataillade JJ, Domenech J, Le Bousse-Kerdiles MC. Stromal cell-derived factor-1 (SDF-1)\CXCR4 couple plays multiple roles on haematopoietic progenitors at the border between the old cytokine and new chemokine worlds: survival, cell cycling and trafficking. Eur Cytokine Netw. 2004;15:177-188. [PubMed] [Google Scholar]
- 39. De La Luz Sierra M, Gasperini P, McCormick PJ, Zhu J, Tosato G. Transcription factor Gfi-1 induced by G-CSF is a negative regulator of CXCR4 in myeloid cells. Blood. 2007;110:2276-2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Broxmeyer HE, Hangoc G, Cooper S, Campbell T, Ito S, Mantel C. AMD3100 and CD26 modulate mobilization, engraftment, and survival of hematopoietic stem and progenitor cells mediated by the SDF-1/CXCL12-CXCR4 axis. Ann N Y Acad Sci. 2007;1106:1-19. [DOI] [PubMed] [Google Scholar]
- 41. Theiss HD, Brenner C, Engelmann MG, et al. Safety and efficacy of SITAgliptin plus GRanulocyte-colony-stimulating factor in patients suffering from acute myocardial infarction (SITAGRAMI-Trial)–rationale, design and first interim analysis. Int J Cardiol. 2010;145:282-284. [DOI] [PubMed] [Google Scholar]
- 42. Theiss HD, Vallaster M, Rischpler C, et al. Dual stem cell therapy after myocardial infarction acts specifically by enhanced homing via the SDF-1/CXCR4 axis. Stem Cell Res. 2011;7:244-255. [DOI] [PubMed] [Google Scholar]
- 43. Marfella R, Sasso FC, Rizzo MR, et al. Dipeptidyl peptidase 4 inhibition may facilitate healing of chronic foot ulcers in patients with type 2 diabetes. Exp Diabetes Res. 2012;2012:892706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Long M, Cai L, Li W, et al. DPP-4 inhibitors improve diabetic wound healing via direct and indirect promotion of epithelial-mesenchymal transition and reduction of scarring. Diabetes. 2018;67:518-531. [DOI] [PubMed] [Google Scholar]
- 45. Takabatake Y, Sugiyama T, Kohara H, et al. The CXCL12 (SDF-1)/CXCR4 axis is essential for the development of renal vasculature. J Am Soc Nephrol. 2009;20:1714-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lotan D, Sheinberg N, Kopolovic J, Dekel B. Expression of SDF-1/CXCR4 in injured human kidneys. Pediatr Nephrol. 2008;23:71-77. [DOI] [PubMed] [Google Scholar]
- 47. Tögel F, Isaac J, Hu Z, Weiss K, Westenfelder C. Renal SDF-1 signals mobilization and homing of CXCR4-positive cells to the kidney after ischemic injury. Kidney Int. 2005;67:1772-1784. [DOI] [PubMed] [Google Scholar]
- 48. Zhu E, Hu L, Wu H, et al. Dipeptidyl Peptidase-4 regulates hematopoietic stem cell activation in response to chronic stress. J Am Heart Assoc. 2017;6:e006394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mahadavan G, Nguyen TH, Horowitz JD. Brain natriuretic peptide: a biomarker for all cardiac disease? Curr Opin Cardiol. 2014;29:160-166. [DOI] [PubMed] [Google Scholar]
- 50. Beleigoli A, Diniz M, Nunes M, et al. Reduced brain natriuretic peptide levels in class III obesity: the role of metabolic and cardiovascular factors. Obes Facts. 2011;4:427-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Fadini GP, Bonora BM, Albiero M, Zaninotto M, Plebani M, Avogaro A. DPP-4 inhibition has no acute effect on BNP and its N-terminal pro-hormone measured by commercial immune-assays. A randomized cross-over trial in patients with type 2 diabetes. Cardiovasc Diabetol. 2017;16:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Devin JK, Pretorius M, Nian H, Yu C, Billings Ft, 4TH, Brown NJ. Dipeptidyl-peptidase 4 inhibition and the vascular effects of glucagon-like peptide-1 and brain natriuretic peptide in the human forearm. J Am Heart Assoc. 2014;3:e001075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Medeiros MD, Turner AJ. Processing and metabolism of peptide-YY: pivotal roles of dipeptidylpeptidase-IV, Aminopeptidase-P, and endopeptidase-24.11. Endocrinology. 1994;134:2088-2094. [DOI] [PubMed] [Google Scholar]
- 54. Mentlein R. Dipeptidyl-peptidase IV (CD26)–role in the inactivation of regulatory peptides. Regul Pept. 1999;85:9-24. [DOI] [PubMed] [Google Scholar]
- 55. Pedragosa-Badia X, Stichel J, Beck-Sickinger AG. Neuropeptide Y receptors: how to get subtype selectivity. Front Endocrinol. 2013;4:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Aytac U, Dang NH. CD26 / Dipeptidyl peptidase IV: a regulator of immune function and a potential molecular target for therapy. Curr Drug Targets Immune Endocr Metabol Disord. 2004;4:11-18. [DOI] [PubMed] [Google Scholar]
- 57. Ohnuma K, Dang NH, Morimoto C. Revisiting an old acquaintance: CD26 and its molecular mechanisms in T cell function. Trends Immunol. 2008;29:295-301. [DOI] [PubMed] [Google Scholar]
- 58. Broxmeyer HE, Hoggatt J, O’Leary HA, et al. Dipeptidylpeptidase 4 negatively regulates colony-stimulating factor activity and stress hematopoiesis. Nat Med. 2012;18:1786-1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. O’Leary HA, Capitano M, Cooper S, et al. DPP4 truncated GM-CSF and IL-3 manifest distinct receptor-binding and regulatory functions compared with their full-length forms. Leukemia. 2017;31:2468-2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wesley UV, McGroarty M, Homoyouni A. Dipeptidyl peptidase inhibits malignant phenotype of prostate cancer cells by blocking basic fibroblast growth factor signaling pathway. Cancer Res. 2005;65:1325-1334. [DOI] [PubMed] [Google Scholar]
- 61. Wilson-Ford V. Health-protective behaviors of rural black elderly women. Health Soc Work. 1992;17:28-36. [DOI] [PubMed] [Google Scholar]
- 62. Kajiyama H, Kikkawa F, Khin E, Shibata K, Ino K, Mizutani S. Dipeptidyl peptidase IV overexpression induces up-regulation of E-cadherin and tissue inhibitors of matrix metalloproteinases, resulting in decreased invasive potential in ovarian carcinoma cells. Cancer Res. 2003;63:2278-2283. [PubMed] [Google Scholar]
- 63. Darsalia V, Klein T, Nyström T, Patrone C. Glucagon-like receptor 1 agonists and DPP-4 inhibitors: anti-diabetic drugs with anti-stroke potential. Neuropharmacol. 2018;136:280-286. [DOI] [PubMed] [Google Scholar]
- 64. Darsalia V, Larsson M, Nathanson D, Klein T, Nyström T, Patrone C. Glucagon-like receptor 1 agonists and DPP-4 inhibitors: potential therapies for the treatment of stroke. J Cereb Blood Flow Metab. 2015;35:718-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Marlet IR, Ölmestig JNE, Vilsbøll T, Rungby J, Kruuse C. Neuroprotective mechanisms of glucagon-like peptide-1-based therapies in Ischaemic stroke: a systematic review based on pre-clinical studies. Basic Clin Pharmacol Toxicol. 2018;122:559-569. [DOI] [PubMed] [Google Scholar]
- 66. Ma M, Hasegawa Y, Koibuchi N, et al. DPP-4 inhibition with linagliptin ameliorates cognitive impairment and brain atrophy induced by transient cerebral ischemia in type 2 diabetic mice. Cardiovasc Diabetol. 2015;14:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Nauck MA, Meier JJ, Cavender MA, Abd El, Aziz M, Drucker DJ. Cardiovascular actions and clinical outcomes with Glucagon-Like Peptide-1 receptor agonists and Dipeptidyl peptidase-4 inhibitors. Circulation. 2017;136:849-870. [DOI] [PubMed] [Google Scholar]
- 68. Darsalia V, Larsson M, Klein T, Patrone C. The high need for trials assessing functional outcome after stroke rather than stroke prevention with GLP-1 agonists and DPP-4 inhibitors. Cardiovasc Diabetol. 2018;17:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Li Y, Huang J, He X, et al. Postacute stromal cell-derived factor-1α expression promotes neurovascular recovery in ischemic mice. Stroke. 2014;45:1822-1829. [DOI] [PubMed] [Google Scholar]
- 70. Robin AM, Zhang ZG, Wang L, et al. Stromal cell-derived factor 1alpha mediates neural progenitor cell motility after focal cerebral ischemia. J Cereb?Blood?Flow?Metab. 2006;26:125-134. [DOI] [PubMed] [Google Scholar]
- 71. Walter HL, van der Maten G, Antunes AR, Wieloch T, Ruscher K. Treatment with AMD3100 attenuates the microglial response and improves outcome after experimental stroke. J Neuroinflammation. 2015;12:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Huang J, Li Y, Tang Y, Tang G, Yang GY, Wang Y. CXCR4 antagonist AMD3100 protects blood–brain barrier integrity and reduces inflammatory response after focal ischemia in mice. Stroke. 2013;44:190-197. [DOI] [PubMed] [Google Scholar]
- 73. Chiazza F, Tammen H, Pintana H, et al. The effect of DPP-4 inhibition to improve functional outcome after stroke is mediated by the SDF-1α/CXCR4 pathway. Cardiovasc Diabetol. 2018;17:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317-1326. [DOI] [PubMed] [Google Scholar]
- 75. White WB, Cannon CP, Heller SR, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013;369:1327-1335. [DOI] [PubMed] [Google Scholar]
- 76. Green JB, Bethel MA, Armstrong PW, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 Diabetes. N Engl J Med. 2015;373:232-242. [DOI] [PubMed] [Google Scholar]
- 77. Kaneko M, Narukawa M. Meta-analysis of dipeptidyl peptidase-4 inhibitors use and cardiovascular risk in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2016;116:171-182. [DOI] [PubMed] [Google Scholar]
- 78. Elgendy IY, Mahmoud AN, Barakat AF, et al. Cardiovascular safety of Dipeptidyl-Peptidase IV inhibitors: a meta-analysis of placebo-controlled randomized trials. Am J Cardiovasc Drugs. 2017;17:143-155. [DOI] [PubMed] [Google Scholar]
- 79. Rosenstock J, Perkovic V, Johansen OE, et al. Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 Diabetes and high cardiovascular and renal risk: the CARMELINA randomized clinical trial. JAMA. 2019;321:69-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Rosenstock J, Marx N, Kahn SE, et al. Cardiovascular outcome trials in type 2 diabetes and the sulphonylurea controversy: rationale for the active-comparator CAROLINA trial. Diabetes Vasc Dis Res. 2013;10:289-301. [DOI] [PubMed] [Google Scholar]
- 81. Marx N, Rosenstock J, Kahn SE, et al. Design and baseline characteristics of the CARdiovascular outcome trial of LINAgliptin versus glimepiride in type 2 Diabetes (CAROLINA®). Diabetes Vasc Dis Res. 2015;12:164-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Abdelmoneim AS, Eurich DT, Light PE, et al. Cardiovascular safety of sulphonylureas: over 40 years of continuous controversy without an answer. Diabetes Obes Metab. 2015;17:523-532. [DOI] [PubMed] [Google Scholar]
- 83. McMurray JJV, Ponikowski P, Bolli GB, et al. Effects of vildagliptin on ventricular function in patients with type 2 Diabetes mellitus and heart failure: a randomized placebo-controlled trial. JACC Heart Fail. 2018;6:8-17. [DOI] [PubMed] [Google Scholar]
- 84. Mannucci E, Mosenzon O, Avogaro A. Analyses of results from cardiovascular safety trials with DPP-4 inhibitors: cardiovascular outcomes, predefined safety outcomes, and pooled analysis and meta-analysis. Diabetes Care. 2016;39 Suppl 2:S196-S204. [DOI] [PubMed] [Google Scholar]
- 85. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 Diabetes. N Engl J Med. 2015;373:2117-2128. [DOI] [PubMed] [Google Scholar]
- 86. Savarese G, Perrone-Filardi P, D’Amore C, et al. Cardiovascular effects of dipeptidyl peptidase-4 inhibitors in diabetic patients: a meta-analysis. Int J Cardiol. 2015;181:239-244. [DOI] [PubMed] [Google Scholar]
- 87. Dicembrini I, Mannucci E. Risk of myocardial infarction in trials with Dipeptidyl peptidase-4 inhibitors: Is duration of study a real issue? Int J Cardiol. 2015;184:543-544. [DOI] [PubMed] [Google Scholar]
- 88. Passos JF, Simillion C, Hallinan J, Wipat A, von Zglinicki T. Cellular senescence: unravelling complexity. Age. 2009;31:353-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Campisi J. Aging, cellular senescence, and cancer. Annu Rev Physiol. 2013;75:685-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Childs BG, Durik M, Baker DJ, van Deursen JM. Cellular senescence in aging and age-related disease: from mechanisms to therapy. Nat Med. 2015;21:1424-1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Minamino T, Miyauchi H, Yoshida T, Ishida Y, Yoshida H, Komuro I. Endothelial cell senescence in human atherosclerosis: role of telomere in endothelial dysfunction. Circulation. 2002;105:1541-1544. [DOI] [PubMed] [Google Scholar]
- 92. Garrido AM, Bennett M. Assessment and consequences of cell senescence in atherosclerosis. Curr Opin Lipidol. 2016;27:431-438. [DOI] [PubMed] [Google Scholar]
- 93. Shimizu I, Minamino T. Cellular senescence in cardiac diseases. J Cardiol. 2019;74:313-319. [DOI] [PubMed] [Google Scholar]
- 94. Katsuumi G, Shimizu I, Yoshida Y, Minamino T. Vascular senescence in cardiovascular and metabolic diseases. Front Cardiovasc Med. 2018;5:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Dookun E, Passos JF, Arthur HM, Richardson GD. Therapeutic potential of senolytics in cardiovascular disease. Cardiovasc Drugs Ther. 2020;2020. doi: 10.1007/s10557-020-07075-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Kang C. Senolytics and senostatics: a two-pronged approach to target cellular senescence for delaying aging and age-related diseases. Mol Cells. 2019;42:821-827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Zhong J, Rao X, Rajagopalan S. An emerging role of dipeptidyl peptidase 4 (DPP4) beyond glucose control: potential implications in cardiovascular disease. Atherosclerosis. 2013;226:305-314. [DOI] [PubMed] [Google Scholar]
- 98. Solini A, Rossi C, Duranti E, Taddei S, Natali A, Virdis A. Saxagliptin prevents vascular remodeling and oxidative stress in db/db mice. Role of endothelial nitric oxide synthase uncoupling and cyclooxygenase. Vasc Pharmacol. 2016;76:62-71. [DOI] [PubMed] [Google Scholar]
- 99. Wiciński M, Górski K, Wódkiewicz E, Walczak M, Nowaczewska M, Malinowski B. Vasculoprotective effects of Vildagliptin. Focus on atherogenesis. Int J Mol Sci. 2020;21:2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kang SM, Jung HS, Kwon MJ, Lee SH, Park JH. Effects of anagliptin on the stress induced accelerated senescence of human umbilical vein endothelial cells. Ann Transl Med. 2021;9:750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Oeseburg H, de Boer RA, Buikema H, van der Harst P, van Gilst WH, Silljé HH. Glucagon-like peptide 1 prevents reactive oxygen species-induced endothelial cell senescence through the activation of protein kinase a. Arterioscler Thromb Vasc Biol. 2010;30:1407-1414. [DOI] [PubMed] [Google Scholar]
- 102. Piao L, Zhao G, Zhu E, et al. Chronic psychological stress accelerates vascular senescence and impairs ischemia-induced neovascularization: the role of Dipeptidyl Peptidase-4/Glucagon-Like Peptide-1-Adiponectin Axis. J Am Heart Assoc. 2017;6:2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Lei Y, Yang G, Hu L, et al. Increased dipeptidyl peptidase-4 accelerates diet-related vascular aging and atherosclerosis in ApoE-deficient mice under chronic stress. Int J Cardiol. 2017;243:413-420. [DOI] [PubMed] [Google Scholar]
- 104. Jin X, Jin C, Nakamura K, et al. Increased dipeptidyl peptidase-4 accelerates chronic stress-related thrombosis in a mouse carotid artery model. J Hypertens. 2020;38:1504-1513. [DOI] [PubMed] [Google Scholar]
- 105. Choi SH, Park S, Oh CJ, Leem J, Park KG, Lee IK. Dipeptidyl peptidase-4 inhibition by gemigliptin prevents abnormal vascular remodeling via NF-E2-related factor 2 activation. Vasc Pharmacol. 2015;73:11-19. [DOI] [PubMed] [Google Scholar]
- 106. Choi SY, Ryu HM, Oh EJ, et al. Dipeptidyl peptidase-4 inhibitor gemigliptin protects against vascular calcification in an experimental chronic kidney disease and vascular smooth muscle cells. PLoS One. 2017;12:e0180393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Varennes O, Mary A, Bricca G, Kamel S, Bellien J. Dipeptidyl peptidase-4 inhibition prevents vascular calcification by potentiating the Insulin-Like growth factor-1 signaling pathway. JACC Basic Transl Sci. 2019;4:113-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Choi B, Kim EY, Kim JE, et al. Evogliptin suppresses calcific aortic valve disease by attenuating inflammation, fibrosis, and calcification. Cells. 2021;10:2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17:11-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8:782-792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Targher G, Mantovani A, Wang XB, et al. Patients with diabetes are at higher risk for severe illness from COVID-19. Diabetes Metab. 2020;46:335-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Li Y, Zhang Z, Yang L, et al. The MERS-CoV receptor DPP4 as a candidate binding target of the SARS-CoV-2 spike. iScience. 2020;23:101400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Pal R, Bhadada SK. Reply to comment on "Should anti-diabetic medications be reconsidered amid COVID-19 pandemic?". Diabetes Res Clin Pract. 2020;164:108192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Raj VS, Mou H, Smits SL, et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013;495:251-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Raj VS, Smits SL, Provacia LB, et al. Adenosine deaminase acts as a natural antagonist for dipeptidyl peptidase 4-mediated entry of the Middle East respiratory syndrome coronavirus. J Virol. 2014;88:1834-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Iacobellis G. COVID-19 and diabetes: Can DPP4 inhibition play a role? Diabetes Res Clin Pract. 2020;162:108125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Solerte SB, D’Addio F, Trevisan R, et al. Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 Diabetes and COVID-19: a multicenter, case-control, retrospective, observational study. Diabetes Care. 2020;43:2999-3006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Mirani M, Favacchio G, Carrone F, et al. Impact of comorbidities and glycemia at admission and Dipeptidyl peptidase 4 inhibitors in patients with type 2 Diabetes with COVID-19: a case series from an academic hospital in Lombardy, Italy. Diabetes Care. 2020;43:3042-3049. [DOI] [PubMed] [Google Scholar]
- 119. Dalan R, Ang LW, Tan WYT, et al. The association of hypertension and diabetes pharmacotherapy with COVID-19 severity and immune signatures: an observational study. Eur Heart J Cardiovasc Pharmacother. 2021;7:e48-e51. [DOI] [PMC free article] [PubMed] [Google Scholar]