Abstract
Introduction: Although intravascular laser irradiation of blood (ILIB) is deemed an innocuous and useful technique for laser therapy, particularly when systemic effects are required, no study, to our knowledge, has been conducted on the effectiveness and innocuousness of ILIB in treating acute kidney injury (AKI).
Objective: This study aimed to assess the feasibility and outcomes of ILIB in the management of patients with AKI and comparing them with the Sham-laser group.
Materials and Methods: Twenty-six patients with intra-renal AKI (24-95 years old) at Tajrish Hospitals were evaluated for enrollment eligibility in this clinical trial study. This study was conducted at the nephrology department of Shahid Beheshti University of Medical Science, Tehran, Iran, between 2018 and 2019. Based on the treatment method, the patients’ assignment to two groups (ILIB or Sham-laser) was randomly done. Demographic characteristics, need for dialysis, hemoglobin and serum biochemistry changes, serum and urine neutrophil gelatinase-associated lipocalin (NGAL) changes, laser complications, and the hospitalization period were recorded.
Results: In terms of the baseline characteristics and biochemistry serum level, no differences were seen between the two groups. All post-treatment parameters, except the hemoglobin value, significantly improved in both groups. Urine NGAL and serum NGAL show declines from the baseline in both groups; however, the reduction slope of these parameters occurred faster in the laser group in a statistically significant manner.
Conclusion: A decline in NGAL levels in the laser group during the treatment may suggest that the ILIB can help patients with AKI recover better.
Keywords: Acute kidney injury, Acute renal failure, Biomarker, Neutrophil gelatinase-associated lipocalin, Laser
Introduction
Acute kidney injury (AKI), which used to be referred to as acute renal failure, remains a destructive problem in critically ill adults.1,2 Lack of a standard, consensus definition has led to considerable variations in the reported frequency of AKI among these patients.3 For example, 5% to 50% of them in the reported series are afflicted with AKI.4
In current clinical practice, the measurement of serum creatinine is usually performed to diagnose AKI.5 However, creatinine is deemed a poor indicator of early changes in kidney function.6 Since serum creatinine is considered an insufficient and late indicator of AKI, neutrophil gelatinase-associated lipocalin (NGAL) might appear as a troponin-like early marker for AKI before long.7 Subsequent clinical studies have revealed that urine NGAL is an early predictor for AKI.7-9 Currently, there is a lack of effective treatments for the prevention of AKI, and management is mainly associated with reversing the underlying cause.
Used for pain relief, wound healing and inflammation control, low-level laser therapy (LLLT) has been advocated since the 1960s.10Intravascular laser irradiation of blood (ILIB) is considered an innocuous and useful technique for laser therapy, particularly when systemic effects are essential.11 ILIB with red, UV, and blue light has extensively been employed to treat different pathologies.12 A catheter in a vein (usually in the forearm) can be used to administer blood irradiation therapy which produces immunocorrective, antibacterial, anti-inflammatory, and vasodilative effects and improves bio-stimulation, the rheological properties of blood, and microcirculation.13
To our knowledge, no study has been conducted on the effectiveness and safety of ILIB in the treatment of AKI. In this clinical trial study, the feasibility and outcomes of ILIB in the management of the patients with AKI were investigated and compared with the Sham-laser group.
Materials and Methods
Study Population
In this clinical trial study, twenty-six patients with intra-renal AKI (age 24-95 years old) at Tajrish Hospital were examined for enrollment eligibility. The present study was conducted at the nephrology department of Shahid Beheshti University of Medical Science, Tehran, Iran, between 2018 and 2019. Informed written consent was given by all patients. On the basis of the creatinine and urine output criteria of the RIFLE (Risk, Injury, Failure, Loss, and End-stage renal disease) classification, AKI was defined.14 Four patients were not included in this study due to their active infection, hepatitis B and C, multi-organ transplant, treatment with immunosuppressive agents, glomeronephritis, pregnancy, and refusal to provide fully informed consent.
The remaining 20 patients underwent such standard medical evaluations as history taking, clinical examination, urine analysis, and routine blood chemistry.
Study Design
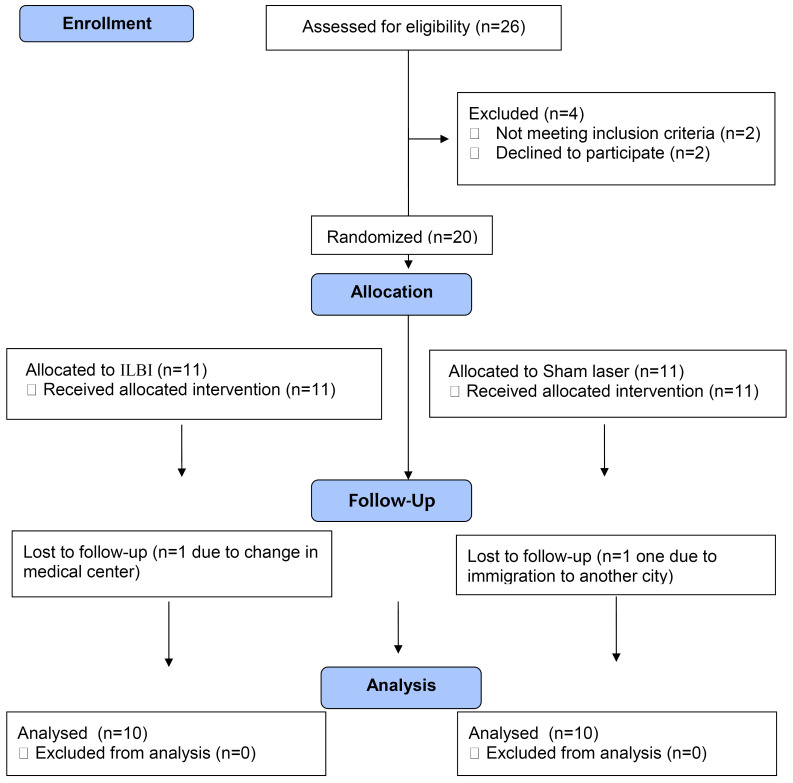
On the basis of the treatment method, the patients were assigned to two groups at random: ILIB or Sham-laser. The sample size was measured according to an unpublished pilot study of ours concerning the changes in serum and urine NGAL after ILIB. Considering a type 1 statistical error < 5%, a type 2 statistical error < 20%, and a dropout rate of 10%, a sample size of 11 patients in each group was calculated. During the study, one participant of each group dropped out due to changing the medical center or missing the follow-up. The data from 10 patients in each of the groups (a total of 20 patients), who completed the study, were amassed for the final analysis. The study design and the follow-up are summarized in Figure 1.
Figure 1.
Flow Diagram of the Study. ILIB = Intravascular laser irradiation of blood.
Procedures
All patients received standard treatment for AKI including hydration during hospitalization. The subject, clinician, and investigator examining the cases were blinded as to which treatment group was the sham. Following the previous study,13 ILIB was utilized intravenously (the laser fiber was placed in the vein by means of a catheter) with a 1.5 mW, continuous, 405-nm laser therapy device (Azor, Russia) via the venue catheter for 30 minutes in the large veins of the upper limb. This protocol was planned based on preceding research studies.13 The treatments were scheduled for 3 sessions every other day (day 1, 3, 5). In the Sham group, the treatments were also administered on days 1, 3, and 5 by the sham probe. For blinding, two probes, namely A and B, were given to the researchers. The probes preset to either active or inactive resembled each other in appearance. While the inactive probe was prepared by an independent operator from the LAMSRC, the company which provided the laser equipment arranged the active probe. The active probe did not produce any light emission, vibrate, get hot, or give off a sound or any other indication pointing to a difference from the inactive probe.
Outcome Assessment
During hospital admission, the patients received regular daily visits. During each visit, a physical examination, measurement of blood pressure, and laboratory calculation of hematological (hemoglobin and pH) and biochemical parameters (serum creatinine, blood urea nitrogen, sodium, potassium, and phosphate) were made.
Serial blood and urine sampling were done for NGAL assessment as follows: the first sample was taken within 12 hours of admission to the nephrology department and before laser intervention, and the second and third samples were obtained after the laser intervention 72 hours and 120 hours after the first sample. Both later samples were taken after laser intervention. Three to 4 mL of blood as well as urine were drawn each time in the ethylenediaminetetraacetic-acid (EDTA) vacutainer. Centrifuged at 3000 rpm for 15 minutes, all samples were aliquoted and stored at − 80°C up to the analysis. Fluorescence immunoassay was employed to analyze the NGAL on Triage® Meter Proby Alere Diagnostics point of care analyzer (CA, USA).
Demographic characteristics, the need for dialysis, changes in hemoglobin and serum biochemistry, changes in serum and urine NGAL, laser complications, and the hospitalization period were recorded. Changes in serum and urine NGAL were used as the primary study endpoint.
The Student’s t test and the chi-square test were run to analyze the collected data, using SPSS software (Statistical Package for the Social Sciences, V. 21.0; SPSS Inc, Chicago, IL, USA). A P value < 0.05 was deemed statistically significant.
Results
The mean ± SD of the patients’ age was 65.2±22.9 years in the ILIB group and 64.8±19.7 years in the sham group respectively. The ratio of males to females was 3 to 1 and the need for dialysis was 20% in both groups. The causes of intrarenal injury were mainly related to infection and sepsis as well as renal toxins (drug, contrast, rhabdomyolysis).
Table 1 shows the baseline characteristics and meticulous peri-procedure variables which include the need for dialysis, urinary output, and change in the hemoglobin and serum level of sodium, potassium, phosphor, pH and creatinine. In terms of the baseline characteristics and the biochemistry serum level, there were not any differences between the two groups. All post-treatment parameters, except the hemoglobin value, significantly improved in both groups.
Table 1. Baseline Characteristics; Pretreatment and Posttreatment Outcomes as well as Complications of Patients of Both Groups.
| ILIB | Sham Laser | P Value | |
| Patients, No. | 10 | 10 | |
| Mean age, year ± SD | 65.2±22.9 | 64.8±19.7 | 0.9 |
| Male to female ratio (%) | 70 | 70 | NS |
| Need for dialysis (%) | 2 (20) | 2 (20) | NS |
| Mean serum sodium, mmol/L ± SD | |||
| Pretreatment | 142.2±4.8 | 140.1±4.7 | 0.3 |
| Posttreatment | 134.7±1.6 | 134.9±1.7 | 0.7 |
| P value | 0. 003* | 0.013* | - |
| Mean serum potassium, mmol/L ± SD | |||
| Pretreatment | 5.5±0.7 | 6.3±1.01 | 0.5 |
| Posttreatment | 4.0±0.1 | 4.03±0.3 | 0.8 |
| P value | 0. 0001* | 0.0001* | - |
| Mean serum phosphor, mmol/L ± SD | |||
| Pretreatment | 6.4±1.1 | 6.3±1.01 | 0.8 |
| Posttreatment | 2.9±0.7 | 3.0±0.7 | 0.7 |
| P value | 0. 0001* | 0.0001* | - |
| Mean serum BUN, mmol/L ± SD | |||
| Pretreatment | 92.7±38.4 | 83.6±29.7 | 0.5 |
| Posttreatment | 26.6±8.1 | 29.2±7.6 | 0.5 |
| P value | 0. 0001* | 0.0001* | - |
| Mean serum creatinine, mmol/L ± SD | |||
| Pretreatment | 6.8±2.2 | 6.7±1.9 | 0.9 |
| Posttreatment | 1.9±0.7 | 1.7±0.5 | 0.4 |
| P value | 0.0001* | 0.0001* | - |
| Mean hemoglobin, g/L ± SD | |||
| Preoperative | 12.6±1.6 | 12.6±1.9 | 0.9 |
| Postoperative | 12.6±1.3 | 12.6±1.6 | 0.8 |
| P value | 0.3 | 0.8 | - |
| Mean serum pH, ± SD | |||
| Pretreatment | 7.12±0.15 | 7.11±0.15 | 0.9 |
| Posttreatment | 7.34±0.28 | 7.34±0.28 | 0.9 |
| P value | 0. 001* | 0.001* | - |
| Mean urinary output, mL/24h ± SD | |||
| Pretreatment | 378.0±334.1 | 444.0±335.5 | 0.6 |
| Posttreatment | 1602.0±380.2 | 1496.0±331.2 | 0.5 |
| P value | 0.0001* | 0. 0001* | - |
ILIB, Intravascular laser irradiation of blood; NS, non-significant.
* Statistically significant.
The primary outcomes in regard to urine and serum levels of NGAL are shown in Table 2. These two parameters show declines from the baseline in both groups; however, the reduction slope of urine NGAL as well as serum NGAL occurred faster in the laser group in a statically significant manner. None of the patients reported any side effects of the treatment in both groups.
Table 2. Serum and Urine NGAL at the Baseline and on Days 3 and 5 in Both Groups.
| ILIB | Sham Laser | P Value | |
| Patients, No. | 10 | 10 | - |
| Mean serum NGAL, ng/mL ± SD | |||
| Day 1 | 687.1±134.7 | 618.0±242.4 | 0.44 |
| Day 3 | 367.8±165.4 | 580.3±233.6 | 0.03* |
| Day 5 | 247.1±85.1 | 406.1±209.9 | 0.04* |
| P value | 0.0001* | 0.0001* | - |
| Mean urine NGAL, ng/mL ± SD | |||
| Day 1 | 723.7±85.1 | 669.9±201.6 | 0.45 |
| Day 3 | 321.0±129.8 | 572.9±206.0 | 0.005* |
| Day 5 | 219.0±64.3 | 392.9±251.1 | 0.04* |
| P value | 0.0001* | 0.0001* | - |
ILIB, Intravascular laser irradiation of blood; NS, non-significant.
* Statistically significant.
Discussion
Being a highly sensitive, specific, predictive, and early biomarker for AKI in many different disease processes7, NGAL is a 25 kDa protein which belongs to the lipocalin superfamily.8 Although it was first discovered in activated neutrophils, a considerable number of cells such as kidney tubular cells may make NGAL in reaction to different insults.7 It has also been revealed that it plays a part in iron metabolism due to its binding with siderophores and in kidney development and tubular regeneration after injury. Further, experiments have indicated that it is highly expressed in reaction to tubular injury.9
ILIB pioneered in Russia is related to the irradiation of blood via an intravenous needle or transcutaneously venous radiation.15 The wavelengths which are frequently used are 890, 630, 650, and recently 450 nm.12 ILIB has been evaluated as a non-invasive treatment for some chronic pathologic diseases such as cardiovascular problems and diabetes.16 It seems that the ILIB mechanism of action in these patients was associated with increasing the content of oxygen and reducing the pressure of carbon dioxide. Also, it removes tissue hypoxia, normalizes tissue metabolism, stimulates oxygenation, releases cytokines, modulates the production of growth factors, and develops new blood vessels.17,18 To our knowledge, this was the first study to investigate the role and the efficacy of ILIB in the treatment of AKI. We hypothesize that ILIB could act through the above-mentioned mechanism to accelerate the improvement of the injured kidney.
In order to evaluate the clinical impact of ILIB on AKI, we used urine and plasma NGAL concentrations to improve our accuracy and rapidity of assessment. The levels of NGAL can be identified in the plasma and the urine of patients as early as 2 hours after the damage. They reach their zenith at about 6 hours and remain high for five days; thereafter, they begin to decrease.19 In our study, the serum levels of urine and plasma NGAL in both groups decreased during the 5-day admission; however, the reduction slope of these parameters occurred faster in the laser group in a statistically significant manner. This finding strengthens our hypothesis that ILIB could accelerate the improvement of the injured kidney. In fact, blood creatinine levels were normal in both groups when the patients were discharged, although a further decline in NGAL levels in the laser group during the treatment may confirm that the ILIB can help patients with AKI recover better.
The present study was, as far as our knowledge allows, the first randomized double-blind placebo-controlled clinical trial which demonstrated the beneficial effect of low-intensity laser irradiation on patients with AKI. As the data from the related literature was extremely scarce and our study was the first in this field, the number of patients included in the present research was limited. This could likely influence the study outcomes. The major strong point of this trial was the double-blind design of the investigation. Whether this phototherapy could be used prophylactically to reduce NGAL levels resulting from AKI, thus shortening the length of a hospital stay and obviating the need for dialysis in these patients, remains to be elucidated by further studies. Further randomized controlled experiments with a lengthier follow-up period and more case numbers are needed to confirm this theory.
Conclusion
A decline in NGAL levels in the laser group during the treatment may suggest that the ILIB can help patients with AKI recover better.
Ethical Considerations
The bioethics board of the Laser Application in Medical Sciences Research Center (LAMSRC) approved the design of this research which followed the ethical guidelines of the 1975 Helsinki Declaration. The trial is registered at the Iranian Registry of Clinical Trials, number IRCT20111121008146N33.
Conflict of Interests
The authors have nothing to disclose and conflict of interest.
Acknowledgment
This study was approved in Laser Application in Medical Sciences Research Center (LAMSRC), Shahid Beheshti University of Medical Sciences, as a research project.
Please cite this article as follows: Razzaghi MR, Ghanei E, Sheida Malekian S, Mazloomfard MM. Intravenous laser therapy in patients with acute kidney injury: A randomized clinical trial. J Lasers Med Sci. 2021;12:e49. doi:10.34172/jlms.2021.49.
References
- 1.Basile DP, Anderson MD, Sutton TA. Pathophysiology of acute kidney injury. Compr Physiol 2. 012;2(2):1303–53. doi: 10.1002/cphy.c110041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomas ME, Blaine C, Dawnay A, Devonald MA, Ftouh S, Laing C. et al. The definition of acute kidney injury and its use in practice. Kidney Int. 2015;87(1):62–73. doi: 10.1038/ki.2014.328. [DOI] [PubMed] [Google Scholar]
- 3.Makris K, Spanou L. Acute Kidney Injury: Definition, Pathophysiology and Clinical Phenotypes. Clin Biochem Rev. 2016;37(2):85–98. [PMC free article] [PubMed] [Google Scholar]
- 4.Mandelbaum T, Scott DJ, Lee J, Mark RG, Malhotra A, Waikar SS. et al. Outcome of critically ill patients with acute kidney injury using the Acute Kidney Injury Network criteria. Crit Care Med. 2011;39(12):2659–2664. doi: 10.1097/CCM.0b013e3182281f1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Grande A, Giuffrida C, Carpinteri G, Narbone G, Pirrone G, Di Mauro A. et al. Neutrophil gelatinase-associated lipocalin: a novel biomarker for the early diagnosis of acute kidney injury in the emergency department. Eur Rev Med Pharmacol Sci. 2009;13(3):197–200. [PubMed] [Google Scholar]
- 6.Lebkowska U, Malyszko J, Lebkowska A, Koc-Zorawska E, Lebkowski W, Malyszko JS. et al. Neutrophil gelatinase-associated lipocalin and cystatin C could predict renal outcome in patients undergoing kidney allograft transplantation: a prospective study. Transplant Proc. 2009;41(1):154–7. doi: 10.1016/j.transproceed.2008.10.092. [DOI] [PubMed] [Google Scholar]
- 7.Soni SS, Cruz D, Bobek I, Chionh CY, Nalesso F, Lentini P. et al. NGAL: a biomarker of acute kidney injury and other systemic conditions. Int Urol Nephrol. 2010;42(1):141–50. doi: 10.1007/s11255-009-9608-z. [DOI] [PubMed] [Google Scholar]
- 8.Bolignano D, Donato V, Coppolino G, Campo S, Buemi A, Lacquaniti A. et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a marker of kidney damage. Am J Kidney Dis. 2008;52(3):595–605. doi: 10.1053/j.ajkd.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Mishra J, Ma Q, Kelly C, Mitsnefes M, Mori K, Barasch J. et al. Kidney NGAL is a novel early marker of acute injury following transplantation. Pediatr Nephrol. 2006;21(6):856–63. doi: 10.1007/s00467-006-0055-0. [DOI] [PubMed] [Google Scholar]
- 10.Cetiner S, Kahraman SA, Yücetaş S. Evaluation of low-level laser therapy in the treatment of temporomandibular disorders. Photomed Laser Surg. 2006;24(5):637–41. doi: 10.1089/pho.2006.24.637. [DOI] [PubMed] [Google Scholar]
- 11.Kazemikhoo N, Rahbar MR, Akrami SM. Low-level laser therapy along with intravascular laser in deep pressure ulcer resistant to conventional therapies. J Skin Stem Cell. 2015;2(4):e30686. doi: 10.17795/jssc30686. [DOI] [Google Scholar]
- 12.KazemiKhoo N, Ansari F. Blue or red: which intravascular laser light has more effects in diabetic patients? Lasers Med Sci. 2015;30(1):363–6. doi: 10.1007/s10103-014-1672-7. [DOI] [PubMed] [Google Scholar]
- 13.Kazemi Khoo N, Iravani A, Arjmand M, Vahabi F, Lajevardi M, Akrami SM. et al. A metabolomic study on the effect of intravascular laser blood irradiation on type 2 diabetic patients. Lasers Med Sci. 2013;28(6):1527–32. doi: 10.1007/s10103-012-1247-4. [DOI] [PubMed] [Google Scholar]
- 14.Ephraim RKD, Darkwah KO, Sakyi SA, Ephraim M, Antoh EO, Adoba P. Assessment of the RIFLE criteria for the diagnosis of Acute Kidney Injury; a retrospective study in South-Western Ghana. BMC Nephrol. 2016;17(1):99. doi: 10.1186/s12882-016-0318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moskvin SV. Low-Level Laser Therapy in Russia: History, Science and Practice. J Lasers Med Sci. 2017;8(2):56–65. doi: 10.15171/jlms.2017.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaviani A, Djavid GE, Ataie-Fashtami L, Fateh M, Ghodsi M, Salami M. et al. A randomized clinical trial on the effect of low-level laser therapy on chronic diabetic foot wound healing: a preliminary report. Photomed Laser Surg. 2011;29(2):109–14. doi: 10.1089/pho.2009.2680. [DOI] [PubMed] [Google Scholar]
- 17.Ihsan FR. Low-level laser therapy accelerates collateral circulation and enhances microcirculation. Photomed Laser Surg. 2005;23(3):289–94. doi: 10.1089/pho.2005.23.289. [DOI] [PubMed] [Google Scholar]
- 18.Schindl A, Schindl M, Schön H, Knobler R, Havelec L, Schindl L. Low-intensity laser irradiation improves skin circulation in patients with diabetic microangiopathy. Diabetes care. 1998;21(4):580–584. doi: 10.2337/diacare.21.4.580. [DOI] [PubMed] [Google Scholar]
- 19.Tuladhar SM, Püntmann VO, Soni M, Punjabi PP, Bogle RG. Rapid detection of acute kidney injury by plasma and urinary neutrophil gelatinase-associated lipocalin after cardiopulmonary bypass. J Cardiovasc Pharmacol. 2009;53(3):261–6. doi: 10.1097/FJC.0b013e31819d6139. [DOI] [PubMed] [Google Scholar]