A 70-year-old female with history of rheumatic fever as a child with resultant surgical mitral valve replacement with bioprosthetic valve ten years prior presented to the hospital with worsening shortness of breath of two days duration. Associating symptoms included orthopnea, dry cough, and lower extremity edema. In the Emergency Room, the patient was afebrile and hemodynamically stable; however, she was tachypneic and hypoxic requiring non-rebreather. Physical examination revealed a systolic and diastolic murmur 3/5 in intensity heard best at the apex along with bilateral basilar crackles. Labs were significant for an elevated N-terminal prohormone of brain natriuretic peptide. The patient was admitted to the Cardiac Care Unit for suspected acute decompensated heart failure. Transthoracic echocardiogram (TTE) was ordered and revealed a preserved ejection fraction with normal diastolic function, however, it also showed the bioprosthetic mitral valve seated angled toward the left ventricular outflow tract rather than the left ventricular cavity (Figure 1). A transesophageal echocardiogram was then performed and confirmed the valve oriented to the basal interventricular septum and left ventricular outflow tract. The effective regurgitant orifice was calculated at 0.54 cm2 with a regurgitant volume of 68 mL/beat, as well as a mean trans-mitral gradient of > 10 mmHg. These findings were consistent with severe mitral regurgitation and severe mitral stenosis ( Figure 2). Structural cardiology was consulted and the patient is currently undergoing evaluation for mitral valve replacement.
Figure 1.
Transesophageal echocardiogram long axis view of mitral valve.
The valve is oriented to basal interventricular septum and left ventricular outflow tract (white arrow) rather than left ventricle cavity.
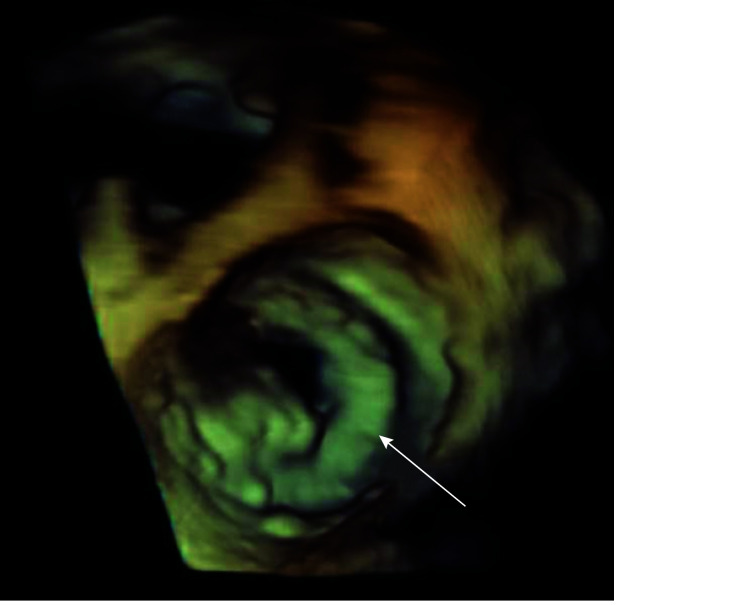
Figure 2.
Transesophageal echocardiogram three-dimensional image of mitral valve.
Image revealing severe stenosis of mitral valve (white arrow).
Rheumatic fever is the leading cause of mitral stenosis. Chronic inflammation leads to thickening of the valve leaflets with formation of fibrous tissue. There is fusion of the mitral commissures, the chordae tendinae will fuse and shorten, and eventually the process leads to narrowing of the apex of the valve creating a “fish mouth.” Over time, heart failure, pulmonary congestion, and pulmonary hypertension with right sided heart failure can develop. Symptoms will include dyspnea on exertion, orthopnea and lower extremity swelling.[1] TTE is accurate for assessing the valvular abnormalities. Normally, the area of the mitral valve is 4–6 cm2. When the valve area is less than 1.5 cm2, this results in severe mitral stenosis (which usually corresponds to a mean mitral gradient of more than 5 mmHg to 10 mmHg).[2] Mitral regurgitation may arise in rheumatic heart disease when there is chordal rupture and flail leaflet. Findings on TTE with severe mitral regurgitation will include an effective regurgitant orifice area of 0.4 cm2 or larger, regurgitant volume of 60 mL or more, or vena contracta of 0.7 cm or larger.[3] The transesophageal echocardiogram is often used in rheumatic heart disease when a TTE is inadequate and for guiding management decisions. Mitral valvotomy is indicated in patients with severe mitral stenosis. Mitral valve replacement is the procedure of choice when there is significant associated mitral regurgitation. Currently, the most common complications of a prosthetic valve include thromboembolism, structural valve dysfunction, and endocarditis. In total, serious complications occur in about 2% to 3% per patient-year.[4] In our patient, she had malposition and stenosis with resulting regurgitation of her bioprosthetic mitral valve.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.
References
- 1.Marijon E, Mirabel M, Celermajer DS, et al Rheumatic heart disease. Lancet. 2012;379:953–964. doi: 10.1016/S0140-6736(11)61171-9. [DOI] [PubMed] [Google Scholar]
- 2.Omran AS, Arifi AA, Mohamed AA Echocardiography in mitral stenosis. J Saudi Heart Assoc. 2011;23:51–58. doi: 10.1016/j.jsha.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Enriquez-Sarano M, Akins CW, Vahanian A Mitral regurgitation. Lancet. 2009;373:1382–1394. doi: 10.1016/S0140-6736(09)60692-9. [DOI] [PubMed] [Google Scholar]
- 4.Vesey JM, Otto CM Complications of prosthetic heart valves. Curr Cardiol Rep. 2004;6:106–111. doi: 10.1007/s11886-004-0007-x. [DOI] [PubMed] [Google Scholar]