Abstract
Background:
Premature rupture of the membrane is a serious public health problem, especially in low- and middle-income countries with significant maternal and perinatal morbidity and mortality. Despite its substantial contributions to feto-maternal complications, the burden of premature rupture of the membrane was not systematically analyzed in Ethiopia. Hence, this review aimed to identify the burden of premature rupture of the membrane and associated factors among pregnant women in Ethiopia.
Methods:
PubMed/Medline, Scopus, and African journal online databases and Google Scholar were searched for articles published in the English language. Independent review authors selected and screened studies. Appraisal for methodological quality of studies was conducted using the Joanna Briggs Institute assessment checklist. RevMan 5.3 software was used for meta-analysis. The I2 statistical significance and Egger’s test were used to assess heterogeneity and publication bias, respectively.
Results:
The pooled prevalence of premature rupture of the membrane among pregnant women in Ethiopia was 9.2% (95% confidence interval = 5.0, 16.4). Factors significantly associated with premature rupture of the membrane were no antenatal care visit (odds ratio = 2.87, confidence interval = 1.34, 6.14), history of premature rupture of the membrane (odds ratio = 4.09, 95% confidence interval = 2.82, 5.91), history of abortion (odds ratio = 3.13, confidence interval = 1.63, 6.01), abnormal vaginal discharge (odds ratio = 6.78, confidence interval = 4.11, 11.16), and urinary tract infection (odds ratio = 3.04, confidence interval = 1.21, 7.63).
Conclusion:
Nearly one in ten pregnancies in Ethiopia encounters premature rupture of the membrane complications. The finding highlights improving antenatal care utilization, thus preventing or treating urinary and reproductive tract infections, and tailored interventions for pregnant women with a history of premature rupture of the membrane or abortion contribute to reduced premature rupture of the membrane.
Keywords: Premature rupture of membrane, meta-analysis, Ethiopia
Introduction
Premature rupture of the membranes (PROMs) are defined as the disruption of fetal membranes before the onset of labor, which is characterized by a painless gush of watery fluid out of the vagina. 1 A PROM that occurs before 37 and after 37 weeks of gestation is referred to as preterm and term premature rupture of membranes, respectively.2,3 The occurrence of PROM ranges from 5% to 15% of all pregnancies worldwide.4,5
Globally, preterm birth is among the three major causes of neonatal death, 6 and PROM contributes to more than 40% of preterm deliveries 7 and is linked with the cause of 18%–20% and 21.4% of perinatal mortalities and morbidity, respectively.8,9 It is a significant cause of perinatal, neonatal, and maternal morbidity and mortality both in high- and low-income countries. 10
Premature rupture membrane causes fetal distress (i.e. due to umbilical cord compression or placental abruption), sepsis, and intraventricular hemorrhage; it increases the risk of cesarean delivery due to non-reassuring fetal heart rate.9,11 In addition to significant mortality, PROM accounts for around 10%–40% of respiratory distress syndrome.12,13 It has been also related to the causes of long-term adverse neurodevelopmental outcomes such as visual or hearing difficulties, intellectual disabilities, developmental and motor delay, cerebral palsy, or death.12,14
PROM contributes to maternal infections (15%–25%), 10 chorioamnionitis (13%–60%), placental abruption (9%–12%), and increase risk of disseminated intravascular coagulopathy and operative deliveries. 9 It rarely causes serious complications such as retained placenta, hemorrhage accompanied by dilation and curettage, and maternal death.15–17 The prevalence and impacts of PROM are disproportionately higher among adolescent women, 18 where they account for more than 11% of births worldwide, 19 suggesting that nutritional deficiencies may play an important role in this complication. 20 Furthermore, the burden of PROM is not limited only to maternal and neonatal mortality and morbidity but also causes a nationwide economic loss due to drug expense, hospitalization, and burden to the health professionals.7,14
Several strategies such as preparing a training manual and guidelines on Basic Emergency Obstetric and Newborn Care to enhance the competency of health professionals in managing obstetric emergencies including PROM, capacitating health facilities, and free maternity service decree to tackle maternal and neonatal mortality were implemented in Ethiopia.21,22 Thus, a significant stride has been made in the past decade in the reduction of maternal and neonatal mortality from 871 per 100,000 and 49 per 1000 in 2000 to 412 and 28 in 2016, respectively. 23 However, maternal and neonatal mortality remained unacceptably high in the world; and to date, the decline for neonatal mortality remained stagnant. 24 Furthermore, PROM is responsible for the significant causes of adverse birth outcomes and common contributor to the three leading causes of neonatal mortality such as preterm birth (26%), intrapartum-related complications (30%), and sepsis (18%) in Ethiopia.25,26 Therefore, failure to improve birth outcomes by 2035 will result in an estimated 116 million deaths and 99 million survivors with disability in the globe. 27 Moreover, the complication of PROM such as low birth weight, birth asphyxia, neonatal infection, puerperal sepsis, and chorioamnionitis is among the serious public health problems in Ethiopia. 28
The primary studies in Ethiopia indicated a varying prevalence of PROM, that is, 3.8% in Oromia 29 and 23.5% in the Harari Region. 30 Moreover, the studies found inconsistent factors associated with PROM, that is, studies stated that history of abortion,13,31 history of smoking, 7 abnormal vaginal bleeding,13,32 and urinary tract infection (UTI) 32 were associated with PROM. On the contrary, abnormal vaginal bleeding,7,30 history of smoking, 13 and UTI13,30 were not significantly associated with PROM in Ethiopia.
Therefore, robust data on the burden of PROM and its associated factors would offer strong evidence for policymakers and program managers to design programs and strategies to prevent neonatal and maternal complications. Hence, this systematic review and meta-analysis aimed to determine the pooled prevalence of PROM and associated factors among pregnant women in Ethiopia.
Materials and methods
The current systematic review and meta-analysis was written following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline checklist 33 (Supplemental file, Table S1).
Eligibility criteria
All peer-reviewed observational (cross-sectional, case–control, and cohort) studies conducted in Ethiopia reported prevalence and/or associated factors of PROM among pregnant women, studies that defined PROM as loss of amniotic fluid before the onset of labor but after fetal viability (>28 weeks of gestation), and English language articles regardless of publication period were eligible. However, studies that reported the outcome of interest emanated from review, commentary, fact sheet, and policy brief was not eligible.
Search and identification of studies
Articles were independently searched systematically from PubMed, Scopus, and African Journals Online (AJOL) databases and Google scholar using appropriate keywords. Database-specific subject headings and free-text terms (premature rupture of membrane OR prelabor rupture of membrane OR premature rupture of fetal membrane OR PROM) AND (risk factors OR determinants OR epidemiological factors OR precipitated factors OR protective factors OR correlates OR predictors) AND Ethiopia were used as appropriate search terms (Supplemental file, Table S2). The two review authors (G.T. and A.M.) independently searched for both published and unpublished studies available until 23 February 2021 G.C.
Study selection
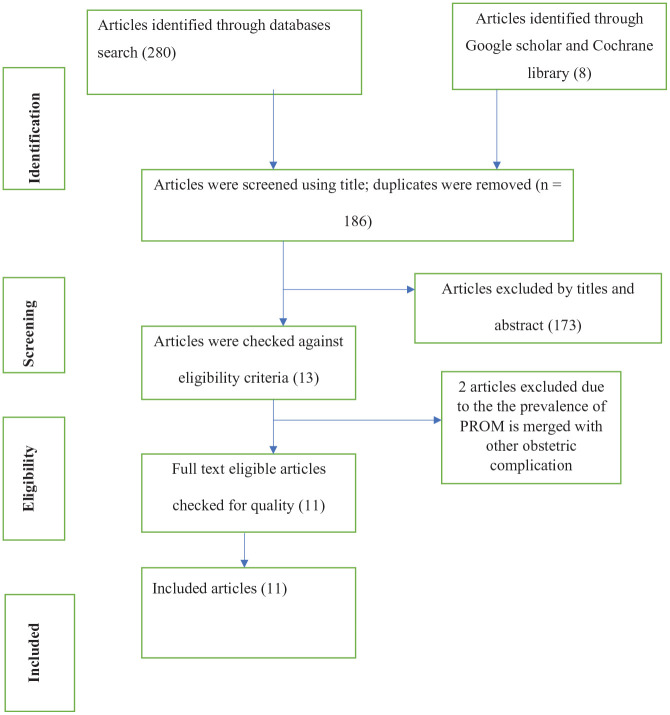
The study selection process had several steps. First, the title and abstract were selected independently by two review authors (G.T. and A.M.) based on eligibility criteria. Second, removing the duplicates, the potentially relevant full-text articles based on the predetermined eligibility criteria were selected through discussion. In the case of disagreement between review authors on the status of studies, the other review authors (K.S., A.K.T., or A.D.) were consulted for the final decision. Finally, the full-text eligible articles were checked for quality. The overall selection process of the studies is available on the PRISMA flow diagram (Figure 1).
Figure 1.
Flowchart showing the procedure of selecting studies for the systematic review and meta-analysis, until 23 February 2021.
Data extraction
The data extraction template was prepared using a Microsoft Excel spreadsheet to record data. The characteristics of the study such as author(s), year of publication, study design, sample size, study setting, regions, and events or cases of PROM were extracted for each article (Table 1).
Table 1.
Descriptive summary of studies included in the meta-analysis of prevalence and associated factors of PROM in Ethiopia.
| First author | Publication year | Study region | Study design | Sample size | Prevalence | Quality of the study |
|---|---|---|---|---|---|---|
| Tadesse et al. 29 | 2017 | Oromia | Cross-sectional | 807 | 3.8 | Low risk |
| Addisu et al. 32 | 2020 | Amhara | Cross-sectional | 424 | 13.8 | Low risk |
| Woyessa et al. 31 | 2020 | Oromia | Cross-sectional | 284 | 13.4 | Low risk |
| Yadeta et al. 30 | 2020 | Harari | Cross-sectional | 1688 | 23.5 | Low risk |
| Mirkuzie et al. 39 | 2016 | Addis Ababa | Cross-sectional | 2820 | 19.7 | Low risk |
| Endale et al. 41 | 2016 | SNNPR | Cross-sectional | 4525 | 4.1 | Low risk |
| Diriba et al. 5 | 2017 | Oromia | Cross-sectional | 2896 | 14.6 | Low risk |
| Woldegeorges et al. 42 | 2019 | Tigray | Cross-sectional | 212 | 13.7 | Low risk |
| Sirak et al. 40 | 2014 | Addis Ababa | Cross-sectional | 8283 | 1.4 | Low risk |
| Workineh et al. 7 | 2017 | SNNPR | Case-control | 298 | – | Low risk |
| Assefa et al. 13 | 2018 | Tigray | Case-control | 2440 | – | Low risk |
PROM: premature rupture of the membrane; SNNPR: South Nations, Nationalities, and People’s Republic.
Outcome measure
The primary outcome of this review was the prevalence of PROM. The secondary outcomes include determinants of PROM such as antenatal care (ANC) visit, history of abortion, history of PROM, UTI, and abnormal or sexually transmitted infections (STIs).
Study quality
The methodological quality of included studies was assessed using the Joanna Briggs Institute (JBI) assessment checklist for cross-sectional and case–control studies. 34 The eight criteria were rated for cross-sectional studies, that is, (1) criteria for inclusion, (2) study subjects and the setting described, (3) exposure measured validly and reliably, (4) standard criteria used for measurement, (5) confounding factors identified, (6) strategies to appropriate statistical analysis deal with confounding factors, (7) outcomes measured validly and reliably and (8) appropriate statistical analysis. Similarly, case–control studies were rated using 10 criteria, that is, (1) comparable groups, (2) cases and controls matched, (3) the same criteria used for identification, (4) exposure measured in a standard, valid, and reliable way, (5) exposure measured in the same way for cases and controls, (6) confounding factors identified, (7) strategies to deal with confounding factors, (8) outcomes assessed in a standard, valid, and reliable way for cases and controls, (9) the exposure period of interest long enough, and (10) appropriate statistical analysis. Finally, studies that scored 50% and above in the quality assessment indicators both for cross-sectional and case–control checklist were considered as low risk and included in the analysis (Supplemental file, Table S3). 35 Two review authors (G.T. and A.M.) independently rated the quality of the eligible studies. The review authors (K.S., A.K.T., or A.D.) was consulted in case of disagreements.
Statistical analysis
The characteristics of included studies were tabulated. Quantitative synthesis of the pooled estimate was computed using RevMan version 5.3 software. The association between PROM and possible factors was reported using odds ratios with a 95% confidence interval. Random effect models were fitted 36 to pool the prevalence of PROM and its associated factors among pregnant women. The level of heterogeneity was determined using the I-squared statistic (I2). 37 Egger’s regression intercept was used to identify publication bias and its presence was declared at a p-value less than 0. 38
Results
As shown in Figure 1, a total of 288 articles were identified during the initial search, of which 13 articles were assessed against eligibility criteria. Two articles were excluded, and the prevalence of PROM is merged with other obstetric complications. Finally, 11 articles were included in this systematic review and meta-analysis (Figure 1).
Characteristics of included studies
A total of 11 studies with 24,677 sample sizes were included, of which nine were cross-sectional,5,29–32,39–42 and two were case–control studies.7,13 The studies included in this systematic review and meta-analysis were from five regions and one city administration of the country (Table 1).
Prevalence of PROM
We included nine cross-sectional studies that reported the proportion of PROM in the pooled prevalence of PROM among pregnant women in Ethiopia. The total sample size of the included studies was 21,939, of which 1828 pregnancies were complicated by the PROM. Therefore, the pooled prevalence of PROM in this study was 9.2% (95% confidence interval (CI) = 5.0, 16.4) among pregnant women in Ethiopia. However, a substantial heterogeneity was observed among the included studies (I2 = 99.3%, p-value < 0.01).
Sub-group analysis
To identify possible sources of heterogeneity, subgroup analysis was done based on sample size, study region, and study setting. The heterogeneity that was present in the overall meta-analysis was partially explained with stratification by sample size. For example, in a subgroup analysis of sample size <500 (odds ratio (OR) = 13.6 (95% CI = 11.2, 16.3); p-value = 0.90; for heterogeneity test, I2 = 0%) was not statistically heterogeneous (Table 2).
Table 2.
Subgroup analysis of the prevalence of PROM in Ethiopia.
| Variable | Characteristics | Number of studies | Sample size | Prevalence (95% CI) | Heterogeneity |
|---|---|---|---|---|---|
| By region | Oromia | 3 | 3987 | 9.3 (4.3, 18.9) | 96.5 |
| Amhara | 1 | 424 | 13.7 (10.3, 17.3) | – | |
| Harari | 1 | 1688 | 23.5 (21.6, 25.6) | – | |
| Addis Ababa | 2 | 11,103 | 5.5 (0.3, 49.7) | 99.8 | |
| SNNPR | 1 | 4525 | 4.1 (3.5, 4.7) | – | |
| Tigray | 1 | 212 | 13.7 (9.7, 19.0) | – | |
| By sample size | <500 | 3 | 708 | 13.6 (11.5, 16.0) | 0.00 |
| 500–1000 | 1 | 807 | 3.8 (2.7, 5.4) | – | |
| >1000 | 5 | 20,212 | 8.6 (3.6, 19.3) | 99.3 | |
| Study setting | General Hospital | 4 | 1727 | 10.1 (5.5, 17.6) | 93.1 |
| Tertiary Hospital | 3 | 15,704 | 4.4 (1.1, 16.4) | 99.6 |
PROM: premature rupture of the membrane; CI: confidence interval; SNNPR: South Nations, Nationalities, and People’s Republic.
Factors associated with premature rupture of membrane
Antenatal care
The association between not receiving ANC and PROM was examined using five studies.7,13,29–31 Although statistically significant heterogeneity was observed (I2 = 69.6%; p-value = 0.27), women who did not receive ANC during the current pregnancy had 2.88 times increased odds of developing PROM compared to their counterparts (OR = 2.88, 95% CI = 1.34, 6.17) (Figure 2).
Figure 2.
Forest plot showing the pooled effect of ANC on PROM in Ethiopia.
Previous history of PROM
This group of analyses was conducted using four studies.13,30–32 The meta-analysis indicated that women with a history of the previous PROM were at increased odds of developing PROM. Accordingly, women who had a history of PROM were 4.09 times more likely to develop PROM compared to their counterparts. Moderate heterogeneity was detected among the included studies (I2 = 57%) (Figure 3).
Figure 3.
Forest plot showing the pooled effect of the previous PROM on premature rupture of the membrane in Ethiopia.
History of abortion
Three studies13,30,31 included in this meta-analysis revealed that women who had a history of abortion had 3.13 times increased odds of PROM (OR = 3.13, 95% CI = 1.63, 6.01) compared to their counterparts. In this review, a statistically significant high heterogeneity was observed among the included studies (I2 = 76%), but Egger’s test showed no evidence of publication bias (p-value = 0.106) (Figure 4).
Figure 4.
Forest plot showing the pooled effect of abortion history on PROM in Ethiopia.
UTIs
As indicated in Figure 5, the pooled effect of two included studies31,32 illustrated that women who had UTI had 2.96 times increased odds of developing PROM (OR = 2.96, 95% CI = 1.08, 8.09) compared to their counterparts (Figure 5).
Figure 5.
Forest plot showing the pooled effect of UTI on PROM in Ethiopia.
Abnormal vaginal discharge
The pooled analysis of two studies identified that the odds of developing PROM were 6.78 times more common among pregnant women who had vaginal discharge compared to their counterparts (OR = 6.78, CI = 4.11, 11.16) (Figure 6).
Figure 6.
Forest plot showing the pooled effect of abnormal vaginal discharge on PROM in Ethiopia.
Publication bias
In the pooled analysis of prevalence studies, Egger’s regression test revealed no evidence of publication bias among the included studies (p-value = 0.30). Similarly, there was no publication bias among the included studies in the factor analysis. Hence, no major threat to the validity of the review.
Discussion
A disproportionate burden of prematurity due to PROM leads to increased neonatal mortality and morbidity in Sub-Saharan African countries.43,44 In Ethiopia, PROM is one of the major causes of prematurity and infection, which in turn are the leading cause of neonatal death.13,28 In addition, puerperal infection, chorioamnionitis, and disseminated intravascular coagulopathy are among the causes of maternal sufferings linked with PROM. 45 Hence, the impact of PROM on neonatal and maternal mortality indicates a need for pooled data on factors related to PROM in Ethiopia.
In this systematic review and meta-analysis, the estimated pooled prevalence of PROM among pregnant women in Ethiopia was found to be 9.2%. Our finding is in the range of worldwide prevalence of PROM which ranges from 5% to 15%. 4 A study from Indonesia also reported relatively similar findings (10%). 46 However, our finding was substantially higher than the global systematic review and meta-analysis report conducted in 2020 (4.33%). 47 The possible explanation for this discrepancy may be due to the differences in the accessibility and the quality of maternity services they deliver for early screening, preventive measures, and treatments of risk factors for PROM. 48 It is also important to note that in Ethiopia where the coverage and quality of maternity care services are low, 23 women will not have an adequate opportunity to get counseling and health education about the likely risk factors of PROM and early treatment measures for asymptomatic reproductive and UTI during pregnancy. In addition, sociodemographic differences such as comparatively low socioeconomic status, geographical barriers in accessing health care and cultural differences in health seeking behaviors may further aggravate the occurrence of PROM in Ethiopia.
In congruent with previous studies, women who had ANC follow-up had decreased odds of developing PROM. 15 This is because ANC is a universally accepted strategy to reduce pregnancy complications by promoting and maintaining the optimal health of the woman throughout her pregnancy. 49 It offers an opportunity for preventive measures and treatments to the causes of genital tract infection which is the likely risk factor for PROM. 50 In addition, ANC provides an opportunity for health promotion and counseling on risk reduction on the potential predisposing factor of PROM such as nutritional advice, personal hygiene, and avoid behavioral risk factors (i.e. smoking and substance use) during pregnancy. 51
Similarly, women who had a history of abortion had increased odds of developing PROM compared to women with no history. Studies in China 52 and Uganda 53 also reported that women who had a history of abortion were more likely to develop PROM. This could be due to women who had a history of abortion may be predisposed to increase systemic inflammation and stimulation of the infection pathway or increased risk of intra-amniotic infection and intrapartum infection.14,31 Cervical trauma from mechanical dilatation during an abortion may increase the risk of cervical incompetence facilitating upper genital tract infection which spread to intra-amniotic infection following pregnancy 12 ; or this association is further explained by, women who have had an abortion in the past, especially multiple abortions, are more likely to have a short cervix, which has been linked to an increased risk of PROM.54,55
The history of PROM was the strongest predictor for premature rupture of membranes in this study. Thus, women who had a previous history of PROM have a 6.08-fold increased odds of developing premature rupture of membrane. A similar association has been noted in past studies.56–58 This may be due to the recurrence of risk factors for PROM in the study participants such as cervical incompetence and connective tissue disorders, and prior untreated genitourinary infection. 12
The pooled analysis showed that UTI and vaginal discharge were predictors of PROM. The findings of this review bear similarity among studies reported from Uganda 53 and Brazil. 48 Genital tract infection such as UTI and abnormal vaginal discharge, which is a common symptom of genital infections caused by a bacterial infection such as Chlamydia trachomatis, bacterial vaginosis, and Neisseria gonorrhoeae. These bacteria release inflammatory mediators or produce proteases, and phospholipases enzymes, and these inflammatory mediators or enzymes produced by genital infections are implicated in weakening of the fetal membranes among pregnant women, causing PROM.12,14,59 However, it has been suggested that intrauterine infection secondary to ascending genital tract colonization can lead to increased cytokine activity that enhances membrane apoptosis, production of proteases, and dissolution of the membrane’s extracellular matrix.9,53 Generally, the study highlighted that reinforcing pregnancy care, tackling abortion-related risk factors, and preventing and treating urinary and genital tract infections would have paramount importance in reducing the public health impacts of PROM.
Strength and limitation of the study
The extensive searches of multiple databases without limiting the search to the study period and the inclusion of unpublished work in this meta-analysis that results in capturing more articles that addresses PROM in Ethiopia are the strength of the systematic review and meta-analysis. However, the absence of primary study representation across all regions of the country due to the unavailability of study from some regions was the limitation of this study. Regardless of these limitations, this study provided important information that is helpful to design an intervention for the reduction of PROM and its pregnancy complications among women and newborns in Ethiopia.
Conclusion
Nearly one in ten pregnancies was complicated by PROM in Ethiopia. The incidence of PROM depends on ANC visit, history of PROM, history of abortion, abnormal vaginal discharge, and UTI. Therefore, promoting utilization of ANC visits, early identification, and treatment of urinary and reproductive tract infection, tailored intervention for pregnant women with a history of abortion, and PROM play a substantial role in reducing PROM among pregnant women in Ethiopia.
Supplemental Material
Supplemental material, sj-doc-1-smo-10.1177_20503121211053912 for Prevalence of premature rupture of membrane and its associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis by Getahun Tiruye, Kassiye Shiferaw, Abera Kenay Tura, Adera Debella and Abdulbasit Musa in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121211053912 for Prevalence of premature rupture of membrane and its associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis by Getahun Tiruye, Kassiye Shiferaw, Abera Kenay Tura, Adera Debella and Abdulbasit Musa in SAGE Open Medicine
Supplemental material, sj-docx-3-smo-10.1177_20503121211053912 for Prevalence of premature rupture of membrane and its associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis by Getahun Tiruye, Kassiye Shiferaw, Abera Kenay Tura, Adera Debella and Abdulbasit Musa in SAGE Open Medicine
Footnotes
Author contributions: G.T., A.M., and K.S. contributed to the conceptualization. G.T. A.M., and K.S. contributed to the methodology, software, formal analysis, validation, and data curation. G.T., A.M., A.K.T., KS., and A.D. contributed to the investigation. G.T., A.M., and K.S. contributed to writing original draft preparation. G.T., A.M., and A.K.T. contributed to writing review and editing. All authors have read and agreed to the published version of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Getahun Tiruye  https://orcid.org/0000-0002-0441-0440
https://orcid.org/0000-0002-0441-0440
Adera Debella  https://orcid.org/0000-0002-8060-0027
https://orcid.org/0000-0002-8060-0027
Supplemental material: Supplemental material for this article is available online.
References
- 1. Konar H. DC Dutta’s textbook of obstetrics. 9th ed. New Delhi, India: Jaypee Brothers Medical Publishers, 2018. [Google Scholar]
- 2. Kuba K, Bernstein PS. ACOG practice bulletin no. 188: prelabor rupture of membranes. Obstet Gynecol 2018; 131(6): 1163–1164. [DOI] [PubMed] [Google Scholar]
- 3. DeCherney A. Current diagnosis & treatment: obstetrics & gynecology medical late pregnancy complication, section: premature rupture of membranes. New York: McGraw-Hill, 2014. [Google Scholar]
- 4. Huang S, Xia W, Sheng X, et al. Maternal lead exposure and premature rupture of membranes: a birth cohort study in China. BMJ Open 2018; 8: e021565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Diriba TD. Incidence, maternal and perinatal outcome of premature rupture of fetal membrane cases in Jimma University Teaching Hospital, South west Ethiopia. EC Gynaecol 2017; 5: 163–172. [Google Scholar]
- 6. United Nations Children’s Fund (UNICEF). Levels and trends in child mortality: report 2010: estimates developed by the UN inter-agency group for child mortality estimation. New York: UNICEF, 2010. [Google Scholar]
- 7. Workineh Y, Birhanu S, Kerie S, et al. Determinants of premature rupture of membrane in Southern Ethiopia, 2017: case control study design. BMC Res Notes 2018; 11: 927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu J, Feng Z-C, Wu J. The incidence rate of premature rupture of membranes and its influence on fetal–neonatal health: a report from mainland China. J Trop Pediatr 2010; 56(1): 36–42. [DOI] [PubMed] [Google Scholar]
- 9. Boskabadi H, Zakerihamidi M. Evaluation of maternal risk factors, delivery, and neonatal outcomes of premature rupture of membrane: a systematic review study. J Pediatr Rev 2019; 7: 77–88. [Google Scholar]
- 10. İflazoğlu N, Eroğlu H, Tolunay HE, et al. Comparison of the maternal serum endocan levels in preterm premature rupture of membrane and normal pregnancy. J Obstet Gynaecol Res 2021; 47(9): 3151–3158. [DOI] [PubMed] [Google Scholar]
- 11. Borna S, Borna H, Khazardoost S, et al. Perinatal outcome in preterm premature rupture of membranes with Amniotic fluid index< 5 (AFI< 5). BMC Pregnancy Childbirth 2004; 4(1): 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gibbs R, Karlan B, Haney A, et al. Danforth’s obstetrics and gynecology. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2008. [Google Scholar]
- 13. Assefa NE, Berhe H, Girma F, et al. Risk factors of premature rupture of membranes in public hospitals at Mekele city, Tigray, a case-control study. BMC Pregnancy Childbirth 2018; 18(1): 386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gabbe SG, Niebyl JR, Simpson JL, et al. Obstetrics: normal and problem pregnancies e-book. Elsevier Health Sciences, 2016. [Google Scholar]
- 15. Singh D, Usham R, Kamei H. Preterm prelabour rupture of membrane 1-year study. J Evol Med Dent Sci 2015; 4(49): 8495–8498. [Google Scholar]
- 16. Vishwakarma K, Patel S, Yadav K, et al. Impact of premature rupture of membranes on maternal & neonatal health in Central India. J Evid Based Med Healthcare 2015; 2(49): 8505–8508. [Google Scholar]
- 17. Idrisa A, Pius S, Bukar M. Maternal and neonatal outcomes in premature rupture of membranes at University of Maiduguri Teaching Hospital, Maiduguri, North-Eastern Nigeria. Trop J Obstet Gynaecol 2019; 36(1): 15–20. [Google Scholar]
- 18. Marković S, Bogdanović G, Cerovac A. Premature and preterm premature rupture of membranes in adolescent compared to adult pregnancy. Med Glas (Zenica) 2020; 17(1): 136–140. [DOI] [PubMed] [Google Scholar]
- 19. Kassa GM, Arowojolu A, Odukogbe A, et al. Adverse neonatal outcomes of adolescent pregnancy in Northwest Ethiopia. PLoS ONE 2019; 14(6): e0218259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. de Azevedo WF, Diniz MB, Fonseca ESVB, et al. Complications in adolescent pregnancy: systematic review of the literature. Einstein (Sao Paulo) 2015; 13: 618–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pearson L, Gandhi M, Admasu K, et al. User fees and maternity services in Ethiopia. Int J Gynaecol Obstet 2011; 115(3): 310–315. [DOI] [PubMed] [Google Scholar]
- 22. Federal Ministry of Health. Management of common obstetric complications. Addis Ababa, Ethiopia: Federal Ministry of Health, 2010. [Google Scholar]
- 23. Central Statistical Agency. Ethiopia demographic and health survey. Addis Ababa, Ethiopia: Central Statistical Agency, 2016. [Google Scholar]
- 24. Central Statistical Agency (CSA). Ethiopia mini demographic and health survey 2019: key indicators. Rockville, MD: EPHI and ICF, 2019. [Google Scholar]
- 25. World Health Organization. Estimates generated by the WHO and maternal and child epidemiology estimation group (MCEE). Geneva: World Health Organization, 2017. [Google Scholar]
- 26. Gedefaw G, Alemnew B, Demis A. Adverse fetal outcomes and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pediatr 2020; 20: 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lawn JE, Blencowe H, Oza S, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet 2014; 384(9938): 189–205. [DOI] [PubMed] [Google Scholar]
- 28. Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiopia and Calverton, MD: Central Statistical Agency and ICF International, 2012. [Google Scholar]
- 29. Tadesse T, Asefa F, Negash Y. Magnitude, associated factors and outcome of preterm premature rupture of membrane at Nekemte Referral Hospital, Western Ethiopia: AAU Institutional repository, 2017. [Google Scholar]
- 30. Yadeta TA, Egata G, Seyoum B, et al. Khat chewing in pregnant women associated with prelabor rupture of membranes, evidence from eastern Ethiopia. Pan Afr Med J 2020; 36: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Woyessa TB, Fulea LG, Edossa AW, et al. Premature rupture of membrane and its associated factors among pregnant women admitted to public hospitals in Nekemte town, western Ethiopia. Int Res J Obstet Gynecol 2020; 3: 27. [Google Scholar]
- 32. Addisu D, Melkie A, Biru S. Prevalence of preterm premature rupture of membrane and its associated factors among pregnant women admitted in Debre Tabor General Hospital, North West Ethiopia: institutional-based cross-sectional study. Obstet Gynecol Int 2020; 2020: 4034680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015. Syst Rev 2015; 4(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mueller M, D’Addario M, Egger M, et al. Methods to systematically review and meta-analysis observational studies: a systematic scoping review of recommendations. BMC Med Res Methodol 2018; 18: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Laelago T, Yohannes T, Tsige G. Determinants of preterm birth among mothers who gave birth in East Africa: systematic review and meta-analysis. Ital J Pediatr 2020; 46: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7(3): 177–188. [DOI] [PubMed] [Google Scholar]
- 37. Ioannidis JP, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ 2007; 335: 914–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mirkuzie AH, Sisay MM, Bedane MM. High proportions of obstetric referrals in Addis Ababa: the case of term premature rupture of membranes. BMC Res Notes 2016; 9: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sirak B, Mesfin E. Maternal and perinatal outcome of pregnancies with preterm premature rupture of membranes (PPROM) at Tikur Anbessa Specialized Teaching Hospital, Addis Ababa, Ethiopia. Ethiop Med J 2014; 52(4): 165–172. [PubMed] [Google Scholar]
- 41. Endale T, Fentahun N, Gemada D, et al. Maternal and fetal outcomes in term premature rupture of membrane. World J Emerg Med 2016; 7(2): 147–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Weldegeorges DA, Welay FT, Mengesha MB, et al. Exploring the incidence of premature rupture of membrane and its associated factors in public hospitals of eastern zone Tigray region, Ethiopia, 2019. Curr Womens Health Rev 2021; 17: 1–12. [Google Scholar]
- 43. Chawanpaiboon S, Vogel JP, Moller A-B, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modeling analysis. Lancet Global Health 2019; 7(1): e37–e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Onwughara CE, Moodley D, Valashiya N, et al. Preterm prelabour rupture of membranes (PPROM) and pregnancy outcomes in association with HIV-1 infection in KwaZulu-Natal, South Africa. BMC Pregnancy Childbirth 2020; 20: 204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sajitha AK, Geetha KC, Mumtaz P. The maternal and perinatal outcome in preterm premature rupture of membrane (PROM): a prospective observational study. Int J Clin Obstet Gynaecol 2020; 5(4): 208–212. [Google Scholar]
- 46. Maryuni M, Kurniasih D. Risk factors of premature rupture of membrane. Kesmas National Pub Health J 2017; 11(3): 133–137. [Google Scholar]
- 47. He W, Jin Y, Zhu H, et al. Effect of Chlamydia trachomatis on adverse pregnancy outcomes: a meta-analysis. Arch Gynecol Obstet 2020; 302(3): 553–567. [DOI] [PubMed] [Google Scholar]
- 48. Hackenhaar AA, Albernaz EP, da Fonseca TM. Preterm premature rupture of the fetal membranes: association with sociodemographic factors and maternal genitourinary infections. J Pediatr (Rio J) 2014; 90(2): 197–202. [DOI] [PubMed] [Google Scholar]
- 49. Cumber S, Diale D, Elive S, et al. Importance of antenatal care services to pregnant women at the Buea Regional Hospital Cameroon. J Family Med Health 2016; 2: 23–29. [Google Scholar]
- 50. World Health Organization. WHO statement on antenatal care. Geneva: World Health Organization, 2011. [Google Scholar]
- 51. World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization, 2016. [PubMed] [Google Scholar]
- 52. Zhou Q, Zhang W, Xu H, et al. Risk factors for preterm premature rupture of membranes in Chinese women from urban cities. Int J Gynaecol Obstet 2014; 127(3): 254–259. [DOI] [PubMed] [Google Scholar]
- 53. Byonanuwe S, Nzabandora E, Nyongozi B, et al. Predictors of premature rupture of membranes among pregnant women in rural Uganda: a cross-sectional study at a tertiary teaching hospital. Int J Reprod Med 2020; 2020: 1862786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Li N. Cause analysis and clinical management experience of the premature rupture of membrane. Open J Obstet Gynecol 2013; 3: 222–226. [Google Scholar]
- 55. Patil S, Patil V. Maternal and foetal outcome in premature rupture of membranes. IOSR J Dental Med Sci 2014; 13: 56–83. [Google Scholar]
- 56. Emechebe CI, Njoku C, K A, et al. Determinants and complications of pre-labour rupture of membranes (PROM) at the University of Calabar Teaching Hospital (UCTH), Calabar, Nigeria. Scholars J Applied Med Sci 2015; 3(5B): 1912–1917. [Google Scholar]
- 57. Lovereen S, Khanum M, Nargis N, et al. Maternal and neonatal outcome in premature rupture of membranes. Bangladesh J Med Sci 2018; 17: 479–483. [Google Scholar]
- 58. Bouvier D, Forest JC, Blanchon L, et al. Risk factors and outcomes of preterm premature rupture of membranes in a cohort of 6968 pregnant women prospectively recruited. J Clin Med 2019; 8: 1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Xia H, Li X, Li X, et al. The clinical management and outcome of term premature rupture of membrane in East China: results from a retrospective multicenter study. Int J Clin Exp Med 2015; 8(4): 6212–6217. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-smo-10.1177_20503121211053912 for Prevalence of premature rupture of membrane and its associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis by Getahun Tiruye, Kassiye Shiferaw, Abera Kenay Tura, Adera Debella and Abdulbasit Musa in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121211053912 for Prevalence of premature rupture of membrane and its associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis by Getahun Tiruye, Kassiye Shiferaw, Abera Kenay Tura, Adera Debella and Abdulbasit Musa in SAGE Open Medicine
Supplemental material, sj-docx-3-smo-10.1177_20503121211053912 for Prevalence of premature rupture of membrane and its associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis by Getahun Tiruye, Kassiye Shiferaw, Abera Kenay Tura, Adera Debella and Abdulbasit Musa in SAGE Open Medicine