Abstract
Background:
Type 2 diabetes (T2DM) contributes to high mortality and morbidity because of its major complications related to kidney, heart, brain, and eyes. It also poses a high risk for mortality because of COVID-19. Studies suggest the possible implications of Yoga in delaying or attenuating such complications.
Methodology:
This was a pan-India multi centered cluster-randomized (4 level) two-armed trial in the rural and urban population of all populous states of India. Data were obtained using mobile app in all adults in the household of the selected clusters.
Results:
We report the diabetes related complications in 16623 adults (48% males, 52% females) from 65 districts (1 in 10 districts, 2011 census) of 29 (out of 35) states and Union Territories of India; mean age was 48.2 ± 12.46 years. Out of this 40% lived in rural and 62% in urban locations. In high risk diabetes individuals (scored ≥ 60 points on Indian diabetes risk score key), 18.0% had self-reported history of (peripheral neuropathy, 6.1% had h/o major strokes, 5.5% had minor strokes (transient ischemic episodes), 18.1% had lower limb claudication, 20.5% leg ulcers, 4.4% had h/o cardiac surgery, 4.8% angioplasty, and 15.1% had diabetes retinopathy. Complications were higher in rural than in urban areas, higher in people with extended duration of diabetes. Integrated yoga module for three months (one hour daily) showed significantly better reduction in symptoms related to complications as compared to control group (P < .001)
Conclusion:
The alarming high prevalence of complications in diabetes population calls for urgent action, where yoga may show the benefits in reduction of symptoms of complications.
Keywords: High-risk diabetes, Complications, Yoga, Prevalence of known and newly diagnosed diabetes
Introduction
In the recently estimated worldwide prevalence of diabetes, it has been appraised that 20% of world diabetes population belongs to South Asia. Many studies on the prevalence of diabetes have demonstrated that India will become the diabetes capital of the world by 2030, with a global increase of type 2 diabetes by 48% (186 million).1, 2, 3, 4
Type 2 Diabetes is known for its complications culminating in mortality and morbidity because of micro-vascular and macro-vascular changes. The association between socio-economic status and the prevalence of diabetes with propensity of for macro-vascular disease has been reported. Mortality in diabetes is chiefly because of the effect of metabolic imbalances affecting the vital organs of the body (including heart, brain, and kidney). 5
Neuropathy in DM
Approximately 50% of adults with diabetes will be affected by peripheral neuropathy in their lifetime. 6 A study in UK on 6487 diabetes patients reported an overall prevalence of neuropathy of 28.5% . When it was compared between type 1 and type 2 diabetes, neuropathy was observed in 22.7% in type 1 and 32 % in type 2 diabetes. An association between peripheral neuropathy and increasing age (5% in 20–29 year age group and 44% in 70–79 year age group) has also been observed. 7
Retinopathy in DM
A pooled analysis of data from eight population-based eye surveys in the United States has shown that the estimated crude prevalence rates for retinopathy and vision-threatening retinopathy were 40.3% and 8.2%, respectively, in patients with diabetes, whereas the prevalence rates in the US general population were only 3.4% and 0.75%, respectively. 8
Looking at the Indian scenario, Chennai urban rural epidemiology study established the overall prevalence of diabetes Retinopathy as17.6% which included 21% in patients with known diabetes and 5% in newly detected diabetes cases. 9 Another Chennai study showed similar results with a diabetes retinopathy prevalence of 18%. Retinopathy was significantly associated with higher risk in men, in those with longer than 15 years duration of diabetes and use of insulin. 10
Heart Disease in DM
The age and sex-adjusted cardiovascular disease incidence rate was 286 per 10000 person-years in the patients who attended examination during 1955–1966, whereas it had increased to 147 per 10000 in the patients who attended examination during 1997–1995. 11
Two systemic reviews and meta analyses have shown that integrated yoga lifestyle that included yogic diet, physical postures, pranayama, relaxation techniques, meditation, and yogic concepts for stress management is a safe and effective intervention that improves not only the glycemic outcomes but reduces the associated risk factors for complications in adults with type 2 diabetes.12, 13, 14 Yoga resulted in significant reduction of BMI, improved glycemic control, and melon aldehyde besides increase in glutathione and vitamin C when compared to standard care groups with micro vascular and macro vascular complications. 15 Other yoga studies have shown improvement in balance and improvement in nerve function in cases with sub-clinical neuropathy. 16 Yoga asana resulted in increase of median nerve conduction velocity. 17
Sahay et al reported lowering of drug requirement and the incidence of acute complications like infection and ketosis, decrease in free fatty acids, increase in lean body mass and decrease in body fat percentage and decline in insulin resistance. 18 Thus, yoga appears to be a vital adjuvant in the management of risk factors, disease progression, and complications of type 2 diabetes. 19
In this study, we plan to report the prevalence of complications of diabetes in a high-diabetes risk (score more than 60 on Indian diabetes risk score [IDRS] key) in the Indian population in 2017 and the effect of a short-term yoga lifestyle intervention on the complications of type 2 diabetes.
Methodology
The study methodology relating to the formation of research advisory committee, ethical clearance, registration of the trial, sample size calculation, four-level randomization in rural and urban locations for selection of the survey clusters, training of personnel, are reported in detail in our earlier publications.20, 21 In brief Niyantrita Madhumeha Bharata (Control of Diabetes in India) 2017, or NMB 2017, was a two-phased nationwide study with the twin objectives of estimating the prevalence of diabetes and prediabetes and its complications in a high-risk population followed by an randomized control trial (RCT) using a validated yoga lifestyle protocol.
Phase 1 was a cross-sectional door-to-door survey using a multilevel stratified cluster sampling technique in randomly selected clusters of urban and rural populations, covering 65 (10%) districts of the most populous states/union territories (29/35) of India. This captured the data on IDRS and self-reported diabetes individuals. This was followed by detailed assessments of the presence of complications, the status of diabetes control, laboratory, and other investigations only in the high diabetes risk (≥ 60 on IDRS) individuals (17852).
Phase 2 was a two-armed RCT for three months on a subsample of 4822 (Yoga: 3,130, control –1692) to test the efficacy of a validated common yoga-based lifestyle protocol.
Intervention
In the current study, the intervention of a validated integrated yoga lifestyle protocol was taught by trained certified yoga therapists at all locations daily for 9 days (2 hours/day) in camps followed by weekly supervised group classes and daily one hour home practice using the help of a video and/or booklet. The yoga module included specific practices that would help in lifestyle change through stress management and long-term behavioral change. This included practices that would correct deep-seated imbalances at (a) physical level: Yogic, simple wholesome nutritionally balanced diet, cleansing techniques (yogic nasal wash—neti, stomach wash—dhoti, and neuro-respiratory detox kriya—kapalabhati), and asanas designed for offering deep rest to the sick tissues; (b) pranayama designed to slow down the rate of breathing to improve parasympathetic tone; (c) meditation and relaxation techniques for autonomic stability; and (d) notional correction and devotional sessions for stress management.
Ethical Clearance
Ethical clearance was obtained by the Institutional Ethical Committee of the Indian Yoga Association. Registration was obtained at the central trial registry of India. Funding was given by the Ministry of Health and Family Welfare and the Ministry of AYUSH Government of India, New Delhi.
Data Acquisition
Details of the methodology of the four-level randomization (clustered 29 populous states into seven zones; randomly selected 1:10 districts in each state; one census enumeration block in one randomly selected ward in one randomly selected urban town, and four villages with 250–300 households in rural areas, covering 4,000 population per district) using randomizer.com, of the urban and rural clusters to collect representative samples from all seven zones of India, is published in earlier. 22 Briefly, in the first phase, the data was collected at two levels, using a screening questionnaire to estimate the frequency of self-reported diabetes and comorbidities, select the population at risk for diabetes on IDRS. In the second level, only those in high risk (> 60 on IDRS) and self-reported diabetes were invited for detailed assessments.
Collection of Data of Complications
Table 1 shows the questions pertaining to complications.
Table 1. Complications - Questions Used for Factor Analysis.
| Code | Medical History Stroke | Answer |
| MHS | Have you ever been told by a health care provider that you have had any of the following problems? | |
| MHS1 | Stroke | No 0 Yes 1 |
| MHS2 | Transient ischemic attacks (TIA or "mini-strokes") | No 0 Yes 1 |
| Heart | Answer | |
| HEA | Have you ever had any of the following operations or procedures related to your heart? (circle one answer on each line) | |
| HEA1 | Coronary artery bypass surgery (open heart surgery) | No 0 Yes 1 |
| HEA2 | Coronary angioplasty ("balloon" heart procedure) | No 0 Yes 1 |
| HEA3 | Heart catheterization (angiogram) | |
| Code | Pain/lesions in body or feet or legs | |
| BFL | Have you ever been told by a health care provider that you have any of the following problems with your shoulder, feet or legs? | |
| BFL1 | Peripheral vascular disease (poor circulation in the legs) Any infected wound or ulcer which is not healing | No 0 Yes 1 |
| BFL2 | Do you have stiffness and pain in your shoulder since last three month or more | No 0 Yes 1 |
| BFL3 | Intermittent claudication (cramping in the calves after exercise) | No 0 Yes 1 |
| BFL4 | Peripheral neuropathy (nerve problems causing numbness, tingling, or burning) | No 0 Yes 1 |
| KD | Kidney disease | |
| KD1 | Have you ever been told by a health care provider that you have kidney disease? | No 0 (skip to next section) Yes 1 |
| KD2 | Do you now take medication for your kidney disease? | No 0 (skip to next section) Yes 1 |
| KD3 | How many tabs/doses and how many times a day do you have to take your medication for kidney disease? | 1. Once a day 2. Twice a day 3. Three times a day 99 Don 't know/Not sure |
| Code | High blood pressure | |
| HBP1 | Have you ever been told by a health care provider that you have High blood pressure? | No 0 (skip to next section) Yes 1 |
| HBP2 | Do you now take medication for your high blood pressure? | No 0 (skip to next section) Yes 1 |
| HBP3 | How many tablets a day do you have to consume for high blood pressure? | 1. Once a day 2. Twice a day 3. Three times a day don't know/Not sure |
| Code | High cholesterol | |
| HC1 | Have you ever been told by a health care provider that you have high cholesterol? | No 0 (skip to next section) Yes 1 |
| HC2 | Do you now take medication for your high cholesterol? | No 0 (skip to next section) Yes 1 |
| HC3 | How many tablets a day do you have to consume for high cholesterol? | 1. One tablet at each intake 2. Two tablets at each intake 3. Three tablets at each intake 4. More than four tablets at each intake Don't know/Not sure |
| Code | Any other disease or complications | |
| CO1 | Have you ever been told by a health care provider that you have any other disease or complications at present? | No 0 (skip to next section) Yes 1 |
| EYE1 | Have you ever been diagnosed with any of the following ocular conditions: e.g.: glaucoma, cataracts, macular degeneration, eye injury, retinal disease, blindness, dry eyes | No 0 Yes 1 |
| C02 | Other complications | |
| C03 | Do you now take medication for your other disease or complications? | No 0 (skip to question xx) Yes 1 |
| CO4 | How many tabs/dose and how many times a day do you have to take your medication for any other disease or complications? | 1. Once a day 2. Twice a day 3. Three times a day Don’t know/Not Sure |
| Reliability and validity of the factors checked by Cronbach’s α for subscales. Results: 0.762 with a factor loading of 0.7 in different factors | ||
The mobile app that was used for detailed data collection included the questions with binary answers (Table 1) to document the complications and associated conditions related to the nervous system, cardiovascular, musculoskeletal, renal, and ophthalmic complications with 3–4 items under each heading.
Statistical Analysis
Data were uploaded via mobile apps by trained field personnel under the supervision of senior research fellows. Uploaded data from screening forms (about 4 < 0.001/district), registration forms, and laboratory data (about 50, < 0.001) were checked for perfect matching of coding. The data set was analyzed using Statistical Package for Social Sciences (SPSS) (23.0) and R software for bio-statistical analyses. Chi-square test was adopted for checking the significance of distribution.
Results
Figure 1 shows the consort diagram. Of the 17852 adults screened, data of 16,623 at high risk for diabetes (> 60 on IDRS) were available for analysis after removing missing values. The mean age was 48.2 ± 12.46 years, 48% were males; 39% rural, and 41% urban clusters. The mean duration of diabetes was 7.6 ± 8.3 years. Of these, data on 4,822 respondents (yoga group 3130, control group 1692) for the intervention were available for analysis.
Figure 1. Study Profile.
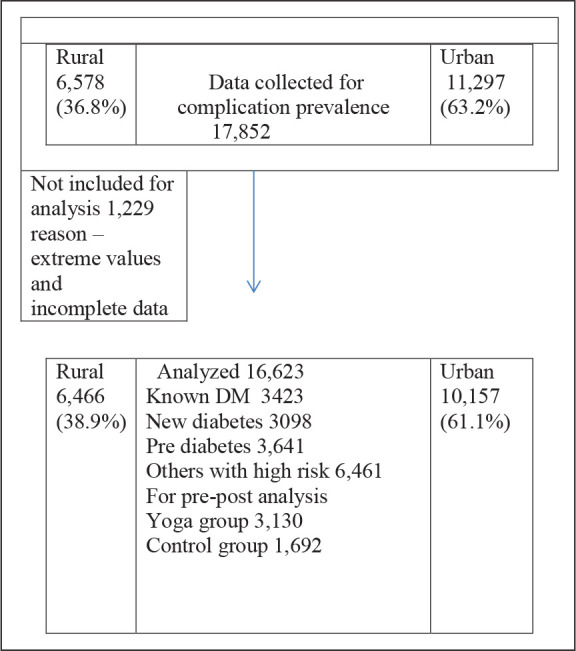
Table 2 shows the percentage of individuals in different categories who reported a history of different complications.
Table 2. Prevalence of Complications in Diabetes Group.
| Groups | Neuro | Cardiac | Kidney Disease | Limb | Eyes | ||||
| Major stroke (in %) | Minor stroke (in %) | Peripheral neuropathy (in %) | Bypass (in %) | Balloon angioplasty (in %) | Claudication (in %) | Foot ulcer (in %) | Patients with diabetes-related eye problems (in %) | ||
| Total DM | 6.1 | 5.5 | 18.0 | 4.4 | 4.8 | 3.2 | 18.1 | 20.5 | 19.9 |
| Self -reported DM | 8.5 | 8.1 | 22.7 | 5.0 | 7.0 | 4.4 | 22.9 | 25.8 | 25.1 |
| New DM | 3.4 | 2.4 | 12.6 | 3.7 | 2.2 | 1.5 | 12.4 | 14.1 | 13.8 |
| Pre DM | 3.0 | 2.2 | 14.4 | 2.2 | 1.8 | 1.3 | 14.0 | 14.8 | 14.6 |
Neurological Complications
Major stroke was reported in 6.1% of patients with diabetes with higher percentages in self-reported known diabetes patients which increased from 4.7% to 8%, as the duration of diabetes increased from 1st to 20th year. Similar trends were found in minor strokes (transient ischemic attacks [TIA]) with an overall prevalence of 5.5%, higher in self-reported (8.1%) known diabetes individuals. Two percent of those who were not aware of their diabetes (newly diagnosed, A1c > 6.5%) already had experienced these minor episodes of TIA.
Peripheral neuropathy was reported in 18.0% of patients with diabetes, higher (22.7%) in the self-reported known diabetes group than newly diagnosed (12.6%) or the prediabetes group (14.4%). In the newly detected and prediabetes adults, leg-related complications (claudication and foot ulcer) were higher when compared to other neurological or cardiac complications. (Table 2)
Cardiovascular Complications
Reports of history of coronary artery bypass graft surgery and angioplasty were higher in self-reported diabetes (5%, 7%) than the newly diagnosed diabetes (3.7%, 2.2%) and prediabetes (2.2%, 1.8%). Peripheral vascular problems with intermittent claudication of lower limbs (18.1%) and leg ulcers (20.5%) showed high prevalence. Retinopathy was found in 15.1% of diabetes adults.
Subgroup Analyses
Looking at the gender differences, most of the major complications such as strokes, claudication, neuropathies, retinopathy, and foot ulcers were higher in females than males. (Table 3), whereas the history of cardiac bypass surgery and angioplasties was higher in males.
Table 3. Prevalence of Complications in The Study Population.
| Groups | Neuro | Cardiac | Kidney Disease | Limb | Eyes | |||||
| Major stroke (in %) | Minor stroke (in %) | Peripheral neuropathy (in %) | Bypass (in %) | Balloon angioplasty (in %) | Claudication (in %) | Foot ulcer (in %) | Patients with diabetes eye (in %) | |||
| Gender | M | 8.1 | 6.7 | 23.0 | 4.4 | 3.2 | 5.3 | 19.7 | 23.1 | 25.2 |
| F | 8.9 | 9.4 | 33.1 | 2.0 | 2.7 | 3.7 | 26.1 | 28.9 | 25.1 | |
| Area | Urban | 7.9 | 7.4 | 25.8 | 5.3 | 2.8 | 5.0 | 23.1 | 25.5 | 26.2 |
| Rural | 9.0 | 8.7 | 35.2 | 4.6 | 3.1 | 4.0 | 22.6 | 26.2 | 23.5 | |
| Age | 20-35 | 7.0 | 6.5 | 25.8 | 2.8 | 2.2 | 7.5 | 17.2 | 24.3 | 11.2 |
| 35-50 | 7.6 | 6.7 | 27.4 | 4.0 | 2.5 | 4.5 | 22.2 | 26.2 | 21.8 | |
| 50-70 | 7.6 | 6.9 | 28.1 | 5.7 | 3.5 | 4.3 | 22.5 | 27.4 | 28.7 | |
| Zones | NW | 2.6 | 1.3 | 25.8 | 2.6 | 1.2 | 0.9 | 23.1 | 14.4 | 31.0 |
| N | 3.6 | 2.7 | 31.8 | 2.2 | 0.9 | 1.3 | 26.0 | 19.7 | 32.1 | |
| NE | 3.3 | 8.1 | 22.5 | 0.5 | 0.4 | 4.3 | 21.4 | 19.0 | 30.0 | |
| W | 5.3 | 3.5 | 24.6 | 5.3 | 1.9 | 2.5 | 24.1 | 27.0 | 24.3 | |
| C | 10.1 | 7.6 | 33.2 | 6.1 | 2.1 | 6.9 | 38.6 | 32.5 | 26.0 | |
| E | 11.2 | 6.0 | 35.4 | 5.8 | 10.1 | 7.2 | 21.2 | 42.9 | 23.4 | |
| S | 5.9 | 3.6 | 24.7 | 5.8 | 2.4 | 4.9 | 16.3 | 20.3 | 23.3 | |
Age and Complications
Foot ulcer, shoulder pain, neuropathies, and eye problems were higher in older age (50–60 years) than younger ones; history of intermittent limb claudication was high in the younger (20–35 group) diabetes population.
Complications in Rural and Urban Population
The number of diabetes patients who reported a history of foot ulcer, shoulder pain, strokes, and or eye-related complaints was higher in the rural regions than urban areas; the prevalence of claudication and nerve problems was high in urban than rural localities.
Complications in Different Zones of India
Number of individuals with foot ulcer, shoulder pain, claudication, and history of stroke was highest in the East zone; nerve problem was highest in the central zone and eye problems were highest in the North zone (Table 3).
The proportion of all complications increased with the increasing duration of diabetes. The percentage of individuals with foot ulcers, shoulder pain, nerve problems, claudication, and eye problems was highest in those with a duration of diabetes of 15–20 years (Table 4).
Table 4. Duration of Diabetes and Complications.
| Complications | 1–5 years (in %) | 5–10 years(in %) | 10–15 years(in %) | 15–20 years(in %) | SignificanceP (Independent Samples t-test) |
| Stroke | 4.7 | 5.7 | 8.2 | 8.0 | .029 |
| Minor stroke | 3.2 | 3.5 | 7.2 | 6.2 | .022 |
| neuropathy | 22.7 | 22.3 | 27.8 | 31.5 | .052 |
| Claudication | 19.9 | 19.2 | 22.7 | 25.3 | .266 |
| Foot ulcer | 22.6 | 23.1 | 29.9 | 25.3 | .122 |
| Kidney disease | 3.2 | 3.3 | 5.2 | 3.2 | .002 |
| Bypass surgery | 3.4 | 3.4 | 9.3 | 9.2 | .002 |
| Balloon surgery | 2.5 | 3.4 | 5.0 | 6.8 | .002 |
| Patients with diabetes retinopathy | 23.4 | 27.7 | 32.1 | 35.8 | .000 |
| Shoulder pain | 24.0 | 25.2 | 31.4 | 32.7 | .011 |
The following changes were noticed in prepost changes in complications: after yoga, 10% reported reduction in foot ulcers, whereas in the control group it increased by 2%. About 5.1% reported a reduction in symptoms related to the eyes. There was 5.1% reduction in diabetes retinopathy in yoga and 7% increase in Control group. Shoulder pain reduced by 9.5%, while in control it increased by 4%; peripheral neuropathy related symptoms reduced by 10.6%, while it increased in the control group by 1%. (Table 5)
Table 5. Symptoms Related to Complications Before and After Intervention.
| Complications | Yoga Pre(in %) | Yoga Post (in %) | Control Pre(in %) | Control Post(in %) | Significance |
| Foot ulcer | 17.3 | 7.2 | 17.9 | 19.5 | P < .001 |
| Shoulder pain | 18.5 | 9.0 | 20.1 | 24.1 | P < .001 |
| Claudication | 15.9 | 6.8 | 15.7 | 17.3 | P < .001 |
| Neuropathy | 16.4 | 5.8 | 16.0 | 17.0 | P < .001 |
| Diabetic eye | 15.6 | 10.5 | 16.8 | 23.8 | P < .001 |
| Patients with diabetes retinopathy | 15.6 | 10.5 | 16.8 | 23.8 | P < .001 |
Discussion
The current pan India community-based cluster-randomized trial of 2017 describes the prevalence ofself-reported complications in 16623 adults with high diabetes risk (score > 60 on IDRS) and also the effect of yoga intervention of three months duration.
Comparisons
Overall, the neurological complications were reported in 29.6%, cardiac (bypass surgery + angioplasty) in 9.2% of diabetes individuals. An earlier study in Goa 23 in 2010 had reported the prevalence of diabetes complications as follows: neuropathy 60%, coronary heart disease -32.3%, cataract 20%, retinopathy 15.4%, peripheral vascular disease 11.5%, and cerebrovascular accidents (CVAs) 6.9% . They also had reported the rising trend in the prevalence of diabetes complications with advancing duration of diabetes which is also seen in our study.
In the present study, we found the prevalence of self-reported known diabetes was higher in females than males, and the prevalence of complications corresponded to the overall prevalence of diabetes in females. This observation of higher prevalence of self-reported diabetes in high-risk females could be because of obesity which is a major risk factor in Indians and is known to be higher in women.24, 25
The prevalence of diabetes complications was higher in rural than urban regions. The awareness about health was found to be much lower in rural areas when compared to urban areas. Studies have discussed that knowledge about diabetes and health awareness is negligible in rural areas 26 . This may be the explanation for the high prevalence of complications in rural areas. As expected, the prevalence was higher among people with a longer duration of diabetes.
A study on the prevalence of neuropathy in 6487 diabetes individuals in the UK in the year 1993 was 32.1% in type 2 diabetes patients. 7 The researchers observed that the prevalence of diabetic peripheral neuropathy increased with age, from 5% in the 20–29 year age group to 44.2% in the 70–79 year age group. But in our study, it was 25.8% in the age group 20–35, in the age group 50–70 it was 28.1%.
Prevalence of neuropathy increases with the duration of diabetes, and earlier studies have reported neuropathy in 20.8 % in patients with diabetes duration of fewer than five years and 36.8 % in those with greater than ten years duration. 7 The prevalence in our study seems to be similar; it increased from 22.7% in those with 1–5 years duration of diabetes to 31.5% in those who had diabetes for 15–20 years.6, 7
We observed a prevalence (25.1%) of retinopathy in our sample. Ghodasra et al observed an 18.0% prevalence of diabetic retinopathy in patients with diabetes in 2006. In their study, the variables that were significantly associated with increased risk of patients with diabetic retinopathy included gender (men at greater risk), use of insulin, and longer duration of diabetes. 10 Similar was our observations in our subjects with known diabetes as we noted an association of retinopathy with increased age, female gender, and duration of diabetes.
Studies have shown strong association between hypertension and hyperlipidemia with diabetic nephropathy. 27 Patients with diabetes complications and/or coronary artery disease had higher prevalence of stroke.31
In the current study, three months of intervention of a validated integrated yoga lifestyle protocol has shown significant (P < .001) reduction in all self-reported complications. We hypothesize that the observed results of reduction of self–reported complications in the present study could be because of stress reduction. It is evident by the earlier studies that patients with diabetes complications have increased oxidative stress levels. 28 It is also known that chronic stress leads to poor control of diabetes with increased risk of micro and macro-vascular complications through activation of the hypothalamic-pituitary-adrenal axis, resulting in increased levels of cortisol, epinephrine, norepinephrine, glucagon, prolactin, leptin, and neuropeptides. 22 Chronic activation of the HPA axis is also associated with increased level of inflammatory cytokines that contribute to insulin resistance in type 2 diabetes. Chronic psychological stress can result in insulin resistance, hypertension, and an increased risk of cardiovascular events. 29 A systematic review on yoga practices on oxidative stress in different populations reported that diabetes patients showed increased glutathione, vitamin C content, and superoxide dismutase activity and decreased malondialdehyde content following yogic practices; prediabetes and hypertensive patients showed reduced malondialdehyde content following yogic practices, and renal disease patients showed decreased protein oxidation and increased superoxide dismutase activity following yogic practices. The review concluded that regular yogic practices can improve antioxidants and reduce oxidative stress in healthy, diabetes, prediabetes, hypertensive, and renal disease patients. 30
Strengths of the Study
It is the first parallel survey covering 29 states/union territories of India on the prevalence of complications and the effect of yoga on all self-reported complications. The self-administered questionnaire used is found to be reliable and valid. This is also the first report that offers evidence to the beneficial effect of yoga in reducing the symptoms (self–reported) related to complications of diabetes.
Limitations of the Study
The limitation of the study was that there were no objective measures of the status of the complications as it was self-reported data.
Conclusions
The prevalence of complications is high in known diabetes individuals. Integrated yoga module can play a significant role in reduction in symptoms related to diabetes complications as self-reported symptoms are reduced. But this should be studied further with bio markers. This study offers important evidence to implement urgent action by policy makers to prevent complications and also offer protection to diabetes community during the present COVID-19 pandemic.
Acknowledgements
We are thankful to the Ministry of health and family welfare and Ministry of AYUSH (routed through Central Council for Research in Yoga and Naturopathy), Government of India for funding this project. We would like to thank the executive committee of Indian yoga Association for their continued support. We also thank Art of Living Institute, Vethathiri Maharishi College of Yoga, Patanjali Yoga-peeth, PGI Chandigarh and SVYASA for providing more than 1200 yoga volunteers. We acknowledge the members of the research advisory board of NMB for their inputs at all stages of the study.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Statement
Ethical clearance was obtained by the Ethics Committee of the Indian Yoga Association. The study was registered on central trial registry of India (Registration Number – Trial REF/2018/02/017724).
This article complies with the International Committee of Medical Journal editor’s (ICMJE) uniform requirements for the manuscript.
Funding
Funding for the study was provided by the Ministry of health and family welfare and the Ministry of AYUSH routed through Central Council for Research in Yoga and Naturopathy, Government of India.
References
- 1.Anjana RM, Pradeepa R, Deepa M. et al. , Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-India DIABetes (ICMR-INDIAB) study. Diabetologia; 2011. December; 54(12): 3022–3027. [DOI] [PubMed] [Google Scholar]
- 2.Deepa M, Grace M, Binukumar B. et al. , High burden of prediabetes and diabetes in three large cities in South Asia: The center for cArdio-metabolic Risk Reduction in South Asia (CARRS) Study. Diabetes Res Clin Pract 2015; 110: 172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohan V, Deepa M, Lanthorn H. et al. , Incidence of diabetes and pre-diabetes in a selected urban South Indian population (CUPS - 19). J Assoc Physicians India 2008 March ; 56: 152–157. [PubMed] [Google Scholar]
- 4.Anjana RM, Rani CSS, Deepa M. et al. , Incidence of diabetes and prediabetes and predictors of progression among Asian Indians: 10-year follow-up of the Chennai urban rural epidemiology study (CURES). Diabetes Care 2015; 38: 1441–1448. [DOI] [PubMed] [Google Scholar]
- 5.Park K. Park’s textbook of preventive and social medicine . Banarsidas. Jabalpur: Banarsidas Bhanot, 2009. [Google Scholar]
- 6.Hicks CW, and Selvin E.. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diab Rep 2019. August 27; 19(10): 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young MJ, Boulton AJM, Macleod AF. et al. , A multicentre study of the prevalence of patients with diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia 1993; 36: 150–154. [DOI] [PubMed] [Google Scholar]
- 8.Kempen JH, O’Colmain BJ, Leske MC. et al. , The Prevalence of Patients with diabetes retinopathy among adults in the United States. Arch Ophthalmol 2004; 122: 552–563. [DOI] [PubMed] [Google Scholar]
- 9.Rema M, Premkumar S, Anitha B. et al. , Prevalence of patients with diabetic retinopathy in urban India: The Chennai Urban Rural Epidemiology Study (CURES) Eye Study, I. Invest Ophthalmol Vis Sci 2005; 46: 2328–2333. [DOI] [PubMed] [Google Scholar]
- 10.Ghodasra DH, and Brown GC.. Prevalence of patients with diabetic retinopathy in India: Sankara Nethralaya patients with diabetic retinopathy epidemiology and molecular genetics study report 2 - Commentary. Evidence-Based Ophthalmol 2009; 10: 160–161. [Google Scholar]
- 11.Fox CS, Coady S, Sorlie PD. et al. , Trends in Cardiovascular Complications of Diabetes. JAMA 2004. November 24; 292(20): 2495–2499. [DOI] [PubMed] [Google Scholar]
- 12.Innes K and Selfe TK.. Yoga for adults with type 2 diabetes: A systematic review of controlled trials. J Diabetes Res 2016; 2016: 6979370. https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84953897530&origin=inward [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cui J, Yan JH, Yan LM. et al. , Effects of yoga in adults with type 2 diabetes mellitus: A meta-analysis. J Diabetes Investig 2017; 8: 201–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bajaj S.RSSDI clinical practice recommendations for the management of type 2 diabetes mellitus 2017. Int J Diabetes Dev Ctries 2018; 38: 1–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hegde S.Effect of 3-month yoga on oxidative stress in type 2 diabetes with or without complications: A controlled clinical trial. Diabetes Care 2011; 34(10): 2208–2210. https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84858717272&origin=inward [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boslego LW.Impact of yoga on balance, balance confidence and occupational performance for adults with patients with diabetic peripheral neuropathy: A pilot study. Br J Occup Ther 2017; 80(3): 155–162. https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85014437002&origin=inward [Google Scholar]
- 17.Malhotra V, Singh S, Tandon OP. et al. , Effect of Yoga asanas on nerve conduction in type 2 diabetes. Indian J Physiol Pharmacol 2002. July; 46(3): 298–306. http://www.ncbi.nlm.nih.gov/pubmed/12613392 [PubMed] [Google Scholar]
- 18.Sahay BK.Role of yoga in diabetes. JAPI. 2007; 55: 121–126. [PubMed] [Google Scholar]
- 19.Raveendran AV, Deshpande A, and Joshi SR.. Therapeutic role of yoga in type 2 diabetes. Endocrinol Metab (Seoul, Korea) 2018; 33(3): 307–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anand A.Narendra Modi’s citizen-centered yoga-diabetes management program: Will Indian state install integrative medicine in premier Institutes? Ann Neurosci 2019; 26(2): 47–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nagendra H, Nagarathna R, Rajesh S. et al. , Niyantrita Madhumeha Bharata 2017, methodology for a nationwide diabetes prevalence estimate: Part 1. Int J Yoga 2019; 12: 179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahajan AS.Role of yoga in hormonal homeostasis. Int J Clin Exp Physiol 2014; 1: 173–178. [Google Scholar]
- 23.Vaz NC, Ferreira AM, Kulkarni MS. et al. , Prevalence of patients with diabetes complications in rural Goa, India. Indian J Community Med 2011; 36: 283–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kautzky-Willer A, Harreiter J, and Pacini G.. Sex and gender differences in risk, pathophysiology, and complications of Type 2 Diabetes Mellitus. Endocr Rev 2016; 37(3): 278–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.India State-Level Disease Burden Initiative Diabetes Collaborators*. The increasing burden of diabetes and variations among the states of India: The Global Burden of Disease Study1990–2016, Lancet Glob Health 2018 September 11; 6: e1352–e1362 https://www.thelancet.com/pdfs/journals/langlo/PIIS2214-109X(18)30387-5.pdf [DOI] [PMC free article] [PubMed]
- 26.Kasliwal RR, Kulshreshtha A, Agrawal S. et al. , Prevalence of cardiovascular risk factors in Indian patients undergoing coronary artery bypass surgery. J Assoc Physicians India 2006; 54: 371–375. [PubMed] [Google Scholar]
- 27.Buren PNV, and Toto R.. Hypertension in patients with diabetes nephropathy: Epidemiology, mechanisms, and management. Adv Chronic Kidney Dis 2011; 18: 28–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kumawat M, Singh N, and Singh S.. Status of antioxidant enzymes and lipid peroxidation in type 2 diabetes mellitus with neuropathy. Ann Neurosci 2005; 12: 49–52. [Google Scholar]
- 29.Innes KE, Bourguignon C, and Taylor AG.. Risk indices associated with insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: A systematic review. J Am Board Fam Pract 2005; 18: 491-519. [DOI] [PubMed] [Google Scholar]
- 30.Pal R and Gupta N.. Yogic practices on oxidative stress and of antioxidant level: A systematic review of randomized controlled trials. J Complement Integr Med 2017. October 25; 16(4): /j/jcim.2019.16.issue-4/jcim-2017-0079/jcim-2017-0079.xml. DOI: 10.1515/jcim-2017-0079. PMID: 29068790. [DOI] [PubMed] [Google Scholar]


