Abstract
Background:
Ankylosing spondylitis (AS) is a chronic autoimmune inflammatory spondyloarthropathy with unclear pathogenesis. The inflammatory pain in AS leads to restricted spinal mobility and significant disability. Yoga is a nonpharmacological intervention that has positive effects on various musculoskeletal-related problems. However, its role in AS is unknown.
Objective:
The present retrospective study assessed the efficacy of a two-week residential yoga intervention on spinal flexibility among AS patients.
Methods:
The records for 24 male AS patients within the age range 30 to 50 years (average age 38.3 ± 10.5 years) who underwent a two-week residential yoga retreat between 2015 and 2020 were obtained from a yoga center located in South India. Yoga intervention consisted of yoga postures, breathing practices, meditation, a healthy diet, and devotional sessions. Pre and Post data of the sit-and-reach test, blood pressure, heart rate, and symptom score were analyzed using Statistical Package for Social Sciences (SPSS).
Results:
Compared to the baseline, the post scores of the sit-and-reach test, systolic blood pressure and heart rate were found to be significantly (P < .05) lower. The symptom score and analgesic medication score also showed significant improvement after two-weeks compared to the baseline.
Conclusion:
This retrospective study indicates the positive impact of on and analgesic use among AS patients. However, additional studies using robust research designs are warranted.
Keywords: Meditation, Inflammation, Back pain, Neurology, Arthritis
Introduction
Ankylosing spondylitis (AS) is a common chronic autoimmune disease that causes significant disability. 1 The global prevalence of AS varies from 1% to 1.5%. 2 Progressive rigidity, back pain, and stiffness over shoulder, neck, hip, and sacroiliac joints are the typical clinical characteristics of AS. As it progresses, AS contributes to significant disability and reduced quality of life of the patients.3, 4 In advanced condition, the inflammation can lead to a complete calcification of the spine, that is, formation of marginal syndesmophytes between adjoining vertebrae of the lumbar region, sacroiliac joints, and adjacent tissue resembling “bamboo,” causing an immobilize position and other morbidities. 5 AS significantly contributes to reduced lung capacity and increases the risk of lung infections. 6 Human Leukocyte Antigen (HLA)-B27 and inflammatory biomarkers such as interleukin 23 and 17 are associated with AS. 7 The pharmacological management of AS is limited to symptomatic relief, that is, to manage pain and improve joint flexibility, through nonsteroidal anti-inflammatory medications (NSAIDs) and TNF-α inhibitors (Anti-Tumor Necrosis Factor (TNF)- α therapy). 5 The unmet need for management of AS involves improvement in functional disability, pulmonary function, and psychological distress. Nonpharmacological management such as exercise, pilates, and yoga are effectively addressing these factors in the management of AS.8–10
Yoga is a discipline of mind-body practices. It encompasses physical postures, breathing techniques, relaxation techniques, and meditation—it provides numerous health benefit effects in both clinical and nonclinical populations. 11 Yoga practice improves various musculoskeletal problems such as back pain, neck pain, and osteoarthritis.12–14 It is effective in improving spinal flexibility and pain management in chronic low back pain patients. 15 Yoga is effective in various chronic inflammatory conditions, such as multiple sclerosis and rheumatoid arthritis. Yoga practice was found to be associated with a decrease in inflammatory markers.16–18
Yoga is an effective intervention in musculoskeletal disorders by improving range of motion and physical functioning and reducing inflammation by down regulating Nuclear factor kappa β (F-Kβ).19, 20 However, the role of yoga in AS patients has not been studied. The current study was a retrospective analysis intended to understand the efficacy of a short-term integrated approach to yoga therapy rehabilitation program in improving spinal flexibility among patients with AS.
Material and Methods
The study was a retrospective study. Records of patients with AS who visited a residential holistic health center in South India for a two-week yoga retreat between the years 2015 and 2020 were retrieved. The data for patients who stayed less than two weeks, were wheelchair bound, having severe disability, having neurological deficits, and who underwent spinal surgery were omitted. A total of 64 records of AS patients were found; of these, 24 fulfilled the study criteria and the same were considered for the analysis.
Procedure
A total of 65 patients with AS visited the center in this duration. After screening, 24 patients were found to be eligible.
The majority of the cases were male patients (n = 23). All these patients attended a two-week residential yoga intervention. All subjects were informed about the study, and written informed consent was obtained.
Intervention
All patients had received a structural yoga module consisting of sukshmavyayama, breathing practices, asana, and mediation, three sessions in a day (see Table 1). In addition to this, patients also had counseling sessions, devotional sessions, and tuning-to-nature sessions in the evening time every day.
Table 1. Yoga Module.
| S.N. | Practices | Duration |
| Loosening Practices | ||
| 1 | Neck movement (front-back-side bending, twisting, and rotation) | 20 min |
| 2 | Shoulder rotation | |
| 3 | Twisting | |
| 4 | Side bending | |
| 6 | Alternate straight leg raising | |
| 7 | Vertical stretch of the knee | |
| 8 | Vertical stretch of the knee of both legs | |
| 9 | Pavanmuktasana lumbar stretch (single and both legs) | |
| 10 | Dorsal stretch | |
| 11 | Alternate foot knee lumbar stretch | |
| 12 | Side leg raising | |
| 13 | Side lumbar stretch | |
| 14 | Quick relaxation techniques | 3 min |
| 1 | Hands in and out breathing | 10 min |
| 2 | Hands stretch breathing | |
| 3 | Tiger breathing | |
| 4 | Shashankasana breathing on chair | |
| 5 | Lumbar stretch breathing | |
| 6 | Chair suryanamaskara | 5 min |
| Asana | ||
| 1 | Tadasana | 10 min |
| 2 | Ardha Kati Chakrasna | |
| 3 | Ardha Chakrasna | |
| 4 | Marjariyasana (Cat pose) | |
| 5 | Makarasana | |
| 6 | Bhujangasana | |
| 7 | Salabhasana | |
| Pranayama | ||
| 1 | Sectional breathing | 5 min |
| 2 | Nadisuddhi | |
| 3 | Bhramari | |
| 4 | Nadanusandhana | |
| 5 | Deep relaxation technique | 5 min |
Source: Department of Rheumatology, Holistic Health Centre, SVYASA University, Bengaluru.
Assessments
Spine Flexibility
Data of sit-and-reach using a goniometer was considered for spinal flexibility assessment. The maximum length reached (in cm) by the patient on the goniometer was recorded before and after the intervention.
Physiological Measures
Physiological measures such as systolic and diastolic blood pressure, heart rate, and respiratory rate were also noted. Participants were asked to sit in a relaxed pose for 10 min before assessments. The analgesic medication score and symptoms score were analyzed. The number of analgesics dosages of medication required per day was monitored. The symptoms score was calculated by a checklist. Patients rated each symptom such as pain on a 10-poin Likert’s scale with 0 indicating no pain and 10 indicating maximum pain.
Statistical Analysis
Data was presented in mean and standard deviation. The paired sample t-test was used for statistical analysis; a P < .05 was considered to be statistically significant (SPSS version 20 [IBM, New York]).
Results
The majority of the patients were males. 21 The average age of the participants was 38.3 ± 10.5 years. The majority of the patients belonging to the upper-middle class.
The average duration of AS was 6.3 ± 3.2 years. Most of the patients had a private job, 12 and most were graduates 12 (see Table 2).
Table 2. Demographics.
| Average age | 38.3 ± 10.5 |
| Education | Below graduation, 7; Graduation, 12; Postgraduation or above, 6. |
| Employment | Private job, 12; Self-employed, 3; Government employees, 3; Nonfunctioning, 3 |
Changes in Variables
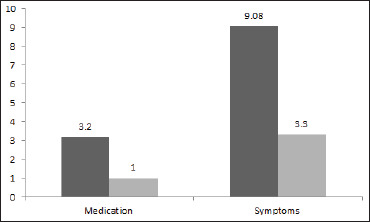
A significant increase (P < .001, 37%) in the sit-and-reach test score measure was observed after two weeks compared to the baseline scores (Figure 1). Analgesic medication requirement and symptoms score also decreased significantly after two weeks compared to the baseline (Table 3; Figure 2).
Figure 1. Significant Increase in the Sit-and-Reach Test Scores Following Yoga.
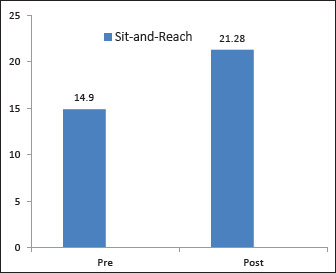
Source: The authors.
Table 3. Represents Baseline and Post-Two-Week Data, % Change, and P-Value of the AS Patients.
| Measures | Pre | Post | % Change in the Mean | t Value | P Value |
| BMI | 24.3 ± 4.5 | 23.9 ± 4.4 | –1.65 | 3.02 | P > .05 |
| HR | 78.05 ± 8.6 | 77.8 ± 6.9 | –0.32 | –0.04 | P > .05 |
| SBP | 123.8 ± 13.3 | 116.1 ± 9.9** | –6.22 | 2.86 | P < .05 |
| DBP | 79 ± 8.3 | 73.4 ± 6.8 | –7.09 | 1.97 | P > .05 |
| Medication | 3.2 ± 4.1 | 1 ± 1.9** | –68.75 | 4.1 | P < .05 |
| Symptoms | 9.08 ± 6.4 | 3.3 ± 3.3** | –63.66 | 4.66 | P < .05 |
| Sit-and-reach | 14.9 ± 7.3 | 21.28 ± 8.1** | 37.5 | –5.9 | P < .001 |
Note: BMI = Body Mass Index, HR = Heart rate, SBP = Systolic Blood pressure, DBP = Diastolic Blood pressure, ** Statistical significance at 0.005 levels, long exhalation time.
Figure 2. Significant Improvement in Medication and Symptom Scores.
Discussion
This retrospective study has shown a promising role of yoga intervention in AS patients. We found significant improvement in lung capacity and spinal flexibility following yoga intervention.
A growing body of literature on yoga indicates the increased use of complementary medicine such as yoga in diverse health-related problems worldwide. 22 Similarly, in this retrospective study, we observed that a significant number of patients with AS (n = 65) had visited centers for alternative therapies. This is suggestive of a patient's positive attitude and hope in alternative therapies such as yoga. This also shows that patients are not 100% satisfied with the current conventional approach of AS management.
No significant change in the SLR test was found, which could be because of short-term intervention. To the best of our knowledge, this is the first study to report the role of yoga in AS. Previously, a study by Lee et al. (2008) found significant improvement in Bath Ankylosing Spondylitis Disease Activity Index following eight weeks of Tai chi intervention (60 min, twice a week). 21 Tai chi is also an alternative medicine shown to have a positive impact on AS.
In our study, there was an improvement in the sit-and-reach. The breath-holding time of the AS patients suggests that yoga can improve the physical functioning and respiratory functions of patients with AS. Previous reports have indicated that patients have an increase in chest wall resistance and a decrease in chest wall compliance.1, 23 Therapies such as inspiratory muscle training, aerobic training, and stretching are given to patients with AS to improve respiratory functions.24–26 Our study did not have any respiratory function test, but there was an improvement in long exhalation time, which is suggestive of a possible chance of improvement in the respiratory function tests.
We also observed a 37.5% improvement in the sit-and-reach test of AS patients after nine days of integrated approach to yoga therapy intervention. Sit-and-reach tests examine the shortening of hamstrings and the lumbar hyperextension. AS patients report stiffening and pain of the lower back often and are prone to have fractures and ligamentous injuries in the lumbosacral region of the spine. 27 Our study suggests an improvement in the flexibility and functional status of these patients.
Possible mechanisms involved in improving spinal flexibility and lung function following yoga could be attributed to a decrease in the pain, inflammation, and stress through modulation in pain sensitivity and HPA axis. 28
As per the authors’ knowledge, our trial is the first study to report the effect of yoga on functional status and breath-holding in AS patients. There were several limitations in the trial including the retrospective prepost design, smaller sample size, no randomization, and no objective parameters. There is a need for a larger randomized controlled trial with more specific parameters to assess the effectiveness of yoga as a rehabilitative tool for patients suffering from AS. The authors would like to report a well-designed randomized controlled trial to evaluate the efficacy of yoga on quality of life and inflammatory markers among AS patients. The study is ethically approved, and a clinical trial registration is awaited, after which the trial will be initiated in India. The study is expected to be initiated by April 2020 and completed by June 2022.
Conclusion
This retrospective study indicates the promising role of yoga intervention in patients with AS. This study suggests that yoga may help in improving spinal flexibility and lung function in AS patients. Further, we recommend the scope of randomized controlled trials in yoga and AS using objective measures.
Acknowledgments
The authors gratefully acknowledge Dr K. S. Nibedita, Dr Monika Jha and the staff of Arogyadhama for their support in the study.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
ORCID iD: Kashinath G. Metri  https://orcid.org/0000-0001-7928-4840
https://orcid.org/0000-0001-7928-4840
Ethical Statement
The study was approved by the “Ethics committee of SVYASA University, Bengaluru.”
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Braun J and Sieper J.. Ankylosing spondylitis. Lancet [Internet]2007. April; 369(9570): 1379–1390. https://linkinghub.elsevier.com/retrieve/pii/S0140673607606357 [DOI] [PubMed] [Google Scholar]
- 2.Akkoc N. Are spondyloarthropathies as common as rheumatoid arthritis worldwide? A review. Curr Rheumatol Rep [Internet] 2008 October 16; 10(5): 371–378. http://link.springer.com/10.1007/s11926-008-0060-3 [DOI] [PubMed] [Google Scholar]
- 3.Boonen A. Withdrawal from labour force due to work disability in patients with ankylosing spondylitis. Ann Rheum Dis [Internet] 2001 November 1; 60(11): 1033–1039. http://ard.bmj.com/cgi/doi/10.1136/ard.60.11.1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barlow JH, Wright CC, Williams B, et al. Work disability among people with ankylosing spondylitis. Arthritis Rheum [Internet] 2001 October; 45(5): 424–429. [DOI] [PubMed] [Google Scholar]
- 5.Zhu W, He X, Cheng K. et al. Ankylosing spondylitis: Etiology, pathogenesis, and treatments. Bone Res [Internet] 2019 December 5; 7(1): 22. http://www.nature.com/articles/s41413-019-0057-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wallis D, Thavaneswaran A, Haroon N, et al. FRI0441 Infection risk in ankylosing spondylitis: results from a longitudinal observational cohort. Annals of the Rheumatic Diseases 2013;72:A524 [Google Scholar]
- 7.Zambrano-Zaragoza JF, Agraz-Cibrian JM, González-Reyes C, et al. Ankylosing spondylitis: From cells to genes. Int J Inflamm 2013; 2013: 1–16. http://www.hindawi.com/journals/iji/2013/501653/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crow EM, Jeannot E, Trewhela A.. Effectiveness of Iyengar yoga in treating spinal (back and neck) pain: A systematic review. Int J Yoga 2015. January; 8(1): 3. http://www.ijoy.org.in/text.asp?2015/8/1/3/146046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pécourneau V, Degboé Y, Barnetche T, et al. Effectiveness of exercise programs in ankylosing spondylitis: A meta-analysis of randomized controlled trials. Arch Phys Med Rehabil 2018 February; 99(2): 383–389.e1. https://linkinghub.elsevier.com/retrieve/pii/S0003999317310195 [DOI] [PubMed] [Google Scholar]
- 10.Altan L, Korkmaz N, Dizdar M, et al. Effect of pilates training on people with ankylosing spondylitis. Rheumatol Int 2012. July 17; 32(7): 2093–2099. http://link.springer.com/10.1007/s00296-011-1932-9 [DOI] [PubMed] [Google Scholar]
- 11.Ward L, Stebbings S, Sherman KJ, et al. Establishing key components of yoga interventions for musculoskeletal conditions: a Delphi survey. BMC Complement Altern Med 2014. December 18; 14(1): 196. https://bmccomplementalternmed.biomedcentral.com/articles/10.1186/1472-6882-14-196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cramer H, Klose P, Brinkhaus B, et al. Effects of yoga on chronic neck pain: A systematic review and meta-analysis. Clin Rehabil 2017. November; 31(11): 1457–1465. [DOI] [PubMed] [Google Scholar]
- 13.Tilbrook HE, Cox H, Hewitt CE, et al. Yoga for chronic low back pain: A randomized trial. Ann Intern Med 2011. Nov 1; 155(9): 569–578. [DOI] [PubMed] [Google Scholar]
- 14.Cheung C, Wyman JF, Resnick B, Savik K. Yoga for managing knee osteoarthritis in older women: a pilot randomized controlled trial. BMC complementary and alternative medicine. 2014. Dec;14(1):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tekur P, Singphow C, Nagendra HR, et al. Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: A randomized control study. J Altern Complement Med 2008. July 1; 14(6): 637–644. [DOI] [PubMed] [Google Scholar]
- 16.Yadav RK, Magan D, Mehta N, et al. Efficacy of a short-term yoga-based lifestyle intervention in reducing stress and inflammation: Preliminary results. J Altern Complement Med 2012. July 1; 18(7): 662–667. [DOI] [PubMed] [Google Scholar]
- 17.Oken BS, Kishiyama S, Zajdel D, et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology 2004. June 8; 62(11): 2058–2064. [DOI] [PubMed] [Google Scholar]
- 18.Evans S, Moieni M, Lung K, Tsao J, Sternlieb B, Taylor M, Zeltzer L. Impact of iyengar yoga on quality of life in young women with rheumatoid arthritis. The Clinical journal of pain. 2013. Nov;29(11):988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sarvottam K and Yadav RK.. Obesity-related inflammation & cardiovascular disease: Efficacy of a yoga-based lifestyle intervention. Indian J Med Res [Internet] 2014. June; 139(6): 822–834. http://www.ncbi.nlm.nih.gov/pubmed/25109716 [PMC free article] [PubMed] [Google Scholar]
- 20.Akyuz G and Kenis-Coskun O.. The efficacy of Tai chi and yoga in rheumatoid arthritis and spondyloarthropathies: A narrative biomedical review. Rheumatol Int 2018. March 4; 38(3): 321–330. http://link.springer.com/10.1007/s00296-017-3867-2 [DOI] [PubMed] [Google Scholar]
- 21.Ünlü E, ÖN Pamuk, Erer B, et al. Diaphragmatic movements in ankylosing spondylitis patients and their association with clinical factors: An ultrasonographic study. Rheumatol Int [Internet] 2012. February 1; 32(2):435–437. http://link.springer.com/10.1007/s00296-010-1657-1 [DOI] [PubMed] [Google Scholar]
- 22.E-N Lee, Y-H Kim, Chung WT, Lee MS.. Tai chi for disease activity and flexibility in patients with ankylosing spondylitis—A controlled clinical trial. Evid Based Complement Alternat Med [Internet] 2008; 5(4): 457–462. http://www.hindawi.com/journals/ecam/2008/345969/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gyurcsik Z, Bodnár N, Szekanecz Z, et al. Treatment of ankylosing spondylitis with biologics and targeted physical therapy. Z Rheumatol [Internet] 2013. December 10; 72(10): 997–1004. http://link.springer.com/10.1007/s00393-013-1240-8 [DOI] [PubMed] [Google Scholar]
- 24.Aytekin E, Caglar NS, Ozgonenel L, et al. Home-based exercise therapy in patients with ankylosing spondylitis: effects on pain, mobility, disease activity, quality of life, and respiratory functions. Clin Rheumatol [Internet] 2012. January 10; 31(1): 91–97. http://link.springer.com/10.1007/s10067-011-1791-5 [DOI] [PubMed] [Google Scholar]
- 25.Wong ML, Anderson RG, Garcia K, et al. The effect of inspiratory muscle training on respiratory variables in a patient with ankylosing spondylitis: A case report. Physiother Theory Pract [Internet] 2017. October 3; 33(10): 805–814. https://www.tandfonline.com/doi/full/10.1080/09593985.2017.1346023 [DOI] [PubMed] [Google Scholar]
- 26.Rustagi T, Drazin D, Oner C, et al. Fractures in spinal ankylosing disorders. J Orthop Trauma [Internet] 2017. September; 31: S57–S74. http://insights.ovid.com/crossref?an=00005131-201709004-00009 [DOI] [PubMed]
- 27.Vera FM, Manzaneque JM, Maldonado EF, et al. Subjective sleep quality and hormonal modulation in long-term yoga practitioners. Biol Psychol [Internet] 2009. July; 81(3): 164–168. https://linkinghub.elsevier.com/retrieve/pii/S0301051109000726 [DOI] [PubMed] [Google Scholar]
- 28.Sarubin N, Nothdurfter C, Schüle C, et al. The influence of Hatha yoga as an add-on treatment in major depression on hypothalamic–pituitary–adrenal-axis activity: A randomized trial. J Psychiatr Res 2014. June 1; 53: 76–83. https://www.sciencedirect.com/science/article/abs/pii/S002239561400072 [DOI] [PubMed] [Google Scholar]


