Abstract
Background:
Poor muscle strength, balance, and functional mobility have predicted falls in older adults. Fall prevention guidelines recommend highly challenging balance training modes to decrease falls; however, it is unclear whether certain modes are more effective. The purpose of this study was to determine whether traditional balance training (BT), virtual reality balance training (VR), or combined exercise (MIX) relative to a waitlist control group (CON) would provoke greater improvements in strength, balance, and functional mobility as falls risk factor proxies for falls in older men.
Hypothesis:
We hypothesized that 8 weeks of MIX will provoke the greatest improvements in falls risk factors, followed by similar improvements after BT and VR, relative to the CON.
Study Design:
Single-blinded randomized controlled trial NCT02778841 (ClinicalTrials.gov identifier).
Level of Evidence:
Level 2.
Methods:
In total, 64 community-dwelling older men (age 71.8 ± 6.09 years) were randomly assigned into BT, VR, MIX, and CON groups and tested at baseline and at the 8-week follow-up. The training groups exercised for 40 minutes, 3 times per week, for 8 weeks. Isokinetic quadriceps and hamstrings strength on the dominant and nondominant legs were primary outcomes measured by the Biodex Isokinetic Dynamometer. Secondary outcomes included 1-legged stance on firm and foam surfaces, tandem stance, the timed-up-and-go, and gait speed. Separate one-way analyses of covariance between groups were conducted for each outcome using baseline scores as covariates.
Results:
(1) MIX elicited greater improvements in strength, balance, and functional mobility relative to BT, VR, and CON; (2) VR exhibited better balance and functional mobility relative to BT and CON; and (3) BT demonstrated better balance and functional mobility relative to CON.
Conclusion:
The moderate to large effect sizes in strength and large effect sizes for balance and functional mobility underline that MIX is an effective method to improve falls risk among older adults.
Clinical Relevance:
This study forms the basis for a larger trial powered for falls.
Keywords: older adults, muscle strength, balance, functional mobility, exercise, exergame
Lower limb muscle strength, balance, and functional mobility are commonly occurring modifiable falls risk factors that are interrelated. 18 Deficits in 1 or more of these falls risk factors can have serious implications for older adults, such as increased risk for falls and fall-related injuries, greater dependency on others, diminished quality of life, and an increased likelihood of hospital stays.6,12,50,55 For these reasons, multiple risk factors should be collected to better capture falls risk. 22 Age-related changes to muscle strength, balance, and functional mobility highlight the importance for interventions targeted at mitigating these deficits.
The most recent guidelines on fall prevention practice in community-dwelling older adults recommend exercise training modes that are highly challenging to balance, can include resistance training as an option in addition to balance training, and do not include brisk walking programs for high-risk older adults. 52 While traditional balance training (BT)2,21,23,26,51 and virtual reality balance training (VR)48,49,58 are both challenging to balance and have improved strength, balance, and functional mobility, research is mixed in terms of whether one training mode is more beneficial than the other in improving falls risk.1,19,28,38 Furthermore, few studies have compared the effects of combined BT and VR (ie, MIX) among older adults, and their influence on falls risk is conflicting.3,30,57 For instance, one pilot study (n = 18) has shown greater improvements in postural sway during the bubble test after MIX (43%), followed by BT (25%), followed by VR (10%). 3 Another study revealed that dynamic balance improved in the BT as well as MIX groups, but not the VR group (n = 36). 57 More recently, complex exercise consisting of strength, flexibility, and endurance exercise plus VR revealed more improvements in knee extension peak torque and dynamic balance relative to VR alone in older adults (n = 20). 30 Altogether, BT, VR, and MIX are challenging balance programs; however, the literature is inconclusive on which program provides the greatest improvement to falls risk factors in older adults because of inconsistent findings as well as small sample sizes (n = 18-36).3,30,57
We therefore conducted a single-blinded randomized controlled trial to determine whether BT, VR, or MIX relative to a waitlist control group (CON) would provoke greater improvements in knee flexion and extension strength, balance, and functional mobility as falls risk factor proxies for falls in older men. Based on previous research, we hypothesized that MIX would elicit the greatest improvements in lower body muscle strength, balance, and functional mobility, with similar improvements after BT and VR, and no improvements in the CON group.
Methods
Study Design, Trial Registration, and Ethics
The Consolidated Standards of Reporting Trials (CONSORT) guidelines were followed to ensure a high quality of reporting. All participants provided written informed consent approved by the Shiraz University of Medical Sciences and the Universiti Putra Malaysia. This was a single-blinded randomized controlled trial registered on clinicaltrials.gov (NCT02778841). A total of 64 participants drew lots out of a hat and were randomly assigned into 4 parallel groups (BT, VR, MIX, CON).
Sample Size Calculation
The sample size estimation was determined a priori using G*Power (Version 3.1.6). Assuming an effect size of 0.23 with an alpha level of 0.05 using a group effect on change in muscle strength as our primary outcome measure, 30 14 participants were required per group with 80% power. Accounting for a dropout rate of 15%, 16 participants were recruited per group, totaling 64 older adults across the 4 groups.
Participants
Participants were recruited via announcements at a local men’s retirement community center. The inclusion criteria consisted of men aged 65 years and older, the ability to walk 10 m independently, the ability to perform daily activities independently, and no experience with BT or VR in the past 6 months. Considering the cultural restrictions of men and women being required to exercise separately, only older men participated in this study because of financial restrictions in hiring trainers. Exclusion criteria consisted of neurological, cognitive, or cardiovascular complications, fractures, and joint replacements of the lower extremity.
Procedures
At the baseline testing session, participants completed a health questionnaire, including medications, diseases, illnesses, and previous surgeries. The study physician went through the Physical Activity Readiness Questionnaire with participants; all participants were cleared for exercise. Participants were tested at baseline and at 8 weeks on the following outcome measures: isokinetic muscle strength, single-leg stance on firm and foam surfaces, tandem stance, the timed-up-and-go test (TUG), and the 10-m walk test (10mWT), as described below.
Primary Outcome Measure
Our primary outcome measure was isokinetic muscle strength. Muscle strength is a measure of falls risk and has predicted falls and recurrent falls in older adults.16,31 Isokinetic muscle strength of lower limbs was quantified by means of the Biodex Isokinetic Dynamometer (Biodex System 3). Participants sat on the Biodex Isokinetic Dynamometer and were strapped across the pelvis, trunk, chest, hips, and thighs. The lever arm of the dynamometer was strapped to the shank superior to the lateral malleolus, while the rotational axis of the dynamometer was aligned with the lateral epicondyle of the femur. Adjustments to the seat height and attachment length depended on the participants’ measurements and were based on the guidelines of the isokinetic machine. 4 Before commencing the test, participants completed a 10-minute warm-up session, including the following: walking down the hallway at a fast pace (heart rate <100 beats/min), 27 static and dynamic lower body stretching, and 3 practice trials on the Biodex Isokinetic Dynamometer. The experimental protocol on the Biodex Isokinetic Dynamometer involved participants performing 3 sets of maximum concentric contractions of the quadriceps and hamstring muscles. Peak torques of flexion and extension of the knee were measured at a speed of 120 deg/s. 30 Test-retest reliability and criterion validity up to 300 deg/s of the Biodex system have been previously established. 13 A cutoff of 1.40 N·m/kg for knee extensor isokinetic strength relative to body weight has been reported in older adults. 40 Dynamometers have been shown to have better standardization, more accurate continuous measurement of torque and velocity, and reduced muscle soreness relative to weight stack machines. 54
Balance Tests
Single-Leg Stance Test on Firm and Foam Surfaces
Participants were asked to stand on 1 leg with eyes open on firm and foam surfaces for as long as possible; the time in seconds was recorded using a stopwatch. Participants completed 3 trials on each leg, and a mean score was calculated for each leg. Rest was permitted between each trial. The test was terminated when (1) the raised foot touched the stance leg or the floor, (2) the participant hopped, and (3) the arm touched a support surface or the investigator. The dominant leg was indicated by the preferred foot when kicking a ball. 10 This test has shown excellent test-retest reliability among healthy older adults, 14 and predictive validity in older adults with Parkinson disease. 20 A cutoff of <10 seconds has discriminated between fallers and nonfallers with Parkinson disease. 20
Tandem Stance Test
Participants placed their feet in tandem stance (ie, heel-to-toe) and held this position for as long as possible. The test was terminated when 1 foot shifted out of position or the arm touched a support surface or the investigator. The mean time to hold the stance was calculated from the 3 trials. This test has shown high construct validity 8 and good test-retest reliability. 34 A cutoff of <10 seconds has been a marker of poor balance in community-dwelling older adults. 59
Functional Mobility Tests
Timed-Up-and-Go Test
The TUG test involved participants’ getting up from a chair, walking 3 meters at a comfortable speed, turning around, walking back to the chair, and sitting down. 45 The time in seconds was recorded between when the examiner verbalized “go” and when the participant’s back touched the backrest of the chair. The average of the 2 experimental trials was used in the analysis. The test has shown high inter- and intrarater reliability, 53 as well as discriminative validity in community-dwelling and institutionalized older adults. 5 A clinical cutoff of ≤12 seconds has been a recognized threshold for normal TUG performance in community-dwelling older adults. 5
Ten-Meter Walk Test
For the 10mWT, participants walked 14 meters at a comfortable pace, and the time in seconds to walk the middle 10 meters of the walkway was recorded. 43 The average gait speed (m/s) of the 2 experimental trials was used in the analysis. The 10mWT has shown excellent test-retest reliability 43 and predictive validity in older adults. 36 Slow gait speed has been characterized as <0.7 m/s, moderate gait speed 0.7 to 1.0 m/s, and fast gait speed >1.1 m/s in community-dwelling older adults. 36
Intervention
The group exercise sessions were facilitated by 3 certified trainers and supervised by a researcher who was not involved in testing (ie, 4:1 participant to trainer ratio). All researchers involved in testing were blinded to group allocation. Participants in the training programs exercised for 40 minutes, 3 times per week, for 8 weeks. Each session was divided into 3 phases: a 5-minute warm-up, 30 minutes of intervention training, and a 5-minute cool-down (40 minutes total). The warm-up and cool-down phases involved slow walking plus static and dynamic stretches with a concentration on the lower limbs, such as calves, hamstrings, quadriceps, tensor fasciae latae, and gluteal muscles. All training programs were individualized and progressive. The Borg Rating of Perceived Exertion (RPE) scale was used to gauge intensity during exercise sessions. The RPE consists of a scale of 6 (no exertion at all) to 20 (maximal exertion). 42 Participants were asked to exercise at a RPE of between 13 and 14 (somewhat hard) and RPE 15 and 16 (hard), 42 and reflected approximately 70% to 80% of VO2 max. 24
Balance Training
BT included exercises such as a single-leg stance with eyes open and closed, standing on heels or toes, tandem and semitandem foot stance, tandem walking, walking backward and forward, and weight shifting. An exercise familiarization session was carried out before the commencement of the training, which involved 1 to 2 sets of 6 to 8 repetitions of each of the exercises. As participants improved, they were progressed by increasing the time to hold balance positions, increasing the number of repetitions, and/or increasing the number of sets.
VR Exercise
Based on the pilot intervention, we selected 3 games that challenged lower body balance: (1) The Light Race (Stomp It) mini-game from the Your Shape fitness package, (2) the Target Kick, and (3) Goalkeeper mini-games from the Sport Xbox Kinect game package. 47 Three consoles were used during the VR sessions; thus, the 4 participants in each group session rotated between the game consoles as well as a break station. An exercise familiarization session was carried out before the commencement of the training, which involved playing each of the 3 games twice. As participants improved, they were progressed by an increase in the difficulty of the VR games.
Mixed Exercise
The MIX group performed the 5-minute warm-up, 15 minutes of BT exercise, 15 minutes of VR exercise, and the 5-minute cool-down 3 times per week for 8 weeks. The MIX group completed BT and VR familiarization, as described above.
Control Group
Participants in the CON were asked to continue with their daily activities and avoid starting new exercise programs during the study period. After the study completion, they were invited to participate in the program of their choice for 8 weeks.
Adherence and Attrition
The trainers kept track of adherence and attrition with the use of logbooks. The mean number of sessions attended out of a total of 24 sessions and adherence rate were calculated.
Changes to Clinical Trial Methods
The hamstring and quadriceps muscles strength tests were added to the methods after clinical trial registration and muscle strength was made the primary outcome measure.
Statistical Analysis
Separate 1-way analysis of covariance (ANCOVA) across 4 groups (VR vs BT vs MIX vs CON) were conducted for quadriceps and hamstring strength on the dominant and nondominant sides, single-leg stance on the dominant and nondominant legs on firm and foam surfaces, tandem stance, the TUG, and gait speed using these baseline variables as covariates. Our a priori analyses were based on previous recommendations to control for pretest scores using a 1-way ANCOVA to account for possible differences between groups at baseline. 39 When applicable, follow-up Bonferroni post hoc tests were conducted. To compare within-group (pre- and posttest) differences, paired-samples t tests were conducted. The effect sizes of each variable were tested using partial eta squared (η2) and omega squared (ω2) values (small effect = 0.01, medium effect = 0.06, and large effect = 0.14). 9 The α level was set to 0.05. In addition, 1-way analyses of variance were conducted on baseline scores across groups.
Results
Participant Characteristics, Attrition, Adherence, and Adverse Events
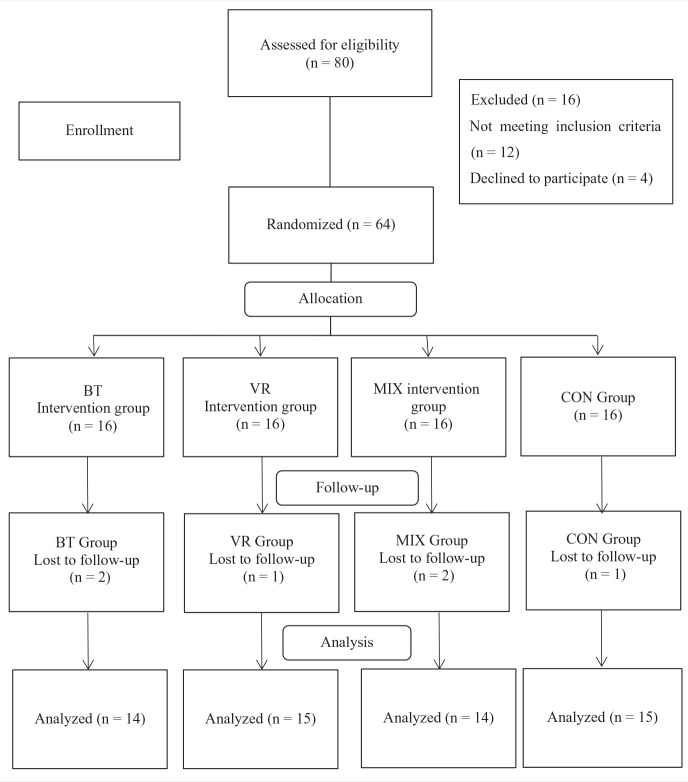
Participant characteristics are reported in Table 1. Of the 64 participants in the randomized controlled trial, 2 participants were lost to follow-up in the BT group (n = 2: traveling), 1 participant was lost to follow-up in the VR group (n = 1: car accident), 2 participants were lost to follow-up in the MIX group (n = 1: traveling, n = 1: disinterest), and 1 participant was lost to follow-up in the CON group (n = 1: sick). The attrition rates of BT and MIX groups were 12.5% and CON and VR groups were 6.25%. The final number of participants was 58 (Figure 1).
Table 1.
Anthropometric variables of participants between groups (mean ± SD)
| Variables | BT (n = 14) | VR (n = 15) | MIX (n = 14) | CON (n = 15) |
|---|---|---|---|---|
| Age, y | 70.4 ± 4.3 | 74.1 ± 7.0 | 70.5 ± 5.1 | 72.2 ± 7.2 |
| Weight, kg | 71.6 ± 7.5 | 68.7 ± 8.7 | 70.7 ± 11.6 | 66.5 ± 10.5 |
| Height, cm | 167.5 ± 8.1 | 166.8 ± 5.1 | 166.0 ± 6.9 | 167.2 ± 5.6 |
| BMI, kg/m2 | 25.5 ± 2.4 | 24.7 ± 2.7 | 25.6 ± 3.5 | 23.7 ± 2.7 |
BMI, body mass index; BT, balance training group; CON, control group; MIX, mixed group; VR, virtual reality group.
Figure 1.
Flowchart of participant recruitment, adherence, and attrition. BT, balance training group; CON, control group; MIX, mixed group; VR, virtual reality group.
In terms of adherence to the training programs, the BT group attended 21.1 ± 0.35 sessions (87.9%), the VR group attended 21.7 ± 0.75 sessions (90.4%), and the MIX group attended 22.1 ± 0.70 sessions (92.1%) out of a total 24 sessions in the program. All participants in the training groups attended at least 80% of their exercise classes. No adverse events occurred during or outside of the training sessions.
Between-Group Comparisons on Strength, Balance, and Functional Mobility
After the intervention period, ANCOVA analyses revealed a main effect of group for quadriceps strength in the dominant (F(3, 59) = 10.60; P = 0.001; η2 = 0.35; ω2 = 0.12), and nondominant legs (F(3, 59) = 10.87; P = 0.001; η2 = 0.36; ω2 = 0.19), as well as hamstring strength in the dominant (F(3, 59) = 4.36; P = 0.01; η2 = 0.18; ω2 = 0.13), and nondominant legs (F(3, 59) = 3.00; P = 0.04; η2 = 0.13; ω2 = 0.05). Follow-up Bonferroni post hoc tests revealed group differences, as shown in Appendix Table A1 (available in the online version of this article).
ANCOVA analyses showed a significant main effect of group for the single leg stance test on firm surface for the dominant (F(3, 59) = 125.44; P < 0.001; η2 = 0.87; ω2 = 0.72), and nondominant legs (F(3, 53) = 101.81; P < 0.001; η2 = 0.85; ω2 = 0.67). Follow-up post hoc tests between groups are reported in Appendix Table A2 (available online). For the single-leg stance test on foam surface, a main effect of group was exhibited for the dominant (F(3, 59) = 9.97; P = 0.001; η2 = 0.34; ω2 = 0.21) and nondominant legs (F(3, 59) = 17.39; P = 0.001; η2 = 0.47; ω2 = 0.31). Follow-up post hoc tests display between-group differences in Appendix Table A3 (available online). For the tandem balance test, a main effect of group emerged (F(3, 59) = 26.22; P = 0.001; η2 = 0.57; ω2 = 0.44). Follow-up post hoc tests between groups are shown in Appendix Table A4 (available online).
A significant main effect of group was observed for the TUG (F(3, 53) = 103.64; P = 0.001; η2 = 0.85; ω2 = 0.73), and gait speed (F(3, 53) = 244.68; P < 0.001; η2 = 0.93; ω2 = 0.89). The Bonferroni post hoc tests displayed group differences in Appendix Table A5 (available online).
Within-Group Comparisons on Strength, Balance, and Functional Mobility
Within-group paired-samples t tests for the strength, balance, and functional mobility measures are reported in Appendix A1 (available online). Mean differences between the pre- and posttests across measures for each group are reported in Appendix Tables A1 to A5 (available online).
Baseline Comparisons on Strength, Balance, and Functional Mobility Across Groups
Appendix A2 (available online) reports the baseline comparisons between groups across outcome measures.
Discussion
Main Findings
This is the first randomized controlled trial powered to examine the influence of BT, VR, MIX, and CON on the primary outcome of leg strength and secondary outcomes of balance and functional mobility in older men. The main findings of this study were that (1) the MIX group showed the greatest improvements in strength, balance, and functional mobility relative to the BT, VR, and CON groups; (2) the VR group exhibited better balance and functional mobility relative to the BT and CON groups; and (3) the BT group exhibited better balance and functional mobility relative to the CON group.
The moderate to large effect sizes in strength, and large effect sizes for balance and functional mobility, underline that MIX is an effective method to improve falls risk factors among older adults. 9 Minimal clinically important improvements in the balance and functional mobility measures have been reported to be 8.7 seconds for the single-leg stance time, 17 −0.8 ± 0.5 seconds for the TUG, 56 and 0.06 m/s for gait speed 41 in older adults; no known meaningful improvements have been established for muscle strength 11 or tandem stance 41 in older adults. Importantly, while all experimental groups exhibited clinically meaningful improvements in balance and functional mobility relative to the CON, the MIX group exhibited clinically meaningful improvements in these measures above and beyond the VR and BT groups. Our results extend previous pilot studies3,30,57 to highlight the importance of combined exercise to improve falls risk factors among older males.
The mechanisms provoking improvements in falls risk factors after BT and VR may have been different, and combining these training types may have elicited synergistic effects. Our BT program involved static (eg, standing on 1 leg) and dynamic balance (eg, walking forward and backward), while our VR program involved standing and stepping in place while performing high speed hand-eye and foot-eye coordination tasks, head movements, jumping, crouching, and reaching.1,7,15,25,29 The BT and VR programs may have improved muscle strength to a similar extent, as there were no strength differences between these groups. Both BT and VR required information processing from visual, auditory, and somatosensory systems 32 ; however, VR may have required greater sensory integration, as it provided biofeedback.1,33 Both BT and VR required planning and decision-making processes, but VR also required greater inhibitory control and episodic memory. 32 Therefore, VR may have afforded a greater challenge to balance, required greater sensory integration, and added a higher cognitive demand than BT1,7,15,19,25,29,32,33; this may explain the greater improvements in balance and functional mobility shown in the VR group relative to the BT group. Nevertheless, while the fast exergame movements have shown benefits to larger muscle groups, the smaller antagonist muscles may be exposed to greater peripheral neuromuscular fatigue.35,46 Because the MIX group completed half BT and half VR, they likely did not experience preemptive fatigue of small muscle groups. Altogether, the MIX group likely benefited from both mechanisms of improvement, which likely resulted in additional gains in strength, balance, and functional mobility than BT or VR alone.
Adherence and Attrition
The training programs were feasible, with the BT group adhering to 87.9%, the VR group adhering to 90.4%, and the MIX group adhering to 92.1% of the program. This is higher than the reported average of 75% for fall prevention intervention protocols. 37 The median attrition rate for interventions has been reported to be 16.2% from baseline to the posttest, 44 which is higher than our attrition rates across groups (range, 6.3%-12.5%).
Implications
Current guidelines on fall prevention suggest highly challenging balance exercise to reduce falls. 52 BT, VR, and MIX were all challenging to balance. Our results extend the current guidelines to suggest that MIX provokes the greatest improvement in lower limb muscle strength, balance, and functional mobility in older males, relative to VR, BT, and CON. This is particularly important in light of the limited health care resources and increasing emphasis on preventive care in both the home and the community. 16 MIX is a safe program, had excellent adherence, and low attrition and can be readily implemented in the community to reduce falls risk in older adults. This study forms the basis for a larger trial powered for falls to be conducted.
Limitations
This study has several limitations. First, the results of this study can only be generalized to community-dwelling older men. We did not have an additional follow-up assessment after the posttest; therefore, it is uncertain whether the intervention groups sustained their improvements over time.
Conclusion
Eight weeks of MIX, VR, and BT resulted in improvements in leg strength, balance, and functional mobility relative to CON, but MIX elicited clinically meaningful improvements above and beyond the other intervention groups. These findings have important implications for the design of future interventions targeting improving strength, balance, and functional mobility fall-risk factors among older adults.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_1941738120986803 for Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial by Hassan Sadeghi, Deborah A. Jehu, Abdolhamid Daneshjoo, Elham Shakoor, Mohsen Razeghi, Alireza Amani, Muhammad Nazrul Hakim and Ashril Yusof in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-2-sph-10.1177_1941738120986803 for Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial by Hassan Sadeghi, Deborah A. Jehu, Abdolhamid Daneshjoo, Elham Shakoor, Mohsen Razeghi, Alireza Amani, Muhammad Nazrul Hakim and Ashril Yusof in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-3-sph-10.1177_1941738120986803 for Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial by Hassan Sadeghi, Deborah A. Jehu, Abdolhamid Daneshjoo, Elham Shakoor, Mohsen Razeghi, Alireza Amani, Muhammad Nazrul Hakim and Ashril Yusof in Sports Health: A Multidisciplinary Approach
Footnotes
The following author declared potential conflicts of interest: D.A.J. is a funded postdoctoral fellow through the Michael Smith Foundation for Health Research. This work was supported by the University of Putra Malaysia.
References
- 1. Bacha JMR, Gomes GCV, de Freitas TB, et al. Effects of Kinect adventures games versus conventional physical therapy on postural control in elderly people: a randomized controlled trial. Games Health J. 2018;7:24-36. [DOI] [PubMed] [Google Scholar]
- 2. Barnett A, Smith B, Lord SR, Williams M, Baumand A. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing. 2003;32:407-414. [DOI] [PubMed] [Google Scholar]
- 3. Bateni H. Changes in balance in older adults based on use of physical therapy vs the Wii Fit gaming system: a preliminary study. Physiotherapy. 2012;98:211-216. [DOI] [PubMed] [Google Scholar]
- 4. Biodex Medical Systems I. BIODEX Multi-Joint System-Pro setup/operation manual. Biodex Medical System; 2007. [Google Scholar]
- 5. Bischoff HA, Stähelin HB, Monsch AU, et al. Identifying a cut-off point for normal mobility: a comparison of the timed “up and go” test in community-dwelling and institutionalised elderly women. Age Ageing. 2003;32:315-320. [DOI] [PubMed] [Google Scholar]
- 6. Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52:1263-1270. [DOI] [PubMed] [Google Scholar]
- 7. Chen PY, Wei SH, Hsieh WL, Cheen JR, Chen LK, Kao CL. Lower limb power rehabilitation (LLPR) using interactive video game for improvement of balance function in older people. Arch Gerontol Geriatr. 2012;55:677-682. [DOI] [PubMed] [Google Scholar]
- 8. Cho BL, Scarpace D, Alexander NB. Tests of stepping as indicators of mobility, balance, and fall risk in balance-impaired older adults. J Am Geriatr Soc. 2004;52:1168-1173. [DOI] [PubMed] [Google Scholar]
- 9. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Lawrence Erlbaum Press; 1988. [Google Scholar]
- 10. Daneshjoo A, Mokhtar AH, Rahnama N, Yusof A. The effects of comprehensive warm-up programs on proprioception, static and dynamic balance on male soccer players. PLoS One. 2012;7:e51568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. De Brandt J, Spruit MA, Hansen D, et al. Changes in lower limb muscle function and muscle mass following exercise-based interventions in patients with chronic obstructive pulmonary disease: a review of the English-language literature. Chron Respir Dis. 2018;15:182-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658-668. [DOI] [PubMed] [Google Scholar]
- 13. Drouin JM, Valovich-McLeod TC, Shultz SJ, Gansneder BM, Perrin DH. Reliability and validity of the Biodex System 3 Pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol. 2004;91:22-29. [DOI] [PubMed] [Google Scholar]
- 14. Franchignoni F, Tesio L, Martino M, Ricupero C. Reliability of four simple, quantitative tests of balance and mobility in healthy elderly females. Aging Clin Exp Res. 1998;10:26-31. [DOI] [PubMed] [Google Scholar]
- 15. Fu AS, Gao KL, Tung AK, Tsang WW, Kwan MM. Effectiveness of exergaming training in reducing risk and incidence of falls in frail older adults with a history of falls. Arch Phys Med Rehabil. 2015;96:2096-2102. [DOI] [PubMed] [Google Scholar]
- 16. Garcia PA, Dias JMD, Azevedo da Silva SL, Dias RC. Identification of clinical and functional falls risk factors among low bone density older women. Top Geriatr Rehabil. 2016;32:134-143. [Google Scholar]
- 17. Goldberg A, Casby A, Wasielewski M. Minimum detectable change for single-leg-stance-time in older adults. Gait Posture. 2011;33:737-739. [DOI] [PubMed] [Google Scholar]
- 18. Hamacher D, Liebl D, Hödl C, et al. Gait stability and its influencing factors in older adults. Front Physiol. 2019;9:1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hung J-W, Chou C-X, Hsieh Y-W, et al. Randomized comparison trial of balance training by using exergaming and conventional weight-shift therapy in patients with chronic stroke. Arch Phys Med Rehabil. 2014;95:1629-1637. [DOI] [PubMed] [Google Scholar]
- 20. Jacobs J, Horak FB, Tran V, Nutt J. Multiple balance tests improve the assessment of postural stability in subjects with Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2006;77:322-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jehu D, Paquet N, Lajoie Y. Balance and mobility training with or without concurrent cognitive training does not improve posture, but improves reaction time in healthy older adults. Gait Posture. 2017;52:227-232. [DOI] [PubMed] [Google Scholar]
- 22. Jehu DA, Davis JC, Liu-Ambrose T. Risk factors for recurrent falls in older adults: a study protocol for a systematic review with meta-analysis. BMJ Open. 2020;10:e033602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jehu DA, Paquet N, Lajoie Y. Balance and mobility training with or without concurrent cognitive training improves the timed up and go (TUG), TUG cognitive, and TUG manual in healthy older adults: an exploratory study.Aging Clin Exp Res. 2017;29:711-720. [DOI] [PubMed] [Google Scholar]
- 24. Jones CJ, Rose DJ. Physical Activity Instruction of Older Adults. Human Kinetics; 2005. [Google Scholar]
- 25. Jorgensen MG, Laessoe U, Hendriksen C, Nielsen OBF, Aagaard P. Efficacy of Nintendo Wii training on mechanical leg muscle function and postural balance in community-dwelling older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2013;68:845-852. [DOI] [PubMed] [Google Scholar]
- 26. Joshua AM, D’Souza V, Unnikrishnan B, et al. Effectiveness of progressive resistance strength training versus traditional balance exercise in improving balance among the elderly—a randomised controlled trial. J Clin Diagn Res. 2014;8:98-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kargarfard M, Shariat A, Shaw I, Haddadi P, Shaw BS. Effects of resistance and aerobic exercise training or education associated with a dietetic program on visfatin concentrations and body composition in overweight and obese women. Asian J Sports Med. 2017;8:e57690. [Google Scholar]
- 28. Kramer A, Dettmers C, Gruber M. Exergaming with additional postural demands improves balance and gait in patients with multiple sclerosis as much as conventional balance training and leads to high adherence to home-based balance training. Arch Phys Med Rehabil. 2014;95:1803-1809. [DOI] [PubMed] [Google Scholar]
- 29. Li R, Polat U, Makous W, Bavelier D. Enhancing the contrast sensitivity function through action video game training. Nat Neurosci. 2009;12:549-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lim J, Cho J-J, Kim J, Kim Y, Yoon B. Design of virtual reality training program for prevention of falling in the elderly: a pilot study on complex versus balance exercises. Eur J Integr Med. 2017;15:64-67. [Google Scholar]
- 31. Lloyd BD, Williamson DA, Singh NA, et al. Recurrent and injurious falls in the year following hip fracture: a prospective study of incidence and risk factors from the Sarcopenia and Hip Fracture study. J Gerontol A Biol Sci Med Sci. 2009;64:599-609. [DOI] [PubMed] [Google Scholar]
- 32. Maguire EA, Burgess N, Donnett JG, Frackowiak RS, Frith CD, O’Keefe J. Knowing where and getting there: a human navigation network. Science. 1998;280:921-924. [DOI] [PubMed] [Google Scholar]
- 33. Mao Y, Chen P, Li L, Huang D. Virtual reality training improves balance function. Neural Regen Res. 2014;9:1628-1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Marchetti GF, Bellanca J, Whitney SL, et al. The development of an accelerometer-based measure of human upright static anterior-posterior postural sway under various sensory conditions: test-retest reliability, scoring and preliminary validity of the Balance Accelerometry Measure (BAM). J Vestib Res. 2013;23:227-235. [DOI] [PubMed] [Google Scholar]
- 35. Miller JP, Croce RV, Hutchins R. Reciprocal coactivation patterns of the medial and lateral quadriceps and hamstrings during slow, medium and high speed isokinetic movements. J Electromyogr Kinesiol. 2000;10:233-239. [DOI] [PubMed] [Google Scholar]
- 36. Montero-Odasso M, Schapira M, Soriano ER, et al. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older.J Gerontol A Biol Sci Med Sci. 2005;60:1304-1309. [DOI] [PubMed] [Google Scholar]
- 37. Nyman SR, Victor CR. Older people’s recruitment, sustained participation, and adherence to falls prevention interventions in institutional settings: a supplement to the Cochrane systematic review. Age Ageing. 2011;40:430-436. [DOI] [PubMed] [Google Scholar]
- 38. Oesch P, Kool J, Fernandez-Luque L, et al. Exergames versus self-regulated exercises with instruction leaflets to improve adherence during geriatric rehabilitation: a randomized controlled trial. BMC Geriatr. 2017;17:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pallant J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using IBM SPSS. Routledge; 2020. [Google Scholar]
- 40. Pereira JC, Neri SGR, Vainshelboim B, et al. Normative values of knee extensor isokinetic strength for older women and implications for physical function.J Geriatr Phys Ther. 2019;42:e25-e31. [DOI] [PubMed] [Google Scholar]
- 41. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743-749. [DOI] [PubMed] [Google Scholar]
- 42. Pescatello LS, Arena R, Riebe D, Thompson PD, Sneak Peek: preview of ACSM’s guidelines for exercise testing and prescription. ACSMs Health Fit J. 2013;17:16-20. [DOI] [PubMed] [Google Scholar]
- 43. Peters DM, Fritz SL, Krotish DE. Assessing the reliability and validity of a shorter walk test compared with the 10-meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. 2013;36:24-30. [DOI] [PubMed] [Google Scholar]
- 44. Pichierri G, Murer K, de Bruin ED. A cognitive-motor intervention using a dance video game to enhance foot placement accuracy and gait under dual task conditions in older adults: a randomized controlled trial. BMC Geriatr. 2012;12:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142-148. [DOI] [PubMed] [Google Scholar]
- 46. Rossman MJ, Garten RS, Venturelli M, Amann M, Richardson RS. The role of active muscle mass in determining the magnitude of peripheral fatigue during dynamic exercise. Am J Physiol Regul Integr Comp Physiol. 2014;306:R934-R940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sadeghi H, Hakim MN, Hamid TA, et al. The effect of exergaming on knee proprioception in older men: a randomized controlled trial. Arch Gerontol Geriatr. 2017;69:144-150. [DOI] [PubMed] [Google Scholar]
- 48. Sato K, Kuroki K, Saiki S, Nagatomi R. Improving walking, muscle strength, and balance in the elderly with an exergame using Kinect: a randomized controlled trial. Games Health J. 2015;4:161-167. [DOI] [PubMed] [Google Scholar]
- 49. Schoene D, Lord SR, Delbaere K, Severino C, Davies TA, Smith ST. A randomized controlled pilot study of home-based step training in older people using videogame technology. PLoS One. 2013;8:e57734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Scott D, Stuart AL, Kay D, Ebeling PR, Nicholson G, Sanders KM. Investigating the predictive ability of gait speed and quadriceps strength for incident falls in community-dwelling older women at high risk of fracture. Arch Gerontol Geriatr. 2014;58:308-313. [DOI] [PubMed] [Google Scholar]
- 51. Seo B, Kim B, Singh K. The comparison of resistance and balance exercise on balance and falls efficacy in older females. Eur Geriatr Med. 2012;3:312-316. [Google Scholar]
- 52. Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51:1750-1758. [DOI] [PubMed] [Google Scholar]
- 53. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther. 2000;80:896-903. [PubMed] [Google Scholar]
- 54. Stauber W, Barill E, Stauber R, Miller G. Isotonic dynamometry for the assessment of power and fatigue in the knee extensor muscles of females. Clin Physiol. 2000;20:225-233. [DOI] [PubMed] [Google Scholar]
- 55. Sturnieks DL, St George R, Lord SR. Balance disorders in the elderly. Neurophysiol Clin. 2008;38:467-478. [DOI] [PubMed] [Google Scholar]
- 56. Thiebaud RS, Funk MD, Abe T. Home-based resistance training for older adults: a systematic review. Geriatr Gerontol Int. 2014;14:750-757. [DOI] [PubMed] [Google Scholar]
- 57. Toulotte C, Toursel C, Olivier N. Wii Fit®training vs. Adapted Physical Activities: which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clin Rehabil. 2012;26:827-835. [DOI] [PubMed] [Google Scholar]
- 58. van Diest M, Lamoth CJ, Stegenga J, Verkerke GJ, Postema K. Exergaming for balance training of elderly: state of the art and future developments. J Neuroeng Rehabil. 2013;10:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Vereeck L, Wuyts F, Truijen S, Van de Heyning P. Clinical assessment of balance: normative data, and gender and age effects. Int J Audiol. 2008;47:67-75. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_1941738120986803 for Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial by Hassan Sadeghi, Deborah A. Jehu, Abdolhamid Daneshjoo, Elham Shakoor, Mohsen Razeghi, Alireza Amani, Muhammad Nazrul Hakim and Ashril Yusof in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-2-sph-10.1177_1941738120986803 for Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial by Hassan Sadeghi, Deborah A. Jehu, Abdolhamid Daneshjoo, Elham Shakoor, Mohsen Razeghi, Alireza Amani, Muhammad Nazrul Hakim and Ashril Yusof in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-3-sph-10.1177_1941738120986803 for Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial by Hassan Sadeghi, Deborah A. Jehu, Abdolhamid Daneshjoo, Elham Shakoor, Mohsen Razeghi, Alireza Amani, Muhammad Nazrul Hakim and Ashril Yusof in Sports Health: A Multidisciplinary Approach