Abstract
The pressure cooker technique was originally ideated to obtain wedge-flow conditions during arteriovenous malformation or arteriovenous fistula embolisation. The anti-reflux plug created with coils or glue around the tip of a detachable microcatheter enables a continuous injection with a more in-depth penetration. Here we describe two illustrative cases performed with a variation of the technique that we describe as the hand-compression pressure cooker technique.
Keywords: Vascular malformation, interventional neuroradiology, arteriovenous fistula, embolisation, endovascular technique
Background and importance
We describe two cases treated with percutaneous embolisation using a new modified version of the original pressure cooker technique, in which the fingers of the operator are used to apply pressure on the proximal end of the microcatheter tip, that we therefore refer to as the hand-compression pressure cooker technique. This technique can be applied to any compressible anatomical location and provides an easy approach to the original pressure cooker technique with major benefits in procedure time, technical complexity while simultaneously providing the same control on backflow. On the other hand, we also describe a potential complication that occurred during the second case that operators could encounter with the application of any different variation of pressure cooker techniques in the soft-tissues.
Case presentation
Case 1
A 25-year-old woman with a diagnosis of non-functioning anterior mediastinal paraganglioma since 2013, considered not eligible for a radical surgical intervention, already treated at our institution with a multistage endovascular procedure in February 2017 and October 2017. The patient presents with symptoms of general malaise, fatigue, thoracic pain with irradiation to the left shoulder and is scheduled for the third embolisation aiming for a residual located in the left mediastinal region around the left brachiocephalic trunk.
The preliminary angiographic study demonstrated blood supply to the tumour through feeders from the left superior thyroid artery, the left ascending pharyngeal artery, the left internal mammary artery and the left deep cervical artery; moreover there were feeders coming from the right supreme intercostal artery and the right inferior thyroid artery. Low-flow contribution was also noted from a sternal artery originating from the left side of the aortic arch (Figure 1).
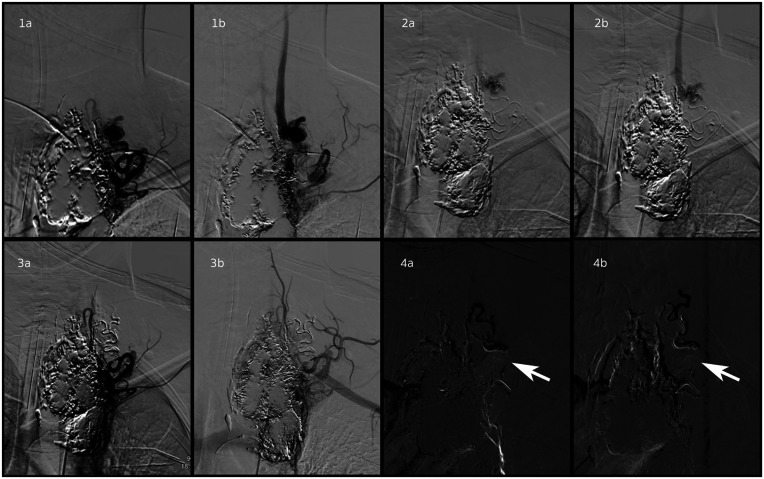
Figure 1.
(1a) and (1b): Demonstration of a high-flow direct shunt between the left deep cervical artery and left jugular external vein. (2a) and (2b): Superselective microcatheter injection demonstrating distal access into the arterial feeder of the arteriovenous fistula. (3a) and (3b): Post-Squid® (Balt Extrusion, Montmorency, France) embolisation selective injection demonstrating no residual arteriovenous shunt. (4a) and (4b): Roadmap guidance image during the embolisation phase demonstrating the operator hand externally compressing the feeding artery just proximal to the microcather tip to control reflux better.
Case 2
A 24-year-old man with a diagnosis of right palpebral arteriovenous malformation without any symptoms, presents to our clinic seeking potential treatment for aesthetic purposes.
The preliminary angiographic study demonstrated direct arterial feeders from the superficial temporal artery and indirect feeders (palpebral artery) coming from the right ophthalmic artery (Figure 2(a) and (b)). We also noted a microvascular supply to the lesion coming from adjacent vessels.
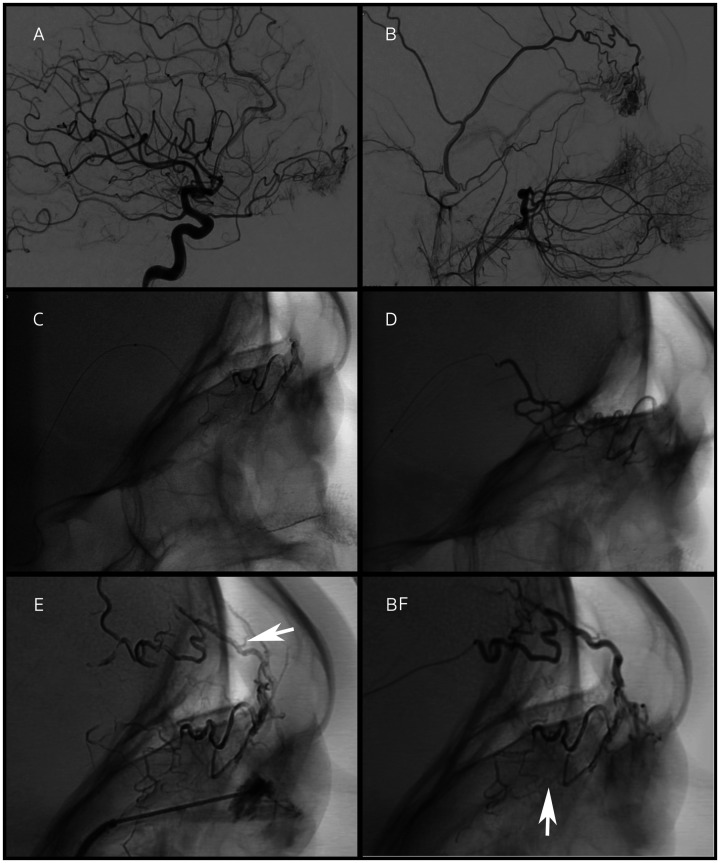
Figure 2.
(a) and (b): Demonstration of a right palpebral arteriovenous malformation with arterial feeders from the superficial temporal artery and indirect feeders (palpebral artery) from the right ophthalmic artery. (c–e): Superselective microcatheter injections of Onyx18 into the arterial feeders are demonstrated during external compression proximal to the microcatheter tip to control reflux of embolic agent. Direct puncture with subsequent injection of n-Butyl Cyanoacrylate Lipiodol Ultra Fluid (NBCALUF) is also seen on the bottom of (e). (e) and (f): White arrows demonstrate deep penetration of Onyx18 in the microvascular supply surrounding the lesion.
Discussion and treatment
Case 1
During the embolisation a direct high-flow shunt (Figure 1(1a) and (1b)) between the left deep cervical artery and the left jugular external vein was successfully embolised using the following technique: a headway 17 microcatheter was advanced distally in the arterial feeder using a 0.014 guidewire and a superselective microinjection was performed; the shunt was excluded with a Squid® (Balt Extrusion, Montmorency, France) injection under continuous roadmap guidance and reflux was avoided with hand external neck compression proximal to the microcatheter tip (Figure 1(2a) and (2b), (3a) and (3b) white arrows, (4a) and (4b)). No complication was noted during the procedure regarding the hand-compression pressure cooker technique.
Case 2
The embolisation was performed injecting n-Butyl Cyanoacrylate Lipiodol Ultra Fluid (NBCALUF) percutaneously (25G needle) through a venous pouch and advancing a duo microcatheter distally in the lateral palpebral arterial branch and injecting Onyx® (Medtronic, Minneapolis, USA) (Figure 2(c–e)) with hand external compression proximal to the microcatheter tip thus avoiding reflux. With this injection we noticed a deep penetration of onyx in the microvascular supply surrounding the lesion (Figure 2(f) white arrow). After the procedure the patient developed a phlegmon on the superior palpebrae that was surgically drained; we hypothesise that the deep microvascular penetration achieved with the pressure cooker technique when used in the soft superficial tissues may be responsible for this complication.
Conclusion
The original pressure cooker technique has already been modified in a various number of fashions (double microcatheter, balloon microcatheter, coils or glue).1–5
This is the first literature report of a hand-compression pressure cooker technique. Furthermore, this technique can be applied to any compressible anatomical location and provides an easy approach to the original pressure cooker technique with major benefits in procedure time, technical complexity while simultaneously providing the same control on backflow. Careful use of the pressure cooker technique should be highlighted in superficial soft tissues because deep penetration may cause superficial necrosis.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article. All author(s) certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaux; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgements
Poster presentation at AINR 2019.
Footnotes
Funding: No funding was received for this research.
Informed consent: Informed consent was obtained from all individual participants included in the study.
ORCID iD: Marco Colasurdo https://orcid.org/0000-0002-7823-3088
References
- 1.Abud D, de Castro-Afonso L, Nakiri G, et al. Modified pressure cooker technique: an easier way to control onyx reflux. J Neuroradiol 2016; 43: 218–222. [DOI] [PubMed] [Google Scholar]
- 2.Chapot R, Stracke P, Velasco A, et al. The pressure cooker technique for the treatment of brain AVMs. J Neuroradiol 2014; 41: 87–91. [DOI] [PubMed] [Google Scholar]
- 3.Clarençon F, Di Maria F, Gabrieli J, et al. Double-lumen balloon for Onyx® embolization via extracranial arteries in transverse sigmoid dural arteriovenous fistulas: initial experience. Acta Neurochirurgica (Wien) 2016; 158: 1917–1923. [DOI] [PubMed] [Google Scholar]
- 4.Griffin A, Befera N, Hauck E. Onyx embolization of a pial AV fistula with a giant venous varix using a flow-directed Scepter balloon catheter: technical note. Intervent Neuroradiol 2018; 24: 702–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang G, Zhu S, Wu P, et al. The transvenous pressure cooker technique: a treatment for brain arteriovenous malformations. Intervent Neuroradiol 2016; 23: 194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]