Abstract
Background
Transradial access for neurointerventional procedures was adopted and modified from cardiovascular intervention and is increasingly established as a safe and effective alternative to transfemoral catheterization. As social media influences public opinion on medical treatment, this study analyzes Twitter conversations to elucidate social media’s depiction of transradial access as a neurointerventional tool.
Materials and methods
Twitter hashtags #RadialFirst and #RadialForNeuro were evaluated using a mixed-method analysis of quantitative social media metrics and qualitative thematic analysis.
Results
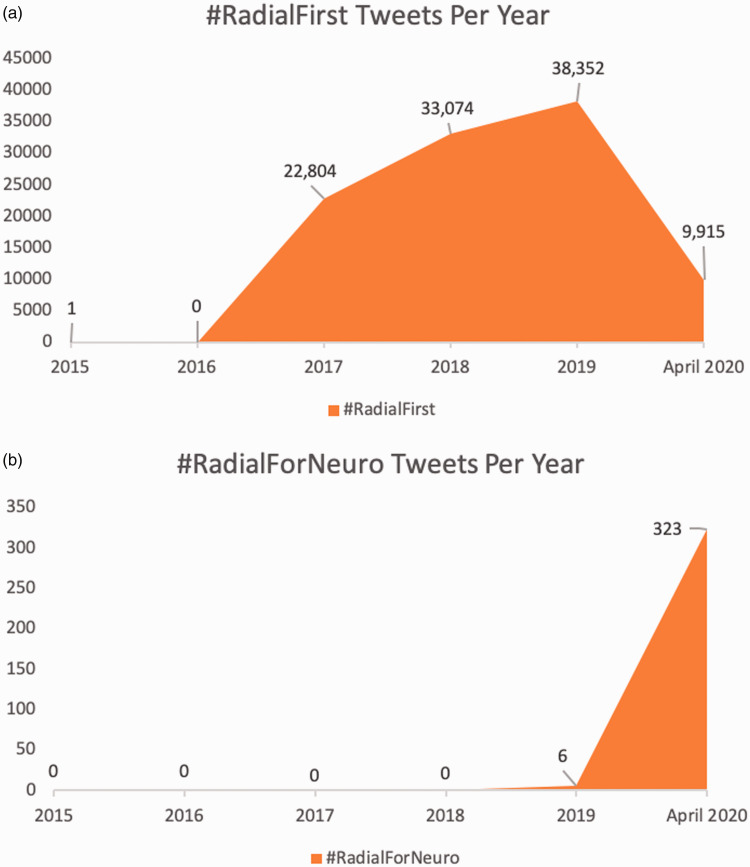
Between January 2015 and April 2020, 104,146 tweets from 141 countries employed the hashtag #RadialFirst (2015 (1); 2016 (0); 2017 (22,804); 2018 (33,074); 2019 (38,352); 2020 (9,915 January-April)). These generated 226,909,374 impressions and were retweeted 80,120 times by 13,707 users. Media was present in 62.5% of tweets (e.g. wrist image, angiographic runs) but only 14.5% had a reference article. Physicians authored 70.8% of tweets; interventional cardiologists accounted for 83% of top 100 influencers. #RadialForNeuro is more nascent (6 posts in 2019; 323 posts January–April 2020), with 392,662 impressions, and 254 retweets by 177 users; physicians authored 35.6%. Compared to #RadialFirst, #RadialforNeuro tweets were more likely to include media (76%), less likely to include citations (9.7%), and more likely to discuss complications and troubleshooting techniques.
Conclusion
Twitter activity regarding transradial access permits information dissemination and discussion on approach benefits and challenges. However, many posts arise from non-physician sources and lack links to peer-reviewed publication. The public should be mindful that tweets may reflect opinions, rather than experience or scientific evidence.
Keywords: Cerebral angiography, endovascular, neurovascular, radial, transradial
Introduction
Radial access is rapidly emerging as a safe and effective alternative to the transfemoral approach within neurointerventional surgery.1–4 This method was pioneered within cardiovascular intervention, as it provided comparable diagnostic and therapeutic technical success, and was associated with fewer access-site related complications than femoral access. 5 A 2018 Cochrane review of 31 interventional cardiology randomized controlled trials concluded that transradial access reduced death from cardiac causes, 30 day all-cause mortality, bleeding, local access-site complications, and hospital length of stay. 6 In neurointerventional surgery, various institutional and multicenter studies have recently corroborated similar safety, feasibility, and clinical benefits of radial catheterization for cerebral and spinal angiography, stroke rescue, tumor embolization, and treatment of aneurysms, arterio-venous fistulas, and vascular malformations.1–4,7–12 The ability to perform transradial catheterization is an important tool to have in a neurointerventional armamentarium. The speed of technique adoption within the field will in part be dependent upon the growing pool of evidence for transradial access efficacy, and the rate of information dissemination.
Historically, the diffusion of innovative technology and techniques across the medical field has relied heavily on peer-reviewed publication and presentations at scientific meetings. While important, these usually impose a cost barrier and less-rapid dissemination, as do traditional instructive textbooks. However, the past decade has demonstrated the importance of social media as a catalyst for literature dissemination, enhanced discussion, and adoption of technology, especially within surgical and interventional specialties.13,14 Today, 72% of the public uses some type of social media, and for many users, social media is part of a daily routine. 15 The use of hashtags (#) permit unified discussion of a topic and permit analysis of public engagement surrounding the idea. The hashtag #RadialFirst emerged within the cardiac community and has expanded to social media conversations within neurointerventional surgery, along with the creation of #RadialForNeuro. While this hashtag is added to features of peer-reviewed publication, it is also used by individuals documenting personal experience and patient-specific cases, generally tilted toward cases with favorable results. A recent systematic review of mechanical thrombectomy results among neurointerventionalists on Twitter heeds warning that the publicized tweets may be biased toward sharing higher thrombectomy success scores. 16 Thus, given the influence of social media on medical practice, it is important to better understand the sources, references, and conversations being propagated around the radial access discussion.
Twitter is a social networking service based in the United States that allows users to communicate through brief messages up to 280 characters. Globally, over 300 million people use the service. 17 This study analyzes Twitter conversations regarding this topic using the popular hashtags #RadialFirst and #RadialForNeuro to provide a quantitative and qualitative evaluation of tweets for thematic analysis and highlight the impact of Twitter in disseminating information regarding the technique, and the role of social media in education and refinement of technical approaches.
Methods
Search strategy and data collection
The Hashtag Finder database (Symplur, Upland, CA, USA) was used to determine the extent of Twitter usage pertaining to transradial approaches. Both #RadialFirst and #RadialForNeuro hashtags were queried for the period between January 2015 and April 2020, since #RadialFirst was initially used in 2015. Data pertaining to the following parameters were compiled from each hashtag search: number of followers for Twitter accounts, timing of tweets, country and state of origin, and type of post (media versus text only) if publicly available. Additional data included the number of impressions (number of times a post is viewed by a user, whether or not the post is clicked), engagements (number of times a post is clicked on to magnify the image or text or view a video), retweets, likes, and URL clicks each post received. Regarding the type categorization of the account owner and his or her profession, Symplur uses machine learning algorithms applied to public data from Twitter account bios and combines that data with human evaluation and quality control to automatically categorize the top influencers of any given healthcare topic into subcategories such as physician or patient. To further evaluate if Twitter account owners were in interventional cardiology, interventional radiology, or neurointerventionalists, our authors reviewed the public biographies of the top 100 influencers. Influencers in this case are defined by two proprietary, recursive algorithms: SymplurRank and Healthcare Social Graph Score, which include a neural network of billions of data points on unique user activity that incorporates but is not limited to followers, retweets, impressions, breadth of influence, and more.
Statistical analysis and ethical considerations
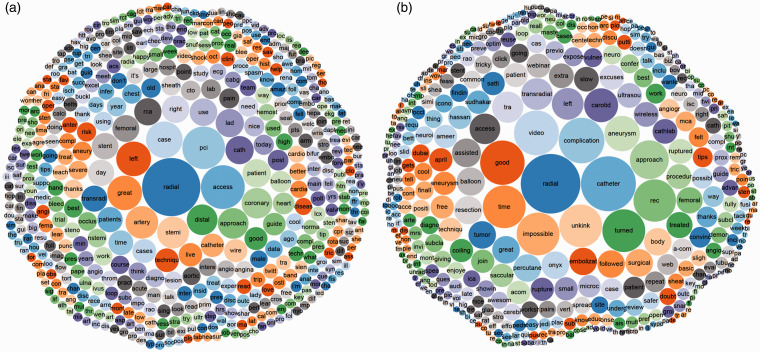
Summary statistics including mean, median, standard deviation, and interquartile range (IQR) for Twitter metrics were calculated. Frequency of term use was displayed in a bubble chart, with bubble size corresponding to term frequency (by Symplur). Analyses were performed with Microsoft Excel. All data were gathered from publicly accessible resources and were strictly archival and cross-section observational, without interaction with users or collection of their usernames.
Results
#RadialFirst
Between January 2015 and April 2020, there were 104,146 tweets from 141 countries using the hashtag #RadialFirst (Table 1). The term was initially used in 2015 but only tweeted once that year. There were no #RadialFirst hashtags in 2016 but the trend truly began in 2017 where there were 22,804 tweets, followed by 33,074 in 2018, 38,352 in 2019, and 9915 by April 2020. These tweets had an overall impression of 226,909,374 and were retweeted 80,120 times by 13,707 users. Media was present in 62.5% of tweets (e.g. wrist image, angiographic runs), but only 14.5% of tweets contained a link to an article. The most frequent journals to cite in tweets were the New England Journal of Medicine (NEJM), the Journal of the American College of Cardiology (JACC): Cardiovascular Interventions, the European Heart Journal – Case Reports, and Circulation: Cardiovascular Interventions. The highest impact tweeted article for #RadialFirst was a NEJM clinical image, 18 followed by a viewpoint article in JACC that illustrated anatomic and physiological principles of distal radial artery access, 19 and a NEJM correspondence regarding a new electrocardiogram pattern in a patient with coronary artery occlusion. 20 Multiple case reports were among the top 10 shared article links. English (92.1%) and Spanish (1.3%) were the most common languages utilized for the tweets. Physicians authored 70.8% of the tweets, followed by 12.4% by academic researchers. Interventional cardiologists accounted for 83% of the top 100 influencers for the hashtag with interventional radiologists making up 6% and neurointerventional surgeons making up 2%. The remaining 9% of top influencers were either bots (an account which automatically re-posts content which is not specifically run by an individual) or by an account which did not reliably fall into one of the abovementioned categories. There were an increasing number of tweets utilizing #RadialFirst over the years (Figure 1(a)). The most common words to accompany the hashtag #RadialFirst were in order: (1) radial, (2) access, (3) PCI, (4) case, (5) left, (6) great, (7) artery, (8) STEMI, (9) distal, and (10) approach (Figure 2(a)).
Table 1.
Statistics for #RadialFirst and #RadialForNeuro Hashtags.
| #RadialFirst n = 104,146 | #RadialForNeuro n = 329 | |
|---|---|---|
| Tweets with mentions | 94,237 (90.5%) | 294 (89.4%) |
| Retweets | 80,120 (76.9%) | 254 (77.2%) |
| Tweets with media | 65,042 (62.5%) | 250 (76%) |
| Tweets with links | 15,148 (14.5%) | 32 (9.7%) |
| Tweet with replies | 6,605 (6.3%) | 4 (1.2%) |
| Users | 13,707 | 177 |
| Impressions | 226,909,374 | 392,662 |
| Countries | 141 | 25 |
Figure 1.
Tweets per year utilizing (a) #RadialFirst and (b) #RadialForNeuro
Figure 2.
Bubble chart of most common words used in conjuncture with (a) #RadialFirst and (b) #RadialForNeuro. Image created on Symplur.com.
#RadialForNeuro
As a spin-off from #RadialFirst, #RadialForNeuro is a more nascent term. Between January 2015 and April 2020, there were 329 tweets from 25 countries using the hashtag #RadialForNeuro (Table 1); 6 times in 2019 and 323 times January–April 2020 (Figure 1(b)). These tweets had an overall impression of 392,662 and were retweeted 254 times by 177 users. Media was present in 76% of tweets, but only 9.7% had a link to an article. The majority of the media images were either of radial artery imaging or cerebral angiograms. Links predominantly referenced articles from the Journal of NeuroInterventional Surgery and the American Journal of Neuroradiology. The articles with most interactions included a systematic review on transradial access, 11 and original research institutional studies.21,22 English (98.2%) and Japanese (0.6%) were the most common languages utilized for the tweets. Physicians authored only 35.6% of the tweets, while 50.5% of accounts were from individuals whose careers were not specifically denoted by their profiles or biography and were listed as unknown. The most common words to accompany the hashtag were: (1) radial, (2) catheter, (3) complication, (4) video, (5) good, (6) time, (7) impossible, (8) unkink, (9) turned, and (10) rec (Figure 2(b)).
Discussion
This analysis of #RadialFirst and #RadialForNeuro hashtag use on Twitter elucidates how the public is utilizing social media in disseminating innovative technology and techniques across medical systems. The presence of #RadialFirst use in 141 countries reflects global awareness of the technique within cardiology, and progressively within the neurointerventional community. The majority of tweets incorporated media, a known strategy to increase post interaction (number of times a post is clicked on to magnify the image or text or view a video), and propagation (retweeting, sharing), 13 and likely contributed to over 200 million interactions. While #RadialForNeuro as a separate entity has only emerged since 2019, it is already being used in 25 countries and has left over 300,000 impressions (number of times a post is viewed by a user, whether or not the post is clicked). This may underrepresent awareness in the neurointerventional surgery community, as many Twitter users will continue to use the more popular #RadialFirst hashtag, even for cerebral and spinal applications.
Demographically, the primary influencers for #RadialFirst were physicians (70.8%) and researchers (12.4%), whereas #RadialForNeuro had only 35.6% physicians. Over half of the #RadialForNeuro accounts belonged to individuals who did not have their profession clearly identified on their profile or in their Twitter biography. The unknown population may reflect neurointerventional surgeons with ambiguous social media accounts, or could reflect occult advocate organizations, patients, and non-healthcare individuals. This population breakdown differs greatly from hashtags that have become more mainstream within the public. For instance, only 8.4% of tweets that utilize #stroke are authored by physicians, while 6.7% are authored by patients, and the majority are generated by advocacy groups and non-healthcare persons. These topics center around stroke prevention, symptoms, associated medical conditions, and treatment options. 23 As #RadialFirst and #RadialForNeuro are more technique-centered rather than disease centered, the core of discussion will likely remain with physician influencers. Additionally, nearly all tweets for both hashtags were in English. Both movements may benefit from broadcasting translations of tweets into other languages to reach more demographics. Free diffusion of early transradial experience has the potential to empower safer and earlier adoption of such access for neurovascular procedures and language is an important aspect of accessibility. For example, users have free access to operator experience in navigating radial loops and avoiding vasospasm or digital ischemia.
The risk of misinformation propagating on Twitter warrants further discussion. It is possible that social media may limit the exposure to diverse perspectives and favor the formation of groups of like-minded users who cultivate a shared narrative. 24 Recent measures by the service include labeling of tweets as potentially misleading when indicated. 25 This caution applies to medical information as well as world affairs, however, measuring how representative and scientifically accurate the information presented in Twitter is poses challenges. For #RadialFirst, approximately 15% of tweets included a reference link to an article, compared to nearly 10% for #RadialForNeuro. The highest impact tweets that contained resource links for #RadialFirst were clinical images, case reports, viewpoints, and correspondence letters from notable journals such as NEJM and Journal of the American College of Cardiology. Such articles do not include robust evidence on the efficacy or effectiveness of approach. In contrast, the highest impact links affiliated with #RadialForNeuro posts were systematic reviews and original research studies. Overall, Twitter posts with reference article links may guide audiences toward evidence-based literature and should be both continued and encouraged.
Regarding the remaining 85–90% of radial access tweets that lack a resource link, there is potential for spreading biased information. In a recent review of Twitter posts for mechanical thrombectomy for stroke, authors noted that individuals documenting personal experience and patient-specific cases disproportionally shared favorable results, which may create an overly positive perception bias for outcomes. 16 Furthermore, author disclosures and financial incentives are seldom apparent, and posts may be used as advertising for specific products or interventions. However, the third most common word used in the #RadialForNeuro discussion was “complication.” Other frequently used terms included “unkinked” and “ruptured,” among multiple positive descriptive terms such as “good” and “rec.” In comparison, the term “complication” was ranked 86th in word frequency for #RadialFirst. This may reflect differences between cardiology and neurointervention in community perspective, openness to discuss obstacles, prevalence of complication, or status of the field on the learning curve of the approach. The prevalence of these terms suggests that the social media discussion is not entirely one-sided, and online exchanges may be facilitating education and refinement of technical approaches through shared experiences of both successes and challenges.
While this study clarifies the landscape of Twitter conversations on transradial access, it has important limitations. First, it only includes tweets containing the #RadialFirst or #RadialForNeuro hashtag and with a potential of an unknown amount of additional radial access related content not included in this analysis. Additionally, the lack of baseline understanding of how many neurointerventionalists or neurosurgeons utilize Twitter as a professional tool limits our understanding of the proportion of engagement with #RadialFirst or #RadialForNeuro tweets, or comparison of social media activity between cardiac and neurological discussions. Regarding demographics, user age and gender are not included in the database, and for #RadialForNeuro, the profession or background of the user was unknown in over 50%. “Tweetstorms” can ignite an opinion stage and could influence many others who have limited hands-on experience in the procedure under evaluation. In addition, an author’s popularity on Twitter and likelihood of successful audience engagement does not necessarily correspond with clinical experience or validity. This is supported by a recent publication that compared a social metric known as the Kardashian index (k-index) with citation index (h-index) scores of interventional neuroradiologists. 26 A lack of association between the k- and h- indices suggests that a robust Twitter presence does not necessarily imply scientific rigor or impactful work. In addition, the demographics and comorbidities of patient cases are also seldom available in order to protect patients according to Health Insurance Portability and Accountability Act (HIPAA) regulations, which introduces unknown bias for case complexity. Finally, the prevalence of hashtag use does not necessarily correspond to increased clinical use. Despite broad use of #RadialFirst within cardiology and extensive literature supporting transradial access over transfemoral for percutaneous coronary intervention, the vast majority (>80%) of proceduralists in the United States remain low radial adopters, and many recent studies continue to be exclusively femoral access.27,28 Nonetheless, this analysis provides useful information about topic trends and discussion within neurointerventional surgery and demonstrates a rise in conversation about the transradial approach.
Conclusion
Twitter communications regarding transradial access for cardiac and neurointerventional care delivery are global, with over 200 million impressions since the origin of the #RadialFirst hashtag. As #RadialForNeuro has differentiated into a new subspecialty discussion, there is evidence of online communication about both the successes and challenges of the approach, as well as sharing of recent original peer-reviewed research. This underscores the impact of Twitter on information dissemination, and the role of social media in education and refinement of technical approaches. The public should be mindful that tweets may reflect opinions, rather than experience or scientific evidence generating mechanisms, and as clinicians engaging in social media conversations, we should strive to propagate unbiased, evidence-based information.
Footnotes
Author note: Naif M Alotaibi is also affiliated to Department of Neurosurgery, National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia.
Conflict of interest: The authors declare that they have no competing interests.
Author contributions: Conception and design: Alotaibi; acquisition of data: Alotaibi; analysis and interpretation of data: all authors; drafting the article: Robertson, Alotaibi; critically revising the article: all authors; reviewed submitted version of manuscript: all authors; approved the final version of the manuscript on behalf of all authors: Alotaibi; statistical analysis: Alotaibi; and study supervision: Alotaibi, Patel.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
ORCID iDs: Faith C Robertson https://orcid.org/0000-0001-7723-9501
Robert W Regenhardt https://orcid.org/0000-0003-2958-3484
References
- 1.Daou BJ, Koduri S, Pandey AS. Commentary: Transition to radial approach for neurovascular procedures is safe and convenient: characterization of a learning experience. Oper Neurosurg (Hagerstown) 2020; 19(5): E469--E470. [DOI] [PubMed] [Google Scholar]
- 2.Galvan Fernandez J, Martínez-Galdámez M, Schüller Arteaga M, et al. Arm-only access for combined transarterial and transvenous neurointerventional procedures. J Neurointerv Surg 2020; 13: 39–41. DOI: 10.1136/neurintsurg-2020-016540. [DOI] [PubMed] [Google Scholar]
- 3.Munich SA, Vakharia K, McPheeters MJ, et al . Transition to transradial access for mechanical thrombectomy-lessons learned and comparison to transfemoral access in a single-center case series. Oper Neurosurg (Hagerstown). Epub ahead of print 22 August 2020. DOI: 10.1093/ons/opaa230. [DOI] [PubMed] [Google Scholar]
- 4.Osbun JW, Patel B, Levitt MR, et al. Transradial intraoperative cerebral angiography: A multicenter case series and technical report. J Neurointerv Surg 2020; 12: 170–175. 2019/09/06. DOI: 10.1136/neurintsurg-2019-015207. [DOI] [PubMed] [Google Scholar]
- 5.Megaly M, Karatasakis A, Abraham B, et al. Radial versus femoral access in chronic total occlusion percutaneous coronary intervention. Circ Cardiovasc Interv 2019; 12: e007778. 2019/06/15. DOI: 10.1161/circinterventions.118.007778. [DOI] [PubMed] [Google Scholar]
- 6.Kolkailah AA, Alreshq RS, Muhammed AM, et al. Transradial versus transfemoral approach for diagnostic coronary angiography and percutaneous coronary intervention in people with coronary artery disease. Cochrane Database Syst Rev 2018; 4(4): 1--116, CD012318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stone JG, Zussman BM, Tonetti DA, et al. Transradial versus transfemoral approaches for diagnostic cerebral angiography: A prospective, single-center, non-inferiority comparative effectiveness study. J Neurointerv Surg 2020; 12: 993–998. 2020/01/25. DOI: 10.1136/neurintsurg-2019-015642. [DOI] [PubMed] [Google Scholar]
- 8.Sattur MG, Almallouhi E, Lena JR, et al. Illustrated guide to the transradial approach for neuroendovascular surgery: A step-by-step description gleaned from over 500 cases at an early adopter single center. Oper Neurosurg (Hagerstown) 2020; 19: 181–189. 2020/06/09. DOI: 10.1093/ons/opaa153. [DOI] [PubMed] [Google Scholar]
- 9.Hanaoka Y, Koyama JI, Ogiwara T, et al. Feasibility and safety of radial-first approach with a radial-specific neurointerventional guiding sheath for intracranial aneurysm coiling in the anterior circulation. World Neurosurg 2020; 142: e297–e306. 2020/07/06. DOI: 10.1016/j.wneu.2020.06.205. [DOI] [PubMed] [Google Scholar]
- 10.Almallouhi E, Al Kasab S, Sattur MG, et al. Incorporation of transradial approach in neuroendovascular procedures: Defining benchmarks for rates of complications and conversion to femoral access. J Neurointerv Surg 2020; 12: 1122–1126. 2020/03/29. DOI: 10.1136/neurintsurg-2020-015893. [DOI] [PubMed] [Google Scholar]
- 11.Joshi KC, Beer-Furlan A, Crowley RW, et al. Transradial approach for neurointerventions: A systematic review of the literature. J Neurointerv Surg 2020; 12: 886. DOI: 10.1136/neurintsurg-2019-015764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohammadian R, Najaran A, Sohrabi B, et al. Vertebral artery orifice stenosis: A report of 43 cases from Northwest Iran treated with angioplasty and stenting. Neuroradiol J 2011; 24: 749–757. 2011/10/31. DOI: 10.1177/197140091102400513. [DOI] [PubMed] [Google Scholar]
- 13.Linzey JR, Robertson F, Haider AS, et al. Online impact and presence of a specialized social media team for the journal of neurosurgery: Descriptive analysis. J Med Internet Res 2020; 22: e17741. 2020/03/13. DOI: 10.2196/17741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luc JGY, Archer MA, Arora RC, et al. Social media improves cardiothoracic surgery literature dissemination: Results of a randomized trial. Ann Thorac Surg 2020; 109: 589–595. DOI: 10.1016/j.athoracsur.2019.06.062. [DOI] [PubMed] [Google Scholar]
- 15.Pew Research Center. Social media use in 2018, https://www.pewinternet.org/fact-sheet/social-media (2019, accessed 7 Sept 2020).
- 16.Dmytriw AA, Sorenson TJ, Morris JM, et al. #Fake news: A systematic review of mechanical thrombectomy results among neurointerventional stroke surgeons on Twitter. J Neurointerv Surg 2019; 11: 460–463. 2018/09/17. DOI: 10.1136/neurintsurg-2018-014319. [DOI] [PubMed] [Google Scholar]
- 17.Tankovska H. Number of Twitter users worldwide from 2014 to 2024, https://www.statista.com/statistics/303681/twitter-users-worldwide/ (accessed 1 March 2021).
- 18.Arboine L, Palacios JM. Left main coronary artery aneurysm. New Engl J Med 2018; 378: e32. DOI: 10.1056/NEJMicm1708877. [DOI] [PubMed] [Google Scholar]
- 19.Sgueglia GA, Di Giorgio A, Gaspardone A, et al. Anatomic basis and physiological rationale of distal radial artery access for percutaneous coronary and endovascular procedures. JACC: Cardiovasc Interv 2018; 11: 2113. DOI: 10.1016/j.jcin.2018.04.045. [DOI] [PubMed] [Google Scholar]
- 20.de Winter RJ, Verouden NJW, Wellens HJJ, et al. A New ECG sign of proximal LAD occlusion. New Engl J Med 2008; 359: 2071–2073. DOI: 10.1056/NEJMc0804737. [DOI] [PubMed] [Google Scholar]
- 21.Knox JA, Alexander MD, McCoy DB, et al. Impact of aortic arch anatomy on technical performance and clinical outcomes in patients with acute ischemic stroke. Am J Neuroradiol 2020; 41: 268. DOI: 10.3174/ajnr.A6422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen SH, Brunet M-C, Sur S, et al. Feasibility of repeat transradial access for neuroendovascular procedures. J Neurointerv Surg 2020; 12: 431. DOI: 10.1136/neurintsurg-2019-015438. [DOI] [PubMed] [Google Scholar]
- 23.Bundy JJ, Chick JFB, Hage AN, et al. #Stroke. J Neurointerv Surg 2018; 10: e33. DOI: 10.1136/neurintsurg-2018-013877. [DOI] [PubMed] [Google Scholar]
- 24.Cinelli M, De Francisci Morales G, Galeazzi A, et al. The echo chamber effect on social media. Proc Natl Acad Sci U S A 2021; 118: e2023301118. DOI: 10.1073/pnas.2023301118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roth Y, Pickles N. Updating our approach to misleading information, https://blog.twitter.com/en_us/topics/product/2020/updating-our-approach-to-misleading-information.html (2020, accessed 10 Oct 2020).
- 26.Vilanilam GK, Wadhwa V, Purushothaman R, et al. The Kardashian index of interventional neuroradiologists: Measuring discrepant social media influence. Neuroradiol J 2020; 33: 525–527. 2020/09/11. DOI: 10.1177/1971400920950928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Badri M, Shapiro T, Wang Y, et al. Adoption of the transradial approach for percutaneous coronary intervention and rates of vascular complications following transfemoral procedures: Insights from NCDR. Catheter Cardiovasc Interv 2018; 92: 835–841. 2018/01/24. DOI: 10.1002/ccd.27490. [DOI] [PubMed] [Google Scholar]
- 28.Hainc N, Mannil M, Anagnostakou V, et al. Deep learning based detection of intracranial aneurysms on digital subtraction angiography: A feasibility study. Neuroradiol J 2020; 33: 311–317. 2020/07/08. DOI: 10.1177/1971400920937647. [DOI] [PMC free article] [PubMed] [Google Scholar]