Abstract
Background: Patient satisfaction with outpatient pharmacy services at our institution was below the target level, due mainly to long waiting times. A lean management strategy to reduce patient waiting time and increase the satisfaction of both patients and staff was developed and implemented. Methods: The project was conducted in the outpatient pharmacy of a comprehensive cancer center in Amman, Jordan. The process started with formation of a multidisciplinary team and A3 problem-solving, which is a 10-step scientific method with measurable patient-centered outcomes. Average patient waiting time and level of patient satisfaction were compared before and after full implementation of the process. In addition, a survey was conducted among the pharmacy staff who worked in the outpatient pharmacy during the process to determine its impact on staff satisfaction. Results: Patient waiting time for prescriptions of fewer than 3 medications and of 3 medications or more decreased significantly (22.3 minutes vs 8.1 minutes, P < .001, and 31.8 minutes vs 16.1 minutes, P < .002, respectively), and patient satisfaction increased (62% vs 69%; P = .005) after full implementation of the project. The majority of the pharmacy staff reported that the process motivated them in their work and that both their jobs and their relationships with their managers and colleagues had improved. Conclusion: Application of lean management in an outpatient pharmacy was effective in reducing patient waiting time and improving the satisfaction of both patients and employees.
Keywords: ambulatory services, dispensing, staff development, management, human resources
Background
“Lean management” refers to a quality improvement philosophy and a set of principles for maximizing customer value while minimizing waste. 1 Its aim is to change organizational thinking and values, ultimately transforming the behavior and culture of an organization. Although the “lean” philosophy originated in the manufacturing industry, it has been used in numerous sectors, including health care, over the past 2 decades.2,3
“Lean” is defined as an organization’s cultural commitment to applying the method to designing, performing, and continuously improving the work delivered by teams of people, leading to measurably better value for patients and other stakeholders. 1 The goal of lean in health care is to create maximum value for patients by reducing waste and waiting time, and it is expected that focusing on patient values will also benefit others involved in health care. 2 Nevertheless, research on its widespread application and sustainability in health care is still limited.2,4
Despite the limited research on lean methodology in the healthcare setting, several institutions around the world described their experiences with lean and its impact on the quality of service and patient care.5–8 The effect of implementing lean bundles on hospital performance in private hospitals in Jordan was recently described. Lean bundles were identified as an effective approach that can improve the performance of private hospitals in Jordan which would be applicable to large, medium, and small hospitals without differences in advantages based on the size of the hospital. 9 At King Hussein Cancer Center (KHCC), the lean methodology was incorporated into the KHCC improvement system as part of the strategic task force, with the main goal of cultivating lean thinking culture in the hospital. 10 The KHCC experience demonstrated how applying lean in healthcare can generate improvement at many levels, but would need support from administration, proper training, and awareness campaigns to build up a culture that motivates lean thinking.
The monthly pharmacy quality reports generated by the quality department at KHCC demonstrated that patients receiving their medications from the hospital’s outpatient pharmacy had low level of satisfaction, due mainly to the long waiting time. As patient satisfaction is one of the major strategic goals of KHCC and a key performance indicator, the pharmacy administration formed a committee to develop a strategy to reduce the waiting time at the outpatient pharmacy and thus improve patient satisfaction. As the hospital was promoting lean culture and thinking at the time, the project was conducted with lean management principles and tools.
The purpose of this paper is to describe the lean management strategy that was used to reduce the waiting time at the hospital’s outpatient pharmacy and show its impact on patients’ and employees’ satisfaction. By describing this experience, our goal is to demonstrate the value of lean methodology in the healthcare settings.
Methods
Study Setting and Design
This project was conducted at KHCC, a 170-bed comprehensive cancer center that serves over 3500 patients each year. The hospital has a pediatrics and a main outpatient pharmacy, which process about 10 000 refill and new prescriptions each month. The 2 pharmacies employ about 40 pharmacists and pharmacy technicians, who rotate between the inpatient and outpatient settings. Patients who receive cancer treatment at KHCC typically receive their discharge medications and their cancer and non-cancer home medications from the outpatient pharmacy. The lean project was conducted in the main outpatient pharmacy, which processes about 4000 new prescriptions a month for adult patients.
The team for the project was multidisciplinary, consisting of 4 members from the pharmacy department, 1 from the information technology department, and 1 from the quality department. All members attended a three-day on-site interactive workshop in lean management given by a lean management consultant and were mentored by the expert during project initiation.
Sampling
All prescriptions that were received and dispensed by the main outpatient pharmacy between June 2015 and December 2016 were included in the analysis of average waiting time. Data between June 2015 and March 2016 were considered as the pre-implementation period while the period between April 2016 and December 2016 was considered the post-implementation phase. The total number of included prescriptions were 67 099 prescriptions, 34 348 in the pre-implementation period and 32 751 prescriptions in the post-implementation period. In addition, the 37-pharmacy staff who worked in the main outpatient pharmacy during the implementation of the project were asked to complete an employee satisfaction survey.
Data for patient satisfaction regarding pharmacy waiting time were obtained from the hospital’s patient satisfaction survey report. The hospital’s quality department uses a satisfaction assessment tool developed by the department which includes elements reflective of the quality key performance indicators for patient satisfaction. The survey asks patients about their satisfaction with several aspects of their patient care. One of the questions asks patients to rate their level of satisfaction with the outpatient pharmacy waiting time on a five-point Likert scale, with 1 being the least satisfied and 5 being the most satisfied. A score of 4 or 5 was considered as satisfied.
Intervention and Data Collection
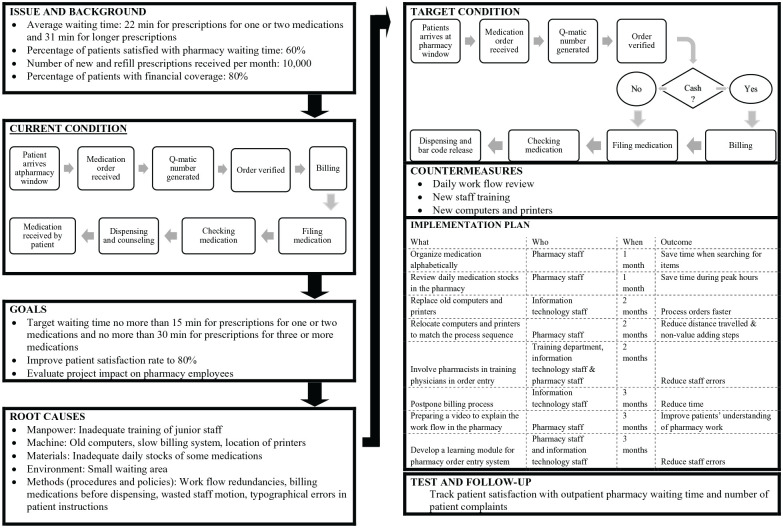
The team began by preparing an “A3 problem-solving report”, a lean management tool written on an A3 paper so that it is large enough for consultation together. The report consists of 10 steps for identifying measurable improvements in issues identified by the team members: (1) issue, (2) background, (3) current condition, (4) goal, (5) root cause, (6) target condition, (7) countermeasures, (8) implementation plan, (9) test, and (10) follow-up. 11 Figure 1 outlines the major elements of the report.
Figure 1.
A3 problem-solving report for the project on reducing waiting time.
(1) Issue and (2) Background: The “issue and background” sections provided details of the average waiting time of patients and their level of satisfaction with the time. The number of prescriptions received by the outpatient pharmacy each month, the number of medications per prescription, and the time taken to prepare each prescription were retrieved from the pharmacy electronic system and listed on the A3 report.
(3) Current condition: The report outlined the steps in processing prescriptions according to pharmacy standard operating procedures (SOPs). The SOP-defined target waiting times were no more than 20 minutes for prescriptions for 1 or 2 medications and no more than 45 minutes for prescriptions for 3 or more medications; however, it was apparent that patient satisfaction with the current waiting times was below target level.
Lean management tools were used to describe the current condition, including “power of observation”, which is a simple approach to collecting data about patients, the work process, and deviations, which are not typically captured in system-generated reports or SOPs. 12 Team members stood in the pharmacy and the patient waiting area twice daily for 3 days, once during peak hour and a second time during less busy hours, over 3 weeks. They recorded their observations. The pharmacy staff was informed about the visits, and the observations made by the team members were discussed and verified with the staff involved.
“Spaghetti diagram”, another lean tool used to describe the current condition, is a visual presentation of the process, consisting of a continuous line tracing the path of an item or activity. A team member traced the movements of 1 pharmacist working in the area on a blueprint of the current area to produce a spaghetti diagram that represented motion in the area. Motion is considered a type of waste to be reduced by lean management. The team also undertook “value stream mapping” of all the steps involved in processing prescriptions and the time required for each step. This is a visual representation of the flow of people, material, and information, which identifies process’s wastes, inefficiencies and steps that do not add value to customers and can be eliminated. 13 The current process was drawn on large pieces of cardboard, with colors, arrows, and sticky notes. Star shapes were added to indicate opportunities, bright spots to indicate what was working during the process, and cloud shapes for challenges. Copies were hung in all areas of the pharmacy and not only in the outpatient pharmacy. All staff, especially “front-line” pharmacy staff, was asked to review the outlined process and suggest how it could be improved.
(4) Goal: The main goals of the project were to reach the reduced target waiting time, improve patient satisfaction from baseline of 62% to 80%, and positively impact pharmacy employees.
(5) Root cause: Once all the notes had been collected, the “root causes” were outlined on the A3 report. A “fishbone diagram” was used to analyze root causes, categorized into 5 sections: manpower (employees), machine (computers), materials (medications), environment (waiting area), and methods (SOPs and policies). 14
(6) Target condition: Billing was observed as the bottleneck that was slowing the flow of prescriptions. In the diagram of the suggested new process, the billing step was moved to the end, so that patients with insurance, who account for about 80%, would no longer have to wait, as they do not have to pay. This step clearly did not add value for these patients, as the finance office could note the prescription after the patients had received their medication. One of the concerns raised about postponing the billing step was the potential discrepancies between the generated pharmacy inventory reports and the actual stocks on hand in the pharmacy, since the reports generated during the day may not reflect the total consumption. However, this was addressed by ensuring that the billing step was an ongoing process throughout the day, parallel to the order processing steps, and that it was completed by the end of each day.
(7) Countermeasures: To reach the target condition, “countermeasures” were listed on the A3 report to rectify the root causes.
(8) Implementation plan: The A3 report included a table outlining the tasks, task leaders, deadlines, and outcome. The “SMARTER” mnemonic was used to define the goals and tasks to ensure that they were “specific, meaningful, achievable, relevant, time-bound and could be evaluated and re-adjusted”. The changes were expected to be implemented gradually over 6 months (October 2015-March 2016). The post-implementation phase included in the analysis reflected the 9 months period after the full implementation of the changes (April 2016-December 2016).
(9) Test and (10) Follow-up: These sections of the A3 report listed the effect of the plan on patient waiting time, their satisfaction, and any changes required to the process. Reports for waiting time were generated from the pharmacy electronic system on a monthly basis. The waiting time reports were calculated by the electronic system and defined as the time interval between patient handing the medication prescription to the pharmacy and receiving the medications from the dispensing window. The time is automatically calculated via the pharmacy electronic system. Though it would have been important to target what patients would consider as an acceptable waiting time for prescriptions, most patients did not have a clear idea of all the steps involved and thus may not be able to determine the reasonable time to complete the processing of orders. Accordingly, the target times were set based on simulating the proposed new workflow in accordance with the SOPs and expected workload. Target waiting time was reduced to 15 minutes for prescriptions for 1 or 2 medications and 30 minutes for prescriptions for 3 or more medications. Patient satisfaction with waiting time was monitored on a monthly basis by evaluating the hospital’s patient satisfaction survey report which included 1 question that asked about the level of satisfaction with the waiting time at the outpatient pharmacy. Achieving satisfaction among greater than or equal to 80% of the surveyed patients was a predefined indicator by the hospital’s quality section.
To assess the impact of the lean management strategy on employees’ satisfaction, a survey was distributed to all pharmacy staff working during implementation of the project in the outpatient pharmacy. The survey contained 14 questions adapted from the National Health Service project in the United Kingdom.15,16
To ensure that patient safety was not compromised by reducing the waiting time, the numbers of pharmacy interventions which include medical errors and order clarification were recorded and assessed monthly for 1 year after initiation of the project.
The team ensured a learning environment throughout the project, as the outcomes of lean are best achieved in a learning institution. 17 The team members discussed the lean thinking concepts and culture continually and emphasized the importance of ensuring that patients were at the center of their work. Discussions were held while the team was in the pharmacy area, during staff meetings, during “brainstorming” sessions, and in general discussions. In addition, the staff was asked to provide feedback and suggestions at all stages of the project.
Data Analyses
All the collected data regarding waiting time and patient satisfaction were included in the statistical analysis of the data. Student t-test was used to analyze the data of the average waiting time and the percentage of prescriptions that were finished within the target time. Chi-square test was used to analyze the data of patients’ satisfaction. The number of monthly pharmacy interventions after implementing the project was compared with the average number before the implementation which was between 60 and 80 interventions a month.
Results
The lean management project was initiated in October 2015 and was fully implemented in March 2016. The analysis of the current workflow based on the Lean management tools utilized led to several findings. Firstly, the analysis of the completed spaghetti diagram showed that the pharmacy staff had to walk relatively long distances back and forth during their daily work due to improper placement of certain medications and hardware devices. This guided the team to challenge the mindset of having to keep all medications in their original locations, and relocate 3 highly dispensed medications to places closer to working areas after marking their bins in a clear manner to maintain the alphabetical order within the pharmacy and to relocate computers and printers to match the process sequence and reduce motion.
Secondly, value stream mapping analysis showed that from the patients’ perspectives, the billing step was considered as a non-value-added step that forms a significant percentage of the total waiting time for any prescription. Thus, moving the billing step to the end of prescription processing for financially covered patients lead to significant reduction in the current waiting time. Other findings and actions are described in the root causes and implementation plan in Figure 1.
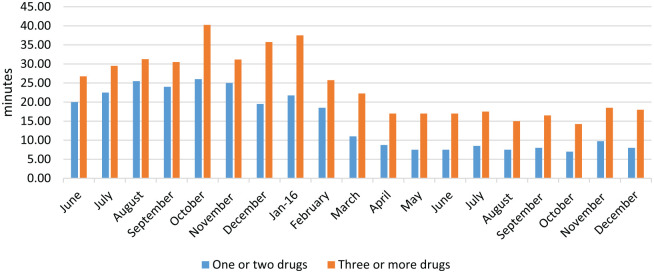
Patient waiting time for all types of prescriptions decreased significantly after full implementation and was maintained for up to 9 months. (Figure 2) The average waiting time for prescriptions for 1 or 2 medications was 22.3 minutes initially and 8.1 minutes (range 7.5-9.8 minutes) after full implementation of the new process (P < .0001). The percentage of prescriptions that were finished within the target time of 15 minutes was significantly increased, from 56.8% to 94.7% (P = .0002). The average waiting time for prescriptions for 3 or more medications was 31.8 minutes initially and 16.1 minutes (range 14.3-22.3 minutes) after full implementation of the new process (P = .0002). The percentage of prescriptions that were finished within the target time of 30 minutes was increased from 44.8% to 93.7% (P < .0001).
Figure 2.
Average patient waiting time in the main outpatient pharmacy per month.
Prior to initialization of the lean project, 604 patients completed the quality survey; of those, 375 (62%) were satisfied with the waiting time at the outpatient pharmacy. After full implementation of the new process, 817 patients completed the quality survey, and 564 (69%) reported being satisfied (P = .005). The improved level of satisfaction was maintained throughout the 9-month follow-up, with 71% of the patients reporting being satisfied at 9 months.
The numbers of interventions that included medication errors and order clarification before initiation of the project and after full implementation of the new process were within the reported daily rates at the outpatient pharmacy (60–80 interventions). The inventory and billing showed no notable discrepancies after postponement of the billing step based on the inventory auditing reports.
The employee satisfaction survey was completed by 30 pharmacists and 7 pharmacy technicians working in the outpatient pharmacies during the project. About two-thirds of those who completed the survey reported that their relationships with their colleagues and managers had improved and that lean had improved their workplace and their motivation for working in an efficient, productive environment (Table 1).
Table 1.
Results of the Employee Satisfaction Survey (N = 37).
| Question | Response | N (%) |
|---|---|---|
| How long have you been working in pharmacy? | <1 year | 12 (32.4%) |
| 1–3 years | 14 (37.8%) | |
| 3–6 years | 4 (10.8%) | |
| 6–12 years | 7 (18.9%) | |
| What is your position in this pharmacy? | Pharmacist | 30 (81%) |
| Pharmacy technician | 7 (19%) | |
| Have relationships with your managers improved in some way since the lean methodology was implemented? | Strongly agree | 1 (2.7%) |
| Agree | 24 (64.9%) | |
| Neutral | 9 (24.3%) | |
| Disagree | 3 (8.1%) | |
| Strongly disagree | 0 (0%) | |
| Have relationships with your colleagues improved in some way since the lean methodology was implemented? | Strongly agree | 0 (0%) |
| Agree | 24 (64.9%) | |
| Neutral | 10 (27.0%) | |
| Disagree | 3 (8.1%) | |
| Strongly disagree | 0 (0%) | |
| My supervisor seeks my opinion in making decisions that impact our team/department. | Strongly agree | 7 (18.9%) |
| Agree | 20 (54.1%) | |
| Neutral | 9 (24.3%) | |
| Disagree | 1 (2.7%) | |
| Strongly disagree | 0 (0%) | |
| My supervisor puts my ideas or suggestions to use. | Strongly agree | 4 (10.8%) |
| Agree | 25 (67.6%) | |
| Neutral | 6 (16.2%) | |
| Disagree | 1 (2.7%) | |
| Strongly disagree | 1 (2.7%) | |
| My supervisor allows me/our team to make decisions that impact my/our team’s work. | Strongly agree | 2 (5.4%) |
| Agree | 28 (75.7%) | |
| Neutral | 5 (13.5%) | |
| Disagree | 1 (2.7%) | |
| Strongly disagree | 1 (2.7%) | |
| Do you believe your assigned tasks are more standardized in a way that avoids wastes such as body motions, waiting, and medication handling since the lean methodology was implemented? | Strongly agree | 3 (8.1%) |
| Agree | 23 (62.2%) | |
| Neutral | 6 (16.2%) | |
| Disagree | 4 (10.8%) | |
| Strongly disagree | 1 (2.7%) | |
| Do you feel more motivated working in an environment focused on efficiency and productivity? | Strongly agree | 7 (18.9%) |
| Agree | 25 (67.6%) | |
| Neutral | 4 (10.8%) | |
| Disagree | 1 (2.7%) | |
| Strongly disagree | 0 (0%) | |
| Do you believe that implementing lean methodology has improved your workplace? | Strongly agree | 4 (10.8%) |
| Agree | 23 (62.2%) | |
| Neutral | 9 (24.3%) | |
| Disagree | 1 (2.7%) | |
| Strongly disagree | 0 (0%) | |
| Do you believe that your job has been improved by implementation of lean methodology? | Strongly agree | 4 (10.8%) |
| Agree | 22 (59.5%) | |
| Neutral | 10 (27.0%) | |
| Disagree | 1 (2.7%) | |
| Strongly disagree | 0 (0%) | |
| I feel that my role makes a difference to patients and service users. | Strongly agree | 8 (21.6%) |
| Agree | 25 (67.6%) | |
| Neutral | 4 (10.8%) | |
| Disagree | 0 (0%) | |
| Strongly disagree | 0 (0%) | |
| I am satisfied with the quality of care I give to patients/services. | Strongly agree | 11 (29.7%) |
| Agree | 8 (21.6%) | |
| Neutral | 13 (35.1%) | |
| Disagree | 5 (13.5%) | |
| Strongly disagree | 0 (0%) | |
| I get recognition for good work. | Strongly agree | 13 (35.1%) |
| Agree | 16 (43.2%) | |
| Neutral | 7 (18.9%) | |
| Disagree | 1 (2.7%) | |
| Strongly disagree | 0 (0%) |
Discussion
Application of lean management in the outpatient pharmacy of a comprehensive cancer center reduced patient waiting time and improved patient satisfaction. Creating a culture of lean in which all pharmacy staff were involved at all stages and developing a patient-centered process were essential not only for the initial success of the interventions but also for the sustainability of the outcomes.
Use of lean management to reduce waiting time has been described in several health care settings.18-21 Sullivan et al. reported on the impact of using lean methodology to improve productivity in a hospital oncology pharmacy. Staff-recommended workflow changes were implemented, including the elimination of 6 steps of no value to patients, which reduced the turnaround time per dose. In this project, billing was identified as a major non-value step and was therefore postponed to after dispensing of medications for all patients who have insurance coverage for their treatment. For Jordanian cancer patients treated at the hospital, the insurance covers their medications during their cancer treatment, and this segment reflected about 80% of our patients.
The impact of lean health care on patient satisfaction is less clear. In a recently published case study, no significant difference in patient satisfaction was found between primary care centers with lean health care and those not working with lean. 22 The authors stated that lean health care primarily targets efficiency, with little attention to the patient perspective. In this project, a patient-centered approach was used and focused on the values important to patients, which contributed to improving their satisfaction. Ng et al. reported improved patient satisfaction after implementation of lean principles in an emergency department. 18 These findings emphasize the importance of incorporating patient values into lean health care to achieve outcomes that are of value to patients.
Although the results demonstrated a significant improvement in patient satisfaction after implementation of the lean process, a greater increase had been anticipated. It is predicted that more emphasis is still needed on patient values; therefore, the next phase of the lean process will be to include 1 or 2 patients on the project team. It is expected that they will provide insights into value and non-value steps that might have been overlooked by the team that worked on the initial phase of the project.
The lean management strategy requires the involvement of staff in optimizing the work process; thus, the approach can be expected to have a positive impact on employee satisfaction and motivation.15,16 At a radiotherapy institute, Simons et al. reported improved waiting times as well as employee satisfaction with the implementation of lean interventions. 21
Conclusions
In this quality improvement project, lean management tools were applied in a health care setting to introduce this way of thinking into daily practice and to reduce the waiting time at the outpatient pharmacy, thus improving patients’ satisfaction. The staff were involved from the beginning, including in decision-making; they thus felt that they “owned” the process and could sustain the results.
Strengths and Limitations
The main limitation in the setting, which may have impacted the results, was the limited space and resources. The limited space restricted the number of computers that can be placed in the pharmacy as well as the stock that could be stored. Another limitation was not having a patient on the working team. The survey conducted to measure patient satisfaction with the pharmacy waiting time included about 1500 patients; however, it was limited to one direct question within a larger department survey about satisfaction in general. The discussions with the pharmacy staff about the recorded observations and patient satisfaction may have influenced the overall performance of the pharmacy staff and thus presents a form of bias, the long-term sustainability of the improvement minimizes the possibility of such potential bias.
The 9-month follow-up of patient satisfaction constitutes a major strength that can be built into a second phase to this project. The second phase will include patients in the team carrying out the quality improvement project, the aim of which will be to further reduce the waiting time. A Criteria will be established for direct involvement of randomly selected patients in team meetings, to get their feedback on their perceptions of waiting and the waiting area, in order to engage them directly in quality improvement and decision-making. The survey will be revised to include more questions that specifically address pharmacy waiting time and patient satisfaction.
Acknowledgments
The authors would like to thank Dr Elisabeth Heselitine for reviewing and editing the manuscript. Also, they thank the outpatient pharmacies staff at King Hussein cancer center for their impact during the application of the lean project.
Footnotes
Authors’ Contributions: SH: contributed to the project development and implementation, analyzing results and writing/ reviewing the manuscript. AA: contributed to the project development and implementation, analyzing results, and writing/reviewing the manuscript. SJ: contributed to the project development and implementation, analyzing results, and reviewing the manuscript. LN: contributed to the project methods, analyzing the results, and writing/reviewing the manuscript. EJ: contributed to the project development, analyzing results, and reviewing the manuscript. RA: contributed to the project development, analyzing results, and reviewing the manuscript. all authors have read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate: This study was approved by the Institutional Review Board in King Hussein cancer center. All the study members had signed a confidentiality agreement consent. There were no patient’s identifiers in the analyzed data.
ORCID iD: Suzan Hammoudeh  https://orcid.org/0000-0002-1928-9591
https://orcid.org/0000-0002-1928-9591
References
- 1. Toussaint JS, Berry LL. The promise of lean in health care. Mayo Clin Proc. 2013;88:74-82. [DOI] [PubMed] [Google Scholar]
- 2. Lawal AK, Rotter T, Kinsman L, et al. Lean management in healthcare: definition, concepts, methodology and effects reported (systematic review protocol). Syst Rev. 2014;3:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lean Enterprise, Inc. What is Lean? Cambridge, MA. 2017. https://www.lean.org/WhatsLean/. Accessed April 5, 2017. [Google Scholar]
- 4. D’Andreamatteo A, Ianni L, Lega F, et al. Lean in healthcare: a comprehensive review. Health Policy. 2015;119:1197–1209. [DOI] [PubMed] [Google Scholar]
- 5. Miller R, Chalapati N. Utilizing lean tools to improve value and reduce outpatient wait times in an Indian hospital. Leadersh Health Serv (Bradf Engl). 2015;28:57-69. [DOI] [PubMed] [Google Scholar]
- 6. Jorma T, Tiirinki H, Bloigu R, Turkki L. LEAN thinking in Finnish healthcare. Leadersh Health Serv (Bradf Engl). 2016;29:9-36. [DOI] [PubMed] [Google Scholar]
- 7. Costa LB, Filho MG, Rentes AF, Bertani TM, Mardegan R. Lean healthcare in developing countries: evidence from Brazillian hospitals. Int J Health Plann Manage. 2017;32:e99-e120. [DOI] [PubMed] [Google Scholar]
- 8. Hassanain M, Zamakhshary M, Farhat G, Al-Badr A. Use of lean methodology to improve operating room efficiency in hospitals across the Kingdom of Saudi Arabia. Int J Health Plann Manage. 2017;32:133-146. [DOI] [PubMed] [Google Scholar]
- 9. Al-Hyari K, Abu Hammour S, Abu Zaid MK, Haffar M. The impact of lean bundle on hospital performance: does size matter? Int J Health Care Qual Assur. 2016;29:877-894. [DOI] [PubMed] [Google Scholar]
- 10. Mansour AH, Nashawati DM, Hamaly MA, Saidan YA. Initiating and sustaining lean management in healthcare: The King Hussein Cancer Center experience. World Hosp Health Serv. 2018;54:40-41. [Google Scholar]
- 11. Bassuk JA, Washington IM. The A3 problem solving report: a 10-step scientific method to execute performance improvements in academic research vivarium. PLoS One. 2013;8:e76833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Arumugam V, Antony J, Douglas A. Observation: a lean tool for improving the effectiveness of Lean Six Sigma. TQM J. 2008;24:275–287. [Google Scholar]
- 13. Gellad ZF, Day TE. What is value stream mapping and how can it help in my practice? Am J Gastroenterol. 2016;111:447–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. American Society for Quality. Fishbone (Ishikawa) diagram. Milwaukee, WI; 2017. http://asq.org/learn-about-quality/cause-analysis-tools/overview/fishbone.html. Accessed April 5, 2017. [Google Scholar]
- 15. Ham C. Improving NHS care by engaging staff and devolving decision-making. London: The King’s Fund; 2014. https://www.kingsfund.org.uk/publications/articles/improving-nhs-care-engaging-staff-and-devolving-decision-making. Accessed April 5, 2017. [Google Scholar]
- 16. Peter Barron Stark Companies. 6 reasons to involve employees in decision making. San Diego, CA; 2014. https://www.peterstark.com/key-to-engagement/#. Accessed April 5, 2017. [Google Scholar]
- 17. Garvin D, Edmondson A, Gino F. Is yours a learning organization? Harvard Business Review, March; 2008. https://hbr.org/2008/03/is-yours-a-learning-organization. Accessed April 5, 2017. [PubMed]
- 18. Ng D, Vail G, Thomas S, et al. Applying the lean principles of the Toyota Production System to reduce wait-times in the emergency department. Can J Emerg Med. 2010;12(1):50–57. [DOI] [PubMed] [Google Scholar]
- 19. Sullivan P, Soefje S, Reinhart D, et al. Using lean methodology to improve productivity in a hospital oncology pharmacy. Am J Health-Sys Pharm. 2014;71(17):1491–1498. [DOI] [PubMed] [Google Scholar]
- 20. Naidoo L, Mohomed OH. Impact of lean on patient cycle and waiting times at a rural district hospital in KwaZulu-Natal. Afr J Prim Health Care Fam Med. 2016;8(1):1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Simons P, Backes H, Bergs J, et al. The effects of a lean transition on process times, patients, and employees. Int J Health Care Qual Assur. 2017;30(2):103–118. [DOI] [PubMed] [Google Scholar]
- 22. Poksinska BB, Fialkowska-Filipek M, Engstrom J. Does lean healthcare improve patient satisfaction? A mixed-method investigation into primary care. BMJ Qual Saf. 2017;26:95–103. [DOI] [PubMed] [Google Scholar]