Introduction
Scarcity of personnel protective equipment (PPE) around the world can compromise patient care and safety of caregivers during the Coronavirus disease 2019 (COVID-19) pandemic. This article suggests creative ideas from pharmacists to ration the use of PPE and limit the exposure for healthcare workers. The collaborative spirit, teamwork, sharing best prasctices and helping each other think of creative solutions will succeed in conquering COVID-19.
Standardization of Medication Administration and Routine Lab Investigation Timing
Standardizing and coinciding the medication administration times and drawing blood samples for routine labs, is a simple and effective PPE stewardship measure. In addition, switching medication administration times to routine nursing care time will also be beneficial.
Change the Frequency of Administration or Use Alternative Medications
Medications which have extended release formulations can ideally be initiated to reduce or avoid medication with more frequent dosing. Avoiding the use of medications which require therapeutic drug monitoring (TDM) and using alternative medications, helps to minimize drawing blood for drug levels. In case of exception, minimize the blood drawn for drug levels and use alternative strategies for higher drug dosing with lesser frequency. If stable medications that are being continued like antiepileptic and mood stabilizers, apply clinical judgment for dose titration and reduce the need for frequent TDM.
Administration of Metered Dose Inhalers (MDIs) Instead of Nebulization
Nebulized medications can generate aerosol and increase the risk of viral transmission. Administering MDIs with or without the use of spacer instead of nebulization reduces risk of exposure for nurses and respiratory therapists.1,2 MDIs can be self-administered by the patient or with the help of a caregiver. Upon patient discharge, the MDIs used during hospital stay should be discarded and if needed new MDIs should be prescribed to take home. In case of MDI shortage, nurse or the respiratory therapist can separate the canister from the plastic mouthpiece, thoroughly wipe the canister, plastic mouthpiece and spacer with disinfectant for 2 minutes each time after use. 3
Drug delivery system spacers for MDIs can be used for mechanically ventilated patients instead of nebulization machines which reduces aerosolized viral transmission and minimizes interruption during continued respiratory support for the patients. These delivery systems are collapsible volumizing chambers which remain in the inspiratory limb of the ventilatory circuit hence, reducing the risk of environmental contamination on disconnection. 4 Similar techniques can be used for bronchodilator administration while receiving non-invasive ventilation (NIV). 5
Maximize Drug Concentration or Increase the Bag Volume
Critically ill patients may require multiple continuous intravenous infusions which includes vasoactive agents, sedatives, analgesics, and neuromuscular blocking agents. Intervening to maximize the drug concentration based on recommendations or increasing the bag volume will help in minimizing frequent bag exchanges. It also restricts fluids especially in patients with acute respiratory distress syndrome to avoid fluid overload. It is important to administer the recommended maximum concentration through central venous catheter which will prevent thrombophlebitis or other safety issues, while the potential risk of extravasation injury must still be considered. 6 An example for maximizing Norepinephrine concentration would be by increasing from standard peripheral line concentration of 4 mg in 250 mL normal saline (NS) to central line concentration of 16 mg or 32 mg in 250 mL NS. An example for increasing the volume of a Dexmedetomidine bag would be from 400 mcg in 100 mL NS to 1000 mcg in 250 mL NS. Drug wastage can be avoided by using minimal concentration infusion bags for patients whom the infusion will be discontinued soon or for patients with low infusion flow rate. Maintaining proper stock of medications and cycling usage among the same class of drugs can help to avoid critical drug shortages.
Extended Tubing to Keep Infusion Pumps Outside Isolation Room
This recommendation comes from the practice of using extended tubing or administration sets to keep infusion pumps away from the scan room for patients undergoing magnetic resonance imaging (MRI). Infusion pump inside the scan room can become a projectile which can potentially harm the patient, healthcare personnel or it can cause significant damage to the MRI facility and environment. 7 Extrapolating this practice to implement extended tubing to keep infusion pumps in the hallway outside isolation rooms helps to minimize healthcare worker exposure and rationalize PPE use. Infusion flow rate challenges like frequent occlusion alarms or back flow of blood in the tubing need to be considered before implementing this strategy. Patient’s intravenous access can be checked whenever the nurse enters the isolation room for positioning the patient or for routine nursing care and assessment. Keeping infusion pumps in the hallway, makes it easy for the nurses to respond to pump alarms and for timely bag exchange without entering the patient’s room. Bedside barcode scanning may not be feasible while independent double check for high alert medications may be limited to the hallway.
Priming the tubing may require large volume; hence, small bore extended tubing can be used. Multiple extension tubing sets may be required for the infusion pump to reach the patient from the hallway. Y-site connectors can also be utilized to infuse compatible medications together via the same line. Securing all the tubing and taping it at each connection site gives a visual reminder thereby reducing the potential risk of any occupational hazard of tripping on the tubing or disconnecting it. However, the decision to implement the extended tubing strategy has to be individualized by balancing the benefits of PPE stewardship, caregiver exposure, patient infection risk and considering the local supply chain challenges, medication and infusion needs.
Antibiotics Given as Intravenous Push Instead of Intermittent Infusion
Administration of antibiotics as intravenous (IV) push instead of intermittent infusion needs to be considered whenever applicable. It is particularly helpful for patients with fluid restriction where IV push uses small volume of fluid for reconstitution. All antibiotics cannot be given as IV push considering the stability and complications associated with rapid push. Potential pharmacokinetic and pharmacodynamic disadvantages of administering beta lactam antibiotics as IV push and the substantial advantages with giving them as extended infusions should be considered prior to implementing this strategy. 8 Table 1 has listed details of antibiotics which can be given as IV push with recommended reconstitution and administration time.9,10
Table 1.
Details of Antibiotics which can be Given as IV Push with Recommended Reconstitution and Administration Time.
| Antibiotics | Reconstitution and IV push administration time | Comment |
|---|---|---|
| Amoxicillin/Clavulanic acid | ● Reconstitute each vial of 600 mg or 1.2 g with 10 mL or 20 mL of sterile water
for injection (SWFI) respectively and immediately administer the full volume over
3 to 5 minutes. ● No further dilution required for any of the above reconstituted solution. |
● Reconstituted solution for IV push is stable only for 20 minutes. |
| Ampicillin | ● Reconstitute each vial of 500 mg or less with 5 mL of SWFI and administer over
3 to 5 minutes. ● Reconstitute each vial of 1 g or 2 g with 7.4 mL or 14.8 mL of SWFI respectively and administer over 10 to 15 minutes. ● No further dilution required for any of the above reconstituted solution. |
● More rapid administration may lead to seizures. |
| Ampicillin/Sulbactam | ● Reconstitute each vial of 1.5 g or 3 g with 3.2 mL or 6.4 mL of SWFI
respectively. ● Further dilute the above reconstituted solution in normal saline (NS) to yield a concentration between 3 and 45 mg/mL (ampicillin sodium 2 to 30 mg/mL and sulbactam sodium 1 to 15 mg/mL). ● Final diluted solution can be administered over 10 to 15 minutes. |
● More rapid administration may lead to seizures. |
| Aztreonam | ● Reconstitute vials of 1 g or 2 g with 6 to 10 mL of SWFI and administer over 3
to 5 minutes. ● No further dilution required for any of the above reconstituted solution. |
● No significant issues were reported. |
| Cefazolin | ● Reconstitute each vial of 1 g with 7.5 mL of SWFI and administer over 3 to
5 minutes. ● No further dilution required for the above reconstituted solution. |
● No significant issues were reported. |
| Cefepime | ● Reconstitute each vial of 1 g or 2 g with 10 mL of SWFI. ● Further dilute the above reconstituted solution in NS to yield a concentration between 1 and 40 mg/mL. ● Final diluted solution can be administered over 5 minutes. |
● Localized phlebitis can occur. |
| Cefotaxime | ● Reconstitute each vial of 500 mg or 1 g or 2 g with 10 mL of SWFI and
administer over 3 to 5 minutes. ● No further dilution required for the above reconstituted solution. ● Maximum concentration for IV push is 200 mg/mL in SWFI. |
● Rapid administration of less than one minute through a central venous catheter can result in life-threatening arrhythmias. |
| Cefoxitin | ● Reconstitute each vial of 1 g or 2 g with 10 mL of SWFI and administer over 3
to 5 minutes. ● No further dilution required for the above reconstituted solution. |
● No significant issues were reported. |
| Ceftazidime | ● Reconstitute each vial of 500 mg, 1 g or 2 g with 5.3 mL, 10 mL or 10 mL of
SWFI respectively and administer over 3 to 5 minutes. ● No further dilution required for the above reconstituted solution. |
● No significant issues were reported. |
| Ceftriaxone | ● Reconstitute each vial of 1 g or 2 g with 9.6 mL or 19.2 mL of SWFI
respectively and administer over 5 minutes. ● No further dilution required for the above reconstituted solution. ● Do not administer simultaneously with calcium containing solutions, products or calcium containing infusions in the same IV line or Y-site due to risk of precipitate formation. |
● IV push only in patients above age of 12 years. |
| Cefuroxime | ● Reconstitute each vial of 750 mg or 1.5 g with 8.3 mL or 16 mL of SWFI
respectively and administer over 3 to 5 minutes. ● No further dilution required for the above reconstituted solution. |
● Localized phlebitis can occur. |
| Chloramphenicol | ● Reconstitute each vial of 1 g with 10 mL of SWFI and administer over one
minute. ● No further dilution required for the above reconstituted solution. |
● No significant issues were reported. |
| Colistimethate sodium | ● Reconstitute each vial of 150 mg with 10 mL of SWFI and administer over 3 to
5 minutes. ● No further dilution required for the above reconstituted solution. |
● No significant issues were reported. |
| Meropenem | ● Reconstitute each vial of 500 mg or 1 g with 10 mL or 20 mL of SWFI
respectively and administer over 3 to 5 minutes. ● No further dilution required for the above reconstituted solution. |
● No significant issues were reported. |
Disposable Pill Pouch
Disposable pill pouches labeled with patient identification, drug name, dose and administration time can be used for medication self-administration for stable patients in isolation rooms. Patients have to be thoroughly educated about this practice of self-administration prior to initiation. 11 These can be easily implemented in hospitals with a unit dose dispensing system.
Deactivating Biometric or Fingerprint Login for Automated Dispensing cabinet (ADC)
Hospitals with automated dispensing cabinets can consider deactivating the biometric identification (BioID) or fingerprint login and activate login through username with secured password. This helps reduce unnecessary PPE removal each time caregiver logs in to the ADC for removal or loading medication. Periodic cleaning of the ADC including the keyboard and scanner will reduce surface contamination. 12
Handling of Rapid Sequence Intubation (RSI) Kit and Emergency Crash Cart
During intubation, emergency response or cardiac arrest in COVID-19 confirmed or suspected patients, take only the required items while entering the isolation room. Prepare medications outside the isolation room and have a dedicated healthcare professional outside the isolation room to help with the necessary medications. This reduces contamination of the RSI kit or crash cart. If the RSI kit is contaminated, discard all disposable things within the room and clean the reusable or non-disposable things with wipes as recommended by equipment cleaning guidelines prior to its removal from the room. 13
Another strategy would be to refill or replace RSI kit or crash cart on the isolation unit, instead of returning or refilling these in the pharmacy. The healthcare provider on the isolation floor sends a request to the pharmacy electronically and pharmacy delivers the requested medications to the clean area on the floor. 12 The healthcare provider cleans the RSI kit or crash cart as recommended by equipment cleaning guidelines and replaces or refills the medications.
Telemedicine for Pharmacy Services
Virtual clinic appointments for patients with heart failure, diabetes mellitus, other chronic diseases, patients on anticoagulation, chemotherapy and transplant patients. Telemedicine helps to follow up with these patients regarding compliance with medications and discuss the signs and symptoms of the primary disease to titrate dose based on patient response. If the patient requires necessary labs to be done for titrating anticoagulation, transplant medications or any other medication, it can be requested to be completed from the nearby laboratory or clinic. 14 Admission medication reconciliation and discharge medication counselling via phone conversation or virtually with the patient.
Home Delivery of Medications
Home delivery of medications is equally beneficial for healthcare and community settings. 15 This protects the frontline pharmacy caregivers and community from unnecessary exposure. Home delivery can be facilitated for medication refills and first time use medications. If the first time use medication is complex and requires pharmacist usage instructions, either the pharmacist is available for these home deliveries or request the patient to collect medication from the pharmacy directly. If the first time use medication is not complex then, the pharmacist can explain usage instructions through phone conversation. Chemotherapy for patients can be rescheduled or organized in the nearby medical facility with instructions and complete details of the chemotherapy cycle. If necessary the chemotherapy and supportive care medications can be delivered to the nearby medical facility which makes it easy for the patient to acquire the medication. 16
Conclusion
Globally as we fight against a common enemy during this COVID-19 pandemic, our frontline healthcare workers are at risk of exposure. It is extremely important to ration the use of PPE to protect ourselves with the limited available resources. Implementing these simple and easy interventions in every healthcare facility which treats confirmed or suspected COVID-19 patients, helps to minimize unnecessary PPE wastage and limits caregiver exposure. These recommendations and suggestions are consolidated from detailed review of different practices across the globe, making sure the quality of patient care is not compromised.
Acknowledgments
The authors wish to thank Pia Beron, Pharmacy Technician for designing the poster (Figure 1).
Figure 1.
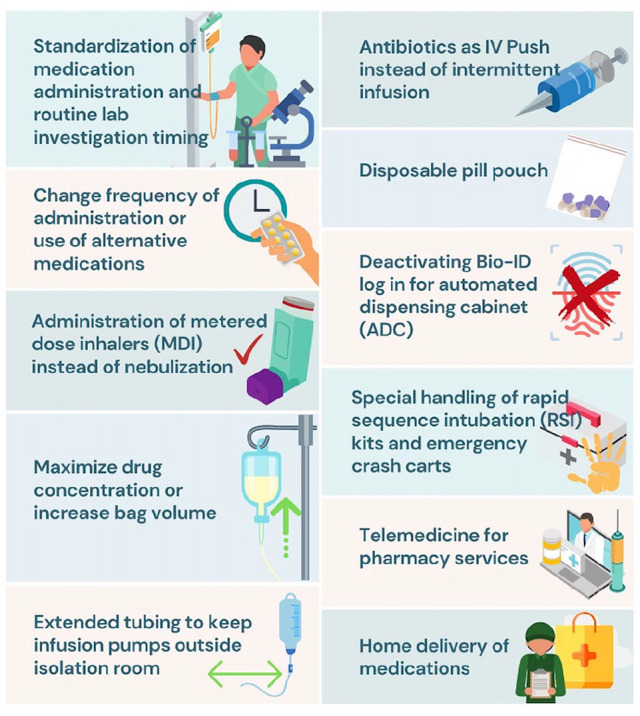
COVID-19 Pharmacy initiatives.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mohamed Hisham  https://orcid.org/0000-0003-0029-3707
https://orcid.org/0000-0003-0029-3707
References
- 1. Amirav I, Newhouse MT. Transmission of coronavirus by nebulizer: a serious, underappreciated risk. CMAJ. 2020;192(13):E346-E346. doi: 10.1503/cmaj.75066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Khoo SM, Tan LK, Said N, Lim TK. Metered-dose inhaler with spacer instead of nebulizer during the outbreak of severe acute respiratory syndrome in Singapore. Respir Care. 2009;54(7):855-860. http://www.rcjournal.com/contents/07.09/07.09.0855.pdf [DOI] [PubMed] [Google Scholar]
- 3. Larson T, Gudavalli R, Prater D, Sutton S. Critical analysis of common canister programs: a review of cross-functional considerations and health system economics. Curr Med. Res Opin. 2015;31:(4)853-860. doi: 10.1185/03007995.2015.1016604. [DOI] [PubMed] [Google Scholar]
- 4. Dhand R. How should aerosols be delivered during invasive mechanical ventilation? Respir Care. 2017;62(10):1343-1367. doi: 10.4187/respcare.05803. [DOI] [PubMed] [Google Scholar]
- 5. Rzepka-Wrona P, Skoczynski S, Wrona D, Barczyk A. Inhalation techniques used in patients with respiratory failure treated with noninvasive mechanical ventilation. Can Respir J. 2018;2018:8959370. doi: 10.1155/2018/8959370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cardenas-Garcia J, Schaub KF, Belchikov YG, Narasimhan M, Koenig SJ, Mayo PH. Safety of peripheral intravenous administration of vasoactive medication. J Hosp Med. 2015;10(9):581-585. doi: 10.1002/jhm.2394. [DOI] [PubMed] [Google Scholar]
- 7. Expert Panel on MR Safety; Kanal E, Barkovich J, Bell C, et al. ACR guidance document on MR safe practices: 2013. J Magn Reson Imaging. 2013;37(3):501-530. doi: 10.1002/jmri.24011. [DOI] [PubMed] [Google Scholar]
- 8. Spencer S, Ipema H, Hartke P, et al. Intravenous push administration of antibiotics: literature and considerations. Hosp Pharm. 2018;53(3):157-169. doi: 10.1177/0018578718760257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lexi-Drugs. Lexicomp. Riverwoods, IL: Wolters Kluwer Health, Inc.. Available at: http://online.lexi.com. Accessed April 9, 2020. [Google Scholar]
- 10. Trissel LA. Handbook on Injectable Drugs. 18th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2014. [Google Scholar]
- 11. Boeni F, Spinatsch E, Suter K, Hersberger KE, Arnet I. Effect of drug reminder packaging on medication adherence: a systematic review revealing research gaps. Syst Rev. 2014;3(1):29. doi: 10.1186/2046-4053-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. American Chemistry Council (ACC) Center for Biocide Chemistries (CBC) - Novel Coronavirus (COVID-19)—Fighting Products. https://www.americanchemistry.com/Novel-Coronavirus-Fighting-Products-List.pdf?mod=article_inline. Updated May 21, 2020. Accessed May 23, 2020.
- 13. Oxygenation and ventilation of COVID-19 patients. American Heart Association website. https://cpr.heart.org/en/resources/coronavirus-covid19-resources-for-cpr-training/oxygenation-and-ventilation-of-covid-19-patients. Updated April 9, 2020. Accessed April 11, 2020. [Google Scholar]
- 14. Jandovitz N, Li H, Watts B, Monteiro J, Kohlberg D, Tsapepas D. Telemedicine pharmacy services implementation in organ transplantation at a metropolitan academic medical center. Digit Health. 2018;4:2055207618789322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schmittdiel JA, Karter AJ, Dyer WT, Chan J, Duru OK. Safety and effectiveness of mail order pharmacy use in diabetes. Am J Manag Care. 2013;19(11):882-887. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4278640/. Assessed April 8, 2020. [PMC free article] [PubMed] [Google Scholar]
- 16. Corbett M, Heirs M, Rose M, et al. The delivery of chemotherapy at home: an evidence synthesis. In: Health Services and Delivery Research, No. 3.14. Southampton, UK: NIHR Journals Library; 2015. https://www.ncbi.nlm.nih.gov/books/NBK285513/doi:10.3310/hsdr03140. Assessed April 20, 2020. [PubMed] [Google Scholar]


