Abstract
Background
Improved access to and quality obstetric care in health facilities reduces maternal and neonatal morbidity and mortality. We examined spatial patterns, within-country wealth-related inequalities and predictors of inequality in skilled birth attendance and caesarean deliveries in sub-Saharan Africa.
Methods
We analysed the most recent Demographic and Health Survey data from 25 sub-Saharan African countries. We used the concentration index to measure within-country wealth-related inequality in skilled birth attendance and caesarean section. We fitted a multilevel Poisson regression model to identify predictors of inequality in having skilled attendant at birth and caesarean section.
Results
The rate of skilled birth attendance ranged from 24.3% in Chad to 96.7% in South Africa. The overall coverage of caesarean delivery was 5.4% (95% CI 5.2% to 5.6%), ranging from 1.4% in Chad to 24.2% in South Africa. The overall wealth-related absolute inequality in having a skilled attendant at birth was extremely high, with a difference of 46.2 percentage points between the poorest quintile (44.4%) and the richest quintile (90.6%). In 10 out of 25 countries, the caesarean section rate was less than 1% among the poorest quintile, but the rate was more than 15% among the richest quintile in nine countries. Four or more antenatal care contacts, improved maternal education, higher household wealth status and frequently listening to the radio increased the rates of having skilled attendant at birth and caesarean section. Women who reside in rural areas and those who have to travel long distances to access health facilities were less likely to have skilled attendant at birth or caesarean section.
Conclusions
There were significant within-country wealth-related inequalities in having skilled attendant at birth and caesarean delivery. Efforts to improve access to birth at the facility should begin in areas with low coverage and directly consider the needs and experiences of vulnerable populations.
Keywords: epidemiology, health economics, health policy, health systems, health services research
Key questions.
What is already known?
Improving access to and quality of obstetric care at facilities is a priority.
Several countries have shown shifts from home deliveries to facility deliveries in the past decade.
What are the new findings?
There were significant pro-rich inequalities in skilled birth attendance and caesarean section.
In most countries, the coverage of caesarean section was extremely low, particularly among the poorer populations.
Women who had a skilled birth attendance or caesarean delivery were more likely to be educated, have access to mass media (television), have four or more ANC contacts, be residents of an urban area or have better geographical access to a health facility.
What do the new findings imply?
Efforts to improve access to obstetric care should start in areas with low coverage and directly consider the needs and experiences of vulnerable populations.
Improving the quality of care to increase the uptake of facility-based delivery.
Country-specific strategies are critical to addressing these inequalities to improve maternal and newborn health.
Introduction
Women and children in sub-Saharan Africa are the most vulnerable subgroups and have limited access to quality reproductive, maternal, neonatal and child health services.1 2 In 2017, 295 000 women died from preventable causes related to pregnancy and childbirth and 2.6 million babies died within the first month of their life worldwide.1 Of those, 195 000 (66%) women and 988 000 (38%) newborns were from sub-Saharan Africa.1 Within countries, the risk of death is disproportionately high among the most vulnerable subgroups.1 3 4 The majority of these deaths can be averted by improving access to quality health services.2 5 While encouraging progress has been made to increase access to health services and reduce maternal and child mortality, preventable deaths are still occurring in sub-Saharan Africa.1 2 6
Successful, consistent and continuous reduction of maternal and child mortality requires improving access to quality maternal and child health services along the continuum of care.6–8 A critical intervention is ensuring that a health worker with midwifery skills is present at every birth and transportation is available in case of emergency.2 9 In the past decade, the world has seen remarkable growth in the number of health facilities and improvements in health infrastructures and access to transport services. These have led to considerable improvements in maternal and child health indicators in some countries (eg, Rwanda), but in many other countries, expectations were not met and targets were not achieved.10 11
Growing evidence from a number of countries has shown significant shifts from home deliveries to facility deliveries in the past decade.12 However, extreme disparities in the use of maternal and child health services continue to exist across regions, within and between countries.11 13 Inequalities in access to and quality of healthcare exist along with the factors such as wealth, geography, gender, religion, ethnicity and race that put some people at a social disadvantage relative to others and places them at risk for discrimination and unequal treatment.14 15
Medically indicated caesarean section (CS) is a life-saving intervention for women and newborns.16 Globally, CS use has increased during the past few decades to a frequency exceeding of the proportion of 10%–15% of births that is thought to be optimal.3 16 A major growth in the rate of non-medically indicated CS in many middle-income and high-income countries has driven the increased use of this procedure.16 However, in low-income countries in general and among the poorer sections of the populations—CS are not always accessible, even when they are clearly indicated.17
The global maternal mortality ratio (MMR) decreased from 385 deaths per 100 000 live births in 1990 to 211 per 100 000 live births in 2017, but there were important regional disparities.1 In 2017, the MMR in sub-Saharan Africa was 542 per 100 000 live births, nearly 26 times the rate in high-income countries.1 The Sustainable Development Goal 3, which focuses on health, aims to reduce the global MMR to less than 70 deaths per 100 000 live births.18 This rate might be difficult to achieve unless disparities are identified at a basic level to determine how health system operations, planning and programming for maternal health and service distribution result in inequitable health outcomes. Hence, closer examination of drivers of disparities in access to critical interventions such as skilled birth attendance (SBA) and CS will inform the planning and programming effort to address inequitable access to maternal health services. We aim to address this gap in knowledge of these disparities by systematically examining spatial patterns, inequalities and predictors of SBA and CS in sub-Saharan Africa.
Methods
Data
We used the most recent Demographic and Health Surveys (DHS) collected from 25 sub-Saharan African countries. The DHS programme uses standardised methods to ensure uniformity of data collected across time and countries. We included all DHS that were conducted from 2013 to 2020. Countries are expected to adopt the full standard model questionnaire, but they can add questions of particular interest. However, questions in the model can be deleted if they are irrelevant for a specific country. The DHS uses standard sampling methods and design across all countries. The sampling methods and design have been described elsewhere.19 The study population includes all women of reproductive age (15–49 years) who had at least one live birth during the 5 years preceding the respective surveys. Only the most recent live birth was included in this analysis to reduce recall bias.
Outcomes
We examined two primary outcomes: birth assisted by skilled attendant and delivery by CS. SBA was defined as whether the delivery took place in the presence of qualified personnel: a doctor, nurse, midwife, auxiliary midwife or other cadres that each country individually considers as skilled delivery attendants. Data on assistance at birth in the survey questionnaires were collected through answers to the question ‘Who assisted with the delivery of (NAME OF THE CHILD)? Information on caesarean sections are based on women’s self-reported answer to the question: ‘Was (NAME OF THE CHILD) delivered by caesarean, that is, did they cut your belly open to take the baby out?”
We also assessed disparities in place of delivery and type of facility (private vs public). Place of delivery was defined as—birth at home that includes the respondent’s home or another non-institutional setting or birth at a health facility (institutional delivery), which may include public health facilities or the private medical sector. Public sector deliveries are those occurring in publicly funded, government health facilities. Private sector births are those occurring in facilities outside the public sector, and can be further divided into two categories: private-for-profit facilities and private not for profit facilities.
Covariates
We used the WHO Commission on Social Determinants of Health framework to explain predictors of inequality in the use of SBA and CS.15 We used household wealth index and education levels to explain socioeconomic position of women. The wealth index was constructed using principal components analysis based on ownership of selected household assets such as television (TV), radio, refrigerator and vehicle; materials used for housing construction; and access to sanitation facilities and clean water. Households were ranked into quintiles from the poorest (Q1) to richest (Q5) depending on their level of wealth. We categorised mothers’ education levels as (no education, primary, secondary or higher). We determined accessibility to health facilities based on the distance to the facility, and ability to afford treatment costs. We considered the distance to a health facility and lack of money for treatment as barriers to accessing health services and categorised—as a big problem or not a big problem. We include exposure to media, which was categorised based on the frequency of reading newspapers, listening to the radio and watching TV as not at all, less than once a week, and once a week or more. We also included the use of antenatal care (ANC) that was categorised as three or fewer contacts, and four or more contacts. Type of place of residence were categorised as urban or rural. Lastly, maternal factors such as age (15–24, 25–29, 30–34) and parity (1–6) were also included in the analysis.
Statistical analysis
We used concentration index (CCI) to estimate wealth-related within-country inequalities in SBA and CS. The CCI ranges between −1 and +1; an index of 0 indicate equality in having SBA or CS. A positive values of CCI indicate a pro-rich coverage of SBA or CS. In contrast, a negative index implies an uneven concentration of SBA among the poor.20
The DHS uses a stratified, two-stage, random sampling design in all countries. Sample weights are included in the DHS to translate unbalanced sampling into national representative data. We used generalised latent linear and mixed model that adjusted for country, clusters and sampling weights to fit multilevel Poisson regression. We specified a three-level model to examine predictors of inequality in SBA and CS. For the first outcome (SBA) models—at level 1, we adjusted for women and household factors (181 191 women); at level 2, we adjusted for clustering (14 643 clusters) and at level 3, we adjusted for a country (25 countries). For the CS models—level 1 included 1 80 837 women; level 2 had 14 643 clusters and level 3 covered 25 countries. Results are presented with adjusted risk ratio (RR) and statistical significance was declared when the p value was <0.05. Analyses were conducted using Stata V.14.2 and IBM Statistical Package for Social Sciences (SPSS) V.25.0. We generated maps using ArcGIS software V.10.7.1.
Patient and public involvement
No patients or the public were directly involved in the design, conduct, reporting or dissemination plans of this research.
Results
We analysed data on 2 88 730 women who had a live birth. We used the most recent (2013–2020) DHSs conducted in 25 sub-Saharan African countries. The majority of women were from rural areas (69%), 56.5% had four or more ANC contacts and 63.7% delivered at health facility.
Inequality in the coverage of SBA
Overall, 63.9% (95% CI 63.1% to 64.7%) of women received assistance during childbirth from a skilled attendant. Of those who received no assistance from a SBA, 17.6% of women (95% CI 17.1% to 18.2%) received care from a traditional birth attendant (TBA), 12.3% (95% CI 11.3% to 12.8%) from a friend or relative and 4.9% (95% CI 4.7% to 5.2%) received no assistance.
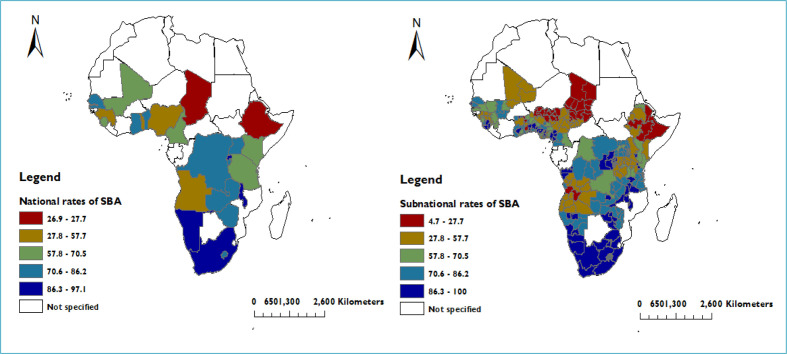
The coverage of SBA ranged from 24.3% in Chad to 96.7% in South Africa (figure 1). The proportion of women who had a SBA was higher than 85% in countries such as Namibia, Malawi, Rwanda and South Africa but, coverage was less than 50% in Angola, Togo, Nigeria, Ethiopia and Chad. Three in seven deliveries were assisted by a midwife or nurse, while only 1 in 10 deliveries were assisted by a physician. More than three-quarters (78.2%, 95% CI 77.6% to 78.8%) of women with four or more ANC contacts received skilled provider assistance during childbirth.
Figure 1.
National and sub-national rates of skilled birth attendance (SBA) in 25 sub-Saharan African countries.
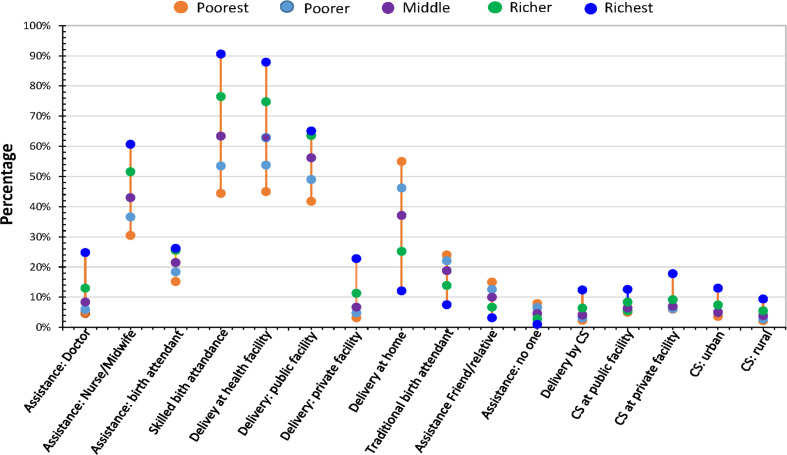
The wealth-related absolute inequality for all countries in having a SBA was extremely high, with a difference of 46.2 percentage points between the poorest quintile (44.4%) and the richest quintile (90.6%) (figure 2). In four countries, the differences exceeded 65 percentage points: Guinea (68.4 percentage points), Cameroon (69.4 percentage points), Angola (72.4 percentage points) and Togo (76.1 percentage points).
Figure 2.
Skilled attendant at birth and caesarean delivery rates by socioeconomic status, providers and place of service. Providers or place of service, represented by five circles (one for each wealth subgroup). Vertical lines indicate the difference between the minimum and maximum rate by provider or place of service (DHS 2013–2021). CS, caesarean section; DHS, Demographic and Health Survey.
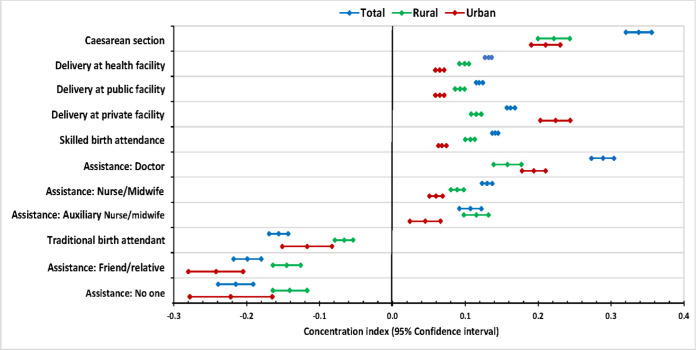
Figure 3 shows statistically significant positive CCI values across all countries that reveal pro-rich wealth-related within-country inequalities in SBA and CS. We observed strong pro-rich distributions of skilled attendants at birth and caesarean deliveries between and within all 25-study countries. Overall, we found that as coverage increased, inequalities decreased. For example, countries such as South Africa, Rwanda and Malawi that had more than 90% coverage of a SBA showed the lowest inequalities: South Africa (CCI 0.013, 95% CI 0.008 to 0.017), Rwanda (CCI 0.025 95% CI 0.02 to 0.031) and Malawi (CCI 0.016, 95% CI 0.012 to 0.02). On the other hand, countries such as Togo, Nigeria, Ethiopia and Chad that had lower coverage (50% or less), exhibited higher inequalities: Togo (CCI 0.371, 95% CI 0.351 to 0.391), Nigeria (CCI 0.35, 95% CI 0.337 to 0.362), Ethiopia (CCI 0.315, 95% CI 0.279 to 0.351) and Chad (CCI 0.292, 95% CI 0.259 to 0.325).
Figure 3.
Concentration indices for skilled birth attendance and caesarean section across 25 sub-Saharan African countries (DHS 2013–2020). DHS, Demographic and Health Survey.
Table 1 shows predictors of a skilled attendant at birth in 25 sub-Saharan African countries. Four or more ANC contacts, higher levels of maternal education, improved access to mass media (radio or TV), and higher household wealth status were associated with increased rates of SBA. While long distances to health facilities and residing in rural areas showed associations with lower rates of SBA. We found higher utilisation rates among women who had four or more ANC contacts (RR 1.26, 95% CI 1.16 to 1.36) compared with women who had three or lower ANC contacts. With increasing levels of maternal education, the rates of SBA also increased; women who had secondary or higher education had 31% higher rates of (RR 1.31, 95% CI 1.16 to 1.49) SBA compared with women who had no education. The rates of SBA increased with increasing levels of household wealth status: women in the poorer fifth had higher rates of (RR 1.12, 95% CI 1.06 to 1.18), middle (RR 1.22, 95% CI 1.12 to 1.33), richer (RR 1.29, 95% CI 1.17 to 1.42) and richest fifth (RR 1.27, 95% CI 1.13 to 1.43) SBA compared with the poorest fifth.
Table 1.
Factors associated with the use of skilled birth attendance in sub-Saharan Africa
| Variables | No | Percentage | Assisted by skilled attendant | Unadjusted RR (95% CI) | P value | Adjusted RR (95% CI) | P value |
| Age groups | <0.001 | 0.199 | |||||
| 15–24 | 82 375 | 28.1 | 66.0 (65.1, 66.8) | 1.0 (Reference) | 1.0 (Reference) | ||
| 25–29 | 80 700 | 27.6 | 64.8 (63.9, 65.7) | 0.97 (0.96 to 0.98) | 0.98 (0.96 to 1.00) | ||
| 30–34 | 62 243 | 21.2 | 64 (63.1, 65.0) | 0.95 (0.93 to 0.97) | 0.98 (0.95 to 1.01) | ||
| 35–49 | 67 600 | 23.1 | 60.2 (59.3, 61.1) | 0.92 (0.90 to 0.94) | 0.97 (0.93 to 1.01) | ||
| No of antenatal contacts | <0.001 | <0.001 | |||||
| Less than 4 ANC | 85 674 | 43.5 | 52.4 (51.4, 53.4) | 1.0 (Reference) | 1.0 (Reference) | ||
| Four or more 4 ANC | 111 190 | 56.5 | 78.2 (77.6, 78.8) | 1.34 (1.22 to 1.48) | 1.26 (1.16 to 1.36) | ||
| Highest educational level | <0.001 | <0.001 | |||||
| No education | 109 926 | 37.5 | 43 (42.0, 44.3) | 1.0 (Reference) | 1.0 (Reference) | ||
| Primary | 102 614 | 35 | 68.2 (67.4, 69.0) | 1.25 (1.13 to 1.37) | 1.21 (1.10 to 1.33) | ||
| Secondary | 80 376 | 27.4 | 86.2 (85.7, 86.7) | 1.48 (1.30 to 1.68) | 1.31 (1.16 to 1.49) | ||
| Wealth index combined | <0.001 | <0.001 | |||||
| Poorest | 66 498 | 22.7 | 44.3 (43.1, 45.4) | 1.0 (Reference) | 1.0 (Reference) | ||
| Poorer | 63 843 | 21.8 | 53.5 (52.3, 54.7) | 1.16 (1.10 to 1.23) | 1.12 (1.06 to 1.18) | ||
| Middle | 58 843 | 20.1 | 63.7 (62.7, 64.8) | 1.32 (1.17 to 1.48) | 1.22 (1.12 to 1.33) | ||
| Richer | 54 794 | 18.7 | 76.4 (75.4, 77.4) | 1.53 (1.31 to 1.79) | 1.29 (1.17 to 1.42) | ||
| Richest | 48 940 | 16.7 | 90.5 (89.8, 91.2) | 1.79 (1.51 to 2.11) | 1.27 (1.13 to 1.43) | ||
| Frequency of listening to radio | <0.001 | 0.026 | |||||
| Not at all | 129 066 | 44.1 | 53.3 (52.3, 54.4) | 1.0 (Reference) | 1.0 (Reference) | ||
| Less than once a week | 56 127 | 19.2 | 69.5 (68.5, 70.5) | 1.11 (1.06 to 1.17) | 1.04 (1.01 to 1.07) | ||
| At least once a week | 107 553 | 36.7 | 74.1 (73.4, 74.8) | 1.15 (1.10 to 1.21) | 1.02 (1.00 to 1.04) | ||
| Frequency of watching television | <0.001 | <0.001 | |||||
| Not at all | 188 316 | 64.4 | 55.1 (54.1, 56.0) | 1.0 (Reference) | 1.0 (Reference) | ||
| Less than once a week | 34 970 | 12 | 72.1 (71.0, 73.1) | 1.18 (1.10 to 1.26) | 1.08 (1.03 to 1.13) | ||
| At least once a week | 69 273 | 23.7 | 84.6 (83.9, 85.3) | 1.32 (1.21 to 1.43) | 1.12 (1.07 to 1.17) | ||
| Getting money needed for treatment | <0.001 | 0.328 | |||||
| No problem | 122 616 | 45.6 | 72.7 (71.9, 73.5) | 1.0 (Reference) | 1.0 (Reference) | ||
| Big problem | 146 152 | 54.4 | 59.8 (58.8, 60.7) | 0.91 (0.88 to 0.93) | 1.01 (0.99 to 1.02) | ||
| Distance to health facility | <0.001 | <0.001 | |||||
| No problem | 163 581 | 60.9 | 72.5 (71.7, 73.3) | 1.0 (Reference) | 1.0 (Reference) | ||
| Big problem | 105 181 | 39.1 | 55.0 (53.9, 56.0) | 0.88 (0.81 to 0.96) | 0.92 (0.89 to 0.95) | ||
| Type of place of residence | <0.001 | <0.001 | |||||
| Urban | 90 751 | 31 | 82.7 (81.7, 83.6) | 1.0 (Reference) | 1.0 (Reference) | ||
| Rural | 202 166 | 69 | 55.6 (54.7, 56.6) | 0.56 (0.49 to 0.64) | 0.84 (0.79 to 0.90) | ||
RR adjusted for the dependent variable—skilled birth attendance.
ANC, antenatal care; RR, risk ratio.
The rates of using a SBA were lower for women who reported long distance to a health facility as a big problem (RR 0.92, 95% CI 0.89 to 0.95) compared with women who thought distance to health facility was not a big problem. Women living in rural areas had (RR 0.84, 95% CI 0.79 to 0.90) lower rates of SBA compared with women living in urban areas.
Inequalities in the coverage of caesarean delivery
The overall average coverage of caesarean deliveries across all countries was 5.4% (95% CI 5.2% to 5.6%), ranging from 1.4% in Chad to 24.2% in South Africa (figure 4). Across all countries except for South Africa, the national caesarean delivery rate was less than 15%. In 10 (40%) countries, the national coverage was less than 5%. Ethiopia and Chad reported the lowest (less than 2%) national rates.
Figure 4.
National and subnational coverage of caesarean delivery in 25 sub-Saharan African countries. CS, caesarean section.
The overall wealth-related absolute inequality in CS showed 10 percentage points difference between the poorest fifth and richest fifth (figure 2). In three countries, the differences exceeded 20 percentage points: South Africa (21.9 percentage points), Namibia (28.6 percentage points) and Ghana (23.9 percentage points).
We found high wealth-related inequalities in caesarean deliveries within all the 25 sub-Saharan African countries analysed. Coverage of CS was low across all countries and socioeconomic levels. The highest wealth-related inequalities were reported in Ethiopia (CCI 0.491, 95% CI 0.364 to 0.618) and Nigeria (CCI 0.568, 95% CI 0.481 to 0.654), while Rwanda and South Africa that had higher coverage showed much lower wealth-related inequalities.
Figure 5 shows wealth-related inequalities in birth assistance providers, place of delivery and CS in 25 sub-Saharan Africa countries. The positive CCIs show pro-rich coverage in delivery at a health facility, CS and SBA. While the distribution of delivery assisted by TBAs, friends/relatives or women assisted by no one showed disproportionate concentration among disadvantaged women.
Figure 5.
Concentration indices for providers of birth assistance and caesarean section in sub-Saharan Africa (DHS 2013–2020). DHS, Demographic and Health Survey.
Table 2 shows predictors of delivery by CS. We found that older age women, higher levels of maternal education, frequently watching TV and higher household wealth were associated with increased rates of CS. By contrast, higher parity and residing in rural areas showed associations with lower rates of CS.
Table 2.
Factors associated with the use of caesarean section in sub-Saharan Africa
| Variables | Had caesarean section | Unadjusted RR (95% CI) | P value | Adjusted RR (95% CI) | P value |
| Age | <0.001 | 0.003 | |||
| 15–24 | 4.8 (4.6, 5.0) | 1.0 (Reference) | 1.0 (Reference) | ||
| 25–29 | 5.4 (5.2, 5.7) | 1.09 (1.02 to 1.17) | 1.50 (1.40 to 1.61) | ||
| 30–34 | 5.8 (5.5, 6.1) | 1.15 (1.03 to 1.28) | 2.09 (1.85 to 2.37) | ||
| 35–49 | 5.7 (5.4, 6.0) | 1.19 (1.03 to 1.37) | 3.04 (2.58 to 3.59) | ||
| Birth order no (parity) | <0.001 | 0.001 | |||
| 1 | 8.6 (8.3, 8.9) | 1.0 (Reference) | 1.0 (Reference) | ||
| 2 | 6.7 (6.4, 7.0) | 0.79 (0.75 to 0.83) | 0.68 (0.64 to 0.72) | ||
| 3 | 5.5 (5.2, 5.8) | 0.72 (0.66 to 0.78) | 0.51 (0.47 to 0.56) | ||
| 4 | 4.0 (3.7, 4.3) | 0.57 (0.51 to 0.62) | 0.37 (0.33 to 0.41) | ||
| 5 | 3.0 (2.8, 3.3) | 0.47 (0.42 to 0.54) | 0.28 (0.24 to 0.34) | ||
| 6th or higher | 2.6 (2.4, 2.8) | 0.45 (0.40 to 0.51) | 0.26 (0.22 to 0.31) | ||
| No of antenatal contacts during pregnancy | <0.001 | <0.001 | |||
| Fewer than 4 ANC | 3.6 (3.4, 3.8) | 1.0 (Reference) | 1.0 (Reference) | ||
| Four or more 4 ANC | 8.1 (7.9, 8.4) | 1.87 (1.60 to 2.18) | 1.45 (1.31 to 1.60) | ||
| Highest educational level | <0.001 | <0.001 | |||
| No education | 2.2 (2.1, 2.4) | 1.0 (Reference) | 1.0 (Reference) | ||
| Primary | 4.9 (4.6, 5.1) | 1.51 (1.29 to 1.77) | 1.17 (1.02 to 1.34) | ||
| Secondary | 10.3 (9.9, 10.7) | 2.90 (2.38 to 3.54) | 1.35 (1.16 to 1.56) | ||
| Wealth index combined | <0.001 | <0.001 | |||
| Poorest | 2.3 (2.2, 2.5) | 1.0 (Reference) | 1.0 (Reference) | ||
| Poorer | 3.1 (2.9, 3.3) | 1.29 (1.13 to 1.48) | 1.17 (1.06 to 1.28) | ||
| Middle | 4.2 (3.9, 4.5) | 1.69 (1.37 to 2.07) | 1.32 (1.17 to 1.48) | ||
| Richer | 6.6 (6.2, 6.9) | 2.58 (2.07 to 3.23) | 1.65 (1.46 to 1.87) | ||
| Richest | 12.6 (12.1, 13.2) | 4.75 (3.66 to 6.18) | 2.14 (1.84 to 2.49) | ||
| Frequency of listening to radio | <0.001 | 0.110 | |||
| Not at all | 3.4 (3.2, 3.6) | 1.0 (Reference) | 1.0 (Reference) | ||
| Less than once a week | 6.0 (5.7, 6.3) | 1.36 (1.23 to 1.50) | 1.06 (0.97 to 1.15) | ||
| At least once a week | 7.5 (7.3, 7.8) | 1.46 (1.33 to 1.60) | 1.00 (0.92 to 1.08) | ||
| Frequency of watching television | <0.001 | <0.001 | |||
| Not at all | 3.4 (3.3, 3.6) | 1.0 (Reference) | 1.0 (Reference) | ||
| Less than once a week | 6.5 (6.1, 7.0) | 1.61 (1.42 to 1.83) | 1.14 (1.04 to 1.24) | ||
| At least once a week | 10.3 (9.9, 10.7) | 2.36 (2.10 to 2.65) | 1.21 (1.10 to 1.33) | ||
| Lack of money for treatment | <0.001 | <0.001 | |||
| No problem | 7.0 (6.8, 7.3) | 1.0 (Reference) | 1.0 (Reference) | ||
| Big problem | 3.9 (3.7, 4.1) | 0.70 (0.66 0.75) | 0.93 (0.87 to 0.99) | ||
| Distance to health facility | <0.001 | 0.091 | |||
| No problem | 6.4 (6.2, 6.7) | 1.0 (Reference) | 1.0 (Reference) | ||
| Big problem | 3.6 (3.4, 3.8) | 0.72 (0.66 to 0.78) | 0.99 (0.92 to 1.06) | ||
| Type of place of residence | <0.001 | <0.001 | |||
| Urban | 9.5 (9.1, 9.9) | 1.0 (Reference) | 1.0 (Reference) | ||
| Rural | 3.6 (3.4, 3.7) | 0.35 (0.30 to 0.40) | 0.81 (0.75 to 0.88) |
RR adjusted for the dependent variable—delivery by caesarean section.
ANC, antenatal care; RR, risk ratio.
We found higher rates of CS among women who had four or more ANC contacts (RR 1.45, 95% CI 1.31 to 1.60) compared with those who had three or lower ANC contacts. The rates of CS increased with increasing levels of maternal education and rising household wealth: women in the wealthiest fifth quintile had the highest rate (RR 2.14, 95% CI 1.84 to 2.49), followed by richer (RR 1.65, 95% CI 1.46 to 1.87), middle (RR 1.32, 95% CI 1.17 to 1.48) and the poorer fifth (RR 1.17, 95% CI 1.06 to 1.28) compared with the poorest fifth quintile. On the other hand, women living in rural areas had (RR 0.81, 95% CI 0.75 to 0.88) lower CS rates than women living in urban areas.
Discussion
We observed differences in the rates of SBA and CS across countries. While some countries showed remarkable achievements, others are expected to expand and improve access and use of these services. Within countries, there were significant geospatial and wealth-related inequalities. The majority of sub-Saharan African countries have implemented free maternal and child health policies.21 However, many women still face considerable difficulty accessing services as they are exposed to direct costs (eg, payments for medication and laboratory tests) and indirect costs (eg, transportation).21 In countries such as Angola, Togo, Nigeria and Ethiopia that reported low rates of SBA and CS, we found strong pro-rich inequalities. In these countries, the World Bank reports that out of pocket health expenditure exceeds 35% of current expenditure and is as high as 62% in Chad and 77% in Nigeria suggesting a high burden of cost on the poor.22 Geospatial inequalities can partly be explained by the common features shared across areas with low coverage that involves less developed basic infrastructures such as health facilities, schools, electricity and roads.23 Low coverage is also common among communities that move from place to place.23
More than three-quarters of women who received birth assistance from skilled providers were attended by either a midwife, nurse or doctor. The remainder of women received assistance from other health professionals, considered by each country to be skilled delivery attendants, but who might not be as skilled as midwives, nurses or doctors.24 In addition, they might lack the necessary training or capacity to handle emergency procedures. For example, health extension workers in Ethiopia work in less equipped facilities and, in many cases, might not even have water supply and electricity to provide quality delivery service.25 While those health professionals are critical to providing services to the most vulnerable and difficult to reach communities, it is vital to increase the capacity of facilities with more highly qualified staff.
In South Africa, Rwanda and Malawi the rates of SBA were greater than 90%. South Africa is one of the richest countries in Africa, which could explain the high rates of SBA. In Rwanda, successes in expanding community-based health insurance, also known as Mutuelles, might have played a significant role in increasing the rates of SBA.26 27 Rwanda implemented policies that restricted home deliveries; this policy was integrated with facility improvements in infrastructure and workforce, better medicines, lowered costs and information campaigns.28 Malawi issued Community Guidelines in 2007 that prohibited the use of TBAs for routine deliveries and promoted SBA.29 The banning of TBAs may have pushed women to seek a facility-based delivery.30 Malawi has now revoked these policies that restricted TBAs. However, the introduction of these policies has brought significant changes over a decade. The SBA coverage increased in Malawi and Rwanda from below 30% to higher than 90% of all births delivered in clinics, hospitals and maternity homes. The implementation of these policies has been challenging in other several sub-Saharan African countries.9
There are many reasons why women in most sub-Saharan African countries experience delays in seeking quality obstetric care.7 A framework presented by Thaddeus and Maine31 suggested three phases of delay to accessing obstetric care1: delays in seeking care2; delays in reaching care and3 delays in receiving care.31 Bohren et al expanded this three-delay model to include the impact of disrespect and abuse on intrapartum care-seeking behaviours and how a woman’s decision to seek care is influenced by their perceptions of the quality of care provided by traditional providers and facility-based health workers.7
Long distances to the health facilities and issues with health referral systems also cause delays in accessing care.8 We found that women who had to travel long distances to a facility were less likely to access both SBA and CS compared with women who did not report distance as a problem. For example, in the Ethiopian three-tier health system, normal delivery services are provided at the primary healthcare units, including health centres.32 However, many women bypass these primary facilities and attend secondary level facilities as they wish to receive better quality services.33 This creates a high volume of clients attending a limited number of facilities resulting in poor-quality service delivery and facility overload. The excessive demand means that women cannot use the limited number of delivery suites leading to deliveries in waiting rooms or corridors.34 35 Evidence from Zambia and Tanzania has also shown how women regularly bypass community clinics to reach first-level hospitals searching for quality services.36 37 Despite substantial additional time and financial costs to the patient, high bypassing rates could indicate significant gaps in health system efficiency and coverage of health services.37 38
Health facility and provider factors that delay receiving care and potentially lower women’s trust in the health systems include poor quality of services exacerbated by disrespect and abuse during childbirth.7 Women have reported verbally and physically abusive providers who are disrespectful and lack compassion and care during childbirth.39 Women have expressed additional concerns regarding facility birth, including exposure to unnecessary surgical interventions (episiotomy or CS), unfamiliar birthing positions and undesirable and intrusive physical examinations.7 39 These negative interactions with providers and exposure to undesirable procedures were heightened for women of low socioeconomic status.34
Evidence suggests CS rates of 10%–15% capture the ideal desirable rates at the population level. We found the highest national rates in Ghana (12.8%), Rwanda (13.0%), Namibia (14.6%) and South Africa (24.2%). The majority of countries (56%) reported CS rates of 5%–15%. A very low rate of CS (<5%) is indicative of poor access to surgical care, that will lead to maternal and neonatal deaths from preventable causes.16 40 Of all births, 1%–2% are associated with conditions such as placenta previa and obstructed labour that require lifesaving CS.41 The very low CS rates reported in some countries might indicate a lack of access, particularly for low-income women. We found rates of less than 3% in Nigeria, Mali, Gambia, Ethiopia and Chad. In 10 (40%) countries, the rate of CS was less than 1% among the poorest quintile but the rate was more than 15% among the richest quintile in nine countries. Such inequalities must be urgently addressed.
Our study demonstrated that socioeconomic factors causing delay in seeking care make significant contributions to disparities in SBA and CS. We found that maternal education, household wealth status and access to mass media were significant predictors of SBA and CS uptake. Having four or more ANC contacts positively influenced the use of SBA and caesarean deliveries. There is strong evidence that the use of quality ANC improves maternal and newborn health outcomes.9 14 15 Having higher levels of education and access to mass media (ie, watching TV) positively influenced the uptake of SBA and CS. Education and mass media are important tools to create awareness and promote health service use.14 Women from rural areas were less likely to have both SBA and CS compared with women residing in urban areas. This finding is consistent with those of earlier studies17 42 and could result from a less developed health infrastructure and fewer skilled providers in rural areas.43 Some studies have also suggested that women from rural areas who attend urban health facilities are more likely to be treated poorly.39
While there is a need for multifaceted interventions to address persistently high rates of maternal and neonatal mortality in sub-Saharan Africa, a lack of capacity and funding and constant challenges of policy change make it difficult to implement well integrated strategies. However, some of these policies can be implemented in a phased manner. Examples include cash incentives in India,44 policies that restrict home deliveries with TBAs in Malawi and Rwanda,28 29 user fee exemptions in many sub-Saharan African countries with a slower follow-up of quality improvements, communication and referral links, outreach health education and transportation funds.
Based on our findings, we make the following policy recommendations. First, strengthening referral systems by expanding delivery services at mid-level facilities and reduce the number of low-quality deliveries at rural facilities. Improvements in the workforce, equipment and supplies in health facilities are core strategies for maternal and child health services in most countries.43 45 These strategies will strengthen lower-level facilities and reduce women’s desire to bypass the nearest primary care facility to seek care in higher-level facilities that places a large financial burden on the most vulnerable families.8 Sometimes women bypass primary facilities to seek care at private facilities because of perceived poor quality care. However, private facilities may not always provide higher quality services and may expose women to out-of-pocket expenditure. Second, there is a need to improve access for vulnerable rural women through funding for transport infrastructure, and targeted subsidies for services.8 44 For example, in 2005, India implemented a national conditional cash transfer programme, known as Janani Suraksha Yojana that increased SBA by 5%–44%, which was highly variable by state.44 Third, a strong focus on quality improvements at all levels of delivery facilities, with a focus on ensuring and achieving respectful, non-abusive and high-quality intrapartum care for all women.7 39 We believe addressing concerns related to low-quality or disrespectful care at facilities would remove an important barrier to facility birth for many women. Fourth, increasing specialised maternity facilities and dedicated maternity wards within larger institutions are needed.
The strengths of our study include the use of a large sample size involving multiple nationally representative population-based surveys collected from 25 sub-Saharan African countries. Most multicountry studies in this area have only focused on addressing wealth related inequalities. Our analysis examined spatial patterns, wealth-related within-country inequalities and critical contributions of other social determinants of health such as maternal education, access to media, use of ANC, place of residence and distance to a health facility. The limitations of our study include using data from the DHSs based on a recall period of 5 years. Second, clinical indications for CS were not available as there was no data to identify whether the procedure was an elective or emergency CS. Third, we used the most recent data available from the DHSs, which dates back to 2013 for some countries, and there may be differences in the current rates for some countries.
Conclusions
Facility-based childbirth is a priority global health agenda. There are encouraging signs of progress and indications that facility-based delivery could become the new normal in most sub-Saharan Africa countries. However, continued efforts are needed to reach vulnerable population subgroups as we found that three in eight women did not have a SBA. Across all countries, we found significant pro-rich inequalities in SBA and CS. Women from the poorest quintile were more likely to miss out on SBA and CS. Those women who did receive SBA or CS were more educated, had access to mass media (TV), had four or more ANC contacts, were residents of an urban area and had no distance problems to access a health facility.
Wealth-related inequalities within countries could be due to a combination of scarce access to CS among the poor and high levels of caesarean use without medical indication among rich. Countries should clearly differentiate between population subgroups and invest in targeted policies and strategies to improve access and ensure equity in SBA and CS. Improving the quality of care, ensuring respectful, non-abusive delivery services are critical strategies to increase the uptake of facility-based delivery. In addition, country-specific strategies are critical to addressing these inequalities to improve maternal and newborn health.
Acknowledgments
The authors thank MEASURE DHS project for their support and free access to the original data.
Footnotes
Handling editor: Seye Abimbola
Contributors: FTB, AA, MW, AD and AH contributed to the study design and conceptualisation. FTB reviewed the literature, performed the analysis and drafted the first draft of this manuscript. AH helped revise the study design, supervised the data analysis. AA, MW, AD and AH provided technical support and critically reviewed the manuscript. FTB had final responsibility to submit for publication. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public, open access repository. Data for this study were sourced from Demographic and Health surveys (DHS) and available here: http://dhsprogram.com/data/available-datasets.cfm.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethics approval was not required for the current analysis, as the data were publicly available. The MEASURE DHS /ICF International, Rockville, Maryland, USA—granted access to data on request.
References
- 1.World Health Organization . Trends in maternal mortality 2000 to 2017: estimates by who, UNICEF, UNFPA. World Bank Group and the United Nations Population Division, 2019. [Google Scholar]
- 2.Bhutta ZA, Das JK, Bahl R, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014;384:347–70. 10.1016/S0140-6736(14)60792-3 [DOI] [PubMed] [Google Scholar]
- 3.Boatin AA, Schlotheuber A, Betran AP, et al. Within country inequalities in caesarean section rates: observational study of 72 low and middle income countries. BMJ 2018;360:k55. 10.1136/bmj.k55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ronsmans C, Etard JF, Walraven G, et al. Maternal mortality and access to obstetric services in West Africa. Trop Med Int Health 2003;8:940–8. 10.1046/j.1365-3156.2003.01111.x [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization . Strategies towards ending preventable maternal mortality (EPMM), 2015. [Google Scholar]
- 6.Victora CG, Barros AJD, Axelson H, et al. How changes in coverage affect equity in maternal and child health interventions in 35 countdown to 2015 countries: an analysis of national surveys. Lancet 2012;380:1149–56. 10.1016/S0140-6736(12)61427-5 [DOI] [PubMed] [Google Scholar]
- 7.Bohren MA, Hunter EC, Munthe-Kaas HM, et al. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reprod Health 2014;11:1–17. 10.1186/1742-4755-11-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montagu D, Sudhinaraset M, Diamond-Smith N, et al. Where women go to deliver: understanding the changing landscape of childbirth in Africa and Asia. Health Policy Plan 2017;32:1146–52. 10.1093/heapol/czx060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adegoke AA, van den Broek N. Skilled birth attendance-lessons learnt. BJOG 2009;116 Suppl 1:33–40. 10.1111/j.1471-0528.2009.02336.x [DOI] [PubMed] [Google Scholar]
- 10.Barros AJD, Ronsmans C, Axelson H, et al. Equity in maternal, newborn, and child health interventions in countdown to 2015: a retrospective review of survey data from 54 countries. Lancet 2012;379:1225–33. 10.1016/S0140-6736(12)60113-5 [DOI] [PubMed] [Google Scholar]
- 11.Countdown to 2030 Collaboration . Countdown to 2030: tracking progress towards universal coverage for reproductive, maternal, newborn, and child health. Lancet 2018;391:1538–48. 10.1016/S0140-6736(18)30104-1 [DOI] [PubMed] [Google Scholar]
- 12.Bhutta ZA, Chopra M, Axelson H, et al. Countdown to 2015 decade report (2000–10): taking stock of maternal, newborn, and child survival. The Lancet 2010;375:2032–44. 10.1016/S0140-6736(10)60678-2 [DOI] [PubMed] [Google Scholar]
- 13.Amouzou A, Ziqi M, Carvajal-Aguirre L, et al. Skilled attendant at birth and newborn survival in sub-Saharan Africa. J Glob Health 2017;7:020504. 10.7189/jogh.07.020504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bobo FT, Asante A, Woldie M, et al. Poor coverage and quality for poor women: inequalities in quality antenatal care in nine East African countries. Health Policy Plan 2021;36:662–72. 10.1093/heapol/czaa192 [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization . A conceptual framework for action on the social determinants of health, 2010. [Google Scholar]
- 16.Boerma T, Ronsmans C, Melesse DY, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet 2018;392:1341–8. 10.1016/S0140-6736(18)31928-7 [DOI] [PubMed] [Google Scholar]
- 17.Yaya S, Uthman OA, Amouzou A, et al. Disparities in caesarean section prevalence and determinants across sub-Saharan Africa countries. Glob Health Res Policy 2018;3:19. 10.1186/s41256-018-0074-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.UN . Transforming our world: the 2030 agenda for sustainable development. resolution A/RES/70/1. Geneva: United Nations, 2015. [Google Scholar]
- 19.Rutstein SO, Rojas G. Guide to DHS statistics. Calverton, MD: ORC Macro, 2006: 38. [Google Scholar]
- 20.O'Donnell O, Van Doorslaer E, Wagstaff A, et al. Analyzing health equity using household survey data: a guide to techniques and their implementation. The World Bank, 2007. [Google Scholar]
- 21.Ansu-Mensah M, Mohammed T, Udoh RH, et al. Mapping evidence of free maternal healthcare financing and quality of care in sub-Saharan Africa: a systematic scoping review protocol. Health Res Policy Syst 2019;17:93. 10.1186/s12961-019-0495-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Bank . Out-Of-Pocket expenditure (% of current health expenditure).
- 23.Molla YB, Rawlins B, Makanga PT, et al. Geographic information system for improving maternal and newborn health: recommendations for policy and programs. BMC Pregnancy Childbirth 2017;17:1–7. 10.1186/s12884-016-1199-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shiferaw BB, Modiba LM. Why do women not use skilled birth attendance service? an explorative qualitative study in North West Ethiopia. BMC Pregnancy Childbirth 2020;20:1–14. 10.1186/s12884-020-03312-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Assefa Y, Gelaw YA, Hill PS, et al. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Global Health 2019;15:1–11. 10.1186/s12992-019-0470-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu C, Chin B, Lewandowski JL, et al. Towards universal health coverage: an evaluation of Rwanda Mutuelles in its first eight years. PLoS One 2012;7:e39282. 10.1371/journal.pone.0039282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Basinga P, Gertler PJ, Binagwaho A, et al. Effect on maternal and child health services in Rwanda of payment to primary health-care providers for performance: an impact evaluation. Lancet 2011;377:1421–8. 10.1016/S0140-6736(11)60177-3 [DOI] [PubMed] [Google Scholar]
- 28.Bucagu M, Kagubare JM, Basinga P, et al. Impact of health systems strengthening on coverage of maternal health services in Rwanda, 2000-2010: a systematic review. Reprod Health Matters 2012;20:50–61. 10.1016/S0968-8080(12)39611-0 [DOI] [PubMed] [Google Scholar]
- 29.Cammack D. Local governance and public goods in Malawi. IDS Bull 2011;42:43–52. 10.1111/j.1759-5436.2011.00210.x [DOI] [Google Scholar]
- 30.Uny I, de Kok B, Fustukian S. Weighing the options for delivery care in rural Malawi: community perceptions of a policy promoting exclusive skilled birth attendance and banning traditional birth attendants. Health Policy Plan 2019;34:161–9. 10.1093/heapol/czz020 [DOI] [PubMed] [Google Scholar]
- 31.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med 1994;38:1091–110. 10.1016/0277-9536(94)90226-7 [DOI] [PubMed] [Google Scholar]
- 32.Federal Democratic Republic of Ethiopia [Ministry of Health] . Health sector transformation plan (HSTP) 2015/16‐2019/20 (2008‐2012 EFY). Federal Democratic Republic of Ethiopia Ministry of Health, 2015. [Google Scholar]
- 33.Nigatu AM, Gelaye KA. Factors associated with the preference of institutional delivery after antenatal care attendance in Northwest Ethiopia. BMC Health Serv Res 2019;19:810. 10.1186/s12913-019-4636-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tekle Bobo F, Kebebe Kasaye H, Etana B, et al. Disrespect and abuse during childbirth in Western Ethiopia: should women continue to tolerate? PLoS One 2019;14:e0217126. 10.1371/journal.pone.0217126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arsenault C, Yakob B, Tilahun T, et al. Patient volume and quality of primary care in Ethiopia: findings from the routine health information system and the 2014 service provision assessment survey. BMC Health Serv Res 2021;21:1–10. 10.1186/s12913-021-06524-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hanson K, McPake B, Nakamba P, et al. Preferences for hospital quality in Zambia: results from a discrete choice experiment. Health Econ 2005;14:687–701. 10.1002/hec.959 [DOI] [PubMed] [Google Scholar]
- 37.Kruk ME, Mbaruku G, McCord CW, et al. Bypassing primary care facilities for childbirth: a population-based study in rural Tanzania. Health Policy Plan 2009;24:279–88. 10.1093/heapol/czp011 [DOI] [PubMed] [Google Scholar]
- 38.Kruk ME, Hermosilla S, Larson E, et al. Bypassing primary care clinics for childbirth: a cross-sectional study in the Pwani region, United Republic of Tanzania. Bull World Health Organ 2014;92:246–53. 10.2471/BLT.13.126417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bohren MA, Vogel JP, Hunter EC, et al. The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLoS Med 2015;12:e1001847. 10.1371/journal.pmed.1001847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Betran AP, Torloni MR, Zhang JJ, et al. WHO statement on caesarean section rates. BJOG 2016;123:667–70. 10.1111/1471-0528.13526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cavallaro FL, Cresswell JA, França GVA, et al. Trends in caesarean delivery by country and wealth quintile: cross-sectional surveys in southern Asia and sub-Saharan Africa. Bull World Health Organ 2013;91:914–22. 10.2471/BLT.13.117598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Joseph G, da Silva ICM, Barros AJD, et al. Socioeconomic inequalities in access to skilled birth attendance among urban and rural women in low-income and middle-income countries. BMJ Glob Health 2018;3:e000898. 10.1136/bmjgh-2018-000898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leslie HH, Spiegelman D, Zhou X, et al. Service readiness of health facilities in Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull World Health Organ 2017;95:738–48. 10.2471/BLT.17.191916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lim SS, Dandona L, Hoisington JA, et al. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. The Lancet 2010;375:2009–23. 10.1016/S0140-6736(10)60744-1 [DOI] [PubMed] [Google Scholar]
- 45.Koblinsky M, Moyer CA, Calvert C, et al. Quality maternity care for every woman, everywhere: a call to action. Lancet 2016;388:2307–20. 10.1016/S0140-6736(16)31333-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public, open access repository. Data for this study were sourced from Demographic and Health surveys (DHS) and available here: http://dhsprogram.com/data/available-datasets.cfm.