Abstract
Acute COVID-19 usually lasts 4 weeks from the onset of symptoms. We report two cases of COVID-19-associated organising pneumonia (OP) occurring beyond 4 weeks from the acute onset of symptoms. Both tested positive for SARS reverse transcription–PCR 2 months before presentation with a resolution of respiratory symptoms. The first case presented with residual fatigue and worsening exertional dyspnoea. Chest CT revealed an OP pattern. The second case presented with worsening cough and new-onset pleuritic chest pain with persistent radiological consolidation. A transbronchial lung biopsy confirmed OP. Both patients responded well to 12 weeks of steroid therapy. This case illustrates the rare presentation of OP as a late sequela of COVID-19 and the good response to steroid therapy.
Keywords: COVID-19, pneumonia (respiratory medicine)
Background
COVID-19-associated organising pneumonia (OP) can be present at different timelines. We do not know the optimal dose and duration of corticosteroid treatment in this condition. We share our experience in managing two cases of delayed COVID-19-associated OP.
Case presentation
Case 1
A 58-year-old woman with mild cough and fatigue tested positive for SARS-CoV-2 reverse transcription–PCR (RT-PCR) and underwent home quarantine. She recovered well with minimal fatigue. Two months later, she presented with a 3-day history of worsening exertional dyspnoea. Her respiratory rate was 26 breaths/min and peripheral oxygen saturation (SaO2) was 70% on room air. On supplemental oxygen of 15 L O2/min on a non-rebreather mask, the arterial blood gas revealed a pH of 7.44, pO2 of 90 mm Hg, pCO2 of 29 mm Hg and SaO2 of 98%. Laboratory investigations showed a total white blood cell count (TWBC) of 10.5×109/L, absolute lymphocyte count (ALC) of 0.8×109/L and C reactive protein (CRP) of 11.7 mg/L.
Chest radiograph revealed extensive ground-glass opacifications in all lobes. High-resolution CT of the thorax was consistent with an OP pattern (figure 1). The SARS‐CoV‐2 nasopharyngeal RT-PCR was positive with a cycle threshold value of 21. The serum SARS-CoV-2 IgM and IgG were detected. The nasopharyngeal swab PCRs for other respiratory viral pathogens were negative. A diagnosis of delayed post-COVID-19 OP was made.
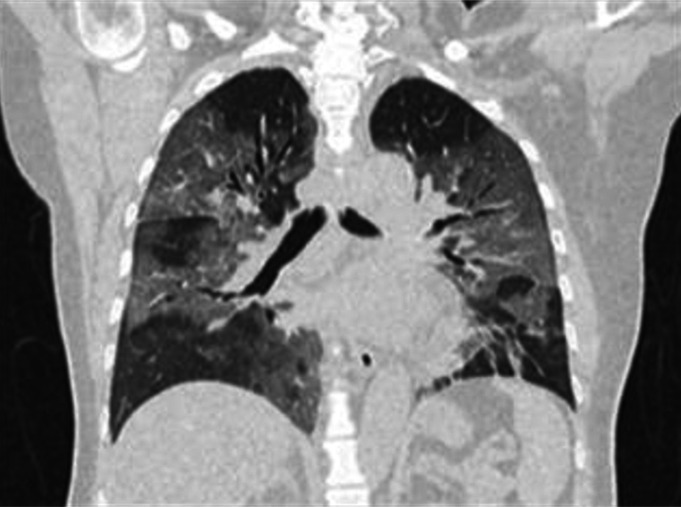
Figure 1.
Baseline CT of the thorax showing bilateral ground-glass opacities with visible intralobular lines.
She received intravenous methylprednisolone 500 mg/day for 3 days, followed by intravenous dexamethasone 6 mg/day for 10 days. Her SaO2 improved over 2 weeks. She was discharged with oral prednisolone at a dose of 0.5 mg/kg/day for 4 weeks, followed by 20 mg/day for another 4 weeks and tapered further to 10 mg/day for 2 weeks and 5 mg/day for 2 weeks.
Case 2
An 81-year-old man with cough and dyspnoea tested positive for SARS-CoV-2 RT-PCR. He was admitted for observation and discharged on day 10 with a residual mild cough. Two months later, he presented with a 1-week history of worsening cough and right-sided pleuritic chest pain. On clinical examination, SaO2 was 98% on room air with a respiratory rate of 16 breaths/min. There were expiratory rhonchi at the right lung base. TWBC was 9.8×109/L; ALC was 1.8×109/L; and CRP was 3.45 mg/dL. Chest radiograph showed a right mid-zone consolidation. Repeat nasopharyngeal SARS‐CoV‐2 RT-PCR was negative, and the patient was treated with a 5‐day course of piperacillin–tazobactam. His symptoms persisted and a contrasted CT of the thorax revealed a right middle lobe lung consolidative mass.
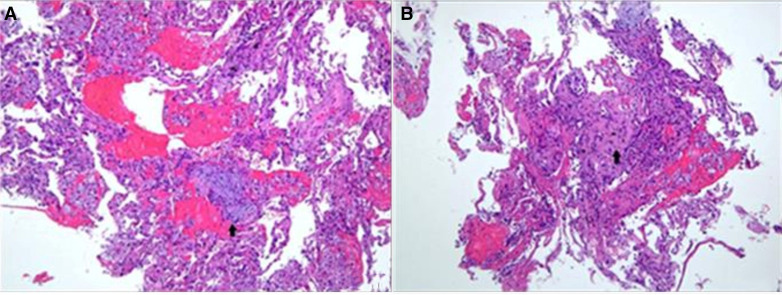
Bronchoalveolar lavage was culture negative. We performed a transbronchial lung biopsy (TBLB) with fluoroscopy targeted to the right middle lobe. Histopathological examination was consistent with OP with foamy macrophages, haemorrhage and occasional fibroblastic foci within the alveolar spaces (figure 2A, B).
Figure 2.
(A) Fragments are composed of benign pneumocytes lining the alveolar spaces, with scattered foamy macrophages, haemorrhage and occasional fibroblastic foci within the space (arrow). H&E, ×100. (B) The alveolar septa are focally fibrotic (arrow) and there are mild to moderate inflammatory cell infiltration within the stroma. H&E, ×100.
He was treated with prednisolone at a dose of 0.5 mg/kg/day for 4 weeks, 20 mg/day for 4 weeks, followed by 10 mg/day for another 2 weeks and tapered over 3 months.
Outcome and follow-up
Case 1
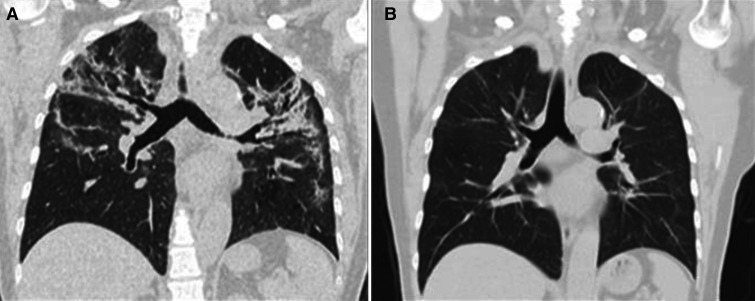
Outpatient review 6 weeks postdischarge showed resolution of dyspnoea with a Modified Medical Research Council Dyspnoea Scale of 0. The spirometry and gas transfer factors were within normal limits (forced expiratory volume in the first second (FEV1): 2.39 L (98%), forced vital capacity (FVC): 2.67 (82%), FEV1:FVC ratio: 90, diffusing capacity of the lungs for carbon monoxide: 109%). The repeat CT of the thorax showed significant resolution of the ground-glass attenuation and linear opacities (figure 3A, B). The 6 min walk test showed a markedly reduced distance of 222 m with no oxygen desaturation.
Figure 3.
(A) CT of the thorax showing improvement of GGO 2 weeks after pulsed methylprednisolone and maintenance dexamethasone. (B) CT of the thorax at 12 weeks showing resolution of GGO after completion of prednisolone therapy. GGO, ground-glass opacity.
Case 2
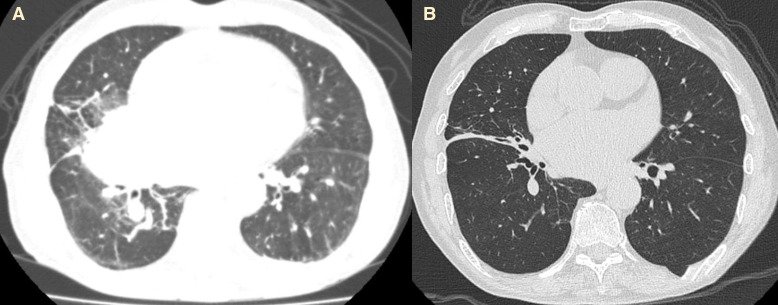
On outpatient review at 12 weeks, there was a resolution of both symptoms and radiographic consolidation (figure 4A, B).
Figure 4.
(A, B) CT of the thorax before and after prednisolone therapy showing improvement of right middle zone consolidation.
Discussion
Post-COVID syndrome is characterised by new, persistent or delayed symptoms 4 or more weeks following SARS-CoV-2 infection. SARS-CoV-2 may infect lung epithelium and drive pulmonary immune dysregulation in patients with COVID-19.1
COVID-19 pneumonia typically evolves within 1–3 weeks. The changes progress from focal, unilateral to diffuse bilateral ground-glass opacities (GGOs) or coexist with consolidation.2 The typical COVID-19-associated OP CT changes are central GGOs surrounded by denser consolidation of crescentic shape (reverse halo sign) and an arcade-like sign of perilobular densities. The diagnosis of COVID-19-associated OP may be made in COVID-19-positive patients with typical symptoms and typical CT changes described earlier. The definitive diagnosis of COVID-19-associated OP requires histological assessment. In our first case, we were unable to perform a lung biopsy due to the presence of severe hypoxic respiratory failure. In our second patient, we were able to perform TBLB, which confirmed the diagnosis of OP.
Radiological evidence of OP has been reported during the later course of COVID-19 pneumonia.2 The reported prevalence of COVID-19-associated OP was 12.5%.3 OP typically presents with mild dyspnoea.4 One study reported approximately one-third of OP cases with complete resolution of lesions at 1–2 months after symptom onset, while those with more consolidation and more lobe involvement were prone to fibrotic-like changes.5 Both patients recovered in varying degrees from their initial COVID-19 infection and went on to have a delayed presentation of OP at 2 months. This biphasic nature may be explained by the different host immune responses and viral dynamics.
Corticosteroids are the cornerstone of therapy for OP. Current consensus recommends an initial dose of 0.75–1.5 mg/kg/day of prednisone for 4 weeks tapered over 3–6 months.4 6 Relapse of OP commonly occurs when the corticosteroid dosing is reduced below 20 mg/day of prednisone equivalents or following the cessation of corticosteroids. Dexamethasone therapy is an effective therapy for COVID-19 pneumonia.7 8 The RECOVERY trial has shown that dexamethasone at a dose of 6 mg once per day for up to 10 days reduces mortality in severe and critical forms of COVID-19 pneumonia.8 Methylprednisolone at a dose of 250 mg/day for 3 days has been shown to increase survival for hospitalised patients with severe COVID-19.9 Meta-analysis had shown a beneficial effect of corticosteroids on short-term mortality and a reduction in the need for mechanical ventilation.10 The role of steroids in patients with milder COVID-19 is less clear.
Case series have reported favourable outcomes with high doses of corticosteroid therapy, and prolonged therapy typically weeks to months in COVID-19-associated OP.3 11 12 A single-centre prospective observational study had shown about one-quarter of post-COVID-19 pneumonia had recurring dyspnoea with radiological findings of OP where resuming corticosteroids resulted in clinical and radiological improvements.13 At present, there is a lack of evidence on whether corticosteroid treatment in COVID-19-associated OP can prevent the relapses of OP or reduce the development of residual pulmonary fibrosis. In both of our patients, we prolonged the corticosteroid therapy to target the inflammatory burden and preserve pulmonary fibrosis. Both patients showed significant radiological improvement with steroids. However, the first case showed reduced distance in the 6 min walk test due to fatigability.
To date, there is no study on the effects of corticosteroids on the resolution of COVID-19-associated OP and long-term pulmonary outcome. A large, multicentre randomised control trial is needed to determine the optimal dosage, duration and benefit of corticosteroid therapy in COVID-19-associated OP. Clinicians should consider the potential risks and benefits of corticosteroids and use CT as a guide on the different phases of CT patterns in patients with COVID-19. We need a precision approach in COVID-19-associated OP as not one size fits all.
Learning points.
It is important to explore the history of recent COVID-19 infection in patients with new-onset respiratory symptoms as this may be a late complication of COVID-19.
COVID-19 organising pneumonia (OP) should be suspected in patients with typical COVID-19 OP CT changes with a negative viral and bacterial pathogen workup.
A delayed biphasic pattern beyond 4 weeks of COVID-19-associated OP can occur in mild disease.
A longer duration of corticosteroid therapy in COVID-19-associated OP should be considered.
Footnotes
Contributors: BHN wrote the case under continuous supervision of AY-LB and MF. BHN and NNNA discussed the case presentation, investigations and management. AY-LB and MF supervised and provided guidance on the management of the patient.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Chen H, Liu W, Wang Y, et al. SARS-CoV-2 activates lung epithelial cell proinflammatory signaling and leads to immune dysregulation in COVID-19 patients. EBioMedicine 2021;70:103500. 10.1016/j.ebiom.2021.103500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020;20:425–34. 10.1016/S1473-3099(20)30086-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vadász I, Husain-Syed F, Dorfmüller P, et al. Severe organising pneumonia following COVID-19. Thorax 2021;76:201–4. 10.1136/thoraxjnl-2020-216088 [DOI] [PubMed] [Google Scholar]
- 4.Cordier J-F. Cryptogenic organising pneumonia. Eur Respir J 2006;28:422–46. 10.1183/09031936.06.00013505 [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Jin C, Wu CC, et al. Organizing pneumonia of COVID-19: time-dependent evolution and outcome in CT findings. PLoS One 2020;15:e0240347. 10.1371/journal.pone.0240347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cottin V, Cordier J-F. Cryptogenic organizing pneumonia. Semin Respir Crit Care Med 2012;33:462–75. 10.1055/s-0032-1325157 [DOI] [PubMed] [Google Scholar]
- 7.WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JAC, Murthy S, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA 2020;324:1330–41. 10.1001/jama.2020.17023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021;384:693–704. 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edalatifard M, Akhtari M, Salehi M, et al. Intravenous methylprednisolone pulse as a treatment for hospitalised severe COVID-19 patients: results from a randomised controlled clinical trial. Eur Respir J 2020;56. 10.1183/13993003.02808-2020. [Epub ahead of print: 24 12 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Paassen J, Vos JS, Hoekstra EM, et al. Corticosteroid use in COVID-19 patients: a systematic review and meta-analysis on clinical outcomes. Crit Care 2020;24:696. 10.1186/s13054-020-03400-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takumida H, Izumi S, Sakamoto K, et al. Sustained coronavirus disease 2019-related organizing pneumonia successfully treated with corticosteroid. Respir Investig 2021;59:377–81. 10.1016/j.resinv.2020.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.In-Gyu B, Kyung-Wook H, Jung Wook Y. Persistent pneumonic consolidations due to secondary organizing pneumonia in a patient recovering from COVID-19 pneumonia: a case report, 2021. Research square. Available: https://www.researchsquare.com/article/rs-37580/v1 [DOI] [PMC free article] [PubMed]
- 13.Myall KJ, Mukherjee B, Castanheira AM, et al. Persistent Post-COVID-19 interstitial lung disease. An observational study of corticosteroid treatment. Ann Am Thorac Soc 2021;18:799–806. 10.1513/AnnalsATS.202008-1002OC [DOI] [PMC free article] [PubMed] [Google Scholar]