Abstract
We tested a dynamic structural equation model (DSEM; Asparouhov, Hamaker, & Muthén, 2018) of positive and negative affect in 254 veterans with approximately 1.5 years of experience sampling data. The analysis provided estimates of several aspects of veteran’s emotional experience including “trait” positive and negative affect (i.e., mean levels), inertia (i.e., tendency for emotions to self-perpetuate), innovation variance (conceptualized as lability, reactivity, or exposure to stressors), and cross-lagged associations between positive and negative affect. Veterans with higher trait negative affect had more negative affect inertia and innovation variance. This suggests a pattern whereby the veteran has more negative reactions, and negative emotions, in turn, tend to maintain themselves contributing to higher trait negative affect. In contrast, veterans with higher trait positive affect exhibited more positive affect innovation variance (e.g., positive reactivity). Although veterans showed some consistency in dynamics across emotions (e.g., positive and negative reactivity were positively correlated), trait positive and negative affect were not significantly associated. Veterans with higher posttraumatic stress symptoms (PTSS) at baseline exhibited higher reactivity to negative events, less positive affect, and more negative affect during the follow-up. Veterans with higher distress tolerance reported not only lower PTSS but also a more adaptive pattern of affective experience characterized by lower inertia and reactivity in negative affect and more positive lagged associations between negative affect and subsequent positive affect. The results demonstrated that distress tolerance and PTSS in veterans were associated with dynamics of positive and negative emotion over time suggesting specific differences in affect regulation processes.
Keywords: affect regulation, PTSD, EMA, ESM
Dysregulated affect is a core feature of posttraumatic stress disorder. Dysregulation is observed in the form of heightened reactivity to internal and external trauma-related cues, avoidance of trauma-related emotion, persistent negative affective states, and heightened arousal and irritability (American Psychiatric Association, 2013). Though often less of a focus in the literature, dysregulation also manifests as deficits in positive affect and reward responsiveness (American Psychiatric Association, 2013; Vujanovic, Wardle, Smith, & Berenz, 2017). Converging advances in data analysis and mobile technologies are paving the way for a renaissance in the study of psychopathology (Asparouhov et al., 2018; Hamaker, Asparouhov, Brose, Schmiedek, & Muthén, 2018; Hamaker & Wichers, 2017). Emotion, behavior, and other psychological processes can now be studied as elements in dynamic systems that interact over time on a moment-to-moment basis (Hamaker et al., 2018; Hamaker & Wichers, 2017). The goal of the current study is to model the dynamic time course of positive and negative affect in a sample of veterans and test effects of posttraumatic stress symptoms (PTSS) and distress tolerance on individual differences in affective dynamics.
Affective dynamics
Affect dysregulation is often assessed via retrospective self-report. For example, assessments may query use of strategies to regulate affect, such as suppression or reappraisal (Preece, Becerra, Robinson, & Gross, 2019), tendency to ruminate (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008), or characteristics of affective experience, such as lability (Oliver & Simons, 2004), reactivity (Nock, Wedig, Holmberg, & Hooley, 2008; Zelkowitz & Cole, 2016), or trait affect (Watson & Clark, 1999). Another approach is to repeatedly assess momentary emotional experience via experience sampling and then calculate descriptive features or directly model the dynamic process (Hamaker, Ceulemans, Grasman, & Tuerlinckx, 2015; Hamaker et al., 2018; Hamaker & Wichers, 2017). For example, lability or emotional instability has been estimated from experience sampling method (ESM) data by calculating mean squared successive differences (MSSD) across assessments (Dejonckheere et al., 2019; Jahng, Wood, & Trull, 2008). Research indicates that lability assessed by MSSD is associated with borderline personality disorder and alcohol dependence symptoms (Simons, Wills, & Neal, 2014; Thompson et al., 2012; Trull et al., 2008). However, a recent meta-analysis suggests that MSSD may have little added value beyond the mean and variance of emotion ratings (Dejonckheere et al., 2019). Alternatively, and consistent with the approach taken here, parameters can be estimated from a time-series model of emotional experience.
Dynamic structural equation models (DSEM) provide a wealth of individual difference parameters that may be conceptualized as manifestations of affect regulation (Asparouhov et al., 2018; Hamaker et al., 2018; Hamaker & Wichers, 2017). In this regard, a univariate DSEM of affect estimates three random effect parameters: mean, autoregression, and residual (Asparouhov et al., 2018; Hamaker et al., 2018). The mean may be conceptualized as trait affect or mean affective level depending on the length of the assessment period. Estimating the mean from the experience sampling data has a number of benefits compared to using the observed mean or single observation retrospective self-report, including accounting for measurement error in the repeated assessments (Ludtke et al., 2008; Preacher, Zyphur, & Zhang, 2010) and minimizing memory biases associated with retrospective assessment of mood (e.g., recency effects; Shiffman, Stone, & Hufford, 2008).
The autoregression parameter may be conceptualized as the inverse of regulatory strength (Hamaker, 2012). Next to mean levels, this parameter has received the most attention in studies of negative affect. Autoregression has been interpreted as emotional inertia and is related to the construct of rumination (Koval, Kuppens, Allen, & Sheeber, 2012; Koval, Pe, Meers, & Kuppens, 2013) and bears similarity to Linehan’s concept of “slow return to baseline” component of emotional vulnerability in borderline personality disorder (Linehan, 1993). Inertia in negative affect has been related to higher mean levels of negative affect (Hamaker et al., 2018; Simons, Emery, Simons, Wills, & Webb, 2016). Research indicates inertia is associated with risk for depressive episodes (Kuppens et al., 2012), though a recent meta-analysis suggests it may have little predictive value over and above mean levels of positive and negative affect (Dejonckheere et al., 2019). Though associations are weaker, inertia in positive affect has also been shown to be inversely associated with well-being and trait positive affect (Hamaker et al., 2018; Houben, Van Den Noortgate, & Kuppens, 2015). In addition, research suggests that alcohol intoxication reduces autoregression in both positive and negative affect (Fairbairn & Sayette, 2013; Simons et al., 2016).
The random residual has been referred to as innovation or random shock (Hamaker, 2012; Hamaker et al., 2018). This reflects unmeasured sources of heterogeneity and is the sum of all unobserved internal and external determinants of affect. In respect to affect regulation, this may be conceptualized as heightened reactivity to stimuli, greater variability in exposure to emotionally relevant environmental stimuli (Hamaker et al., 2018), or, more broadly, affective lability (Simons et al., 2017). Though limited, previous research indicates the negative affect innovation parameter is positively associated with both mean levels of negative affect as well as inertia (Hamaker et al., 2018), suggesting that negative affect innovation variance may reflect reactivity and dysregulated negative affect. In contrast, innovation variance for positive affect has been both positively and inversely associated with mean levels of positive affect and inversely associated with positive affect inertia (Hamaker et al., 2018). In summary, DSEM can quantify individual differences in mean affect, inertia, and reactivity or exposure to emotionally evocative events from an intensive longitudinal assessment of affect.
Whereas a univariate model DSEM model of affect would model the dynamics of a single affective state over time (e.g., negative affect), a bivariate model examines the dynamics of two affective states overtime. In addition to modeling the means, autoregression, and residual for each affective state, the bivariate model also models how, for example, positive and negative affect predict each other through cross-lagged effects. That is, the bivariate model estimates the extent to which negative affect predicts subsequent positive affect and the extent to which positive affect predicts subsequent negative affect. Like a traditional cross-lagged panel model, the residuals may be expected to correlate, signifying that unexplained heterogeneity (i.e., residual error) in positive and negative affect may have a common source. For example, if a veteran was unexpectedly exposed to reminders of their traumatic war experience on a Thursday at 5 p.m., this cue exposure may result in large deviations in levels of both positive and negative affect on subsequent assessments. In the DSEM model, when residuals are allowed to be random parameters at the between-person level (i.e., random innovation), an additional random parameter, the covariance in the residuals can be estimated. A random person-level parameter would suggest, for example, that a veteran may be particularly reactive to emotionally laden stimuli and that this reactivity is observed in both positive and negative affect (e.g., experiencing large changes in both positive and negative affect when hearing about a bombing on the news). In summary, the bivariate DSEM model of positive and negative affect extends the univariate model to also include cross-lagged effects and covariance in the residual parameter, which quantify the interdependence of positive and negative affect.
PTSD and affect dysregulation
Posttraumatic stress disorder symptoms include persistent negative emotional states, anhedonia or low levels of positive emotions, loss of interest and deficits in goal directed activity, and heightened emotional reactivity (American Psychiatric Association, 2013). These symptoms are mirrored by research tying PTSD to a host of related traits. For example, PTSD is positively associated with levels of negative affect in cross-sectional (Badour, Resnick, & Kilpatrick, 2017; Brown et al., 2014; Byllesby, Charak, Durham, Wang, & Elhai, 2016; Vujanovic et al., 2013) and experience sampling research (Dornbach-Bender et al., 2019). PTSD has been consistently associated with heightened emotional reactivity (Fitzgerald et al., 2018; Greene, Gelkopf, Epskamp, & Fried, 2018; Kaczmarek & Zawadzki, 2014; Lieberman, Gorka, DiGangi, Frederick, & Phan, 2017; Spiller et al., 2019), or variants of emotional reactivity, such as affect lability (Dutton, Badour, Jones, Mischel, & Feldner, 2016; Simons et al., 2017). Finally, several studies indicate positive associations between PTSD and rumination on negative affect, suggesting potential associations with inertia (Borders, McAndrew, Quigley, & Chandler, 2012; Brown, Hetzel-Riggin, Mitchell, & Bruce, 2018; Erwin et al., 2018; Spinhoven, Penninx, Krempeniou, van Hemert, & Elzinga, 2015; Viana et al., 2017). Collectively, these findings suggest that PTSD may be associated with individual differences in affective dynamics reflecting higher mean negative affect (Dornbach-Bender et al., 2019), increased negative affect inertia (Borders et al., 2012), and higher reactivity in negative affect (i.e., innovation variance; Lieberman et al., 2017).
The association between PTSD and positive affect has been less consistent in the literature, with most studies showing decreased levels of positive affect in individuals with higher levels of PTSS (Bersani et al., 2016; DePierro, D’Andrea, Frewen, & Todman, 2018; Newton & Ho, 2008; Seligowski & Orcutt, 2016), although not always (Brown et al., 2014; Dornbach-Bender et al., 2019). Low levels of positive affect are thought to reflect, in part, broad deficits in reward functioning (Vujanovic et al., 2017). Of note, PTSD is associated with reduced responsiveness to positive stimuli (Nawijn et al., 2015; Vujanovic et al., 2017). Such deficits are most pronounced in respect to social stimuli. In the current study, this may manifest in either heightened positive affect inertia or low reactivity in positive affect. Deficits in reward responsiveness may account for comorbidity of PTSD and substance use disorders. Indeed, laboratory research suggests that rewarding effects of alcohol are, in part, due to its ability to reduce inertia in positive affect (Fairbairn & Sayette, 2013). Collectively, previous research suggests that PTSS may be associated with lower mean positive affect (Bersani et al., 2016), heightened positive affect inertia (Nawijn et al., 2015), and lower positive affect reactivity (i.e., innovation variance; Vujanovic et al., 2017).
Distress tolerance
Tolerance for emotional distress allows one to maintain goal directed activity when distressed, including engaging in more adaptive regulation of negative affect (Jeffries, McLeish, Kraemer, Avallone, & Fleming, 2015; Simons & Gaher, 2005). Distress tolerance is inversely associated with PTSD (Boffa, Short, Gibby, Stentz, & Schmidt, 2018; Erwin et al., 2018; Marshall-Berenz, Vujanovic, Bonn-Miller, Bernstein, & Zvolensky, 2010; Vujanovic, Bonn-Miller, Potter, Marshall, & Zvolensky, 2011), internalizing symptoms (Banducci, Lejuez, Dougherty, & MacPherson, 2017; Felton et al., 2017), trait negative affect (Kiselica, Rojas, Bornovalova, & Dube, 2015; Simons & Gaher, 2005), lability (Simons & Gaher, 2005), and rumination (Erwin et al., 2018; Jeffries et al., 2015; Magidson et al., 2013; Naragon-Gainey, McMahon, & Chacko, 2017). Distress tolerance can also buffer (i.e., moderate) associations between negative affect and risk for psychopathology, including PTSD. For example, at the between person level, the strength of the association between negative affect intensity and PTSS was greatest when distress tolerance was low (Vujanovic et al., 2013). Though distress tolerance has been primarily connected to experience of negative affect, there is some evidence of associations with heighted positive affect or decreased anhedonia, though effects tend to be weaker and are inconsistent across studies (Bernstein, Zvolensky, Vujanovic, & Moos, 2009; Kiselica et al., 2015; Simons & Gaher, 2005). Collectively, previous research suggests distress tolerance may be associated with lower mean negative affect (Kiselica et al., 2015), less negative affect inertia (Erwin et al., 2018), and less negative affect reactivity (Simons & Gaher, 2005).
Previous findings suggest that distress tolerance will be inversely associated with PTSS. However, whether distress tolerance is a preexisting factor reducing the severity of PTSS, PTSD symptomology alters tolerance for distress, or they exhibit more complex reciprocal associations is less clear (Vujanovic, Litz, & Farris, 2015). Limited longitudinal research indicates that, controlling for baseline symptoms, changes in distress tolerance during treatment predict lower PTSS post-treatment (Banducci, Connolly, Vujanovic, Alvarez, & Bonn-Miller, 2017; Boffa et al., 2018). Similarly, a study of an adolescent sample indicated that distress tolerance, interacting with perceived social support, prospectively predicted PTSS following a natural disaster (Cohen, Danielson, Adams, & Ruggiero, 2016). In addition, though trauma exposure and PTSS may affect distress tolerance, individual differences in the ability to tolerate distress developmentally precede trauma exposure. Hence, we structured the model such that distress tolerance predicts PTSS (rather than vice versa).1 We propose that distress tolerance will exhibit a pattern of direct and indirect effects on affective dynamics via PTSS reflecting individual differences in affect regulation.
Current study
The current study tested a DSEM of positive and negative affect over time following the approach illustrated by Hamaker and colleagues (2018). From the cross-lagged model of positive and negative affect, we sought to estimate nine random effects reflecting individual differences in the time course of emotional experience. These random effects are theorized to reflect important aspects of affect regulation (Hamaker et al., 2018; Koval et al., 2012; Kuppens et al., 2012), which we expected to be associated with baseline levels of distress tolerance and PTSS. Our hypotheses focused on affect means, autoregression (i.e., inertia), and innovation. We did not make specific hypotheses about effects on the cross-lagged associations or innovation covariance. Specifically, we hypothesized PTSS would be positively associated with higher levels of negative affect (NA), more NA inertia, and more NA reactivity. Conversely, PTSS were expected to be inversely associated with mean positive affect (PA). However, to the extent that inertia in positive affect as well as low positive affect innovation may reflect deficits in engaging with the changing environment (Fairbairn & Sayette, 2013), we hypothesized positive associations between PTSS and positive affect inertia (similar to expected effects with NA inertia) and negative effects on the positive affect innovation parameter. Effects of distress tolerance were expected to be opposite in sign from the PTSS effects (e.g., less NA, more PA). Distress tolerance was hypothesized to have indirect effects on the outcomes via PTSS, but also exhibit direct effects on the outcomes over and above PTSS. This pattern reflects the theoretical proposition that distress tolerance is a transdiagnostic factor contributing to more adaptive regulation of affect (Gaher, Hofman, Simons, & Hunsaker, 2013; Sandin, Simons, Valiente, Simons, & Chorot, 2017).
Method
Participants
Participants were 276 Operation Iraqi Freedom, Operation Enduring Freedom, and Operation New Dawn (OIF/OEF/OND) veterans age 21 to 51 (M = 33.31, SD = 6.57). Fourteen percent were women. The sample was 82% white, 10% black, 3% multiracial, 1% Asian, and 5% other races or did not respond. Eight percent were Hispanic. Additional details regarding sample characteristics can be found in three previous papers based on this sample (Simons et al., 2018; Simons et al., 2017; Simons et al., 2019). A semi-structured diagnostic interview indicated approximately 39% met criteria for a current PTSD diagnosis and 5% for a lifetime history of PTSD (Structured Clinical Interview for DSM–IV–TR Axis I-Patient Edition; First, Spitzer, Gibbon, & Williams, January, 2010). The average age of onset of PTSD was 26.82 years old (SD = 6.39) corresponding to a mean of 6.64 (SD = 4.12) years prior to the baseline interview. Approximately 23% reported being in mental health treatment at baseline. The analysis sample for the DSEM model was 254 (see retention and compliance section).
Procedure
Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF) and Operation New Dawn (OND) veterans were recruited from two communities (Tampa Bay area, FL and Vermillion / Sioux Falls, SD). Participants were recruited from the local Veteran Affairs Medical Centers, local universities, and surrounding communities via newspaper advertisements, flyers, mail correspondence, and clinician referral. Inclusion criteria were OIF/OEF/OND veteran status, current or past history of alcohol use, and ability to read English at an eighth grade level. Exclusion criteria included psychosis and severe alcohol dependence (i.e., presenting acute medical risk). Participants completed a baseline assessment and then were enrolled in an ESM study for approximately 1.5 years. The ESM study was a measurement burst design with 10 weeks of sampling in 7 bursts across the 1.5 years. Burst 1 was 2 weeks, burst 4 was 3 weeks, and bursts 2, 3, 5, 6 and 7 were 1 week in length. The bursts were separated by approximately 3 months and research staff contacted participants to schedule the appointments.
Eight experience sampling assessments per day occurred between 10 a.m. and 2 a.m. Random prompts were followed by a reminder prompt 15 minutes later and then expired after 30 minutes. Each assessment took approximately 2 to 3 minutes to complete. Although emotional experience may be continuous with moment-to-moment fluctuations, the sampling schedule results in approximately 2-hour lags between assessments. We believe this schedule is a reasonable balance of the competing demands of maximizing temporal fidelity and minimizing participant burden. Two hour time lags have been used frequently in previous research (Gaher et al., 2014; Larson & Csikszentmihalyi, 1983; Simons, Gaher, Oliver, Bush, & Palmer, 2005; Simons et al., 2014). A recent metanalysis of 15 affect dynamic studies (Dejonckheere et al., 2019), included time lags ranging from 1.3 hours to 1 day. Our 2-hour lag is thus close to the shortest lags used in this research area. Research indicates that observed effects in autoregressive models may vary as a function of the specified time lag (de Haan-Rietdijk, Kuppens, & Hamaker, 2016; Dormann & Griffin, 2015; Gollob & Reichardt, 1987; Hamaker & Wichers, 2017). The results of this study are thus specific to the chosen 2-hour time lag.
Participants could disable prompts when sleeping or when they would otherwise be unsafe or unable to respond (e.g., while driving). All procedures were approved by the respective institutional review boards. Participants were paid $25 for the baseline assessment and up to $100 per week in the ESM study contingent on performance. Participation was voluntary and responses were confidential. Additional information regarding the procedure is in Simons et al. (2018).
Baseline measures
PTSS.
The PTSD checklist for DSM-IV - military version (PCL-M) was used to assess posttraumatic stress disorder symptoms at baseline (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Weathers, Litz, Herman, Huska, & Keane, 1993). The PCL-M consists of 17 items rated on 5-point scales (1 = not at all, 5 = extremely). PTSS comprised a latent variable with three indicators reflecting the avoidance, intrusion, and hyperarousal subscales.
Distress tolerance.
The Distress Tolerance Scale (DTS) was used to assess distress tolerance (Simons & Gaher, 2005). The scale has 15 items rated on 5-point scales (1 = strongly agree, 5 = strongly disagree) with higher scores indicating greater tolerance for emotional distress. The four subscales of absorption, tolerance, regulation, and appraisal were used as indicators of a latent distress tolerance construct.
Experience sampling measures
Affect.
Positive and negative affect in the last 30 minutes were assessed at each random prompt. Responses were made on a 7-point rating scale (1 = not at all, 7 = extremely). Items were based on the PANAS-X (Watson & Clark, 1999). Positive affect included five items: happy, joyful, excited, enthusiastic, and energetic. Negative affect consisted of nine items: sad, downhearted, blue, jittery, nervous, anxious, angry, hostile, and irritable. We calculated reliability (Omega; McDonald, 1999) of the positive and negative affect scales at the within and between level following procedures of Geldhof, Preacher, and Zyphur (2014). The scales exhibited good reliability at both the within- (PA ω = .92; NA ω = .87) and between-person (PA ω = .95; NA ω = .92) levels.
Analysis plan
We tested a DSEM in Mplus 8.3 with the Bayes estimator (Asparouhov et al., 2018; Muthén & Muthén, 2018). The analytic approach closely follows that of Hamaker (2018), who provides a more technical overview of a bivariate DSEM of affect. The data were defined as a two-level structure with signals nested in persons. Other nesting structures are possible with these data (e.g., signals, nested within days, nested within burst, nested within persons). However, research suggests that three level structures with signals nested within days may result in unreliable estimates of day-level intercepts (de Haan-Rietdijk et al., 2016) and hence a 2-level model was estimated. A second analytic concern was in regard to the uneven spacing of assessments due to the random prompts within measurement bursts, gaps introduced by sleep, and the measurement burst design (space between bursts). To address this, we employed an Mplus feature to impose a temporal grid of approximately 2 hours (reflecting the temporal grid for the random assessments), which provides roughly equal spacing between assessments and incorporates missing data points during gaps (e.g., overnight). Simulation results indicate that the approach provides unbiased estimates with as much as 85% missing data (e.g., missing data included due to gaps in the time series; Asparouhov et al., 2018). In order to avoid adding a tremendous amount of planned missingness introduced by the gaps between assessment bursts and given the focus here on stationary affective dynamics as opposed to longer term growth, we reduced gaps between bursts to 48 hours, which should be sufficient for autoregressive effects to dissipate.
The DSEM decomposes the repeated measures data into within- and between-person variance components based on a latent-mean approach (Asparouhov et al., 2018). At level 1 (within-person), positive affect and negative affect at time 𝑡 are regressed on their preceding assessments at time 𝑡−1, representing a time-lag of approximately 2 hours (see Figure 1). These two paths are the autoregressive paths, φpp and φnn, respectively. In addition, positive affect and negative affect at time 𝑡 are regressed on the other emotion at time 𝑡−1. These are the cross-lagged effects, φpn and φnp, respectively. These four within-person associations were estimated as random effects, allowing for between-person variation in the strength of the associations. Finally, we estimated random residual variances and covariances. Τhe residual variance of an emotion, ζ, is comprised of the unique variance δ, and the covariance is specified as the variance ψ of the common factor η. The residual variances are referred to as innovation variances and are estimated at level 2 with a log normal distribution in order to ensure they are positive and to allow covariances with the other random effects (Hamaker et al., 2018). Following Hamaker and colleagues (2018), we constrained the innovation covariance to be negative across persons by specifying the loadings of η to be 1 and −1, and estimated the log of this random effect at level 2.2 Thus, the DSEM estimated nine random effect parameters from the time-series data (two intercepts (μPA, μNA), two autoregressive effects (φpp, φnn), two cross-lagged effects (φpn, φnp), and two innovation variances and the covariance (estimated as the logs at level 2 (log(πPA), log(πNA), and log(ψ)).
Figure 1.
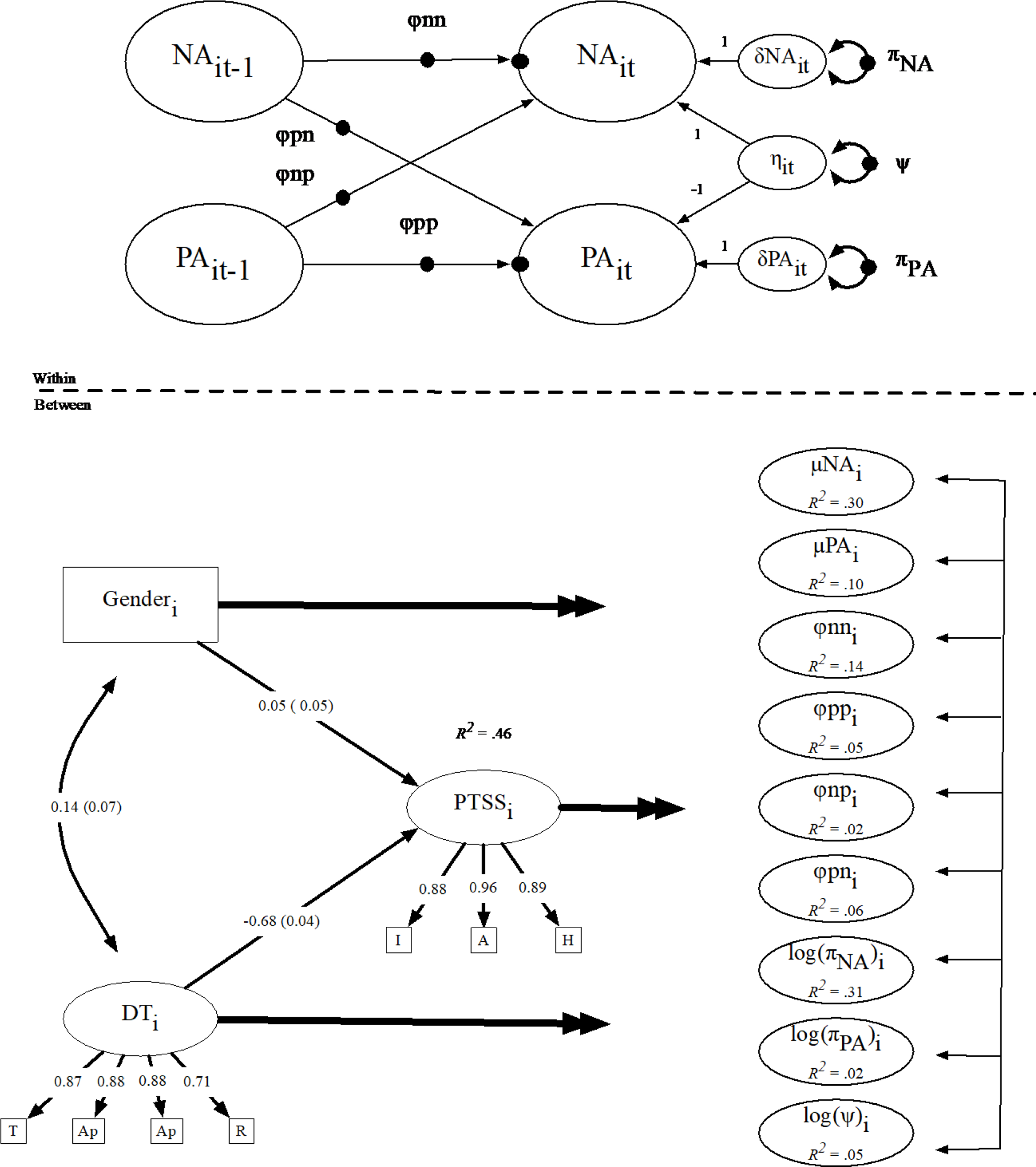
DSEM. Double headed arrows signify paths to all random effects. See Table 3 for coefficients. Depicted factor loadings and effects are standardized. All are significant based on the 95% credibility interval (CI) aside from the path from gender to posttraumatic stress symptoms (PTSS). All R2 values are significant based on the 95% credibility intervals. DT= distress tolerance, and subscales T (tolerance) Ap (appraisal), Ab (absorption), R (regulation). PTSS subscales are I (intrusion, A (avoidance), H (hyperarousal). PA = positive affect. NA = negative affect.
The nine correlated random effects were regressed on gender and two latent variables, distress tolerance and PTSS. Distress tolerance and gender were exogenous variables with paths to PTSS and the nine random effects. Distress tolerance and gender had both direct and indirect, via PTSS, effects on the level 2 random effects. Hence, the level 2 structural model is a saturated model with 0 degrees of freedom.
Our model parameters (e.g., fixed-intercepts, fixed-effects and random-effects parameters for the autoregressive and cross-lag effects, residual variances and covariances) were assumed to be constant across time. These assumptions lead to strict form of stationarity of the time series variables, positive and negative affect. Specifically, the model specification assumed no mean level changes, no time-related trends, as well as constant variance, constant within-time covariance, and constant lagged covariance for the time-series variables. We examined mean-level and trend-level stationarity using the Augmented Dickey-Fuller (ADF) test for stationarity relative to the individual mean on each individual time series for positive and negative affect. The ADF test indicated that five of the time series (two for positive affect and three for negative affect) were non-stationary. Given the large number of tests (508) performed, the small number of non-stationary time series with respect to mean levels, and the high proportion of stationary time series (> 99%), we decided not to detrend the data prior to performing the DSEM analyses. The assumption of a constant lagged covariance structure is unlikely to hold for every participant; however, this assumption cannot be thoroughly examined with the modeling tools presently available.
The model was estimated using the default noninformative priors in Mplus for the Bayes estimator (Asparouhov & Muthén, 2010). The MCMC estimation proceeded in two chains and convergence was determined by the potential scale reduction (PSR) which is the ratio of total variation to between chain variation (Asparouhov & Muthén, 2010). We initially estimated the model with 5,000 iterations and thinning of 10 and then re-estimated it with 50,000 iterations and thinning of 10 to ensure stable convergence. Subsequent to estimation, we examined trace plots to evaluate difficulty in the mixing of the two chains. In the results, we report Bayesian 95% credibility intervals for the posterior distributions.
Results
Retention and protocol compliance
Of the 276 participants completing the baseline assessment, 271 initiated the ESM study. The analysis sample was comprised of the 254 participants who provided at least 1 week of data with more than a 33% response rate for the analyses. The analysis sample completed 71% of the random prompts. At the person-level, the random response rate was M = 0.69 (SD = 0.16, median = .70, minimum = 0.27, maximum = 0.98). Random response rate was inversely associated with PCL-M scores (r = −.25, p = .0001) and positively associated with distress tolerance (r = .15, p = .0208) but not with gender (r = .10, p = .1053). On average, participants provided 64.63 (median = 73.5) days of data and the mean time in the study was 1.56 (SD = 0.63) years. Retention in the study (defined by subject mean elapsed days) was inversely associated with PCL-M scores (r = −.24, p = .0001) but not distress tolerance (r = .10, p = .1132) or gender (r = −.01, p = .9316).
Descriptive statistics
Table 1 includes descriptive statistics for the analytic sample. Table 2 presents the between-person correlations. Distress tolerance and PTSS exhibited moderate to strong inverse correlations. Distress tolerance was moderately inversely correlated with subject mean negative affect and had small to moderate positive associations with subject mean positive affect. PTSS had strong positive correlations with negative affect and moderate inverse correlation with positive affect. Mean positive and negative affect exhibited a modest inverse correlation. In respect to the signal level data, the intraclass correlation (ICC) for positive affect was 0.52 and the ICC for negative affect was 0.49 indicating about half of the variance for each was at the between-person level.
Table 1.
Descriptive statistics
| Variable | N | M or % | SD | Min | Max | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|
| Gender | 254 | 85.4% Male | |||||
| DTS_tol | 250 | 3.36 | 1.15 | 1.00 | 5.00 | −0.30 | −0.86 |
| DTS_abs | 250 | 3.49 | 1.10 | 1.00 | 5.00 | −0.38 | −0.72 |
| DTS_app | 251 | 3.45 | 1.01 | 1.00 | 5.00 | −0.24 | −0.79 |
| DTS_reg | 254 | 3.09 | 1.14 | 1.00 | 5.00 | 0.14 | −0.93 |
| PCL_intr | 254 | 2.59 | 1.18 | 1.00 | 5.00 | 0.42 | −0.98 |
| PCL_avoid | 254 | 2.66 | 1.19 | 1.00 | 5.00 | 0.24 | −1.12 |
| PCL_arous | 254 | 3.19 | 1.20 | 1.00 | 5.00 | −0.20 | −1.13 |
| NA | 90802 | 1.47 | 0.81 | 1.00 | 7.00 | 2.52 | 7.25 |
| PA | 91015 | 2.78 | 1.54 | 1.00 | 7.00 | 0.68 | −0.38 |
Note. Boldface are experience sampling measures. DTS = Distress tolerance scale, tol = tolerance, abs=absorption, app=appraisal, reg= regulation. PCL = PTSD checklist, intr=intrusion, avoid=avoidance, arous=arousal. NA=negative affect, PA= positive affect.
Table 2.
Correlation matrix
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | 1.00 | ||||||||
| 2. DTS_tol | 0.12 | 1.00 | |||||||
| 3. DTS_abs | 0.15* | 0.78*** | 1.00 | ||||||
| 4. DTS_app | 0.14* | 0.76*** | 0.76*** | 1.00 | |||||
| 5. DTS_reg | 0.02 | 0.63*** | 0.61*** | 0.62*** | 1.00 | ||||
| 6. PCL_intr | −0.04 | −0.46*** | −0.48*** | −0.58*** | −0.44*** | 1.00 | |||
| 7. PCL_avoid | −0.06 | −0.51*** | −0.57*** | −0.64*** | −0.43*** | 0.84*** | 1.00 | ||
| 8. PCL_hyper | 0.01 | −0.47*** | −0.51*** | −0.55*** | −0.37*** | 0.78*** | 0.85*** | 1.00 | |
| 9. NA | −0.01 | −0.34*** | −0.40*** | −0.41*** | −0.14* | 0.48*** | 0.51*** | 0.45*** | 1.00 |
| 10. PA | 0.10 | 0.17** | 0.22*** | 0.31*** | 0.11 | −0.24*** | −0.30*** | −0.29*** | −0.19** |
Note. N ranges from 250–254. DTS = Distress tolerance scale, tol = tolerance, abs=absorption, app=appraisal, reg= regulation. PCL = PTSD checklist, intr=intrusion, avoid=avoidance, arous=arousal. NA= person mean of negative affect, PA= person mean of positive affect.
p < 0.05,
p < 0.01,
p < 0.001
Dynamic Structural Equation Model
We estimated the DSEM in Mplus 8.3 with the Bayes estimator (see Figure 1) with approximately 90,000 assessments of positive and negative affect from 254 persons (see Table 1). This led to 256,579 observations due to incorporating missing data points into the temporal grid (see analysis plan). In the analysis, covariance coverage exceeded .35, which is acceptable based on simulation results indicating unbiased estimation with missing data rates up to 80–85% (Asparouhov et al., 2018) and simulation results (Schultzberg & Muthén, 2018) suggested adequate power for the model. The model included nine random effects; the intercept, autoregressive parameter (inertia), and the innovation variance (e.g., reactivity, lability, or exposure to stressors) for positive and negative affect, the two cross-lagged paths, and the innovation covariance. Table 3 includes the within-person standardized fixed effects (i.e., the within-person standardized effect for each parameter averaged across persons). The table includes the parameter estimate, the standard deviation of the posterior distribution (PSD), and the 95% credibility interval from the Bayes model. In Bayes analysis, parameters are considered to be variables and the analysis results in a distribution of the parameter given the data likelihood and the prior distribution (non-informative priors are used in the current analysis; Muthén, 2010; van de Schoot et al., 2014). Unlike confidence intervals, which typically assume a symmetric distribution, the credibility interval can be non-symmetric and reflect the probability that the parameter is within the specified range in the estimated posterior distribution (Muthén, 2010; van de Schoot et al., 2014). The fixed effects (average within-person association) for the autoregressive parameters for both positive (φpp) and negative affect (φnn) were significant (credible interval did not include 0) and moderately positive. There was a weak inverse association between lagged positive affect and subsequent negative affect (i.e., the cross-lagged effect from PA to NA (φnp)). The association between lagged negative affect and subsequent positive affect was not significant (i.e., the cross-lagged effect of NA to PA (φpn; see Table 3).
Table 3.
Within-level standardized estimates
| Parameter | β | PSD | 95% CI |
|---|---|---|---|
| φnn | 0.37 | 0.004 | (0.357, 0.374) |
| φpp | 0.48 | 0.004 | (0.476, 0.491) |
| φnp | −0.03 | 0.004 | (−0.035, −0.019) |
| φpn | 0.00 | 0.004 | (−0.008, 0.007) |
| δPAit | 0.65 | 0.003 | (0.641, 0.655) |
| δNAit | 0.52 | 0.006 | (0.508, 0.530) |
| ψit by | |||
| PA | 0.25 | 0.003 | (0.239, 0.250) |
| NA | −0.48 | 0.005 | (−0.488, −0.469) |
Note. φnn = NA autoregression, φpp PA autoregression, φpn= cross-lagged effect NA->PA, φnp= cross-lagged effect PA->NA, δPAit positive affect innovation, δNAit = negative affect innovation. ψit is the variance of the common factor η of the residuals, i.e., the residual covariance. The innovation parameters corresponding level 2 random variance terms are referred to as πPA and πNA (for the variances) and ψ for the covariance in subsequent tables of the between person effects. PSD = posterior standard deviation. CI = Bayes credibility interval.
The between-person variances and correlations of the random effects are in Table 4. A visual representation of the correlation structure is represented in Figure 2. Consistent with previous research (Hamaker et al., 2018), mean negative affect (μNA), negative affect inertia (φnn), and the negative affect innovation parameter (πNA) were positively correlated. Mean positive affect (μPA) and the positive affect innovation parameter (πPA) were positively associated as expected. However, the expected inverse association between positive affect inertia (φpp) and mean positive affect (μPA) was not observed (Hamaker et al., 2018; Houben et al., 2015). Mean positive (μPA) and negative affect (μNA) were not significantly associated; however, the innovation variance parameters (πPA and πNA) and autoregression effects (φnn and φpp) were significantly positively correlated. The cross-lagged effects (φnp and φpn) exhibited a very strong positive correlation. Other associations across affect were inverse. For example, negative affect inertia (φnn) was inversely associated with both the positive affect innovation variance parameter (πPA) and mean positive affect (μPA). Similarly, the positive affect inertia (φpp) was inversely associated with the negative affect innovation variance parameter (πNA) and mean negative affect (μNA).
Table 4.
Residual variances and correlations of random effects
| Variance (CI) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. φnn | 0.037 (0.030,0.046) | 1.00 | ||||||||
| 2. φpp | 0.027 (0.022,0.033) | 0.33 | 1.00 | |||||||
| 3. φnp | 0.002 (0.001,0.002 | 0.04 | −0.18 | 1.00 | ||||||
| 4. φpn | 0.012 (0.008,0.016) | −0.27 | −0.06 | 0.81 | 1.00 | |||||
| 5. log(πPA) | 0.891 (0.742,1.081) | −0.23 | −0.05 | 0.00 | −0.04 | 1.00 | ||||
| 6. log(πNA) | 1.749 (1.431,2.165) | 0.18 | −0.29 | 0.08 | −0.06 | 0.16 | 1.00 | |||
| 7. log(ψ) | 2.335 (1.918,2.858) | 0.04 | 0.05 | −0.41 | −0.27 | 0.44 | 0.13 | 1.00 | ||
| 8. μPA | 1.161 (0.971,1.402) | −0.18 | 0.07 | −0.14 | −0.08 | 0.43 | −0.19 | 0.39 | 1.00 | |
| 9. μNA | 0.223 (0.184,0.272) | 0.34 | −0.15 | 0.18 | 0.07 | 0.02 | 0.53 | 0.06 | −0.01 | 1.00 |
Note. μPA=positive affect mean (random intercept), μNA= negative affect mean (random intercept). φnn = NA autoregression, φpp PA autoregression, φpn= cross-lagged effect NA->PA, φnp= cross-lagged effect PA->NA, log(πPA) = log positive affect innovation variance, log(πNA)= log negative affect innovation variance, log(ψ)=log of negative innovation covariance. Bold face effects are significant based on 95% credibility interval (CI).
Figure 2.
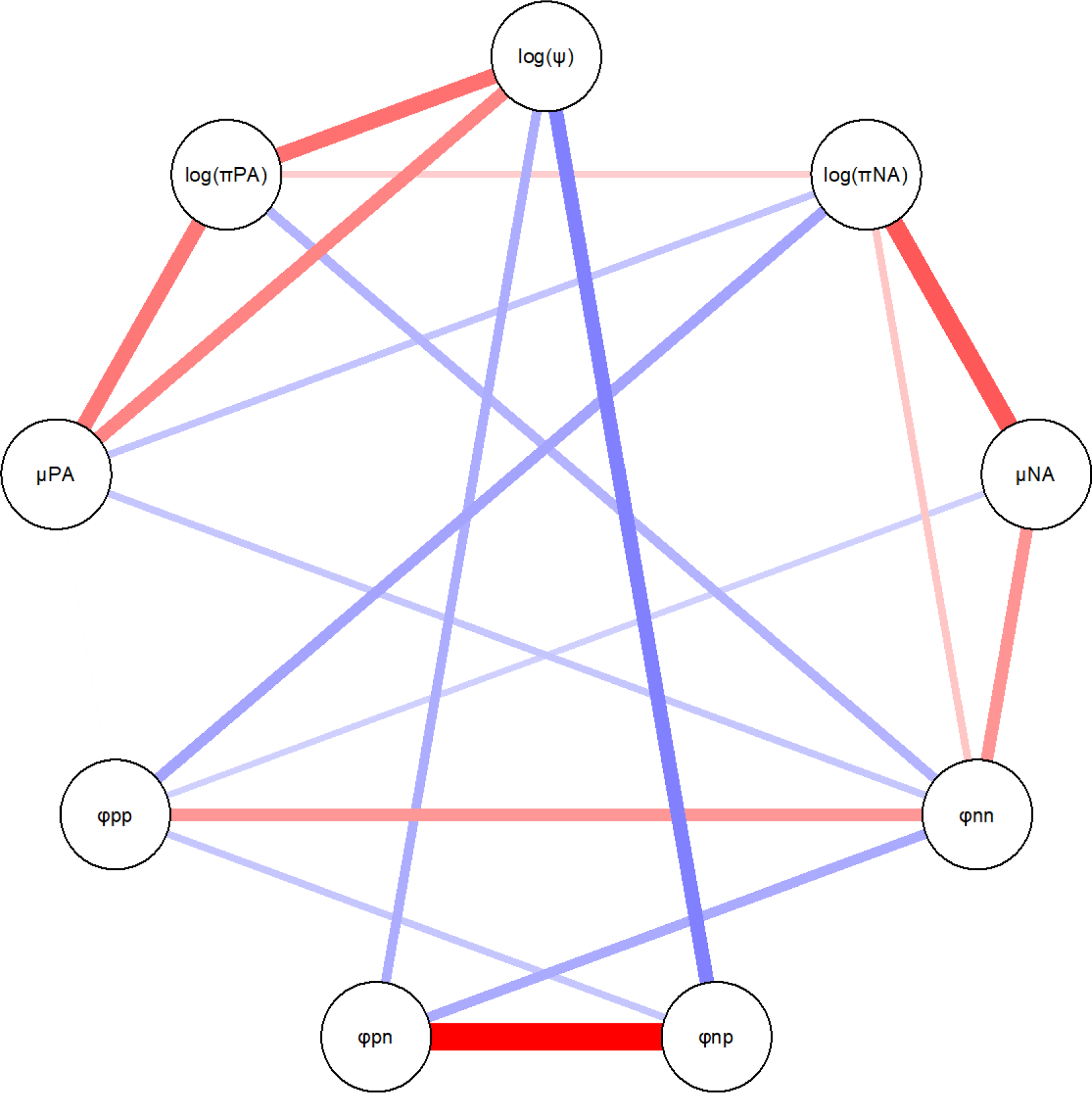
Significant correlations between random effects based on the 95% credibility interval. Red lines (grayscale solid) are positive correlations and blue lines (grayscale dashed) are negative. Stronger correlations are thicker and more saturated. Figure is include to aid comparison with Hamaker et al. (2018). Plot is made with qgraph (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012). μPA=positive affect mean (random intercept), μNA= negative affect mean (random intercept). φnn = NA autoregression, φpp PA autoregression, φpn= cross-lagged effect NA->PA, φnp= cross-lagged effect PA->NA, log(πPA) = log positive affect innovation variance, log(πNA)= log negative affect innovation variance, log(ψ)=log of negative innovation covariance.
Consistent with our hypothesis, PTSS at baseline were associated with higher mean levels of negative affect and lower mean levels of positive affect over the study period (see Table 5). The hypothesized association between PTSS and negative affect innovation variance was also significant. Distress tolerance predicted lower levels of negative affect inertia as expected. However, PTSS were not associated with increased negative affect inertia. Expected associations between the baseline measures and positive affect inertia or positive affect innovation variance were not supported. Though not a specific hypothesis, distress tolerance was associated with more positive associations between lagged negative affect and subsequent positive affect. This refers to a moderating effect of distress tolerance on the cross-lagged effect on negative affect to positive affect. However, decomposing the interaction to test simple effects (i.e., the strength of the cross-lagged effect at various levels of distress tolerance) indicated that the cross-lagged effects were not significant within the range of distress tolerance M −1 SD (b = −0.034 95% CI[−0.061, 0.008]) and distress tolerance M +1 SD (b = 0.026 95% CI[−0.001, 0.071]). Effects of gender were generally not significant. However, male gender was associated with weaker positive affect autoregressive effects (inertia) and men exhibited more tolerance for emotional distress relative to women.
Table 5.
Level 2 direct effects
| Variables | β | PSD | 95% CI |
|---|---|---|---|
| φnn ON | |||
| PTSS | 0.13 | 0.09 | (−0.06, 0.31) |
| DT | −0.23 | 0.10 | (−0.41, −0.04) |
| gender | −0.11 | 0.06 | (−0.23,0.02) |
|
| |||
| φnn ON | |||
| PTSS | −0.07 | 0.10 | (−0.26, 0.13) |
| DT | 0.08 | 0.10 | (−0.12, 0.27) |
| Gender | −0.16 | 0.07 | (−0.29, −0.03) |
|
| |||
| φnn ON | |||
| PTSS | 0.01 | 0.12 | (−0.23, 0.25) |
| DT | 0.00 | 0.13 | (−0.24, 0.25) |
| Gender | 0.04 | 0.08 | (−0.12, 0.20) |
|
| |||
| φnn ON | |||
| PTSS | 0.16 | 0.13 | (−0.10, 0.41) |
| DT | 0.27 | 0.12 | (0.03, 0.51) |
| Gender | 0.01 | 0.08 | (−0.15, 0.17) |
|
| |||
| log(πPA) ON | |||
| PTSS | 0.02 | 0.09 | (−0.17, 0.20) |
| DT | 0.12 | 0.10 | (−0.07, 0.30) |
| Gender | 0.04 | 0.06 | (−0.09, 0.16) |
|
| |||
| log(πNA) ON | |||
| PTSS | 0.54 | 0.08 | (0.38, 0.68) |
| DT | −0.02 | 0.09 | (−0.19, 0.15) |
| Gender | −0.04 | 0.06 | (−0.14, 0.07) |
|
| |||
| log(ψ) ON | |||
| PTSS | 0.09 | 0.10 | (−0.11, 0.28) |
| DT | −0.12 | 0.10 | (−0.31, 0.08) |
| Gender | −0.01 | 0.07 | (−0.14, 0.12) |
|
| |||
| μPA ON | |||
| PTSS | −0.24 | 0.09 | (−0.41, −0.06) |
| DT | 0.07 | 0.09 | (−0.11, 0.26) |
| Gender | 0.08 | 0.06 | (−0.05, 0.20) |
|
| |||
| μNA ON | |||
| PTSS | 0.48 | 0.08 | (0.33, 0.63) |
| DT | −0.08 | 0.08 | (−0.25, 0.08) |
| Gender | 0.01 | 0.06 | (−0.10, 0.12) |
Note. Standardized effects are reported. PSD = posterior standard deviation. μPA=positive affect mean (random intercept), μNA= negative affect mean (random intercept). φnn = NA autoregression, φpp PA autoregression, φpn= cross-lagged effect NA->PA, φnp= cross-lagged effect PA->NA, log(πPA) = log positive affect innovation variance, log(πNA)= log negative affect innovation variance, log(ψ)=log of negative innovation covariance. Bold face effects are significant based on 95% credibility interval (CI). DT=distress tolerance. PTSS=posttraumatic stress symptoms.
In addition to the direct effects of distress tolerance, there were several significant indirect effects (see Table 6). Distress tolerance, via its effect on PTSS, was indirectly associated with higher mean positive affect, lower mean negative affect, and lower negative affect innovation variance. Finally, though the direct and indirect effects of distress tolerance on the log of the negative innovation covariance were not significant, there was a significant total effect. This inverse total effect indicates that distress tolerance was associated with weaker covariance (closer to 0) between the innovations.
Table 6.
Level 2 indirect (via PTSS) and total effects of distress tolerance
| Indirect | total | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Outcome | b | PSD | 95% CI | b | PSD | 95% CI |
| φnn | −0.018 | 0.013 | (−0.045, 0.008) | −0.065 | 0.014 | (−0.094, −0.037) |
| φpp | 0.008 | 0.011 | (−0.015, 0.030) | 0.020 | 0.012 | (−0.003, 0.044) |
| φnp | 0.000 | 0.003 | (−0.007, 0.006) | 0.000 | 0.004 | (−0.008, 0.007) |
| φpn | −0.012 | 0.010 | (−0.032, 0.008) | 0.018 | 0.010 | (−0.001, 0.039) |
| log(πPA) | −0.010 | 0.062 | (−0.131, 0.116) | 0.101 | 0.066 | (−0.028, 0.231) |
| log(πNA) | −0.578 | 0.106 | (−0.803, −0.387) | −0.616 | 0.108 | (−0.833, −0.409) |
| log(ψ) | −0.092 | 0.106 | (−0.301, 0.114) | −0.276 | 0.112 | (−0.499, −0.058) |
| μPA | 0.181 | 0.073 | (0.043, 0.332) | 0.260 | 0.078 | (0.112, 0.418) |
| μNA | −0.184 | 0.036 | (−0.259, −0.119) | −0.232 | 0.038 | (−0.308, −0.160) |
Note. Effects are unstandardized. μPA=positive affect mean (random intercept), μNA= negative affect mean (random intercept). φnn = NA autoregression, φpp PA autoregression, φpn= cross-lagged effect NA->PA, φnp= cross-lagged effect PA->NA, log(πPA) = log positive affect innovation variance, log(πNA)= log negative affect innovation variance, log(ψ)=log of negative innovation covariance.
Bold face effects are significant based on 95% credibility interval (CI). PSD = posterior standard deviation.
Discussion
The current study applied recent advances in statistical modeling of intensive longitudinal data to understand individual differences in regulation of positive and negative affect in a sample of OIF/OEF/OND veterans. Consistent with previous research trait negative affect (i.e., mean across time) was positively associated with negative affect inertia (i.e., autoregression) as well as higher innovation variance (Hamaker et al., 2018; Simons et al., 2016). These findings suggest that veterans who experience greater sadness, anxiety, and anger may find these emotional states to be self-perpetuating and difficult to alleviate. In addition, their experience of negative emotion may seem erratic and unpredictable. Innovation variance reflects unobserved sources of heterogeneity (Asparouhov et al., 2018; Hamaker et al., 2018). In respect to emotional experience, this may be the result of increased reactivity or exposure to stressors (Hamaker et al., 2018). Irrespective of its cause, this may manifest as emotional lability (Simons et al., 2017). Less research has been conducted on the time course of positive affect. Here, we observed positive associations between trait positive affect and positive affect innovation variance but not positive affect inertia. Trait positive affect was inversely associated with negative affect inertia and well as negative affect innovation variance. Thus, veterans’ positive emotional experience is associated with both less persistence in negative affect as well as less labile negative states. Consistent with our hypothesis, PTSS in these veterans were positively associated with higher levels of negative affect and negative affect innovation variance (e.g., reactivity, lability) as well as lower trait positive affect. Distress tolerance exhibited indirect effects on these outcomes via its effect on PTSS at baseline. In addition, distress tolerance predicted lower negative affect inertia and more positive lagged effects between negative affect and subsequent positive affect. Thus, veterans’ who report better ability to withstand distress and maintain goal directed behavior when negatively aroused may tend to experience negative affect as more transient and less volatile and be characterized by more positive mood. Main findings are discussed in turn below.
Innovation variance
Innovation variance reflects the effect of all unobserved processes on the outcome (Hamaker et al., 2018). In our model, negative affect at time 𝑡𝑡 is a function of negative and positive affect at time t – 1, a lag of approximately 2 hours. The innovation variance is the variance of the residual and reflects factors, both internal and external, that contribute to momentary deviations in negative affect not accounted for by its modeled time course and the effect of the previous level of positive affect. This was modeled as a random effect and quantifies the extent to which an individual’s momentary mood deviates from expectation. Though speculative, this “uncertainty” in the statistical model may correspond to a sense of uncertainty and unpredictability for the veteran. Indeed, uncertainty-related anxiety has been tied to trauma and PTSD (Hirsh, Mar, & Peterson, 2012). Larger variance in negative affect residuals may reflect greater reactivity and/or exposure to stressors (Hamaker et al., 2018). Reactivity to trauma cues figure prominently in models of PTSD (Pineles et al., 2013), affect lability is associated with PTSS (Simons et al., 2017), and reactivity in negative affect more broadly is a common feature of regulatory problems associated with negative affectivity or neuroticism (Lahey, 2009). Here, we demonstrated that PTSS at baseline were associated with higher negative affect innovation variance, consistent with the interpretation of innovation variance reflecting greater stress reactivity or lability. Indeed, the prediction of negative affect innovation variance was one of the most robust findings, with the model accounting for 31% of the variance. Veterans struggling with symptoms of PTSD may experience negative emotions as volatile and unpredictable, contributing to an uncertain and potentially threating future.
Consistent with the pattern for negative affect, positive affect innovation variance was positively associated with trait positive affect. This may reflect an adaptive engagement with varied environmental stimuli (e.g., mindfulness; Chambers, Gullone, & Allen, 2009; Garland, Farb, Goldin, & Fredrickson, 2015); however, previous results have been mixed, observing both positive and inverse associations between positive affect innovation and trait positive affect (Hamaker et al., 2018). In addition, hypothesized associations between distress tolerance as well as PTSS and positive affect innovation variance were not supported. Hence further research is needed to understand the meaning of positive affect innovation variance in respect to affect regulation.
The DSEM for positive and negative affect included an innovation negative covariance, which reflected common sources of unobserved heterogeneity in positive and negative affect over time. Previous research indicated that depression is associated with stronger negative innovation covariance (Hamaker et al., 2018). This has been theorized to reflect deficits in emotional differentiation. Here, distress tolerance was associated with weaker innovation covariance. Previous research indicated inverse associations between alexithymia (e.g., poor emotional differentiation) and distress tolerance and thus results are supportive of this conceptualization of the negative covariance term (Gaher et al., 2013).
Inertia
Autoregression in emotion has been termed inertia or regulatory weakness (Hamaker, 2012; Hamaker et al., 2018; Koval et al., 2012; Kuppens et al., 2012). Conceptually this reflects the extent to which future emotional states are determined by current states. Individuals with high autoregression in negative affect may have difficulty regulating emotion to return to baseline and may engage in rumination (Koval et al., 2012). Whereas PTSS exhibited a positive direct effect on negative affect innovation, distress tolerance exhibited a significant inverse direct effect on negative affect inertia. The Distress Tolerance Scale includes a factor assessing the tendency to be “absorbed” by distress. The results here suggest that good tolerance for emotional distress may be associated with lower negative affect inertia and minimize perpetuation of negative affective states. Hence, veterans who perceive themselves as being able to effectively manage negative emotions have negative emotions that are more transient. The model accounted for 14% of the variance in negative affect inertia, whereas prediction of inertia in positive affect was considerably weaker (R2 = .05). Inertia in positive affect has been studied somewhat less and its interpretation is less clear. However, inertia in positive affect also exhibits inverse, albeit weaker, associations with well-being (Houben et al., 2015; Koval, Sütterlin, & Kuppens, 2016). In addition, laboratory research suggests that alcohol facilitates positive affect and sociability in part by reducing inertia in positive affect, allowing one to respond fully to momentary positive social cues (Fairbairn & Sayette, 2013). These findings suggest, that like negative affect inertia, inertia in positive affect is potentially maladaptive. Consistent with this idea, Hamaker and colleagues (2018) found positive associations between positive and negative affect inertia and an inverse association between positive affect inertia and trait positive affect in their younger community sample of 20 to 31 years old participants. However, findings are mixed, as positive affect inertia did not have these associations in their older sample (age 65 to 80 years). In addition, in the current sample and in Hamaker’s younger community sample, inertia in positive affect was inversely associated with negative affect innovation variance (e.g., reactivity). Finally, positive affect inertia was inversely associated with trait negative affect in the current sample. Hypothesized associations between PTSS, distress tolerance, and positive affect inertia were not supported. Further research is needed to understand how these parameters map onto adaptive and maladaptive emotional regulation processes.
Cross-lagged effects
Within-person cross-lagged effects were not significant and mean levels of positive and negative affect were not significantly correlated at the between person level. This is consistent with theoretical models that indicate the relative independence of the positive and negative affect systems (Paulus et al., 2017; Watson & Naragon, 2009). At the between-persons level, the cross-lagged effects were strongly positively related and exhibited weaker inverse associations with positive and negative affect inertia as well as the negative innovation covariance, which was consistent with the pattern observed in Hamaker and colleague’s (2018) younger sample. Though not a specific hypothesis, distress tolerance significantly moderated the lagged effect of negative affect on subsequent positive affect. Veterans with higher levels of tolerance for emotional distress tended to respond to negative affect with subsequent increases in positive affect. Such an effect may reflect the use of more adaptive emotion regulation strategies such as reflection or reappraisal in promoting change in positive affect (Brans, Koval, Verduyn, Lim, & Kuppens, 2013).
Strengths and Limitations
This is the largest experience sampling study of momentary affective experience of OIF/OEF/OND veterans to date with over 90,000 assessments of current emotion. The strengths of the dataset are complimented by recent developments in DSEM (Asparouhov et al., 2018) to provide a more comprehensive analysis of the time course of emotion than has previously been possible. The novelty of the approach also brings with it certain limitations. This paper closely followed the approach of Hamaker et al. (2018), which to our knowledge is the only comparable analysis in the literature. As such, there is not a large body of literature upon which to base hypotheses regarding either the pattern of random effects (e.g., correlations between innovation variances, inertia, cross-lagged effect, etc.) or the effects of PTSS and distress tolerance on these potential indices of affect regulation. The extant literature regarding associations between PTSD, distress tolerance, and affect regulation afford some hypotheses (e.g., expected associations between PTSS and negative affect innovation variance (e.g., reactivity)) but do not permit “strong” hypotheses (e.g., constraining a path to zero). As such we took a simpler approach and regressed all estimated parameters from the time-series model onto the predictors (i.e., gender, PTSS, and distress tolerance). Though estimated within the context of a model, the large number of estimated effects potentially increases the chance of type 1 errors. However, we think this approach is appropriate given the status of existing theory and empirical data.
Despite the complexity of the model, it does not address how the observed differences in affective dynamics relate to future PTSS. Hamaker and colleagues (2018) found that only negative affect inertia and the negative affect innovation covariance mediated associations between pre- and post- depressive disorder symptoms. Future research is needed to test hypotheses regarding affective dynamics and risk for and maintenance of PTSD and other forms of pathology. For example, the results here indicate that PTSS were associated with greater negative affect innovation variance (e.g., reactivity, lability) as hypothesized. However, the results do not speak to whether such reactivity predicts future symptoms over and above other affective dynamic parameters (e.g., negative affect mean or inertia). A recent meta-analysis of 16 affect dynamic constructs did not include innovation variance parameters nor PTSS (Dejonckheere et al., 2019). However, they concluded that many affect dynamic constructs (e.g., inertia, MSSD) explained little variance in retrospective assessments of well-being, depression, and borderline personality symptoms once the mean and standard deviation of negative and positive affect were controlled for (Dejonckheere et al., 2019).
In addition, the role of the dynamics of positive affect in respect to PTSD require further examination. Though research and theory implicate deficits in positive affect systems in PTSD (Vujanovic et al., 2017), we observed direct associations only with mean levels of positive affect. Further research in needed to clarify the role and meaning of autoregression and innovation variance in positive affect vis-a’-vis affect dysregulation. In addition, irrespective of valence, it should be emphasized that the innovation variance reflects all unobserved influences on the process (Hamaker, 2012). In respect to emotion, the innovation variance parameter may broadly correspond to emotional lability (i.e., the frequency, speed, and range of changes in emotion) that is unaccounted for by the model. However, the extent to which this reflects individual differences in emotional reactivity, exposure to stressors, or other factors is unknown. We have often conceptualized the innovation variance as reflecting differences in reactivity. However, further research is needed to examine how indices of emotional regulation are related to the innovation variance parameter.
Distress tolerance and PTSS were assessed together at baseline and the person-level affect dynamic parameters, though derived from the subsequent ESM study, represent a single measure of these individual difference variables. Hence, the between-person structural model does not allow for causal inference nor strong inferences regarding the temporal order of the variables. In the supplemental materials, we provide results from simpler univariate models as well as an equivalent unstructured multivariate model. Finally, the results reported here are specific to a 2-hour time lag. Analyses of the time course of affect that incorporate different time lags (e.g., 1 hour, 1 day) may result in different conclusions. Future research is needed to determine the sensitivity of the results to changes in the temporal lags.
Summary
Converging advances in data analysis and mobile technologies are paving the way for a renaissance in the study of psychopathology (Asparouhov et al., 2018; Hamaker et al., 2018; Hamaker & Wichers, 2017). Emotion, behavior, and other psychological processes can now be studied as dynamic systems that unfold over time on a day-to-day or moment-to-moment basis (Greene et al., 2018; Hamaker et al., 2018; Hamaker & Wichers, 2017). Decades of research in social and personality psychology highlights fundamental limitations in human’s ability to accurately identify causes of actions, acknowledge limitations of their expertise, and characterize their personality traits (Connelly & Ones, 2010; Huprich, Bornstein, & Schmitt, 2011; Kruger & Dunning, 1999; Ross, 2018). Indeed, an impetus for experience sampling and other forms of daily self-monitoring is to reduce effects of memory biases on retrospective self-report (Shiffman et al., 2008). Though retrospective self-report will, and should, remain a cornerstone of psychological assessment, data analytic approaches like those used here have the potential to provide insight into individuals’ moment-to-moment emotional experience that they may simply be unable to access through self-reflection. The results of this study, we hope, will provide a basis for future inquiries to advance understanding of the manifestation of emotion regulation difficulties experienced by veterans.
Supplementary Material
Acknowledgments
Data from this sample has been previously reported in Simons, Simons, O’Brien, Stoltenberg, Keith, & Hudson (2017), Simons, Simons, Walters, Keith, O’Brien, Andal, & Stoltenberg (2019), and Simons, Simons, Keith, Grimm, Stoltenberg, O’Brien, & Andal (2018). The previous papers do not include the affect experience sampling data reported here.
Research was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number R01AA020519. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Department of Veterans Affairs, or the United States Government. This research was supported with resources and the use of facilities at the Sioux Falls VA Health Care System, Bay Pines VA Health Care System, and the University of South Dakota.
Footnotes
Structured paths with cross-sectional data are often criticized. Ultimately, the association between distress tolerance and PTSS is likely a complex reciprocal association over time that cannot be modeled with these data. A third alternative that we considered was a simultaneous model with gender, distress tolerance, and PTSS being freely correlated exogenous predictors. We elected not to do this as it would not show the total effects of distress tolerance. However, we provide results of three additional models requested by reviewers in the supplemental materials (1. model with only distress tolerance, 2. model with only PTSS, 3. model with gender, distress tolerance, and PTSS unstructured).
Prior to testing the model with the random residual variances and covariance, we tested the model without random residual variances. For this model, the correlation between the positive and negative affect residuals was r = −.13 95%CI = [−.14, −.12], DIC = 1,416,018.68. In addition, we estimated a model with random residual variances and a positive covariance (DIC = 1,180,505.33). The lower DIC in the model with the negative random residual covariance (DIC = 1,056,655.27) in combination with the observed negative residual covariance in the model without random residual components supports the modeling of the negative covariance in the final model.
Contributor Information
Jeffrey S. Simons, Department of Psychology, The University of South Dakota
Raluca M. Simons, Disaster Mental Health Institute, Department of Psychology, The University of South Dakota
Kevin J. Grimm, Department of Psychology, Arizona State University
Jessica A. Keith, Bay Pines VA Health Care System
Scott F. Stoltenberg, Department of Psychology, The University of Nebraska – Lincoln
References
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Asparouhov T, Hamaker EL, & Muthén B (2018). Dynamic structural equation models. Structural equation modeling: a multidisciplinary journal, 25, 359–388. [Google Scholar]
- Asparouhov T, & Muthén B-O (2010). Bayesian Analysis Using Mplus: Technical Implementation: Version 3. Retrieved from Loas Angeles, CA: [Google Scholar]
- Badour CL, Resnick HS, & Kilpatrick DG (2017). Associations between specific negative emotions and DSM-5 PTSD among a national sample of interpersonal trauma survivors. Journal of Interpersonal Violence, 32, 1620–1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banducci AN, Connolly KM, Vujanovic AA, Alvarez J, & Bonn-Miller MO (2017). The impact of changes in distress tolerance on PTSD symptom severity post-treatment among veterans in residential trauma treatment. Journal of Anxiety Disorders, 47, 99–105. doi: 10.1016/j.janxdis.2017.01.004 [DOI] [PubMed] [Google Scholar]
- Banducci AN, Lejuez CW, Dougherty LR, & MacPherson L (2017). A Prospective Examination of the Relations Between Emotional Abuse and Anxiety: Moderation by Distress Tolerance. Prevention Science, 18, 20–30. doi: 10.1007/s11121-016-0691-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, Vujanovic AA, & Moos R (2009). Integrating Anxiety Sensitivity, Distress Tolerance, and Discomfort Intolerance: A Hierarchical Model of Affect Sensitivity and Tolerance. Behavior Therapy, 40, 291–301. doi: 10.1016/j.beth.2008.08.001 [DOI] [PubMed] [Google Scholar]
- Bersani FS, Morley C, Lindqvist D, Epel ES, Picard M, Yehuda R, . . . Mellon SH (2016). Mitochondrial DNA copy number is reduced in male combat veterans with PTSD. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 64, 10–17. doi: 10.1016/j.pnpbp.2015.06.012 [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Boffa JW, Short NA, Gibby BA, Stentz LA, & Schmidt NB (2018). Distress tolerance as a mechanism of PTSD symptom change: Evidence for mediation in a treatment-seeking sample. Psychiatry Research, 267, 400–408. doi: 10.1016/j.psychres.2018.03.085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borders A, McAndrew LM, Quigley KS, & Chandler HK (2012). Rumination Moderates the Associations Between PTSD and Depressive Symptoms and Risky Behaviors in U. S. Veterans. Journal of Traumatic Stress, 25, 583–586. doi: 10.1002/jts.21733 [DOI] [PubMed] [Google Scholar]
- Brans K, Koval P, Verduyn P, Lim YL, & Kuppens P (2013). The regulation of negative and positive affect in daily life. Emotion, 13, 926–939. doi: 10.1037/a0032400 [DOI] [PubMed] [Google Scholar]
- Brown WJ, Bruce SE, Buchholz KR, Artime TM, Hu E, & Sheline YI (2014). Affective Dispositions and PTSD Symptom Clusters in Female Interpersonal Trauma Survivors. Journal of Interpersonal Violence, 31, 407–424. doi: 10.1177/0886260514555866 [DOI] [PubMed] [Google Scholar]
- Brown WJ, Hetzel-Riggin MD, Mitchell MA, & Bruce SE (2018). Rumination Mediates the Relationship Between Negative Affect and Posttraumatic Stress Disorder Symptoms in Female Interpersonal Trauma Survivors. Journal of Interpersonal Violence, 0886260518818434. doi: 10.1177/0886260518818434 [DOI] [PubMed] [Google Scholar]
- Byllesby BM, Charak R, Durham TA, Wang X, & Elhai JD (2016). The Underlying Role of Negative Affect in the Association between PTSD, Major Depressive Disorder, and Generalized Anxiety Disorder. Journal of Psychopathology and Behavioral Assessment, 38, 655–665. doi: 10.1007/s10862-016-9555-9 [DOI] [Google Scholar]
- Chambers R, Gullone E, & Allen NB (2009). Mindful emotion regulation: An integrative review. Clinical Psychology Review, 29, 560–572. doi: 10.1016/j.cpr.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Cohen JR, Danielson CK, Adams ZW, & Ruggiero KJ (2016). Distress Tolerance and Social Support in Adolescence: Predicting Risk for Internalizing and Externalizing Symptoms Following a Natural Disaster. Journal of Psychopathology and Behavioral Assessment, 38, 538–546. doi: 10.1007/s10862-016-9545-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connelly BS, & Ones DS (2010). An other perspective on personality: Meta-analytic integration of observers’ accuracy and predictive validity. Psychological Bulletin, 136, 1092–1122. doi: 10.1037/a0021212 [DOI] [PubMed] [Google Scholar]
- de Haan-Rietdijk S, Kuppens P, & Hamaker EL (2016). What’s in a day? A guide to decomposing the variance in intensive longitudinal data. Frontiers in psychology, 7, 891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dejonckheere E, Mestdagh M, Houben M, Rutten I, Sels L, Kuppens P, & Tuerlinckx F (2019). Complex affect dynamics add limited information to the prediction of psychological well-being. Nat Hum Behav, 3, 478–491. doi: 10.1038/s41562-019-0555-0 [DOI] [PubMed] [Google Scholar]
- DePierro J, D’Andrea W, Frewen P, & Todman M (2018). Alterations in positive affect: Relationship to symptoms, traumatic experiences, and affect ratings. Psychol Trauma, 10, 585–593. doi: 10.1037/tra0000317 [DOI] [PubMed] [Google Scholar]
- Dormann C, & Griffin MA (2015). Optimal time lags in panel studies. Psychological Methods, 20, 489–505. doi: 10.1037/met0000041 [DOI] [PubMed] [Google Scholar]
- Dornbach-Bender A, Ruggero CJ, Schuler K, Contractor AA, Waszczuk M, Kleva CS, . . . Kotov R (2019). Positive and negative affect in the daily life of world trade center responders with PTSD: An ecological momentary assessment study. Psychol Trauma. doi: 10.1037/tra0000429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutton CE, Badour CL, Jones AC, Mischel ER, & Feldner MT (2016). Affective lability predicts decreased habituation in posttraumatic stress symptom responding during a single laboratory session of imaginal exposure. Journal of Anxiety Disorders, 43, 52–57. doi: 10.1016/j.janxdis.2016.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, & Borsboom D (2012). qgraph: Network Visualizations of Relationships in Psychometric Data. Journal of Statistical Software, 48, 1–18. [Google Scholar]
- Erwin MC, Mitchell MA, Contractor AA, Dranger P, Charak R, & Elhai JD (2018). The relationship between distress tolerance regulation, counterfactual rumination, and PTSD symptom clusters. Comprehensive Psychiatry, 82, 133–140. doi: 10.1016/j.comppsych.2018.01.012 [DOI] [PubMed] [Google Scholar]
- Fairbairn CE, & Sayette MA (2013). The effect of alcohol on emotional inertia: A test of alcohol myopia. Journal of Abnormal Psychology, 122, 770–781. doi: 10.1037/a0032980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felton JW, Banducci AN, Shadur JM, Stadnik R, MacPherson L, & Lejuez CW (2017). The developmental trajectory of perceived stress mediates the relations between distress tolerance and internalizing symptoms among youth. Development and Psychopathology, 29, 1391–1401. doi: 10.1017/s0954579417000335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (January, 2010). Structured Clinical Interview of DSM-IV-TR Axis I Disorders Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/ PSY SCREEN). New York: New York State Psychiatric Institute. [Google Scholar]
- Fitzgerald JM, Gorka SM, Kujawa A, DiGangi JA, Proescher E, Greenstein JE, . . . Phan KL (2018). Neural indices of emotional reactivity and regulation predict course of PTSD symptoms in combat-exposed veterans. Prog Neuropsychopharmacol Biol Psychiatry, 82, 255–262. doi: 10.1016/j.pnpbp.2017.11.005 [DOI] [PubMed] [Google Scholar]
- Gaher RM, Hofman NL, Simons JS, & Hunsaker R (2013). Emotion regulation deficits as mediators between trauma exposure and borderline symptoms. Cognitive Therapy and Research, 37, 466–475. [Google Scholar]
- Gaher RM, Simons JS, Hahn AM, Hofman NL, Hansen J, & Buchkoski J (2014). An Experience Sampling Study of PTSD and Alcohol-Related Problems. Psychology of Addictive Behaviors. doi: 10.1037/a0037257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Farb NA, Goldin P, & Fredrickson BL (2015). Mindfulness Broadens Awareness and Builds Eudaimonic Meaning: A Process Model of Mindful Positive Emotion Regulation. Psychological Inquiry, 26, 293–314. doi: 10.1080/1047840X.2015.1064294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geldhof GJ, Preacher KJ, & Zyphur MJ (2014). Reliability estimation in a multilevel confirmatory factor analysis framework. Psychological Methods, 19, 72–91. doi: 10.1037/a0032138 [DOI] [PubMed] [Google Scholar]
- Gollob HF, & Reichardt CS (1987). Taking account of time lags in causal models. Child Development, 58, 80–92. doi: 10.2307/1130293 [DOI] [PubMed] [Google Scholar]
- Greene T, Gelkopf M, Epskamp S, & Fried E (2018). Dynamic networks of PTSD symptoms during conflict. Psychological Medicine, 48, 2409–2417. doi: 10.1017/S0033291718000351 [DOI] [PubMed] [Google Scholar]
- Hamaker E, Ceulemans E, Grasman R, & Tuerlinckx F (2015). Modeling affect dynamics: State of the art and future challenges. Emotion Review, 7, 316–322. [Google Scholar]
- Hamaker EL (2012). Why researchers should think “within-person”: A paradigmatic rationale. In Mehl MR & Conner TS (Eds.), Handbook of research methods for studying daily life (pp. 43–61). New York: Guilford. [Google Scholar]
- Hamaker EL, Asparouhov T, Brose A, Schmiedek F, & Muthén B (2018). At the Frontiers of Modeling Intensive Longitudinal Data: Dynamic Structural Equation Models for the Affective Measurements from the COGITO Study. Multivariate Behavioral Research, 1–22. doi: 10.1080/00273171.2018.1446819 [DOI] [PubMed] [Google Scholar]
- Hamaker EL, & Wichers M (2017). No time like the present: Discovering the hidden dynamics in intensive longitudinal data. Current Directions in Psychological Science, 26, 10–15. [Google Scholar]
- Hirsh JB, Mar RA, & Peterson JB (2012). Psychological entropy: A framework for understanding uncertainty-related anxiety. Psychological Review, 119, 304–320. [DOI] [PubMed] [Google Scholar]
- Houben M, Van Den Noortgate W, & Kuppens P (2015). The relation between short-term emotion dynamics and psychological well-being: A meta-analysis. Psychological Bulletin, 141, 901–930. doi: 10.1037/a0038822 [DOI] [PubMed] [Google Scholar]
- Huprich SK, Bornstein RF, & Schmitt TA (2011). Self-report methodology is insufficient for improving the assessment and classification of Axis II personality disorders. Journal of Personality Disorders, 25, 557–570. doi: 10.1521/pedi.2011.25.5.557 [DOI] [PubMed] [Google Scholar]
- Jahng S, Wood PK, & Trull TJ (2008). Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychological Methods, 13, 354–375. doi: 10.1037/a0014173 [DOI] [PubMed] [Google Scholar]
- Jeffries ER, McLeish AC, Kraemer KM, Avallone KM, & Fleming JB (2015). The Role of Distress Tolerance in the Use of Specific Emotion Regulation Strategies. Behavior Modification, 40, 439–451. doi: 10.1177/0145445515619596 [DOI] [PubMed] [Google Scholar]
- Kaczmarek M, & Zawadzki B (2014). Exposure to Trauma, Emotional Reactivity, and Its Interaction as Predictors of the Intensity of PTSD Symptoms in the Aftermath of Motor Vehicle Accidents. Journal of Russian & East European Psychology, 50, 47–64. doi: 10.2753/rpo1061-0405500303 [DOI] [Google Scholar]
- Kiselica AM, Rojas E, Bornovalova MA, & Dube C (2015). The Nomological Network of Self-Reported Distress Tolerance. Assessment, 22, 715–729. doi: 10.1177/1073191114559407 [DOI] [PubMed] [Google Scholar]
- Koval P, Kuppens P, Allen NB, & Sheeber L (2012). Getting stuck in depression: the roles of rumination and emotional inertia. Cogn Emot, 26, 1412–1427. doi: 10.1080/02699931.2012.667392 [DOI] [PubMed] [Google Scholar]
- Koval P, Pe ML, Meers K, & Kuppens P (2013). Affect dynamics in relation to depressive symptoms: Variable, unstable or inert? Emotion, 13, 1132–1141. [DOI] [PubMed] [Google Scholar]
- Koval P, Sütterlin S, & Kuppens P (2016). Emotional Inertia is Associated with Lower Well-Being when Controlling for Differences in Emotional Context. Frontiers in psychology, 6. doi: 10.3389/fpsyg.2015.01997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger J, & Dunning D (1999). Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. Journal of Personality and Social Psychology, 77, 1121–1134. [DOI] [PubMed] [Google Scholar]
- Kuppens P, Sheeber LB, Yap MBH, Whittle S, Simmons JG, & Allen NB (2012). Emotional inertia prospectively predicts the onset of depressive disorder in adolescence. Emotion, 12, 283–289. doi: 10.1037/a0025046 [DOI] [PubMed] [Google Scholar]
- Lahey BB (2009). Public health significance of neuroticism. The American psychologist, 64, 241–256. doi: 10.1037/a0015309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson R, & Csikszentmihalyi M (1983). The Experience Sampling Method. New Directions for Methodology of Social & Behavioral Science, 15, 41–56. [Google Scholar]
- Lieberman L, Gorka SM, DiGangi JA, Frederick A, & Phan KL (2017). Impact of posttraumatic stress symptom dimensions on amygdala reactivity to emotional faces. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 79, 401–407. doi: 10.1016/j.pnpbp.2017.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM (1993). Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Ludtke O, Marsh HW, Robitzsch A, Trautwein U, Asparouhov T, & Muthen B (2008). The multilevel latent covariate model: a new, more reliable approach to group-level effects in contextual studies. Psychological Methods, 13, 203–229. doi: 10.1037/a0012869 [DOI] [PubMed] [Google Scholar]
- Magidson JF, Listhaus AR, Seitz-Brown C, Anderson KE, Lindberg B, Wilson A, & Daughters SB (2013). Rumination mediates the relationship between distress tolerance and depressive symptoms among substance users. Cognitive Therapy and Research, 37, 456–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, Bonn-Miller MO, Bernstein A, & Zvolensky MJ (2010). Multimethod study of distress tolerance and PTSD symptom severity in a trauma-exposed community sample. Journal of Traumatic Stress, 23, 623–630. doi: 10.1002/jts.20568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald RP (1999). Test theory: A unified treatment. Mahwah, NJ: Erlbaum. [Google Scholar]
- Muthén BO (2010). Bayesian analysis in Mplus: A brief introduction. Retrieved from [Google Scholar]
- Muthén LK, & Muthén BO (2018). Mplus Statistical Modeling Software: Release 8.2. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Naragon-Gainey K, McMahon TP, & Chacko TP (2017). The structure of common emotion regulation strategies: A meta-analytic examination. Psychological Bulletin, 143, 384–427. doi: 10.1037/bul0000093 [DOI] [PubMed] [Google Scholar]
- Nawijn L, van Zuiden M, Frijling JL, Koch SBJ, Veltman DJ, & Olff M (2015). Reward functioning in PTSD: A systematic review exploring the mechanisms underlying anhedonia. Neuroscience and Biobehavioral Reviews, 51, 189–204. doi: 10.1016/j.neubiorev.2015.01.019 [DOI] [PubMed] [Google Scholar]
- Newton T, & Ho I (2008). Posttraumatic Stress Symptoms and Emotion Experience in Women: Emotion Occurrence, Intensity, and Variability in the Natural Environment. Journal of Psychological Trauma, 7, 276–297. doi: 10.1080/19322880802492237 [DOI] [Google Scholar]
- Nock MK, Wedig MM, Holmberg EB, & Hooley JM (2008). The emotion reactivity scale: development, evaluation, and relation to self-injurious thoughts and behaviors. Behavior Therapy, 39, 107–116. doi: 10.1016/j.beth.2007.05.005 [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, & Lyubomirsky S (2008). Rethinking rumination. Perspectives on Psychological Science, 3, 400–424. doi: 10.1111/j.1745-6924.2008.00088.x [DOI] [PubMed] [Google Scholar]
- Oliver MNI, & Simons JS (2004). The Affective Lability Scales: Development of a Short-form Measure. Personality and Individual Differences, 37, 1279–1288. doi: 10.1016/j.paid.2003.12.013 [DOI] [Google Scholar]
- Paulus MP, Stein MB, Craske MG, Bookheimer S, Taylor CT, Simmons AN, . . . Fan B (2017). Latent variable analysis of positive and negative valence processing focused on symptom and behavioral units of analysis in mood and anxiety disorders. Journal of Affective Disorders, 216, 17–29. doi: 10.1016/j.jad.2016.12.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineles SL, Suvak MK, Liverant GI, Gregor K, Wisco BE, Pitman RK, & Orr SP (2013). Psychophysiologic reactivity, subjective distress, and their associations with PTSD diagnosis. Journal of Abnormal Psychology, 122, 635–644. doi: 10.1037/a0033942 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Zyphur MJ, & Zhang Z (2010). A general multilevel SEM framework for assessing multilevel mediation. Psychological Methods, 15, 209–233. doi: 10.1037/a0020141 [DOI] [PubMed] [Google Scholar]
- Preece DA, Becerra R, Robinson K, & Gross JJ (2019). The emotion regulation questionnaire: Psychometric properties in general community samples. Journal of Personality Assessment. doi: 10.1080/00223891.2018.1564319 [DOI] [PubMed] [Google Scholar]
- Ross L (2018). From the fundamental attribution error to the truly fundamental attribution error and beyond: My research journey. Perspectives on Psychological Science, 13, 750–769. doi: 10.1177/1745691618769855 [DOI] [PubMed] [Google Scholar]
- Sandin B, Simons JS, Valiente RM, Simons RM, & Chorot P (2017). Psychometric properties of the spanish version of The Distress Tolerance Scale and its relationship with personality and psychopathological symptoms. Psicothema, 29, 421–428. doi: 10.7334/psicothema2016.239 [DOI] [PubMed] [Google Scholar]
- Schultzberg M, & Muthén B (2018). Number of subjects and time points needed for multilevel time-series analysis: A simulation study of dynamic structural equation modeling. Structural equation modeling: a multidisciplinary journal, 25, 495–515. [Google Scholar]
- Seligowski AV, & Orcutt HK (2016). Support for the 7-factor hybrid model of PTSD in a community sample. Psychol Trauma, 8, 218–221. doi: 10.1037/tra0000104 [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32. [DOI] [PubMed] [Google Scholar]
- Simons JS, Emery NN, Simons RM, Wills TA, & Webb MK (2016). Effects of alcohol, rumination, and gender on the time course of negative affect. Cogn Emot, 1–14. doi: 10.1080/02699931.2016.1226162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motiv Emot, 29, 83–102. [Google Scholar]
- Simons JS, Gaher RM, Oliver MNI, Bush JA, & Palmer MA (2005). An experience sampling study of associations between affect and alcohol use and problems among college students. Journal of Studies on Alcohol, 66, 459 – 469. [DOI] [PubMed] [Google Scholar]
- Simons JS, Simons RM, Keith JA, Grimm KJ, Stoltenberg SF, O’Brien C, & Andal K (2018). PTSD symptoms and alcohol-related problems among veterans: Temporal associations and vulnerability. Journal of Abnormal Psychology, 127, 733–750. doi: 10.1037/abn0000376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Simons RM, O’Brien C, Stoltenberg SF, Keith JA, & Hudson JA (2017). PTSD, alcohol dependence, and conduct problems: Distinct pathways via lability and disinhibition. Addictive Behaviors, 64, 185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Simons RM, Walters KJ, Keith JA, O’Brien C, Andal K, & Stoltenberg SF (2019). Nexus of despair: A network analysis of suicidal ideation among veterans. Arch Suicide Res, 1–44. doi: 10.1080/13811118.2019.1574689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Wills TA, & Neal DJ (2014). The many faces of affect: A multilevel model of drinking frequency/quantity and alcohol dependence symptoms among young adults. Journal of Abnormal Psychology, 123, 676–694. doi: 10.1037/a0036926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiller TR, Liddell BJ, Schick M, Morina N, Schnyder U, Pfaltz M, . . . Nickerson A (2019). Emotional Reactivity, Emotion Regulation Capacity, and Posttraumatic Stress Disorder in Traumatized Refugees: An Experimental Investigation. Journal of Traumatic Stress, 32, 32–41. doi: 10.1002/jts.22371 [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Penninx BW, Krempeniou A, van Hemert AM, & Elzinga B (2015). Trait rumination predicts onset of Post-Traumatic Stress Disorder through trauma-related cognitive appraisals: A 4-year longitudinal study. Behaviour Research and Therapy, 71, 101–109. doi: 10.1016/j.brat.2015.06.004 [DOI] [PubMed] [Google Scholar]
- Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, & Gotlib IH (2012). The everyday emotional experience of adults with major depressive disorder: Examining emotional instability, inertia, and reactivity. Journal of Abnormal Psychology, 121, 819–829. doi: 10.1037/a0027978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, & Watson D (2008). Affective instability: measuring a core feature of borderline personality disorder with ecological momentary assessment. Journal of Abnormal Psychology, 117, 647–661. doi: 10.1037/a0012532 [DOI] [PubMed] [Google Scholar]
- van de Schoot R, Kaplan D, Denissen J, Asendorpf JB, Neyer FJ, & van Aken MAG (2014). A Gentle Introduction to Bayesian Analysis: Applications to Developmental Research. Child Development, 85, 842–860. doi: 10.1111/cdev.12169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viana AG, Paulus DJ, Garza M, Lemaire C, Bakhshaie J, Cardoso JB, . . . Zvolensky MJ (2017). Rumination and PTSD symptoms among trauma-exposed Latinos in primary care: Is mindful attention helpful? Psychiatry Research, 258, 244–249. doi: 10.1016/j.psychres.2017.08.042 [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Bonn-Miller MO, Potter CM, Marshall EC, & Zvolensky MJ (2011). An evaluation of the relation between distress tolerance and posttraumatic stress within a trauma-exposed sample. Journal of Psychopathology and Behavioral Assessment, 33, 129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Hart AS, Potter CM, Berenz EC, Niles B, & Bernstein A (2013). Main and Interactive Effects of Distress Tolerance and Negative Affect Intensity in Relation to PTSD Symptoms among Trauma-Exposed Adults. Journal of Psychopathology and Behavioral Assessment, 35, 235–243. doi: 10.1007/s10862-012-9325-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Litz BT, & Farris SG (2015). Distress Tolerance as Risk and Maintenance Factor for PTSD: Empirical and Clinical Implications Comprehensive Guide to Post-Traumatic Stress Disorder (pp. 1–13). [Google Scholar]
- Vujanovic AA, Wardle MC, Smith LJ, & Berenz EC (2017). Reward functioning in posttraumatic stress and substance use disorders. Current Opinion in Psychology, 14, 49–55. doi: 10.1016/j.copsyc.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1999). The PANAS - X: Manual for the Positive and Negative Affective Schedule. The University of Iowa: Unpublished Manuscript. [Google Scholar]
- Watson D, & Naragon K (2009). Positive affectivity: The disposition to experience positive emotional states. In Lopez SJ & Snyder CR (Eds.), Oxford handbook of positive psychology (2nd ed.). (pp. 207–215). New York, NY US: Oxford University Press. [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, & Keane T (1993). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the International Society of Traumatic Stress Studies, San Antonio, TX. http://www.pdhealth.mil/library/downloads/PCL_sychometrics.doc [Google Scholar]
- Zelkowitz RL, & Cole DA (2016). Measures of emotion reactivity and emotion regulation: Convergent and discriminant validity. Personality and Individual Differences, 102, 123–132. doi: 10.1016/j.paid.2016.06.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


