Abstract
BACKGROUND/OBJECTIVE:
The Centers for Medicare & Medicaid Services (CMS) reimburses clinicians for advance care planning (ACP) discussions with Medicare patients. The objective of the study was to examine the association of CMS-billed ACP visits with end-of-life (EOL) healthcare utilization.
DESIGN:
Patient-level analyses of claims for the random 20% Medicare fee-for-service (FFS) sample of decedents in 2017. To account for multiple comparisons, Bonferroni adjusted P value <.008 was considered statistically significant.
SETTING:
Nationally representative sample of Medicare FFS beneficiaries.
PARTICIPANTS:
A total of 237,989 Medicare FFS beneficiaries who died in 2017 and included those with and without a billed ACP visit during 2016–17.
INTERVENTION:
The key exposure variable was receipt of first billed ACP (none, >1 month before death).
MEASUREMENTS:
Six measures of EOL healthcare utilization or intensity (inpatient admission, emergency department [ED] visit, intensive care unit [ICU] stay, and expenditures within 30 days of death, in-hospital death, and first hospice within 3 days of death). Analyses was adjusted for age, race, sex, Charlson Comorbidity Index, expenditure by Dartmouth hospital referral region (high, medium, or low), and dual eligibility.
RESULTS:
Overall, 6.3% (14,986) of the sample had at least one billed ACP visit. After multivariable adjustment, patients with an ACP visit experienced significantly less intensive EOL care on four of six measures: hospitalization (odds ratio [OR] = .77; 95% confidence interval [CI] = .74–.79), ED visit (OR = .77; 95% CI = .75–.80), or ICU stay (OR = .78; 95% CI = .74–.81) within a month of death; and they were less likely to die in the hospital (OR = .79; 95% CI = .76–.82). There were no differences in the rate of late hospice enrollment (OR = .97; 95% CI = .92–1.01; P = .119) or mean expenditures ($242.50; 95% CI = −$103.63 to $588.61; P = .169).
CONCLUSION:
Billed ACP visits were relatively uncommon among Medicare FFS decedents, but their occurrence was associated with less intensive EOL utilization. Further research on the variables affecting hospice use and expenditures in the EOL period is recommended to understand the relative role of ACP.
Keywords: advance care planning, Medicare, end of life
Advance care planning (ACP) is increasingly recognized as important for quality end-of-life (EOL) care.1–3 It helps patients make important decisions and have control over the care they receive.4 ACP is associated with a lower likelihood of dying in the hospital,5 intensive care unit (ICU) admission6 or hospital admission in the last 30 days,7 and receiving life-supporting measures,6,8 and with a higher likelihood of hospice enrollment5,6,8 and receipt of timely hospice care before death.5,6 The associations between ACP and EOL care have generally relied on measures such as completion of advance directives (ADs) or living wills, or assignment of durable power of attorney (DPOA), and they have used proxy interviews to obtain this information about the decedents.1,5,9,10
The paradigm of ACP has evolved over the years. Although historically the documentation of living wills or ADs was considered successful ACP, the current consensus is that ACP “is a process, rather than a singular moment or document, that supports adults at any age or stage of health in understanding and sharing their personal values, life goals, and preferences regarding future medical care.”11 This “communication-based ACP, not just form-based ACP” has been “shown to have a range of benefits including an increased likelihood that patients’ wishes will be honored at the end of life, as well as decreased stress for surrogate decision makers.”11 To account for this, one study of EOL quality defined ACP broadly as having an AD or DPOA or having discussions with the next of kin.5 Another used electronic health records from a small sample of patients to retrieve ACP documentation from the problem list.7
Starting in 2016, the Centers for Medicare & Medicaid Services (CMS) began compensating clinicians for time-based ACP services using Common Procedural Technology codes 99497 and 99498.12 To bill for ACP using the primary code (99497), clinicians are required to speak with their patients, with or without families, for at least 15 to 30 minutes. If the conversation continues beyond 30 minutes, clinicians can bill using an additional secondary code (99498) for every additional 30 minutes. By requiring conversation, the institution of billing codes may impact downstream care more than just the presence of ADs. Recent investigations described the initial uptake of ACP billing codes among Medicare beneficiaries13,14 but without examining the impact of these services on EOL care patient outcomes.14 We used national Medicare claims to examine the association of having billed ACP conversations with EOL care outcomes among Medicare beneficiaries who died in 2017. We hypothesized that patients with billed ACP conversations will receive less intensive EOL care measures.
METHODS
Data Set and Study Population
We used the CMS administrative enrollment and claims data to select a 20% random sample of fee-for-service (FFS) Medicare beneficiaries from 2016 to 2017, excluding patients with managed care coverage. In our cohort, we identified beneficiaries aged 65 and older who died in 2017 but were continuously enrolled in Medicare Parts A and B plan coverage in the full calendar year 2016 and up until death in 2017. Claims for these individual patients were linked with the Medicare Beneficiary Summary file, Inpatient, Outpatient, Skilled Nursing Facility (SNF), Hospice, and Carrier files for 2 years using the Beneficiary Identification Code. Beneficiaries with their first ACP claims within 30 days of death were excluded from analysis to ensure temporality of the exposure (billed ACP) and EOL outcomes. For example, the emergency department (ED) visit may have prompted the ACP visit, thus reversing the direction of causality. In other words, if ACP claims from within 30 days of death are included in analyses, the time period of exposure measurement will overlap with the measurement time period for EOL outcomes, impeding our ability to confirm that the exposure preceded the outcome.
Advance Care Planning Billed Visits
The exposure variable was receipt of ACP identified via ACP claims using either the primary code 99497 (first 30 minutes) or the secondary code 99498 (extended time beyond 30 minutes) or both. Multiple billing codes for the same visit on the same day were counted only once for analysis. After excluding beneficiaries who received their first ACP within 30 days of death, the remaining beneficiaries were classified into “no billed ACP” (if neither the primary nor the secondary billing code was used in any visit from 2016 to 2017) and “had billed ACP” (if at least one billing code was used in any visit from 2016 to 2017, until 30 days before the death). Beneficiaries with multiple ACP claims were classified as “had ACP,” and only their first ACP claim was used for analyses.
End-of-Life Utilization Measures
We used six measures of EOL healthcare utilization or intensity based on the literature and those that were endorsed by the National Quality Forum.15–17 (1) “Inpatient admission,” defined as at least one hospital admission within the last 30 days of life; (2) “in-hospital death,” defined as a death that occurred in the hospital; (3) “ED visit,” defined as at least one ED visit within the last 30 days of life; (4) “ICU stay,” defined as at least one admission to ICU within the last 30 days of life; (5) “late hospice,” defined as first hospice referral within the last 3 days before death5; and (6) “expenditures,” calculated as total costs including all the inpatient, outpatient, SNF, and hospice expenses in the last 30 days of life.
Confounding Variables
Analyses were adjusted for the following potential confounders based on the previous literature on EOL outcomes and EOL care intensity18–20: sex (male, female), age (65–69, 70–74, 75–79, 80–84, 85–89, 90–94, and ≥95 years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian, other, or unknown), Charlson Comorbidity Index (CCI) using a 12-month look-back period in 2016 (0, 1, 2, 3, 4, 5, or more), and dual-eligibility status for Medicare and Medicaid. Because EOL intensity is known to exhibit geographic variation, we assigned patients to hospital referral regions (HRRs), a standard geographic unit for assessing variation in health services used by the Dartmouth Institute.21 Total Medicare spending by HRR was computed by averaging the age, sex, and race-adjusted expenses for all Medicare beneficiaries over a 5-year period from 2012 to 2016 (https://atlasdata.dartmouth.edu/static/general_atlas_rates#spending). Each HRR was then categorized into “high” (>75th percentile), medium (25th to 75th percentile), or low (<25th percentile) level of spending.
Statistical Analysis
A retrospective patient-level analysis was conducted to examine EOL care among those who “had billed ACP” as compared with patients with “no billed ACP.” Chi-square tests were used to report bivariate results. Multivariable logistic regression models were computed for binary outcomes to produce the odds of an outcome among “had billed ACP” patients compared with “no billed ACP” patients, adjusting for confounders. For EOL expenditures, a multivariable linear regression model was computed to produce adjusted mean expenditures. All significance tests were two sided. To adjust for multiple hypothesis testing for the six outcomes, the P value was adjusted using Bonferroni correction22 to consider P < .008 as statistically significant. SAS software, v.9.4 (SAS Institute, Cary, NC) was used to conduct all analyses. The study was approved by the institutional review board at Partners Healthcare. Data were provided by the CMS and used under an appropriate Data Use Agreement.
RESULTS
Sample Characteristics
A total of 269,646 FFS Medicare beneficiaries in the 20% sample died in 2017. Excluding 9,209 individuals who received the first billed ACP within the last 30 days of death, 22,108 who were younger than 65 years, and 340 who had any missing variables of interest or confounding variables, the final analytic sample consisted of 237,989 decedents. Most were females (54.3%), 85 to 89 years of age (19.8%), and non-Hispanic white (87.2%). A total of 55% of the patients were assigned to the medium intensity HRRs based on their Medicare spending. Approximately 24% of the patients had a CCI of 5 or above, and 26.9% had dual eligibility (Table 1). Among decedents, 6.3% had a first ACP claim before the last 30 days of life. There was an average of 209.7 days between first billed ACP and death (median = 166), and an average of 169.1 days between most recent billed ACP and death (median = 120). Also, 34.4% of beneficiaries who had billed ACP had more than one ACP visit before death. Table 1 provides the proportion of patients within each of the two groups (“no billed ACP” and “had billed ACP”) who have the listed demographic, comorbidity, and dual-eligibility characteristics. The groups were dissimilar in all listed characteristics (P < .05), and the difference ranged from .0 to 8.5 percentage points. As compared with the beneficiaries without a billed ACP, those with a billed ACP visit were more likely to be female (55.8% vs 54.2%), older, such as 80 to 84 years (17.6% vs 17.1%), 85 to 89 years (21.4% vs 19.7%), and 90 to 94 years (17.6% vs 17.0%), non-Hispanic black (8.7% vs 7.9%), Hispanic (1.6% vs 1.4%), Asian (2.0% vs 1.4%), belonging to the high-intensity spending HRRs (30.7% vs 26.9%), with four comorbidities (16.0% vs 14.5%), and with five or more comorbidities (32.1% vs 23.7%).
Table 1.
Characteristics of Medicare Patients Who Died in 2017 (N = 237,989)
| Total | No billed ACP | Had billed ACP | |||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | P value | |
| 237,989 | 100.0 | 223,003 | 93.7 | 14,986 | 6.3 | ||
| Sex | |||||||
| Male | 108,835 | 45.7 | 102,205 | 45.8 | 6,630 | 44.2 | .0002 |
| Female | 129,154 | 54.3 | 120,798 | 54.2 | 8,356 | 55.8 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| Age categories, y | |||||||
| 65–69 | 21,623 | 9.1 | 20,525 | 9.2 | 1,098 | 7.3 | <.0001 |
| 70–74 | 30,622 | 12.9 | 28,804 | 12.9 | 1818 | 12.1 | |
| 75–79 | 34,804 | 14.6 | 32,610 | 14.6 | 2,194 | 14.6 | |
| 80–84 | 40,861 | 17.2 | 38,218 | 17.1 | 2,643 | 17.6 | |
| 85–89 | 47,191 | 19.8 | 43,979 | 19.7 | 3,212 | 21.4 | |
| 90–94 | 40,587 | 17.1 | 37,957 | 17.0 | 2,630 | 17.6 | |
| ≥95 | 22,301 | 9.4 | 20,910 | 9.4 | 1,391 | 9.3 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| Race/Ethnicity | |||||||
| Non-Hispanic white | 207,510 | 87.2 | 194,645 | 87.3 | 12,865 | 85.9 | <.0001 |
| Non-Hispanic black | 18,938 | 8.0 | 17,633 | 7.9 | 1,305 | 8.7 | |
| Hispanic | 3,428 | 1.4 | 3,185 | 1.4 | 243 | 1.6 | |
| Asian | 3,346 | 1.4 | 3,051 | 1.4 | 295 | 2.0 | |
| Other | 3,768 | 1.6 | 3,536 | 1.6 | 232 | 1.6 | |
| Unknown | 999 | .4 | 953 | .4 | 46 | .3 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| Medicare spending by HRR | |||||||
| Low | 42,341 | 17.8 | 39,986 | 17.9 | 2,355 | 15.7 | <.0001 |
| Medium | 130,994 | 55.0 | 122,969 | 55.1 | 8,025 | 53.6 | |
| High | 64,654 | 27.2 | 60,048 | 26.9 | 4,606 | 30.7 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| Charlson Comorbidity Index | |||||||
| 0 | 22,844 | 9.6 | 22,143 | 9.9 | 701 | 4.7 | <.0001 |
| 1 | 34,926 | 14.7 | 33,173 | 14.9 | 1753 | 11.7 | |
| 2 | 44,992 | 18.9 | 42,450 | 19.0 | 2,542 | 17.0 | |
| 3 | 42,851 | 18.0 | 40,070 | 18.0 | 2,781 | 18.6 | |
| 4 | 34,789 | 14.6 | 32,396 | 14.5 | 2,393 | 16.0 | |
| ≥5 | 57,587 | 24.2 | 52,771 | 23.7 | 4,816 | 32.1 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| Dual-eligibility status | |||||||
| No | 173,981 | 73.1 | 162,916 | 73.1 | 11,065 | 73.8 | .0371 |
| Yes | 64,008 | 26.9 | 60,087 | 26.9 | 3,921 | 26.2 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
Note: Reported percentages are the proportion of sample with the listed row characteristics among the two exposure groups (“no billed advance care planning [ACP]” and “had billed ACP”).
Abbreviation: HRR, hospital referral region.
Association of Advance Care Planning with End-of-Life Outcomes
Among decedents, 21.7% died in the hospital, 48.0% were admitted to a hospital in the last 30 days, 18.5% were admitted to an ICU in the last 30 days, 16.9% received late hospice care, and 52.8% visited an ED in the last 30 days. The average expenditures in the last 30 days were $15,310.9 (±$21,059.8) (Table 2). In unadjusted bivariate analyses, compared with those with no billed ACP, beneficiaries with an ACP claim were less likely to die in the hospital (20.0% vs 21.8%), to be admitted to an ICU in the last 30 days (17.0% vs 18.6%), or have an ED visit in the last 30 days (51.5% vs 52.9%) (all P < .008).
Table 2.
Healthcare Utilization in the Last 30 Days of Life for Medicare Patients Who Died in 2017, by Advance Care Planning Status
| Total | No billed ACP | Had billed ACP | |||||
|---|---|---|---|---|---|---|---|
| Outcomes | N | % | N | % | N | % | P value |
| Location of death | |||||||
| Not in hospital | 186,346 | 78.3 | 174,351 | 78.2 | 11,995 | 80.0 | <.001 |
| In hospital | 51,643 | 21.7 | 48,652 | 21.8 | 2,991 | 20.0 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| Admission in the last 30 d | |||||||
| No | 123,761 | 52.0 | 115,894 | 52.0 | 7,867 | 52.5 | .212 |
| Yes | 114,228 | 48.0 | 107,109 | 48.0 | 7,119 | 47.5 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| ICU visit in last 30 d | |||||||
| No | 193,897 | 81.5 | 181,463 | 81.4 | 12,434 | 83.0 | <.0001 |
| Yes | 44,092 | 18.5 | 41,540 | 18.6 | 2,552 | 17.0 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| Timely hospice care | |||||||
| ≥4 d before death | 197,667 | 83.1 | 185,337 | 83.1 | 12,330 | 82.3 | .0085 |
| <4 d before death | 40,322 | 16.9 | 37,666 | 16.9 | 2,656 | 17.7 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
| EOL healthcare expenditures a | |||||||
| Mean, SD | $15,310.92 ($21,059.78) | $200,890 | $15,233.87 ($21,116.92) | $14,131 | 16,406.32 ($20,198.97) | <.001 | |
| ED visit in last 30 d | |||||||
| No | 112,351 | 47.2 | 105,080 | 47.1 | 7,271 | 48.5 | .0009 |
| Yes | 125,638 | 52.8 | 117,923 | 52.9 | 7,715 | 51.5 | |
| Total | 237,989 | 100.0 | 223,003 | 100.0 | 14,986 | 100.0 | |
Abbreviations: ACP, advance care planning; ED, emergency department; EOL, end of life; ICU, intensive care unit; SD, standard deviation.
EOL expenditures in the last month of life from all settings including ambulatory, inpatient, skilled nursing, and hospice settings but not Part D drug expenditures.
After adjusting for confounders, beneficiaries who received a billed ACP were significantly less likely to die in the hospital (odds ratio [OR] = .79; 95% confidence interval [CI] = .76–.82; P < .0001), to be admitted to a hospital in the last 30 days (OR = .77; 95% CI = .74–79; P < .0001), to visit an ICU in the last 30 days (OR = .78; 95% CI = .74–.81; P < .0001), or to have visited an ED in the last 30 days (OR = .77; 95% CI = .75–.80; P < .0001). Late hospice care (OR = .97; 95% CI = .92–1.01; P = .119) was not significantly associated with a billed ACP (Figure 1 and Supplementary Tables 1–7 show the complete results of multivariable models).
Figure 1.
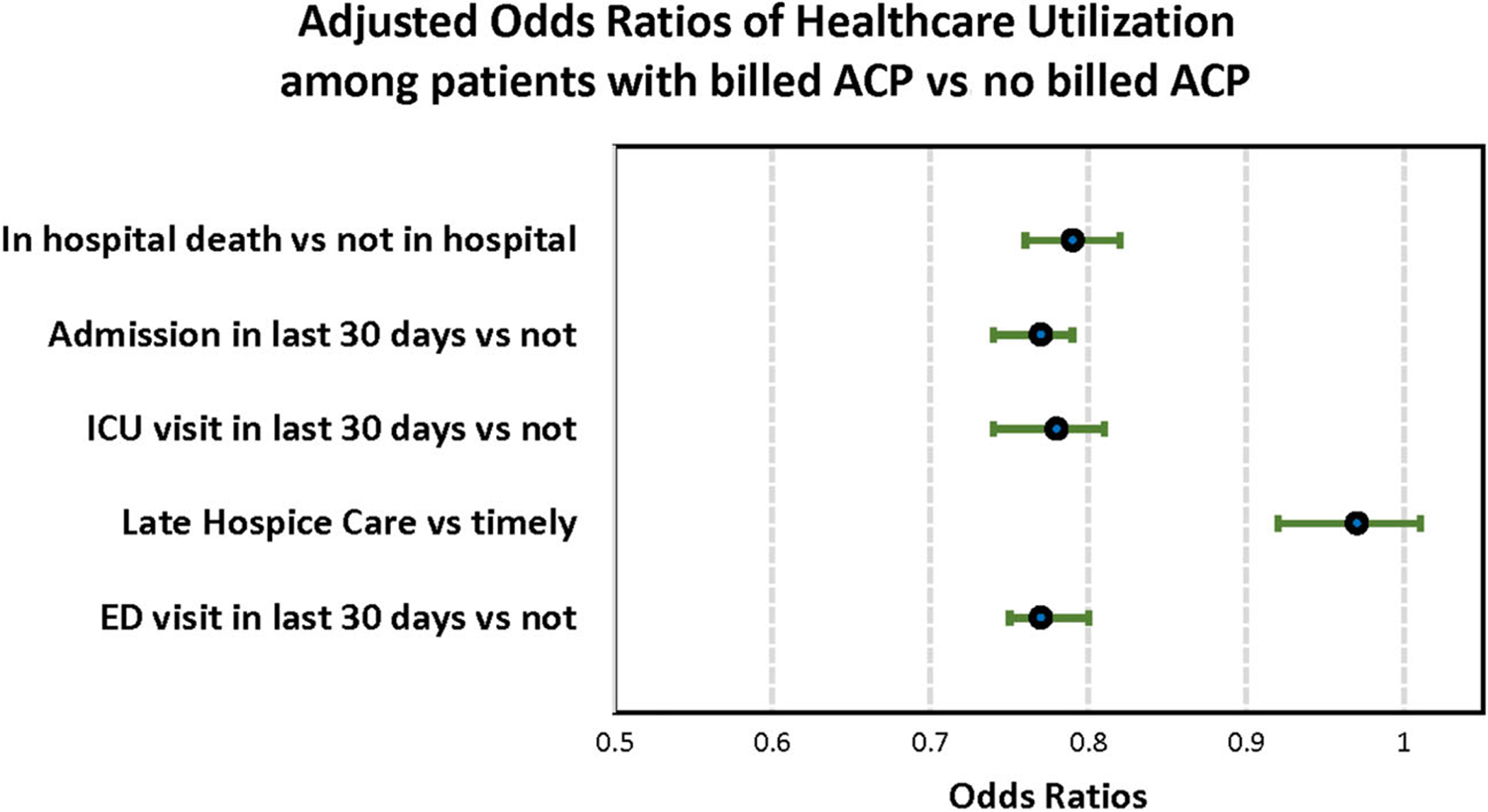
Adjusted odds ratios of healthcare utilization in the last 30 days of life for Medicare patients who died in 2017 with a billed advanced care planning (ACP) status. ED, emergency department; ICU, intensive care unit.
For expenditures, in unadjusted analyses, decedents with an ACP claim had higher EOL expenditures in the last 30 days ($16,406.3 vs $15,233.8; P < .0001) (Table 2). However, subcategories of EOL expenditures behaved differently. Hospice and SNF expenditures were much higher among beneficiaries who had billed ACP as compared with the “no billed ACP” group. Mean per person hospice expenditures were $340.41 higher among billed ACP versus not billed patients ($1,816.80 [±$2,294.76] vs $1,456.39 [±$2,079.53]), and mean per person SNF expenditures were $150.98 higher ($870.74 [±$2,552.93] vs $719.76 [±$2,671.57]). Inpatient and outpatient expenditures were higher for beneficiaries who did not have a billed ACP. Mean per person expenditures for inpatient setting were $7,417.41 (±$13,289.69) among those with billed ACP and $7,994.08 (±$14,499.95) among those without billed ACP (P < .0001). Mean expenditures for the outpatient setting were $405.97 (±$1,282.11) among those with billed ACP and $511.11 (±$1,504.14) among those without billed ACP (P < .0001) (results not shown in table). After adjusting for the potential confounders, the total mean expenditures ($242.50; 95% CI = −103.63 to 588.61; P = .169) were not significantly different among those who were billed versus not billed for ACP. However, among the subcategories of expenditures, those who had ACP had higher hospice expenditures as compared with the “no ACP group” (311.17; 95% CI = $262.70–$359.65; P < .0001). The inpatient (−934.46; 95% CI = −1,252.60 to −616.32; P < .0001) and outpatient expenditures (−123.75, 95% CI = −157.64 to −89.85; P < .0001) were significantly less among individuals who had ACP as compared with those who did not have ACP (results not shown in the table).
DISCUSSION
In a nationally representative sample of Medicare decedents, we found that a billed ACP conversation was associated with less intensive healthcare utilization in the last 30 days of life for four of six common EOL measures: dying in the hospital, hospital admission, ICU admission, and ED visit. Although we did not find a significant association of billed ACP with overall expenditures in the last 30 days of life and with the likelihood of late hospice care, we found an evidence of cost shifting from inpatient and outpatient to hospice. The National Quality Forum has endorsed ICU visits, ED visits, hospital admission, death in acute care setting, hospice enrollment, and timely hospice enrollment as EOL care standards.17 A strength of our study was its use of an objective/standardized measure of ACP (billing codes) on a national sample of Medicare beneficiaries. Although these findings confirm previous studies that have captured ACP by different means,1,5,6,8 they also raise new questions about ACP billing, EOL expenditures, and hospice care, as discussed later. Also, ACP billing codes were introduced only recently, and consistent with the previous literature, they have experienced low uptake.13,14 Therefore, the findings of this article may represent actions resulting from early adopters of these codes.
Care practices during the EOL period is a significant concern in U.S. healthcare policy. Bereaved family members report care inconsistent with the decedent’s preferences.15 The initiative of the CMS to reimburse providers for having ACP discussions is an effort to incentivize awareness of these preferences.23 The default practice of aggressive care is not associated with an improved quality of life.20 Instead, there is a preference for spending the final days at home as opposed to in a hospital or nursing home, as well as for palliative medications and comfort care, as opposed to life-prolonging medications and a ventilator for short extensions of life.5,19
One of the EOL quality indicators that was not associated with billed ACP in our study was timely hospice referral, defined as hospice care more than 3 days before death. Because a preference for “comfort care” is associated with a lower likelihood of hospice stay of 3 days or less,5 our findings could be a result of actual differences in stated preferences. Our findings could also be a result of the exclusion of billed ACP visits within the last 30 days of life that may have excluded visits leading to timely hospice care. A study based on patient or proxy interviews among cancer patients found a lower likelihood of hospice stay of less than a week among patients who received EOL discussions.6 However, the prevalence of EOL discussions in their sample was much higher (ranging from 61.5% to 16.2%)6 than our sample. Others found a lower likelihood of hospice stay of 3 days or less among those whose proxies reported an AD, DPOA, or a discussion with the next of kin for the decedent.
It is difficult to compare our results with these studies because of the difference of more than a decade in the data analyzed. It is possible that the awareness for and the availability of hospice care have changed since then. Another reason making it difficult to compare results is that our study examined billed ACP visits versus proxy interviews in the referenced study. In a more recent study examining the association between ACP billing codes and discharge status for Medicare inpatients from a large national physician practice, it was found that mandatory education in the use of ACP billing codes and physician priming to think about the risk of dying for all patients in the next year at the time of admission increased the rate of billed ACP, and the group with a billed ACP visit was significantly more likely to be discharged to hospice.24 Our study was based on a national sample and not restricted to in-patient ACP, which might have diluted the likelihood of hospice referral. The timeliness of hospice enrollment is as important as the efforts to increase the number of individuals who access hospice because without timely hospice use, we will miss “opportunities to leverage the benefits of hospice care in mitigating high end-of-life care intensity.”20
In addition to care practices, spending during the EOL period is another concern in U.S. health policy because the default is expensive.25 We did not find an overall significant association between billed ACP and total expenditures in the last 30 days of life. However, our analyses of the subcomponents of expenditure showed that having an ACP discussion significantly reduced the inpatient and outpatient expenditures, and the simultaneous increase in hospice expenditures following ACP might have balanced the overall expenditures to produce a null effect. This implies that cost shifting might be in play as a result of ACP discussions. Although it is also possible that SNF expenditures could increase as a result of ACP discussion, our analyses did not find a significant increase in SNF expenditures. Our results are aligned with previous studies that found no association between ADs and healthcare expenditures in the EOL period.26–32 Regardless of these associations, it is important to note that the “primary purpose of ADs is to convey patient preferences and instructions to guide future care during a period of mental incapacity, not to save scarce societal resources.”28,29 Irrespective of the impact on the overall healthcare costs, the impact on patients’ health and well-being is an important measure of the effectiveness of EOL policies.3
Our study has several limitations. First, we were not able to assess if the EOL outcomes were concordant with the discussed goals of care for the patients. Although the use of billed ACP standardizes the measurement of ACP as compared with the previous studies that used interviews, billed ACP might be a poor proxy of actual ACP practice.14 The use of billed ACP can vary with hospital policies and physician awareness/training on the use of codes. Therefore, it is likely that our measure of exposure underestimated the extent of ACP in real practice. It is possible that the beneficiaries who did have an ACP discussion but were not billed for ACP have different outcomes than those who were billed for their ACP discussions.
Second, we were not able to account for the quality or the content of ACP discussions. For example, ACP discussions could include a preference for a treatment-limiting versus all-care directive, that is, a preference for either limiting the type of care provided or a preference for requesting all care during the EOL period.9 Such preferences could have had a different influence on our EOL care intensity outcomes.
Third, our study could be subject to decedent-analysis bias.33 Our inclusion of decedents precludes a population-level conclusion about ACP by selecting beneficiaries who died and ascertaining a look-back period for outcome measurement. However, this bias is likely to affect our results minimally because the use of ACP billing code is not tied to any diagnosis of illness, and all Medicare beneficiaries are expected to have these conversations. Irrespective of the reason for death, the results show the differences in EOL care outcomes between those who were billed and not billed for ACP. Inclusion of decedents hence offered the best possible risk adjustment in our sample.
Fourth, by excluding beneficiaries who received a billed ACP in the last 30 days before death, our findings did not capture the impact of in-the-moment discussions on the EOL care decisions. These in-the-moment first ACP discussions could also be a result of the critically ill stage of the beneficiaries that, if included in the analyses, could have confounded the associations with the EOL outcomes. Fifth, the possibility of residual confounding due to factors such as education level and social support cannot be negated. Sixth, although our study could not analyze data on non-FFS Medicare beneficiaries, we would hypothesize that non-FFS delivery modes would prioritize value over services, and hence non-FFS Medicare beneficiaries might be more likely to have ACP conversations and a more value-based care plan. Finally, as with any administrative data set, the findings are subject to the accuracy of the claims data.
In conclusion, this is the first study to examine the association of billed ACP visits with healthcare utilization at EOL for Medicare beneficiaries. Given the low uptake in the first few years, it is possible that the positive results we found for four of six measures may be due to behaviors by early adopters. Future studies to examine the factors associated with the timeliness of hospice referral will be important to understand how ACP discussions could be structured to inform decisions for hospice referral. In addition, future studies should explore the impact of billed ACP on the specific components of EOL care expenses, to help manage the high total EOL care costs.
Supplementary Material
Supplementary Table S1: Association Between Billed ACP and Location of Death.
Supplementary Table S2: Association Between Billed ACP and Hospital Admission in Last 30 Days.
Supplementary Table S3: Association Between Billed ACP and ICU Visit in Last 30 Days.
Supplementary Table S4: Association Between Billed ACP and Late Hospice Use.
Supplementary Table S5: Association Between Billed ACP and Expenditures in Last 30 Days.
Supplementary Table S6: Association Between Billed ACP and ED Use in Last 30 Days.
Supplementary Table S7: Adjusted Associations Between ACP and Expenditures by Setting and HRR Regions.
ACKNOWLEDGMENTS
We would like to sincerely thank Stephen Perez, Daniel Sturgeon, and Jill Swan for their assistance and contributions at several phases of the manuscript.
Financial Disclosures:
This study was funded by the National Institutes of Nursing Research (RO1 No. NR017034).
Sponsor’s Role:
The sponsor had no role in the design, methods, subject recruitment, data collections, analysis, and preparation of the article.
Footnotes
Conflict of Interest: The authors have declared no conflicts of interest for this article.
Previous presentations: Poster related to this article was presented at AcademyHealth Annual Research Meeting 2019, Washington, DC.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
REFERENCES
- 1.Silveira MJ, Kim SYH, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13): 1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.OʼHanlon CE, Walling AM, Okeke E, Stevenson S, Wenger NS. A framework to guide economic analysis of advance care planning. J Palliat Med. 2018;21:1480–1485. [DOI] [PubMed] [Google Scholar]
- 3.Gawande A. Quantity and quality of life: duties of care in life-limiting illness. JAMA. 2016;315:267–269. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services. Medicare Learning Network. Advance Care Planning - Fact Sheet. Advance Care Planning https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/advancecareplanning.pdf. Accessed July 20, 2019. [Google Scholar]
- 5.Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc. 2013;61(2):209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prater L, Wickizer T, Bose-Brill S. The documentation of advance care planning in the EHR and quality outcomes for older adults nearing the end of life. Innov Aging. 2018;2(suppl 1):1018. [Google Scholar]
- 8.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc. 2007;55:189–194. [DOI] [PubMed] [Google Scholar]
- 9.Nicholas LH, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA. 2011;306(13):1447–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higel T, Alaoui A, Bouton C, Fournier J. Effect of living wills on end-of-life care: a systematic review. J Am Geriatr Soc. 2019;67(1):164–171. [DOI] [PubMed] [Google Scholar]
- 11.David D, McMahan RD, Sudore RL. Living wills: one part of the advance care planning puzzle. J Am Geriatr Soc. 2019;67(1):9–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehta A, Kelley AS. Advance care planning codes—getting paid for quality care. JAMA Intern Med. 2019;179:830–831. [DOI] [PubMed] [Google Scholar]
- 13.Pelland K, Morphis B, Harris D, Gardner R. Assessment of first-year use of Medicareʼs advance care planning billing codes. JAMA Intern Med. 2019; 179(6):827–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belanger E, Loomer L, Teno JM, Mitchell SL, Adhikari D, Gozalo PL. Early utilization patterns of the new Medicare procedure codes for advance care planning. JAMA Intern Med. 2019;179:829–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teno JM, Gozalo P, Trivedi AN, et al. Site of death, place of care, and health care transitions among US medicare beneficiaries, 2000–2015. JAMA. 2018; 320:264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sudore RL, Heyland DK, Lum HD, et al. Outcomes that define successful advance care planning: a Delphi panel consensus. J Pain Symptom Manage. 2018;55:245–255. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Quality Forum. National Voluntary Consensus Standards for Palliative Care and End-of-Life Care. 2012. https://www.qualityforum.org/Projects/Palliative_Care_and_End-of-Life_Care.aspx#t=1&s=&p=. Accessed May 13, 2019.
- 18.Mack JW, Weeks JC, Wright AA, Block SD, Prigerson HG. End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol. 2010; 28(7):1203–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences?: a study of the US Medicare population. Med Care. 2007;45(5):386–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang S-Y, Aldridge MD, Gross CP, et al. End-of-life care intensity and hospice use. Med Care. 2016;54(7):672–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dartmouth Atlas Project. The Dartmouth Atlas of Healthcare https://www.dartmouthatlas.org/.Accessed May 10, 2019.
- 22.Bland JM, Altman DG. Statistics notes: multiple significance tests: the Bonferroni method. BMJ. 1995;310(6973):170–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Emanuel EJ. The status of end-of-life care in the United States: the glass is half full. JAMA. 2018;320(3):239–241. [DOI] [PubMed] [Google Scholar]
- 24.Barnato AE, OʼMalley AJ, Skinner JS, et al. Use of advance care planning billing codes for hospitalized older adults at high risk of dying: a national observational study. J Hosp Med. 2019;14(4):229–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luta X, Maessen M, Egger M, Stuck AE, Goodman D, Clough-Gorr KM. Measuring intensity of end of life care: a systematic review. PLOS One. 2015;10:e0123764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fonk J, Davidoff D, Lutzow T, Chesley N, Mathiowetz N. The effect of advance directives on end-of-life cost experience. J Health Care Poor Under-served. 2012;23:1137–1156. [DOI] [PubMed] [Google Scholar]
- 27.Schneiderman LJ, Kronick R, Kaplan RM, Anderson JP, Langer RD. Effects of offering advance directives on medical treatments and costs. Ann Intern Med. 1992;117:599–606. [DOI] [PubMed] [Google Scholar]
- 28.Kaambwa B, Ratcliffe J, Bradley SL, et al. Costs and advance directives at the end of life: a case of the “coaching older adults and carers to have their preferences heard (COACH)” trial. BMC Health Serv Res. 2015;15:545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Teno J, Lynn J, Connors AF, et al. The illusion of end-of-life resource savings with advance directives. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. J Am Geriatr Soc. 1997;45(4):513–518. [DOI] [PubMed] [Google Scholar]
- 30.Tan TS, Jatoi A. End-of-life hospital costs in cancer patients: do advance directives or routes of hospital admission make a difference? Oncology. 2011;80:118–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garrido MM, Balboni TA, Maciejewski PK, Bao Y, Prigerson HG. Quality of life and cost of care at the end of life: the role of advance directives. J Pain Symptom Manage. 2015;49:828–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154(4):235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bach PB, Schrag D, Begg CB. Resurrecting treatment histories of dead patients: a study design that should be laid to rest. JAMA. 2004;292: 2765–2770. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Association Between Billed ACP and Location of Death.
Supplementary Table S2: Association Between Billed ACP and Hospital Admission in Last 30 Days.
Supplementary Table S3: Association Between Billed ACP and ICU Visit in Last 30 Days.
Supplementary Table S4: Association Between Billed ACP and Late Hospice Use.
Supplementary Table S5: Association Between Billed ACP and Expenditures in Last 30 Days.
Supplementary Table S6: Association Between Billed ACP and ED Use in Last 30 Days.
Supplementary Table S7: Adjusted Associations Between ACP and Expenditures by Setting and HRR Regions.


