ABSTRACT
Background: Coronavirus disease-2019 (COVID-19) pandemic has shown unpredictable course in individual patients. Few patients develop severe disease with progression after admission to a healthcare facility. Multiple parameters have been investigated to identify a marker to predict disease progression. Neutrophil-to-lymphocyte ratio (NLR) or platelet-to-lymphocyte (PLR) ratio has shown some promise. The current investigation explores the role of NLR and PLR to predict the disease progression.
Materials and methods: After obtaining ethics committee approval, 608 patients were screened for inclusion in the prospective observational study, and 201 patients were included in the final analysis. The NLR and PLR were derived from routinely obtained complete blood count analysis. The patients were followed to determine the development of severity of the disease during the course. The NLR and PLR were analyzed in both univariate and multivariable models to assess the association and prediction.
Results: In nonsevere (NS) group, the mean age of patients was 50.9 ± 16.3 years, and 66 (61.2%) were male, while in severe group (S), the mean age of patients was 53.7 ± 16.4 years, and 65 (69.89%) were male. NLR at day 1 and day 3 was significantly lower in survivors as compared to nonsurvivors, while the relation of PLR in both the groups was not statistically significant. The NLR is better in predicting the severity of disease as well as mortality than PLR.
Conclusion: The NLR calculated at the time of admission has high predictive value for disease deterioration and adverse clinical outcome.
How to cite this article: Singh Y, Singh A, Rudravaram S, Soni KD, Aggarwal R, Patel N, et al. Neutrophil-to-lymphocyte Ratio and Platelet-to-lymphocyte Ratio as Markers for Predicting the Severity in COVID-19 Patients: A Prospective Observational Study. Indian J Crit Care Med 2021;25(8):847–852.
Keywords: COVID-19 mortality, COVID-19, COVID-19 infection, Mortality, Mortality prediction
INTRODUCTION
Coronavirus disease-2019 (COVID-19) has been declared as pandemic by the World Health Organization,1 and it has infected over 79 million people worldwide with more than 1.7 million deaths.1,2 COVID-19 has shown a varied spectrum of presentation ranging from asymptomatic to severe illness requiring intensive care.3,4 While most of the infected are either asymptomatic or presented with mild symptoms like fever and dry cough, >14% developed severe disease with dyspnea, tachypnea, and desaturation requiring hospitalization and oxygen supplementation.5 Older age, male sex, heart failure, and obesity are some of the discernible risk factors associated with severe illness.6 High viral load and over exuberant host immune response manifesting as cytokine storm contribute to pathogenesis of multiple organ dysfunction, including acute respiratory distress syndrome, coagulation dysfunction, acute cardiac injury, and renal injury.7,8
Early clinical diagnosis and treatment of COVID-19 may help in decreasing the severity, mortality of patients as well as controlling the spread of the virus. Despite all the measures, diagnosing the COVID-19 patients early and predicting the patient’s severity and mortality remain challenging. Many techniques like hemogram and biochemical analysis that can be used to facilitate the diagnosis and prognosis of COVID-19 early are being used. Certain markers derived from the peripheral blood such as white blood cell count (WBC count), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and even certain biochemical markers like CRP and LDH have been used independently for predicting the prognosis in systemic inflammatory conditions. 15,16,17
Both NLR and PLR are the well-established inflammatory markers in systemic inflammatory conditions.9,10 Few studies until recently had shown that elevated NLR can be predictors for severity and poor outcome in COVID-19 patients.11–14 Timely identification of these markers plays a pivotal role in the management and thus the outcome of the disease. Though there is an exhausting list of predictors of severe COVID-19 illness, the simplicity and cost-effectiveness of the NLR and PLR markers are more suitable to low-resource establishment and third world countries. Here in this study, we evaluated the role of NLR and PLR in the peripheral blood to predict the severity in COVID-19 patients and overall mortality.
MATERIALS AND METHODS
This prospective, single-center, observational study was conducted after obtaining the approval from Institutional Ethics Committee, AIIMS, New Delhi (Approval No-IEC-555/19.06.2020, CTRI/2020/07/026574).
A total of 608 laboratory-confirmed COVID-19 patients admitted to JPNATC, from June 15, 2020, to October 30, 2020, were included in the study. The participants were diagnosed COVID-19 positive on the basis of the RT-PCR report. The enrolled patients were examined by the doctors at the time of admission and were divided into two groups based on the severity of illness: Group NS (nonsevere) and Group S (severe), and shifted accordingly in the ward and ICU, respectively.
Group NS: Patients having fever, mild respiratory symptoms, typical X-ray/CT showing image abnormalities of viral pneumonia.
Group S: Patients with any one of the following features (a) Shortness of breath, RR>30/minute and (b) oxygen saturation in the resting state <93% with PaO2/FiO2 ≤300 mm Hg were considered.
Patients with age less than 6 years, pregnancy, dialysis dependent, known malignancy, and psychiatric illness were excluded from the study.
After obtaining informed consent, the clinical symptoms, signs, comorbidities, laboratory investigations, and treatment received were collected from hospital’s electronic medical records. After the participant was enrolled in the study, he/she was followed till discharge or death. If required, follow-up on telephone consultation was done after the discharge. One researcher recorded the demographic data, clinical symptoms/signs, and comorbidities, and the other researcher recorded laboratory data and followed up the patients. The complete blood count was noted on the first and the third day of the admission. NLR and PLR were derived in accordance with the CBC results. NLR was calculated as the ratio of the absolute neutrophil count to the absolute lymphocyte count, and PLR as the ratio of the platelet count to the absolute lymphocyte count.
Statistical Analysis
All the statistical analyses were carried out using R software, and two-sided p <0.05 was considered significant. Continuous data are reported as mean ± SD, median and interquartile range (IQR) as applicable, while categorical data are expressed as frequency and percentage. Shapiro–Wilk test was performed for the normality of the sample data. An independent-sample t-test was used for univariate analysis, while Student’s t-test for parametric data and Mann–Whitney U-test for nonparametric were applied to compare the independent groups. Multivariable analysis was done, and odd ratio was calculated. The logistic regression models were performed to identify the factors affecting the severity in COVID-19 patients. The ROC analysis was performed to predict the severity of COVID-19.
RESULTS
A total of 608 patients with COVID-19 confirmed with RT-PCR were screened for possible inclusion in the study. Three hundred and fifty-eight patients satisfied the inclusion criteria. Further, 157 patients were excluded from the study due to the lack of laboratory and clinical data and trauma patients. The study finally included 201 patients who were categorized into severe and nonsevere based on their initial clinical presentation at the time of admission. The NS group had 108 patients, while S group had 93 patients (Flowchart 1).
Flowchart 1.
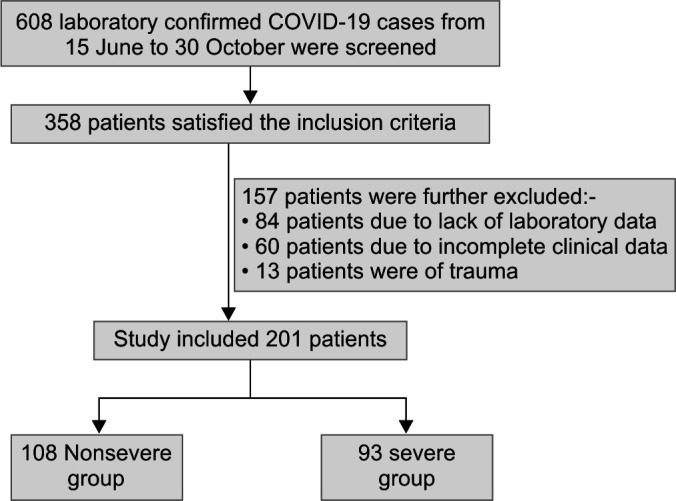
Inclusion and exclusion criteria (flow diagram)
Baseline Demographics
In NS group, the mean age of patients was 50.9 ± 16.3 years, and 66 (61.2%) were male and 42 (38.8%) were female, while in S group, the mean age of patient was 53.7 ± 16.4 years, and 65 (69.89%) were male and 28 (30.10%) were female. The most common comorbidities in both groups were diabetes and hypertension. There was no significant difference in age, sex, or comorbidities in both the groups except for CVA, which was significantly higher in S group (Table 1).
Table 1.
Demographics and clinical characteristics of patients diagnosed with COVID-19
| Characteristics | Nonsevere (n = 108) | Severe (n = 93) | p value |
|---|---|---|---|
| Age (years) | 50.9 ± 16.3 | 53.7 ± 16.4 | 0.23 |
| Male | 66 | 65 | 0.19 |
| Female | 42 | 28 | |
| Comorbidity (%) | |||
| Diabetes | 41.66 | 43 | 0.84 |
| Hypertension | 41.66 | 35.48 | 0.37 |
| CAD | 10.01 | 10.75 | |
| COPD | 2.77 | 2.15 | 0.77 |
| ASTHMA | 4.85 | 3.22 | 0.61 |
| CLD | 10.01 | 6.45 | 0.343 |
| CKD | 14.81 | 15.5 | 0.96 |
| CVA | 4.62 | 12.90 | 0.03 |
| Laboratory parameters (median, IQR) | |||
| Hb1 (mean ± SD) | 10.9 ± 2.63 | 11.6 ± 2.28 | 0.04 |
| Hb3 (mean ± SD) | 10.6 ± 2.45 | 11.1 ± 2.28 | 0.15 |
| TLC1 | 9,765 (6,860) | 11,900 (8,100) | 0.005 |
| TLC3 | 9,400 (6,935) | 11,840 (5,450) | 0.004 |
| PL1 | 166,500 (100,500) | 167,000 (120,000) | 0.8 |
| PL3 | 190,000 (150,000) | 191,000 (116,000) | 0.29 |
| N1 | 7,955 (6,255) | 10,323 (7,658) | 0.001 |
| N3 | 7,830 (7,696) | 10,350 (5,557) | 0.01 |
| L1 | 1,312 (797) | 980 (939) | 0.001 |
| L3 | 1,235 (1,305) | 1,080 (805) | 0.01 |
| NLR 1 | 7.36 (7.37) | 10.8 (10.2) | 0.001 |
| NLR 3 | 7.73 (7.74) | 9.11 (9.90) | 0.009 |
| PLR 1 | 135 (146) | 182 (178) | 0.001 |
| PLR 3 | 167 (196) | 163 (121) | 0.239 |
| Mode of respiratory support at admission in number (n) | |||
| Initial respiratory Support (IRS) | <0.001 | ||
| Room air (RA) | 15 | 0 | |
| Face mask (FM) | 79 | 12 | |
| Nasal prongs (NP) | 6 | 1 | |
| Non-re-breathing mask (NRBM) | 8 | 16 | |
| High-flow nasal cannula (HFNC) | 0 | 16 | |
| Noninvasive ventilation (NIV) | 0 | 8 | |
| Mechanical ventilation (MV) | 0 | 40 | |
| Outcome analysis (median, IQR) | |||
| Escalation % (n) | 39.8 (43) | 81.7 (76) | 0.001 |
| ICU stay (days) | 5 (8) | 12 (11) | 0.001 |
| Hospital stay (days) | 13 (9) | 14 (12) | 0.3 |
| Mortality % (n) | 25.9 (28) | 67.7 (63) | 0.001 |
CAD, coronary artery diseases; COPD, chronic obstructive pulmonary diseases; CLD, chronic liver disease; CKD, chronic kidney disease; CVA, cerebrovascular accident; Hb 1 and Hb 3, hemoglobin at first and third day of admission; TLC1 and TLC3, total leukocyte count at first and third day of admission; PL1 and PL3, platelet at first and third day of admission, N1 and N3, absolute neutrophil count at first and third day of admission; L1 and L3, absolute lymphocyte count at first and third day of admission; NLR 1 and NLR 3, neutrophil-to-lymphocyte ratio at first and third day of admission; PLR 1and PLR 3, platelet-to-lymphocyte ratio at first and third day of admission; IRS, initial respiratory support; RA, room air; FM, face mask; NP, nasal prongs; NRBM, non-re-breathing mask; HFNC, high-flow nasal cannula; NIV, noninvasive ventilation; MV, mechanical ventilation; Escalation, increase in respiratory support and oxygen requirement. p value <0.05 considered statistically significant
Mode of Respiratory Support at Time of Admission
In NS group, out of 108 patients, 79 patients received oxygen via face mask (FM), 8 via non-re-breathing mask (NRBM), 6 via nasal prongs (NP), and 14 maintained saturation on room air (RA). In S group, out of 93 patients, 40 patients were mechanically ventilated, 16 patients via high-flow nasal cannula (HFNC) and NRBM each, 8 were given noninvasive ventilation (NIV), 12 was on FM, and one was on NP. The table shows that NS patients had lower oxygen requirements, and most of the patients maintained oxygen saturation with oxygen therapy via FM, while in S group, most of the patients required mechanical ventilation and higher form of oxygen therapy via HFNC, NRBM, and NIV (Tables 1 and 2).
Table 2.
Factors associated with severity of COVID-19 disease
| Factors | Odd ratio (95% CI) | p value |
|---|---|---|
| Multivariable analysis | ||
| Age (years) | 1 (0.96–1.03) | 0.896 |
| Comorbidity | 2.16 (0.39–11.86) | 0.375 |
| Hb1 | 1.21 (0.96–1.53) | 0.095 |
| TlC1 | 1 (0.99–1) | 0.82 |
| NLR1 | 1.05 (0.96–1.14) | 0.23 |
| PLR1 | 0.99 (1–1) | 0.45 |
| Escalation | 4.34 (1.45–12.96) | 0.008 |
| Initial respiratory support | ||
| HFNC-FM | 8.49 (0.0–∞) | 0.98 |
| MV-FM | 233.27 (26.69–2038.16) | 0.001 |
| NRBM-FM | 13.12 (3.65–47.13) | 0.001 |
| NIV-FM | 4.10 (0.0–∞) | 0.99 |
| NP-FM | 0.99 (0.09–11.04) | 0.99 |
| RA-FM | 0.77 (0.08–7.290) | 0.82 |
Hb 1, hemoglobin at first day of admission; TLC1, total leukocyte count at first day of admission; NLR 1, neutrophil-to-lymphocyte ratio at first day of admission; PLR 1, platelet-to-lymphocyte ratio at first day of admission; RA, room air; FM, face mask; NP, nasal prongs; NRBM, non-re-breathing mask; HFNC, high-flow nasal cannula; NIV, noninvasive ventilation; MV, mechanical ventilation; Escalation, increase in respiratory support and oxygen requirement. p value <0.05 considered statistically significant
Laboratory Parameters
The laboratory test showed that the total leucocyte count and neutrophil count were significantly higher, while the lymphocyte count was significantly lower in S group as compared to NS group. The NLR and PLR were significantly higher in the S group as compared to NS group at the time of admission (Table 1).
Outcome Measures
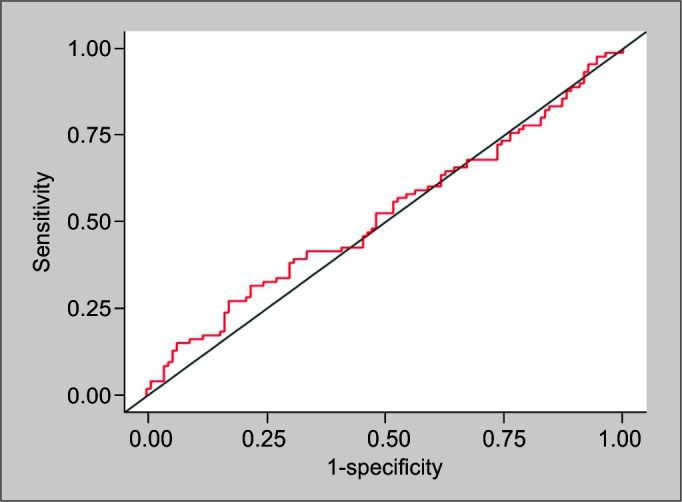
Forty-three patients in NS group and 76 patients in S group had a significant escalation of disease. The median ICU stay was significantly lower in NS group than in S group, but the total hospital stay in both the groups was not significant. The mortality rate was significantly lower in NS group (Table 1). Analysis of NLR and PLR in survivors and death showed that NLR at day 1 and day 3 was significantly lower in survivors as compared to nonsurvivors, while the relation of PLR in both the groups was not statistically significant (Table 4, Figs 4 and 5). The NLR is better in predicting the severity of disease as well as mortality than PLR (Table 3). In univariate analysis, NLR1 has an AUC of 0.6 (Fig. 1) with the sensitivity and specificity of 60 and 55%, respectively. On the other hand, PLR1 has AUC OF 0.52 (Fig. 2) with the sensitivity and specificity of 51% (Table 3).The model comprising factors such as age, comorbidities, Hb, TLC, NLR 1, PLR 1, escalation, and initial respiratory support (IRS) showed the sensitivity of 88%, specificity of 87% and AUC of 0.94 for predicting the severity of COVID-19 at the time of admission (Fig. 3).
Table 4.
Overall NLR and PLR in survivors and nonsurvivors (mean ± SD)
| Parameters | Survivor (n = 110) | Nonsurvivors (n = 91) | p value |
|---|---|---|---|
| NLR 1 | 9.72 ± 7.83 | 13.15 ± 12.28 | 0.01 |
| NLR 3 | 8.68 ± 7.22 | 11.67 ± 7.50 | 0.0003 |
| PLR 1 | 192.72 ± 141.75 | 220.15 ± 178.66 | 0.57 |
| PLR 3 | 212.27 ± 172.13 | 183.43 ± 128.08 | 0.54 |
NLR 1 and NLR 3, neutrophil-to-lymphocyte ratio at first and third day of admission; PLR 1 and PLR 3, platelet-to-lymphocyte ratio at first and third day of admission; p value <0.05 considered significant
Fig. 4.
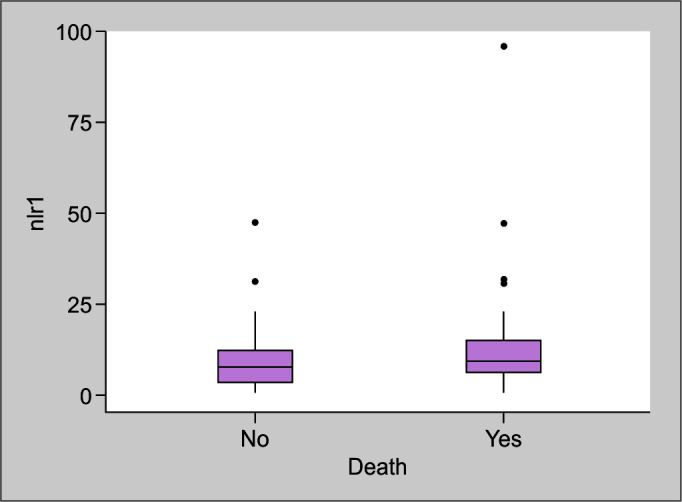
Comparison of neutrophil to lymphocyte ratio at first day of admission in survivor and non-survivor (NLR1)
Fig. 5.
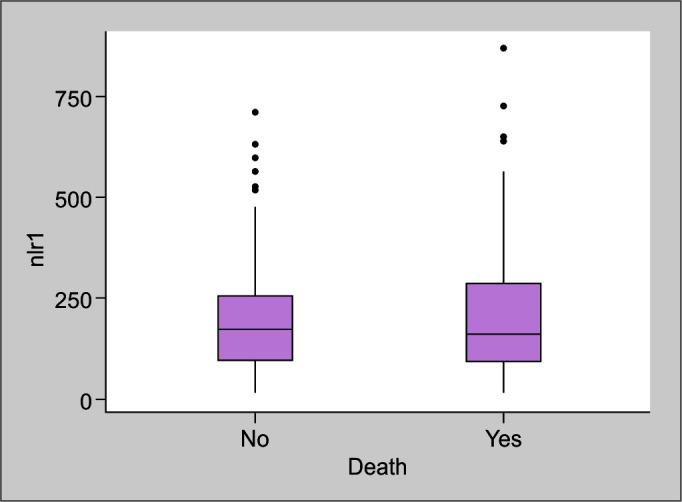
Comparison of platelet to lymphocyte ratio at first day of admission in survivor and non-survivor (PLR1)
Table 3.
Receiver-operating curve analysis of NLR 1 and PLR1
| AUC (95% CI) | Cutoff value | Sensitivity | Specificity | p value | |
|---|---|---|---|---|---|
| NLR1 | 0.60 | 0.43 | 0.60 | 0.55 | 0.001 |
| PLR1 | 0.52 | 0.44 | 0.51 | 0.51 | 0.001 |
NLR 1, neutrophil-to-lymphocyte ratio at first day of admission; PLR 1, platelet-to-lymphocyte ratio at first day of admission; p value <0.05 considered significant
Fig. 1.
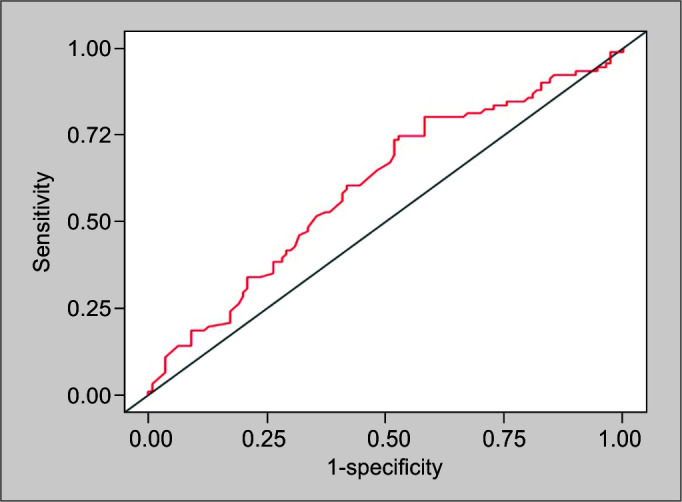
Receiver operating characteristics curve of neutrophil to lymphocyte ratio on first day of admission (NLR1) (cut off value-0.43)
Fig. 2.
Receiver operating characteristics curve of platelet to lymphocyte ratio on first day of admission (PLR1) (cut off value-0.44)
Fig. 3.
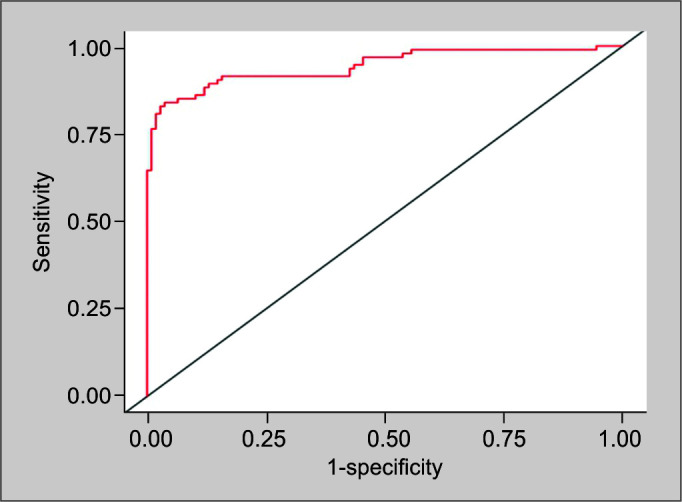
Receiver operating characteristics curve of model including multiple variables (cut off value 0.3)
DISCUSSION
In this study, we have evaluated the role of NLR and PLR at admission in predicting the severity and mortality in COVID-19 patients. Our study has showed that higher NLR and PLR values at the time of admission were associated with an increased risk of severe disease, while increased NLR significantly showed higher mortality in COVID-19 patients. This study shows that this simple and easily available parameter can be used to predict the course of disease and prognosis in COVID-19 patients. Patient in S group has 4.34 times higher risk of escalation of disease and mortality as compared to patients in NS group. The above clinical manifestation can be explained as COVID-19 patients suffering from severe disease present with leukocytosis, thrombocytopenia, lymphopenia, and neutrophilia than with the patients suffering from nonsevere disease.18 These patients have a higher likelihood of developing ARDS requiring ICU admission and mechanical ventilation.19–20 Various mechanisms of lymphopenia in COVID-19 patients have been associated with the ability of COVID-19 virus to infect T lymphocytes through angiotensin-converting enzyme 2 (ACE2) receptors and cluster differentiation (CD) 147-spike proteins.21,22 The final outcomes are the reduced levels of CD4+, CD8+ T lymphocytes and raised levels of regulatory T cells. Increased levels of proinflammatory cytokines along with T-cell lymphopenia result in severe cytokine storm, leading to even greater lymphocytic apoptosis and multi-organ dysfunction. This manifests as an increase in NLR or PLR, which correlates with disease severity.23–25
Liu et al. in their study have found that NLR was an independent risk factor for the in-hospital mortality and proper assessment of NLR of COVID-19 patients will help to identify high-risk individual.25 Li et al. in their meta-analysis regarding the predictive value of NLR on disease severity and mortality in COVID-19 patients have concluded that NLR can help the clinicians in early identification of severe cases, help in early triage and starting of proper treatment on time, which will help to reduce the overall mortality of COVID-19.26 Yang et al. showed that raised NLR and age were associated with severe COVID-19 illness and independently predicted the poor clinical outcome of COVID-19. Ciccullo et al. demonstrated that younger age and NLR below 3 were associated with clinical improvement, while NLR over 4 predicted the transfer to ICU.27 Liu et al. in their study showed that patients with more than 50 years and NLR ≥3.13 are more likely to develop critical illness.28
Various other researchers around the globe have concluded that NLR and PLR can be used to stratify COVID-19 patients and high NLR at admission has been associated with poor outcome.11,29–31 Our study prospectively validates the findings of previous studies and demonstrates that NLR can be used as a tool to predict disease deterioration and serious clinical outcomes. In further analyzing the data for the overall mortality, the NLR1 and NLR3 ratios were found to be significantly high in the patients with death than in survivors.
Our study too has various limitations. First, it was single-center study. Second, the sample size of the study was not large enough to evaluate the predictive performance of NLR on COVID-19 disease severity and mortality. Third, the effect of other treatment modalities before admission to our hospital on NLR has not been excluded. Steroids have been used in the treatment, which can cause leukocytosis, thus affecting it. Moreover, the NLR and PLR are time-sensitive variables, and values are dynamic during the course of disease. Hence, multicenter studies with large sample size are needed to evaluate predictive performance of the NLR and PLR in determining COVID-19 severity and mortality.
CONCLUSION
Our study demonstrated that NLR calculated at the time of admission has high predictive value for disease deterioration and adverse clinical outcome. It can be used for early stratification of patients; thus, patients with higher NLR can be given higher-level critical and supportive care.
Footnotes
Source of support: Nil
Conflict of interest: None
ORCID
Yudhyavir Singh https://orcid.org/0000-0002-5101-7609
Abhishek Singh https://orcid.org/0000-0002-4690-5118
Swetha Rudravaram https://orcid.org/0000-0002-6553-3102
Kapil D Soni https://orcid.org/0000-0003-1214-4119
Richa Aggarwal https://orcid.org/0000-0002-4531-2759
Nishant Patel https://orcid.org/0000-0001-9376-4963
Naveet Wig https://orcid.org/0000-0002-6603-601X
Anjan Trikha https://orcid.org/0000-0002-6001-8486
REFERENCES
- 1.World Health Organization. Director-General’s remarks at the media briefing on 2019-nCoV on 11 February 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 [Accessed on February 12, 2020].
- 2.Kuzmin IV, Bozick B, Guagliardo SA, Kunkel R, Shak JR, Tong S, et al. Bats, emerging infectious diseases, and the rabies paradigm revisited. Emerg Health Threats J. 2011;;4::1.. doi: 10.3402/ehtj.v4i0.7159.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan JF, Yuan S, Kok KH, Kai-Wang K, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;;395((10223):):514––523.. doi: 10.1016/S0140-6736(20)30154-9.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;;395((10223):):497––506.. doi: 10.1016/S0140-6736(20)30183-5.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;;323((13):):1239––1242.. doi: 10.1001/jama.2020.2648.. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;;369::m1966.. doi: 10.1136/bmj.m1966.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parasher A. COVID-19: current understanding of its pathophysiology, clinical presentation and treatment. Postgraduate Med J. 2020;;97((1147).) doi: 10.1136/postgradmedj-2020-138577.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang B, Zhou X, Zhu C, Song Y, Feng F, Qiu Y, et al. Immune phenotyping based on the neutrophil-to-lymphocyte ratio and igg level predicts disease severity and outcome for patients with COVID-19. Front Mol Biosci. 2020;;7::157.. doi: 10.3389/fmolb.2020.00157.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qin C, Zhou L, Hu Z. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020;;71((15):):762––768.. doi: 10.1093/cid/ciaa248.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meng L, Yu Z, Guo P, Wang Q, Qi R, Shan M, et al. Neutrophils and neutrophil-lymphocyte ratio: inflammatory markers associated with intimal-media thickness of atherosclerosis. Thromb Res. 2018;;170::45––52.. doi: 10.1016/j.thromres.2018.08.002.. DOI: [DOI] [PubMed] [Google Scholar]
- 11.Seyit M, Avci E, Nar R, Senol H, Yilmaz A, Ozen M, et al. Neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio and platelet to lymphocyte ratio to predict the severity of COVID-19. Am J Emerg Med. 2021;;40::110––114.. doi: 10.1016/j.ajem.2020.11.058.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;;84::106504.. doi: 10.1016/j.intimp.2020.106504.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zou X, Li S, Fang M, Hu M, Bian Y, Ling J, et al. Acute physiology and chronic health evaluation II score as a predictor of hospital mortality in patients of coronavirus disease 2019. Crit Care Med. 2020;;48((8):):e657––e665.. doi: 10.1097/CCM.0000000000004411.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liang W, Liang H, Ou L, Chen B, Chen A, Li C, et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. 2020;;180((8):):1––9.. doi: 10.1001/jamainternmed.2020.2033.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han Q, Wen X, Wang L, Han X, Shen Y, Cao J, et al. Role of hematological parameters in the diagnosis of influenza virus infection in patients with respiratory tract infection symptoms. J Clin Lab Anal. 2020;;34((5):):23191.. doi: 10.1002/jcla.23191.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shen Y, Huang X, Zhang W. Platelet-to-lymphocyte ratio as a prognostic predictor of mortality for sepsis: interaction effect with disease severity-a retrospective study. BMJ Open. 2019;;9((1):):022896.. doi: 10.1136/bmjopen-2018-022896.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JH, Song S, Yoon SY, Lim CS, Song JW, Kim HS. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as diagnostic markers for pneumonia severity. Br J Biomed Sci. 2016;;73((3):):140––142.. doi: 10.1080/09674845.2016.1209898.. DOI: [DOI] [PubMed] [Google Scholar]
- 18.Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020;;58((7):):1021––1028.. doi: 10.1515/cclm-2020-0369.. DOI: [DOI] [PubMed] [Google Scholar]
- 19.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;;180((7):):934––943.. doi: 10.1001/jamainternmed.2020.0994.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;;323((11):):1061––1069.. doi: 10.1001/jama.2020.1585.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;;579((7798):):270––273.. doi: 10.1038/s41586-020-2012-7.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang K, Chen W, Zhou Y-S, et al. SARS-CoV-2 invades host cells via a novel route: CD147-spike protein. bioRx-iv. 2020. doi: 10.1038/s41392-020-00426-x.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Wang T, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;;130((5):):2620––2629.. doi: 10.1172/JCI137244.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perdersen SF, Ho Y-C. SARS-CoV-2: a storm is raging. J Clin Invest. 2020;;130((5):):2202––2205.. doi: 10.1172/JCI137647.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Y, Du X, Chen J, Jin Y, Peng L, Wang HHX, et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020;;81((1):):e6––e12.. doi: 10.1016/j.jinf.2020.04.002.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li X, Liu C, Mao Z, Xiao M, Wang L, Qi S, et al. Predictive values of neutrophil-to-lymphocyte ratio on disease severity and mortality in COVID-19 patients: a systematic review and meta-analysis. Crit Care. 2020;;24((1):):647.. doi: 10.1186/s13054-020-03374-8.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ciccullo A, Borghetti A, Zileri Dal Verme L, Tosoni A, Lombardi F, Garcovich M, et al. Neutrophil-to-lymphocyte ratio and clinical outcome in COVID-19: a report from the Italian front line. Int J Antimicrob Agents. 2020;;56((2):):106017.. doi: 10.1016/j.ijantimicag.2020.106017.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. 2020;;18((1):):206.. doi: 10.1186/s12967-020-02374-0.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan AS, Rout A. Use of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in COVID-19. J Clin Med Res. 2020;;12((7):):448––453.. doi: 10.14740/jocmr4240.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jimeno S, Ventura PS, Castellano JM, García-Adasme SI, Miranda M, Touza P, et al. Prognostic implications of neutrophil-lymphocyte ratio in COVID-19. Eur J Clin Invest. 2021;;51((1):):13404.. doi: 10.1111/eci.13404.. DOI: [DOI] [PubMed] [Google Scholar]
- 31.Imran MM, Ahmad U, Usman U, Ali M, Shaukat A, Gul N. Neutrophil/lymphocyte ratio – a marker of COVID-19 pneumonia severity. Int J Clin Pract. 2021;;75((4):):13698.. doi: 10.1111/ijcp.13698.. DOI: [DOI] [PubMed] [Google Scholar]


