ABSTRACT
Objectives: To describe the clinical outcomes of hypoxic coronavirus disease 2019 (COVID-19) patients treated with intravenous methylene blue (MB) in a tertiary care hospital.
Materials and methods: We conducted a case series of 50 patients with hypoxic COVID-19 treated with intravenous MB admitted to our hospital between June 01 and September 10, 2020. Intravenous MB was administered as rescue therapy in dosage of 1 mg/kg body weight, with a maximum of five doses, to patients with high oxygen requirements (SpO2/FiO2 <200) apart from the standard of care after obtaining G6PD levels. Data were abstracted from multiple electronic data sources or patient charts to provide information on patient characteristics, clinical and laboratory variables and outcomes.
Results: The median age of the patients was 53.3 (range 25–74 years) and most patients (74%) were men. About 68% of patients had pre-existing comorbidity. Median SpO2/FiO2 ratio progressively improved from 132.5 (predose) to 284 before the terminal event (death or discharge), ventilator-free days, and decrease in the proinflammatory biochemical parameter was significantly higher after the second dose of MB. A total of six patients out of 50 required invasive mechanical ventilation (IMV). Thirty patients were discharged with a recovery rate of 60%, while 20 patients succumbed to the illness. There was no major side effect or adverse event reported in any of the patients.
Conclusion: MB due to its polypharmacological action against SARS‐CoV‐2, an inexpensive and widely available drug with minimal side effects, has a significant potential in the treatment of COVID-19.
How to cite this article: Mahale N, Godavarthy P, Marreddy S, Gokhale SD, Funde P, Rajhans PA, et al. Intravenous Methylene Blue as a Rescue Therapy in the Management of Refractory Hypoxia in COVID-19 ARDS Patients: A Case Series. Indian J Crit Care Med 2021;25(8):934–938.
Keywords: Acute respiratory distress syndrome, Coronavirus disease 2019, Methylene blue, Rescue therapy
INTRODUCTION
Coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome‐coronavirus 2 (SARS‐CoV‐2) has severely impacted healthcare systems all over the world. Though the exact pathogenesis of SARS-CoV-2 is unknown, various hypotheses have proposed cytokine storm or hyperinflammatory syndrome as probable causes for the rapid worsening of the disease.1–3 Various drugs have been repurposed for treatment in the absence of definitive therapy with emphasis on the provision of supportive care including oxygenation, ventilator support, and other critical care life supports.4
The first COVID positive patient admitted at our hospital was on March 22, 2020, and to date, around 1,200 moderately to severe hypoxic COVID patients have been managed at our ICU. In view of resource-limited setting, rationing of available medical resources and constant modification of treating protocols keeping the patient safety were done to keep up with the pace of increased patient load.
Methylene blue (MB) or Bis (dimethylamino) phenazathionium chloride trihydrate, an organic dye, has been used extensively in an array of clinical conditions for the past two centuries. Few clinical conditions where the role of MB has been documented include treatment of malaria, refractory septic shock, catecholamine refractory vasoplegia, methemoglobinemia, and therapeutic benefit in hypoxia caused due to pulmonary vasodilation in patients of hepatopulmonary syndrome due to inhibition of guanylate cyclase and nitric oxide synthetase.5–9
Various theories have been postulated highlighting the benefits of administering MB as a salvage therapy among COVID-19 patients for its antiviral, anti-inflammatory, and antioxidant properties and have been proposed as a rescue therapy for improving the refractory hypoxia in COVID-19 patients.10,11 Till date, no clinical trials have been conducted evaluating the clinical effects of MB among COVID-19 patients.
Henry et al.12 proposed that MB could be of considerable help in the management of COVID-19 based on a survey of 2,500 French patients, treated with a combination of α-lipoic acid, hydroxycitrate, and MB as part of cancer care, in whom nil infections of the virus were reported. Also, MB in presence of light has broad-spectrum virucidal activity and has been used to inactivate viruses in blood products prior to transfusions.13 Recently, Cagno et al.14 documented in vitro antiviral properties of MB at low micromolar concentrations when incubated with Vero E6 cells and SARS-CoV-2 for 20 hours in the dark. Damir Bojadzic et al.15 proposed that MB inhibits the viral attachment and entry of SARS-CoV-2 by blocking the protein–protein interaction (PPI) of its spike protein with ACE2 on the host cell which is the first critical step initiating the viral entry. They suggested that this antiviral activity could be useful in the prevention and treatment of COVID-19 either as an oral or inhaled medication.
A phase one clinical trial documented a positive response in four out of five severely ill COVID-19 patients who were administered MB as a part of a three-drug regimen comprising of MB, vitamin C, and N-acetyl cysteine.16
In this study, we present a case series of 50 moderate to severe hypoxic COVID-19 patients who were administered intravenous MB as a rescue therapy at the discretion of the treating physician in addition to the standard of care treatment. Apart from the proposed above-mentioned clinical benefits, excellent safety profile, easy availability, low cost and minimal interactions with other drugs were factors considered for treatment with MB.
MATERIALS AND METHODS
Study Overview
The study was conducted by the Department of Critical Care Medicine in a tertiary care hospital located in Pune, India. The study was approved by the Institutional Ethics Committee and owing to the retrospective nature of the study, and waiver of informed consent was obtained.
Criteria for Patient Selection
Based on the clinical information available about MB at that time, the treating physicians preagreed upon the following inclusion and exclusion criteria.
Inclusion Criteria
Confirmed case of COVID-19 (by RT-PCR, antigen)
Admission to intensive care unit
PaO2/FiO2 <200 or SpO2/FiO2 <200
Exclusion Criteria
Pregnancy and breastfeeding
History of G6PDH deficiency
Severe renal insufficiency (glomerular filtration rate <30 mL/minute/1.73 m2)
Severe hepatic disease defined by SGOT or SGPT levels three times above the normal upper limit
Patients with a history of allergic reaction or significant sensitivity to MB
Owing to the huge deluge of patients and with limited resources, PaO2/FiO2 ratio of all patients could not be calculated and SpO2/FiO2 ratio was used as a substitute to monitor the patients. SpO2/FiO2 ratio has been validated in various clinical settings as an alternate to PaO2/FiO2 ratio.17–19
Standard of care, such as antivirals, steroids, and anticoagulants, was administered apart from oxygen supplementation by nasal cannula, nonrebreather mask (NRBM), high flow nasal cannula (HFNC), or noninvasive ventilation (NIV) as per the hospital protocol and discretion of the treating physician. Invasive mechanical ventilation was initiated based on the clinical assessment and SpO2/ FiO2 of the patients.
Intravenous MB was administered as rescue therapy in dosage of 1 mg/kg body weight to critically Ill patients admitted to ICU with high oxygen requirements (SpO2/FiO2 <200) and those who met the inclusion criteria apart from the standard of care after obtaining G6PD levels. A maximum of five doses of MB was given as per the clinical improvement, side effects, and discretion of treating physicians.
Data Source
Data were collected between June 01 and September 10, 2020, and the clinical outcomes were monitored till October 30, 2020. Demographics, clinical, and laboratory data on admission and the subsequent trends, mode of respiratory support (invasive mechanical ventilation, noninvasive mechanical ventilation, and oxygen mask), fraction of inspired oxygen (FiO2), SpO2/FiO2 ratio and treatment administered were collected from the electronic medical records. The collected data were analyzed and interpreted by two independent intensivists. The clinical team provided clarification on missing or redundant data.
Data Analysis
Data were analyzed using descriptive statistics. Pair-wise statistical comparisons of normally distributed continuous variables were done using repeated measures analysis of variance or non-normally distributed continuous variables the Pair-wise statistical comparisons were done using Wilcoxon’s signed-rank test. The underlying normality assumption was tested before subjecting study variables to RMANOVA. In the entire study, the p-values less than 0.05 were considered to be statistically significant. The entire data were statistically analyzed using Statistical Package for Social Sciences (SPSS ver 22.0, IBM Corporation, USA) for MS Windows.
STUDY OUTCOMES
Results
A total of 50 patients were included in the study. The age of the patients ranged from 25 to 74 years (mean 53.3 ± 12.2 years; Table 1). The majority of patients were male (74%). Pre-existing comorbidities were reported in 68% of patients with diabetes (14%), hypertension (16%), 30% of patients reported having both diabetes and hypertension, and 8% of patients other comorbidities.
Table 1.
Distribution of demographic characteristics of cases studied
| No. of cases | % of cases | ||
|---|---|---|---|
| Age group (years) | <40 | 7 | 14.0 |
| 40–49 | 11 | 22.0 | |
| 50–59 | 15 | 30.0 | |
| 60–69 | 10 | 20.0 | |
| >70 | 7 | 14.0 | |
| Mean ± SD | 53.3 ± 12.2 | ||
| Sex | Male | 37 | 74.0 |
| Female | 13 | 26.0 | |
| Comorbidity | Absent | 16 | 32.0 |
| Diabetes mellitus | 7 | 14.0 | |
| Hypertension | 8 | 16.0 | |
| Diabetes mellitus + hypertension | 15 | 30.0 | |
| Other | 4 | 8.0 |
Patients with SpO2/FiO2 <200 were included in the study, the lowest ratio was 84 and the highest was 196 (mean 132.5, SD 33.3). Eighty-two percentage patients were on HFNC, 8% on NRBM, 10% on NIV prior to starting of MB (Table 4).
Table 4.
Requirement of invasive mechanical ventilation among patients given MB
| Prior to MB | After dose 1 | After dose 2 | After dose 3 | |
|---|---|---|---|---|
| HFNO | 41 | 43 | 39 | 25 |
| NIV | 5 | 3 | 2 | 3 |
| NRBM | 4 | 2 | 6 | 2 |
| IMV | 0 | 2 | 3 | 1 |
| IMV ratio | 2/50 | 3/48 | 1/31 | |
| IMV (%) | 4 | 6.25 | 3.22 |
Distribution of Mean SpO2/FiO2 Ratio Prior and Post-MB Administration.
Median SpO2/FiO2 ratio improved from 132.5 (predose) to 189.3 after administration of third or higher doses of MB with a mean ratio of 284 documented before the terminal event (death or discharge). The distribution of the mean SpO2/FiO2 ratio post-MB administration was significantly higher compared to mean SpO2/ FiO2 ratio prior to MB administration (p-value <0.001) (Figs 1 and 2, Tables 2,3,5).
Fig. 1.
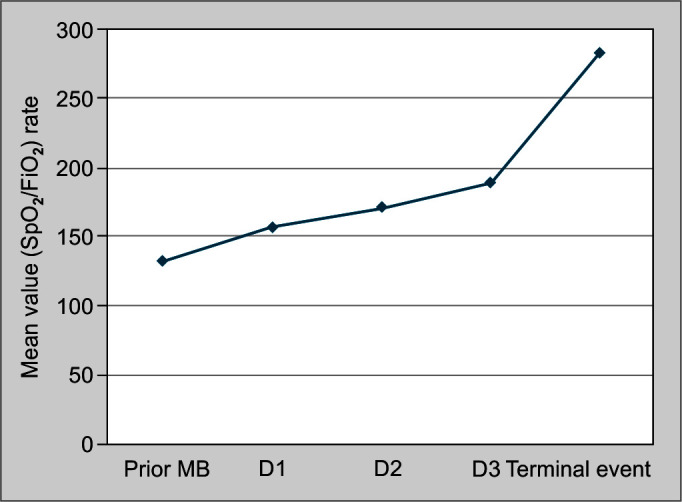
Distribution of mean SpO2/FiO2 ratio prior and post-MB administration
Fig. 2.
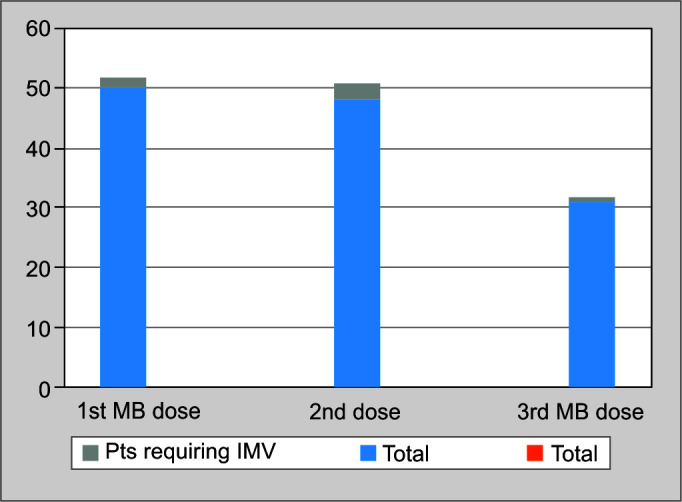
Distribution of requirement of IMV vs dosage of MB
Table 2.
Distribution of mean SpO2/FiO2 ratio prior and post-MB administration
| SpO2/FiO2 ratio | Prior to first dose of MB | Post-first dose | Post-second dose | Post-third dose | Before the terminal event (death or discharge) | p value |
|---|---|---|---|---|---|---|
| n | 50 | 50 | 49 | 31 | 50 | |
| Mean | 132.5 | 156.9 | 171.4 | 189.3 | 284.1 | 0.001*** |
| SD | 33.3 | 47.9 | 53.9 | 63.1 | 159.0 |
p value by repeated measures ANOVA (RMANOVA); p-value <0.05 is considered to be statistically significant.
p-value <0.001
Table 3.
Distribution of mean SpO2/FiO2 ratio vs ventilator-free days
| Characteristics | Ventilator-free days | p value | |||
|---|---|---|---|---|---|
| n | Mean | SD | |||
| SpO2/FiO2 (After dose 1) n = 50 |
<200 | 42 | 24.2 | 6.2 | 0.353NS |
| >200 | 8 | 26.0 | 2.7 | ||
| SpO2/FiO2 (After dose 2) n = 50 |
<200 | 36 | 23.4 | 6.6 | 0.041* |
| >200 | 14 | 26.8 | 2.3 | ||
| SpO2/FiO2 (After dose 3) n = 31 |
<200 | 17 | 22.9 | 7.6 | 0.265NS |
| >200 | 14 | 25.6 | 5.6 | ||
| SpO2/FiO2 (terminal event) | <200 | 20 | 22.0 | 4.8 | 0.007** |
| >200 | 30 | 26.2 | 5.7 | ||
p value by Wilcoxon’s signed-rank test; p-value <0.05 is considered to be statistically significant,
p-value <0.001; NS, statistically non significant
Table 5.
Distribution of median CRP and ALC prior and post-MB administration
| Parameter | Prior to MB | Post-MB | p value | |
|---|---|---|---|---|
| CRP | Median | 106.6 | 22.7 | 0.001*** |
| Min–max | 13.69–325.70 | 2.80–275.77 | ||
| ALC | Median | 820.0 | 880.0 | 0.079NS |
| Min–max | 80–1,850 | 80–4,220 |
p value by Wilcoxon’s signed-rank test; p-value <0.05 is considered to be statistically significant;
p-value <0.001; NS, statistically non-significant
Dose 1 of MB: Mean duration of ventilator-free days did not differ significantly between the two group of cases with SpO2/FiO2 less than or more than 200 (p >0.05).
Dose 2 of MB: Mean duration of ventilator-free days was significantly higher in group of cases with SpO2/FiO2 >200, compared to cases with SpO2/FiO2 <200 (p <0.05).
Dose 3 of MB: Mean duration of ventilator-free days did not differ significantly between the two group of cases with SpO2/ FiO2 less than or more than 200 (p-value >0.05).
Before terminal event: Mean duration of ventilator-free days was significantly higher in group of cases with SpO2/FiO2 more than 200 compared to group of cases with SpO2/FiO2 less than 200 (p-value <0.05).
Six out of 50 patients required Invasive mechanical ventilation during the period of study.
A significant decrease in the proinflammatory biochemical parameter (CRP) was noticed post-MB administration.
No significant improvement in absolute lymphocyte count (ALC) was observed post-MB administration.
Thirty patients were discharged with a recovery rate of 60. The average total length of stay during hospitalization was 14.24 ± 4.15 days.
No patient was lost to follow up and there were no major side effects or adverse events reported in any of the 50 patients, except for temporary bluish discoloration of urine.
DISCUSSION
This case series would be to our knowledge the first study in India that presents data of hypoxic COVID-19 patients treated with intravenous MB. During the review of the literature, we could not find any data or clinical trials pertaining to the administration of intravenous MB for the treatment of COVID-19 patients.
The rapid surge in the number of patients infected with COVID and the high caseload on the hospitals have led medical researchers to identify new drugs that could help treat patients with COVID- 19. Various drugs with known safety profiles, easy availability, and effectiveness in managing complications have been studied. MB an organic dye has been used extensively in an array of clinical conditions for the past two centuries and has been proposed as a rescue therapy for improving the refractory hypoxia in COVID-19 patients. Various theories have been postulated highlighting the benefits of administering MB as a salvage therapy among COVID- 19 patients including antiviral, anti-inflammatory, and antioxidant properties.20
MB in presence of light has broad-spectrum virucidal activity and has been used to inactivate viruses in blood products prior to transfusions.13 Recently, Cagno et al.14 documented in vitro antiviral properties of MB at low micromolar concentrations when incubated with Vero E6 cells and SARS-CoV-2 for 20 hours in the dark. Bojadzic et al.15 proposed that MB inhibits the viral attachment and entry of SARS-CoV-2 by blocking the PPI of its spike protein with ACE2 on the host cell which is the first critical step initiating the viral entry. They suggested that this antiviral activity could be useful in the prevention and treatment of COVID-19 either as an oral or inhaled medication. Gendrot et al.21 demonstrated that nonphoto-activated MB showed high in vitro antiviral effective activity against SARS-CoV-2 with an inhibitory concentration (IC) IC50 (0.3 μM) and IC90 (0.75 μM) compatible with oral uptake and IV administration. This in vitro activity was higher than those obtained with drugs such as hydroxychloroquine (1.5 μM), azithromycin (20.1 μM), remdesivir (23 μM), lopinavir (26.6 μM), or ritonavir (>100 μM). Barber et al. and Vardhana et al. reported that MB by blocking the downstream cosignaling PPIs of the cytotoxic T lymphocytes, restores their cytotoxicity, activation, proliferation, and cytokine secreting activity thereby restoring T cell homeostasis and function, which in turn improves viral clearance.22,23
Henry et al.12 proposed that MB could be of considerable help in the management of COVID-19 based on a survey of 2,500 French patients treated with a combination of α-lipoic acid, hydroxycitrate, and MB as part of cancer care in whom nil infections of the virus were reported. They proposed that upon absorption, MB undergoes one-electron reduction and becomes a neutral lipophilic MB radical. This radical acts as a weak base (pKa ~9) which could cause transient alkalization of cytosolic spaces. As acidic media (PH <5) is mandatory for endosome maturation and function, this alkalization could inhibit endosome maturation at intermediate stages of endocytosis resulting in failure of further import of virions into the cytosol. These antiviral properties of MB could be used as a treatment in COVID patients. Ghahestani et al.10 described the pivotal role of the Kininogen system in the pathogenesis of SARS-CoV-2 and suggested the hypothetical potential of MB being an inhibitor of NO synthetase could abort effects of bradykinin and could be used in the treatment of SARS-CoV-2 to improve oxygen saturation.
MB is generally safe, but dose-dependent toxicity with nausea, vomiting, hemolysis, and other undesired side effects at doses >7 mg/kg (i.e., >500 mg) is known.6,7
At our center, intravenous MB was administered as per the discretion of the treating physician in patients who had SpO2/ FiO2 ratio <200 and was refractory to the best of supportive care being provided. Dosage was restricted to a maximum of 5 mg/kg of intravenous MB in a divided dose. No major adverse events were documented in any of the fifty patients who were administered intravenous MB except for temporary bluish discoloration of urine.
There was a significant improvement in the SpO2/FiO2 ratios progressively after the second dose of IV MB and it was statistically significant at the terminal event (death or discharge). The distribution of mean SpO2/FiO2 ratio post-MB administration was higher compared to the ratio prior to MB administration. We also noted that the mean duration of ventilator-free days was significantly higher in group with SpO2/FiO2 >200 compared to the group with SpO2/FiO2 <200 before the terminal event. Progression from noninvasive to IMV was seen in 6 patients out of 50. A significant reduction in the proinflammatory biochemical parameter (CRP) was noticed post-MB dosage.
Limitations
We acknowledge the limitations of our study. First, this was a case series carried out in a single center with all its inherited biases. Second, the data were collected from electronic medical health record database, thereby precluding detailed information about the patient’s demographics and baseline medications. Third, the nonuniformity in the selection of the study subjects due to the participants’ inclusion criteria as well as by the studies design, limited investigations were conducted due to cost constraints, high heterogeneity observed in the number of doses as well as the timing of administration of the drug making the data redundant for comparative analysis.
Implications for Future Research
Larger trials with a more robust study design, randomized control trials comparing IV MB with a standard of care in regards to important clinical outcome variables.
CONCLUSION
MB due to its polypharmacology in the action against SARS-CoV-2, being an inexpensive and widely available drug potentially has a significant role in the treatment of COVID-19.
Footnotes
Source of support: Nil
Conflict of interest: None
ORCID
Nilesh Mahale https://orcid.org/0000-0002-7952-8259
Purushotham Godavarthy https://orcid.org/0000-0002-5727-3419
Srinath Marreddy https://orcid.org/0000-0002-8405-7500
Snehal D Gokhale https://orcid.org/0000-0002-0183-2023
Pradip Funde https://orcid.org/0000-0003-0790-9949
Prasad A Rajhans https://orcid.org/0000-0002-0111-6123
Prasad V Akole https://orcid.org/0000-0001-5655-7471
Balasaheb Pawar https://orcid.org/0000-0001-9622-8357
Bhagyashri Bhurke https://orcid.org/0000-0002-5139-7955
Pradip Dalvi https://orcid.org/0000-0002-7690-5426
Prasanna Marudwar https://orcid.org/0000-0002-2730-8641
Shradha Gugale https://orcid.org/0000-0003-1476-248X
Manasi S Shahane https://orcid.org/0000-0002-5304-9647
Sarang N Kshirsagar https://orcid.org/0000-0002-5541-2905
Sameer A Jog https://orcid.org/0000-0002-1134-1260
REFERENCES
- 1.van de Veerdonk F, Netea MG, van Deuren M, van der Meer JW, de Mast Q, Bruggemann RJ, et al. Kinins and cytokines in COVID-19: a comprehensive pathophysiological approach. Preprints. 2020. doi: 10.20944/preprints202004.0023.v1.. DOI: [DOI] [Google Scholar]
- 2.Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;;368((6490):):473––474.. doi: 10.1126/science.abb8925.. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘cytokine storm’ in COVID-19. J Infect. 2020;;80((6):):607––613.. doi: 10.1016/j.jinf.2020.03.037.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salvi R, Patankar P. Emerging pharmacotherapies for COVID-19. Biomed Pharmacother. 2020;;128::110267.. doi: 10.1016/j.biopha.2020.110267.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwok ES, Howes D. Use of methylene blue in sepsis: a systematic review. J Intensive Care Med. 2006;;21((6):):359––363.. doi: 10.1177/0885066606290671.. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Bistas E, Sanghavi D. StatPearls [Internet]. Treasure Island (FL):: StatPearls Publishing;; 2021. Methylene Blue. [Updated 2020 Jul 2]. Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557593/ [PubMed] [Google Scholar]
- 7.Clifton J, Leikin JB. Methylene blue. Am J Therapeut. 2003;;10((4):):289––291.. doi: 10.1097/00045391-200307000-00009.. DOI: [DOI] [PubMed] [Google Scholar]
- 8.Schenk P, Madl C, Rezaie-Majd S, Lehr S, Müller C. Methylene blue improves the hepatopulmonary syndrome. Ann Intern Med. 2000;;133((9):):701––706.. doi: 10.7326/0003-4819-133-9-200011070-00012.. DOI: [DOI] [PubMed] [Google Scholar]
- 9.Mayer B, Brunner F, Schmidt K. Inhibition of nitric oxide synthesis by methylene blue. Biochem Pharmacol. 1993;;45((2):):367––374.. doi: 10.1016/0006-2952(93)90072-5.. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Ghahestani SM, Shahab E, Karimi S, Madani MH. Methylene blue may have a role in the treatment of COVID-19. Med Hypotheses. 2020;;144::110163.. doi: 10.1016/j.mehy.2020.110163.. ISSN 0306-9877. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Floyd RA, Schinazi RF. Antiviral therapy using thiazine dyes. Google Patents. 2002::6346529.. Available from: http://www.freepatentsonline.com/6346529.html.
- 12.Henry M, Summa M, Patrick L, Schwartz L. A cohort of cancer patients with no reported cases of SARS-CoV-2 infection: the possible preventive role of Methylene Blue. Substantia. 2020;;4((1):):888.. doi: 10.13128/Substantia-888.. DOI: [DOI] [Google Scholar]
- 13.Yu B, Jin C, Zhang J, Wu H, Zhou X, Yao H, et al. Methylene blue photochemical treatment as a reliable SARS-CoV-2 plasma virus inactivation method for blood safety and convalescent plasma therapy for the COVID-19 outbreak. BMC Infect Dis. 2021;;21((1):):357.. doi: 10.1186/s12879-021-05993-0.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Cagno V, Medaglia C, Cerny A, Cerny T, Tapparel C, Cerny E. Methylene blue has a potent antiviral activity against SARS-CoV-2 in the absence of UV-activation in vitro. bioRxiv. 2020. doi: 10.1101/2020.08.14.251090.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bojadzic D, Alcazar O, Buchwald P. Methylene Blue inhibits the SARS-CoV-2 Spike–ACE2 Protein–Protein interaction – a mechanism that can contribute to its antiviral activity against COVID-19. Front Pharmacol. 2021;;11::600372.. doi: 10.3389/fphar.2020.600372.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alamdari DH, Moghaddam AB, Amini S, Keramati MR, Zarmehri AM, Alamdari AH, et al. Application of methylene blue-vitamin C-Nacetyl cysteine for treatment of critically ill COVID-19 patients, report of a phase-I clinical trial. Eur J Pharmacol. 2020;;885::173494.. doi: 10.1016/j.ejphar.2020.173494.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rice TW, Wheeler AP, Bernard GR, Hayden DL, Schoenfeld DA, Ware LB. Comparison of the SpO2/FiO2 ratio and the PaO2/FiO2 ratio in patients with acute lung injury or ARDS. Chest. 2007;;132((2):):410––417.. doi: 10.1378/chest.07-0617.. DOI: [DOI] [PubMed] [Google Scholar]
- 18.Pisani L, Roozeman JP, Simonis FD, Giangregorio A, van der Hoeven SM, Schouten LR, et al. Risk stratification using SpO2/FiO2 and PEEP at initial ARDS diagnosis and after 24 h in patients with moderate or severe ARDS. Ann Intensive Care. 2017;;7((1):):108.. doi: 10.1186/s13613-017-0327-9.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown SM, Grissom CK, Moss M, Rice TW, Schoenfeld D, Hou PC, et al. NIH/NHLBI PETAL Network Collaborators. Nonlinear imputation of PaO2/FiO2 from SpO2/FiO2 among patients with acute respiratory distress syndrome. Chest. 2016;;150((2):):307––313.. doi: 10.1016/j.chest.2016.01.003.. DOI: PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Golwalkar D. Treatment for COVID-19 using methylene blue. Medium. 2020. Available at: https://medium.com/@dr.deepak.golwalkar/treatment-for-covid-19-using-methylene-blue-d23fc5a31a4d [Accessed April 12, 2020].
- 21.Gendrot M, Andreani J, Duflot I, Boxberger M, Bideau ML, Mosnier J, et al. Methylene blue inhibits replication of SARS-CoV-2 in vitro. Int J Antimicrob Agents. 2020;;56::106202.. doi: 10.1016/j.ijantimicag.2020.106202.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barber DL, Wherry EJ, Masopust D, Zhu B, Allison JP, Sharpe AH, et al. Restoring function in exhausted CD8 T cells during chronic viral infection. Nature. 2006;;439((7077):):682––687.. doi: 10.1038/nature04444.. DOI: [DOI] [PubMed] [Google Scholar]
- 23.Vardhana SA, Wolchok JD. The many faces of the anti-COVID immune response. J Exp Med. 2020;;217((6):):e20200678.. doi: 10.1084/jem.20200678.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]


