How to cite this article
Long MT, Grate J, Bradley KV. Postoperative Hemidiaphragmatic Paralysis and Platypnea–Orthodeoxia Syndrome. Indian J Crit Care Med 2021;25(8):951–953.
Keywords: Critical care, Echocardiography, Hypoxia, Hypoxemia right to left shunt echocardiography
Platypnea–orthodeoxia syndrome (POS) is an uncommon clinical syndrome characterized by dyspnea and hypoxia in the upright position and is most often due to hepatopulmonary syndrome. POS can also, however, result from an intracardiac shunt even in the face of normal intracardiac pressures.1 We report a case of platypnea-orthodeoxia due to postoperative right hemidiaphragmatic paralysis, which caused right atrial compression and shunting through an atrial septal aneurysm with an associated atrial defect. Written consent was obtained from the patient to discuss this clinical case.
A 67-year-old woman with a medical history of obesity was admitted for persistent hypoxia after resection of a thymoma via a right-sided muscle-sparing thoracotomy. She was found to have platypnea-orthodeoxia with oxygen saturations of 88 to 89% when supine and 80 to 83% when upright. Initial chest radiography revealed right hemidiaphragmatic elevation with a small pleural effusion; computerized tomography (CT) of the chest with contrast on postoperative day (POD) three was only notable for hemidiaphragmatic elevation abutting the right atrium (Fig. 1). With lack of resolution, a transesophageal echocardiogram (TEE) was performed on POD 12, demonstrating compression of the right atria from the diaphragm in addition to a large atrial septal aneurysm with an associated interatrial communication (Fig. 2). Next, a transthoracic echocardiogram (TTE) was performed in the supine and upright positions, revealing a bulging atrial septal aneurysm and a shunt only when upright (Fig. 3). Cardiac catheterization showed normal intracardiac pressures and right atrial compression that shifted the heart leftward and favored blood flow from the inferior vena cava toward the fossa ovalis and atrial septal aneurysm. Percutaneous closure of the defect was performed.
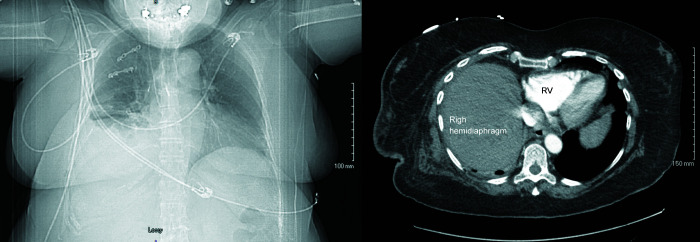
Fig. 1.
CT of the chest with pulmonary angiography. Imaging obtained on POD three for persistent hypoxia was negative for pulmonary embolism but was notable for persistent hemidiaphragmatic elevation (left) and abutting the right atrium (right)
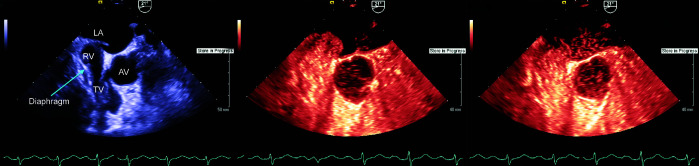
Fig. 2.
Transesophageal echocardiography (TEE). Imaging demonstrated compression of the right atria by the diaphragm, in addition to a large atrial septal aneurysm and interatrial communication (left), with a positive bubble study (middle to right). LA, left atrium; AV, aortic valve/proximal aorta; TV, tricuspid valve; RA, right atrium ; RV, right ventricle
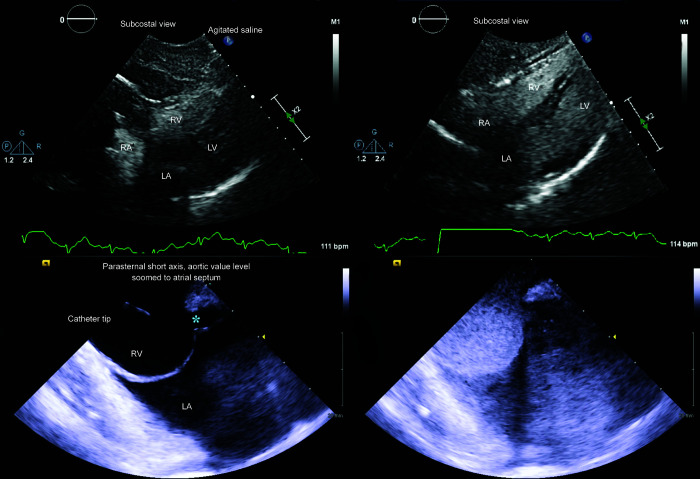
Fig. 3.
Transthoracic echocardiography (TTE). Subcostal imaging confirmed an interatrial communication in the upright position in both subcostal (upper, left to right), and short-axis, aortic valve level (lower, left to right) views. RV, right ventricle; LV, left ventricle; LA, left atria; RA, right atria. The atrial septal aneurysm-associated defect is labeled with an asterisk (*)
POS results in hypoxia and dyspnea in the upright position due to positional right-to-left shunt unrelated to intracardiac pressure gradients. Typical anatomic aberrations that result in POS alter caval drainage into the right atria and direct caval blood toward an interatrial communication.2 Most anatomic aberrations that result in POS are at the level of the heart, including postoperative anatomic shifts after aortic valve repair, certain tricuspid regurgitant jets, and others.2 Postsurgical right hemidiaphragmatic paralysis, however, can compress the right atria and point blood toward the preexisting atrial septal aneurysm and interatrial communication.3
Postoperative development of POS is rare and is diagnosed by observing supine-to-upright decrements in pulse oximetry. Shunt should be assessed for via supine and upright echocardiography, utilizing an agitated bubble study with Valsalva maneuver.3 If no shunt is identified, noncardiac etiologies of POS should be assessed for with respiratory and abdominal imaging.2 If a shunt is present and imaging is not declarative, cardiac catheterization to assess right atrial pressure should be performed. If normal, anatomic abnormalities that cause POS can be assessed for with radiography, CT, fluoroscopy, or cardiac magnetic resonance imaging.4 Management emphasizes percutaneous closure of the anatomic defect.3
Micah T Long directed the creation of the work and prepared, drafted, and revised the manuscript, including important intellectual content, and approved the final manuscript.
Kaitlyn V Bradley prepared and drafted the initial manuscript, critically reviewed the manuscript, provided commentary, and approved the final version of the document.
Jeremy Grate critically revised the manuscript for important intellectual content and approved the final version of the document.
Footnotes
Source of support: Nil
Conflict of interest: None
ORCID
Micah T Long https://orcid.org/0000-0002-7297-5304
Jeremy Grate https://orcid.org/0000-0002-3737-8037
Kaitlyn V Bradley https://orcid.org/0000-0001-5858-7260
REFERENCES
- 1.Agrawal A, Palkar A, Talwar A. The multiple dimensions of platypnea-orthodeoxia syndrome: a review. Respir Med. 2017;;129::31––38.. doi: 10.1016/j.rmed.2017.05.016.. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Knapper JT, Schultz J, Das G, Sperling LS. Cardiac platypnea-orthodeoxia syndrome: an often unrecognized malady. Clin Cardiol. 2014;;37((10):):645––649.. doi: 10.1002/clc.22301.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sakagianni K, Evrenoglou D, Mytas D, Vavuranakis M. Platypnea-orthodeoxia syndrome related to right hemidiaphragmatic elevation and a ‘stretched’ patent foramen ovale. BMJ Case Rep. 2012;;2012::bcr-2012-007735.. doi: 10.1136/bcr-2012-00735.. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dundon B, Psaltis P, Worthley S. Cardiac magnetic resonance and “augmented” right-to-left intracardiac shunting through a patent foramen ovale. J Invasive Cardiol. 2008;;20((4):):197––198.. PMID: [PubMed] [Google Scholar]