Abstract
A case of silicosis presenting as middle lobe syndrome is described in a middle-aged female. The diagnosis was confirmed by both bronchoscopy and demonstration of right middle lobe lumen narrowing and compression by calcified hilar lymph nodes on computerized tomographic scan. Simultaneous occurrence of endobronchial silicosis and bronchial stenosis by enlarged calcified peribronchial lymph nodes causing middle lobe syndrome has not been described previously as reported in this case.
Keywords: Middle lobe syndrome, silicosis, lymph node
INTRODUCTION
Silicosis is an age old and most prevalent pneumoconiosis that is caused by the inhalation of crystalline silica dust. Diagnosis of silicosis is based on the history of silica exposure sufficient enough to cause illness, along with chest radiographic features consistent with silicosis and absences of other illnesses that mimic silicosis. The characteristic radiographic features of silicosis are small rounded opacities, usually symmetrically distributed with upper zone predominance. In some patients, diffuse interstitial fibrosis pattern is seen without classical nodular pattern. Opacities larger than 1 cm form progressive massive fibrosis. With progression, there is hyperinflation with bullae formation and enlargement of hilar and mediastinal lymph nodes with subsequent calcification.[1]
The right middle lobe consolidation and atelectasis that is classically described as middle lobe syndrome is rarely seen in silicosis.[2] This communication describes a case of silicosis presenting with right middle lobe syndrome.
CASE REPORT
A 54-year-old female presented with a history of cough, breathlessness and chest pain off and on for the last 2 years. There was no history of fever or hemoptysis. She denied any history of tuberculosis in her past or in the family.
She had worked in a stone cutter factory for about 12 years without any protective device or mask against stone dust. She used to work for 7-8 hours in a day for the whole week with only a few non-working days due to yearly religious festivals. She was illiterate, non-smoker with no addiction history. She was average built but poor nourished having a body mass index of 17.12 with anemia. Respiratory examination revealed reduced intensity of breath sounds and crepitation's over the right mammary area.
Skiagram chest posteroanterior (PA) view showed multiple small rounded opacities in both the lung fields along with enlarged calcified hilar lymph nodes and atelectasis of the right middle lobe [Figure 1]. CT scan of the lung revealed multiple well-defined dense pulmonary nodules with random distribution in the bilateral lung fields along with mosaic attenuation, fibro-parenchymal changes with bronchiectasis, soft tissue density lesion with volume loss and calcified areas in the right middle lobe and multiple enlarged mediastinal and hilar lymph nodes with nodular calcification Figures [2a and b, 3a]. Right middle lobe bronchostenosis and protrusion of calcified nodes causing luminal distortion were also evident. The radiographic features were suggestive of silicosis.
Figure 1.
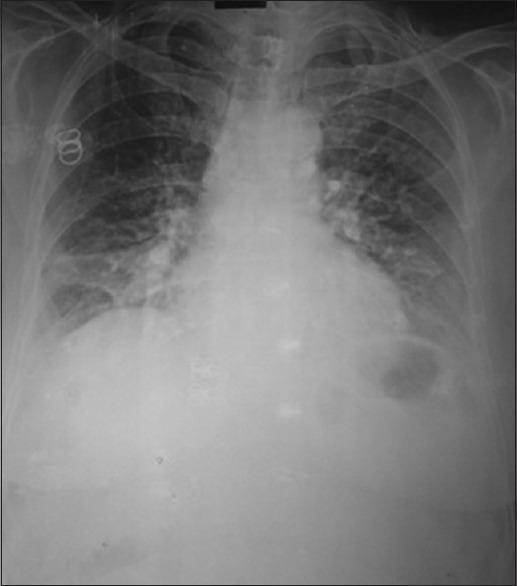
X-ray chest PA view showing bilateral pulmonary nodules with hilar calcification and wedge-shaped right middle lobe opacity
Figure 2.
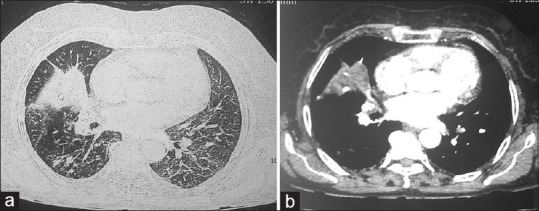
(a) CT scan showing bilateral, randomly distributed dense pulmonary nodules with right middle lobe atelectasis and hilar calcification with bronchostenosis and distorted lumen (b)
Figure 3.
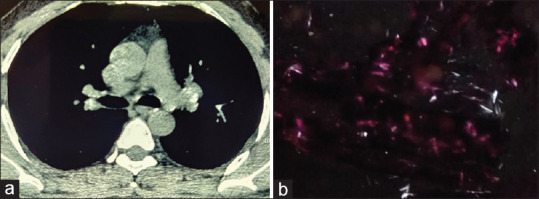
(3a) CT scan showing bilateral calcified hilar lymph nodes on non-contrast scan () and (b) photomicrograph of endobronchial biopsy tissue showing birefringent crystals on polarized microscopy
Spirometry revealed forced expiratory volume in the first second (FEV1) value of 1.43 l (56% predicted), forced vital capacity (FVC) 1.46 l (49% predicted), FEV1% 98.4 (124% predicted), forced expiratory flow at 25–75% of forced vital capacity (FEF25–75%) 1.92 l/s (59% predicted) and peak expiratory flow (PEF) 3.72 l/s (59% predicted). A six-minute walk distance was 126 m. Her SpO2 was 95% at room air and it fell to 90% after a 6-minute walk test. On advanced pulmonary function testing, the diffusion lung capacity for carbon monooxide (DLCO) was 11.23 mL/min/mmHg (47% predicted) with a ratio of DLCO to alveolar volume (DLCO/VA) 85% predicted and residual volume (RV) 76% predicted and TLC 56% predicted.
On fibreoptic bronchoscopy, right middle lobe lumen was grossly narrowed with focal protruded wall medially. The endobronchial mucosa was thickened, hyper pigmented with brownish black patches. Biopsy tissues were taken along with brush cytology smears and bronchial lavage from the affected areas. Bronchial brushing showed chronic inflammation but no acid fast bacilli. The bronchial lavage on cartridge based nucleic acid amplification test (CBNAAT) did not detect mycobacterium tuberculosis. The histopathology of biopsy material revealed mainly dense fibrotic areas with whorled collagenous tissue and scanty cellular areas showing chronic inflammatory cells and anthracotic pigment-laden macrophages but no granulomas or acid fast bacilli. On polarizing microscopy, scattered birefringent crystals were seen [Figure 3b].
DISCUSSION
Middle lobe syndrome is a rare but an important clinical entity characterized by chronic or recurrent collapse of middle lobe of the right lung, and sometimes, lingula of the left lung. First reported by Graham et al.[3] in 1948, this condition is pathophysiologically divided into two forms: obstructive and non-obstructive type. Non-obstructive type is more common, seen in adults and children with recurrent pneumonia in relation to asthma, cystic fibrosis and bronchitis. The obstructive type is caused by endobronchial obstruction (mostly due to benign or malignant tumors) or extrinsic compression of the right middle lobe by enlarged peribronchial lymph nodes. Less commonly, this is seen with aspirated foreign body, broncholiths, endobronchial granulomas, etc.[4] The right middle lobe is also more susceptible for collapse due to inherent anatomical and physiological peculiarities, i.e., longer with narrow angle with orifice, inefficient collateral ventilation, close surrounding lymph nodes, etc.[5]
Three cases of silicosis that complicated to middle lobe atelectasis were first described in 1982 in Chinese literature.[6] In silicosis, the right middle lobe syndrome may be contributed by the external compression of enlarged lymph nodes or endobronchial obstruction. Chien HP et al.[2] described four cases of endobronchial silicosis causing the right middle lobe atelectasis without any external compression. Endobronchial silico-tuberculosis lesion without extrinsic compression is also reported to cause the right middle lobe syndrome in a 72-year-old male from Australia.[7] Tracheobronchial obstruction by calcified mediastinal lymph nodes compression and erosion is also reported to cause middle lobe atelectasis.[8] Endobronchial silicotic lesions are very rare and various mechanism of middle lobe atelectasis in silicosis includes local bronchial wall fibrosis, broncholithiasis, endoluminal erosion of peribronchial lymphadenopathy and extrinsic compression by enlarged peribronchial lymph nodes causing bronchostenosis.[2] In our case, the cause for the middle lobe syndrome was both endobronchial lesion as well as external compression by the calcified lymph nodes evident both on CT image and on bronchoscopy. This dual mechanism causing the middle lobe syndrome in silicosis has not been described previously in literature as seen in present case.
Endobronchial silicosis and calcified peribonchial silicotic lymph nodes causing middle lobe atelectasis although rarely described in literature, should also be included in the differential diagnosis of the middle lobe syndrome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hansell DM, Lynch DA, McAdams HP, Banker AA. Imaging of diseases of the chest. 5th ed. St Louis, MO: Mosby Elsevier; 2010. pp. 463–8. [Google Scholar]
- 2.Chien HP, Lin TP, Chen HL, Huang TW. Right middle lobe atelectasis associated with endobronchial silicotic lesions. Arch Pathol Lab Med. 2000;124:1619–22. doi: 10.5858/2000-124-1619-RMLAAW. [DOI] [PubMed] [Google Scholar]
- 3.Graham EA, Burford TH, Mayer JH. Middle lobe syndrome. Postgrad Med. 1948;4:29–34. doi: 10.1080/00325481.1948.11693655. [DOI] [PubMed] [Google Scholar]
- 4.Gudbjartsson T, Gudmundsson G. Middle lobe syndrome: A review of clinicopathological features, diagnosis and treatment. Respiration. 2012;84:80–6. doi: 10.1159/000336238. [DOI] [PubMed] [Google Scholar]
- 5.Inners CR, Terry PB, Traystman RJ, Menkes HA. Collateral ventilation and the middle lobe syndrome. Am Rev Respir Dis. 1978;118:305–10. doi: 10.1164/arrd.1978.118.2.305. [DOI] [PubMed] [Google Scholar]
- 6.Xu LY, Yang DN, Shyy JC. Silicosis leading to the development of right middle lobe atelectasis: Report of 3 cases. Chin J Prev Med. 1982;16:303–5. [PubMed] [Google Scholar]
- 7.Anderson JJ, Fong KM, Godbolt DB, Leong SC, Marshall HM. Endobronchial silicosis and tuberculosis presenting as the right middle lobe syndrome. J Bronchology Interv Pulmonol. 2016;23:e35–7. doi: 10.1097/LBR.0000000000000302. [DOI] [PubMed] [Google Scholar]
- 8.Cahill BC, Harmon KR, Shumway SJ, Mickman JK, Hertz MI. Tracheobronchial obstruction due to silicosis. Am Rev Respir Dis. 1992;145:719–21. doi: 10.1164/ajrccm/145.3.719. [DOI] [PubMed] [Google Scholar]


