Abstract
Background
Self-medication with antibiotics (SMA) is an important public health issue, which can result in the facilitated development of antibiotic resistance, and may increase the risk of inappropriate utilization of antibiotics. So, the objective of the present study was to estimate the prevalence rate of SMA and to also explore SMA practices among the lay population of Kuala Lumpur (Malaysia).
Methods
The current study was cross-sectional population-based and used a convenient sampling technique. Moreover, Lorenz’s formula was used to calculate the sample size and the required sample size was 480. Data were collected through face-to-face interviews with a pre-validated questionnaire and the study was conducted in Kuala Lumpur (Malaysia). Descriptive statistics, cross-tabulation, and logistic regression were executed by using SPSS version 24.
Results
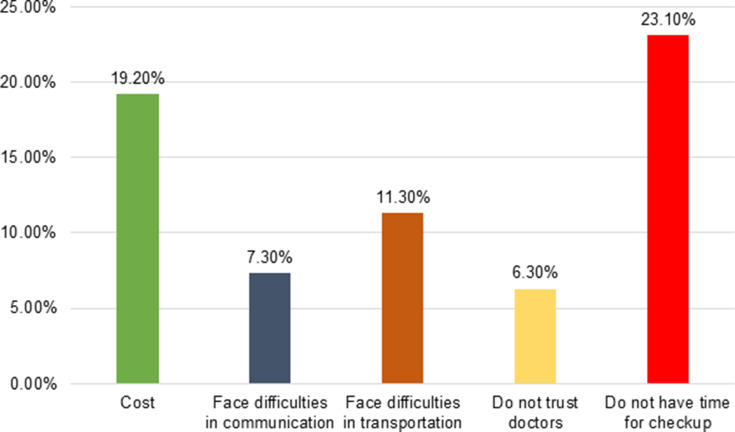
Out of 480 participants, 45.8% were polled male and the prevalence of SMA in this study was found to be 15.1%. The majority of participants 23.1% indicated that they practiced antibiotics at least once in the last six months. The commonly self-medicated antibiotics were amoxicillin-clavulanate 20.6%, ampicillin/cloxacillin 14.2%, and levofloxacin 8.3%. Moreover, 64.8% of participants indicated that they bought their antibiotics from pharmacies. Whereas, most of the participants practice antibiotics to save money 19.2% and time 23.1%. Findings from multivariate logistic regressions showed that predictors of SMA were male gender, (95% CI: 0.300–0.877) occupation (95% CI: 0.122–10.797), health insurance (95% CI: 0.025–0.472), and education (95% CI: 0.084–0.800).
Conclusion
The results of this study indicate that SMA persists among the community and education level has a significant impact on this behavior. Thus, concerning health management authorities should step in with developing legislation to stop this practice, and by implementing such interventions and policies to educate and to raise awareness about the risk of SMA for the future.
Keywords: self-medication, antibiotics, Malaysia, questionnaire, practices, resistance, cross-sectional
Background
Ever since the introduction of penicillin, the first antibiotic about 92 years ago, antibiotics have become a significant and vital part of modern healthcare, in the treatment of infectious ailments caused by bacteria. However, the frequent and inappropriate use (the use of antibiotics not prescribed by a medical professional) of antibiotics has prompted the phenomenon of antimicrobial resistance, which has turned into a global public health issue.1 Most of the people who did not have appropriate knowledge about the dangers of non-prescribed antibiotic consumption (antibiotic misuse and other types of unnecessary use of antibiotics) can contribute to accelerating the process of antibiotic resistance.2 For example, the use of non-prescribed antibiotics for the treatment of viral infection (ie, influenza and common colds) is not an appropriate indication.3–5 Antibiotics consumed inappropriately by the people not only result in wastage of resources but also carry potential life-threatening severe adverse effects and the emergence of bacteria with extensive drug resistance;6,7 the reason behind this practice is the easy availability of antibiotics. Several studies reported that people from low and middle-income countries (LMICs) buy antibiotics easily without a proper prescription, and this is the most critical driver of antimicrobial overuse.8–11 Studies performed in LMICs showed that people mostly buy their antibiotics easily from pharmacies without a prescription.3,12,13 In addition to this, the most common reasons behind the frequent practice of self-medication with antibiotics (SMA) among the population of LMICs were prior good experience, easy availability of antibiotics, ignorance regarding the seriousness of the disease, and easily affordable in terms of time and money, knowledge of the antibiotics, and suggestions from others.4,11 All these issues encourage the population to use non-prescription antibiotics without medical consultation and this behavior can ultimately increase antibiotics resistance and SMA prevalence. Although the information regarding the prevalence and practices of SMA on sociodemographic factors have been described extensively in both developing and developed countries, such data on Malaysia is scarce. Furthermore, the studies previously performed in Malaysia14–16 were conducted several years ago, with self-administered questionnaires and this may cause bias in the reported results. In addition, these studies did not explore the reasons and predictors of SMA, which are critical for understanding such inappropriate behavior. It is necessary to conduct research regularly to understand the typical patterns associated with imprudent antibiotic utilization and also associated factors related to such use. Moreover, it is also necessary to conduct a study that can help government authorities in the formulation of strict policies to regulate inappropriate use of antibiotics and also help in the preparation of educational interventions and also define goals for future interventions to deal with SMA and its causes. So, the purpose of the present study was to determine the prevalence of SMA and to examine the sociodemographic factors that are associated with SMA. Furthermore, this study also explores common reasons and factors linked to SMA in Malaysia.
Methodology
Study Design and Settings
The current research adopted a cross-section study design, and the study was conducted in Kuala Lumpur (Malaysia) and Kuala Lumpur is the capital city of Malaysia and has an estimated population of 1.78 million, with an area of 243 km2.17
Study Population
The participants included in this study were adults willing to participate, without having any communication problems either due to illness or some other special reasons. As this study included lay people only (ie, people not having expert knowledge or professional qualifications in a particular subject),18 participants with a medical background such as doctors, pharmacists, nurses, and paramedical and allied health professionals were excluded from this study. The respondents or participants were selected through convenience and snowball sampling methods. Furthermore, this study only included those participants who were able to read and write Bahasa Melayu and English. This study was conducted in accordance with the Declaration of Helsinki.
Sample Size Calculation
Lorenz’s formula was used to calculate the sample size in the current study= n = z2 (p) × (q)/d2.19 At 95% confidence interval, the Z statistic value is 1.96, and P, pre-study estimates of self-medication (SM) prevalence was determined to be 0.5 from a previous study (as reported by Yama et al, 2018). Assuming a degree of precision (in the proportion of one, d = 0.05), and a 20% increase in final sample size to strengthen the results and the final sample size (n) was found to be 480 persons.
Study Instrument
The current study utilized a validated questionnaire that had been developed previously by study investigators and it included both open-ended and closed-ended questions.20 The questionnaire comprises 43 different questions with a total of 71 statements. The items in the questionnaire were grouped broadly into the following four categories: (i) sociodemographic characteristics of the participants (gender, age, marital status, education level, employment status, health care expense covered); (ii) personal information on health and medicine use (iii) practice towards SMA and factors contributing SMA and (iv) Public-reported outcomes. A forward and backward translation method was used for the translation of the English questionnaire into the Malay Language. The translated questionnaire was assessed for internal consistency (Cronbach alpha), reliability (test-retest reliability), face validity, and content validity. The questionnaire was also pilot tested on 100 people to determine questionnaire structure and clarity of language. After the pilot testing of the questionnaire, some necessary changes were highlighted, which were incorporated in the final version of the instrument.
Data Collection
The data was collected at public places, including shopping malls, supermarkets, public parks, buses, and metro stations. The final version of the questionnaire was used to collect data through the interview administered method from Feb 2019 to June 2019. A written signed informed consent form was taken from all participants who agreed to take part in this study. At the same time, an introductory letter was given to all respondents, which included a brief description of the study objectives and their importance. The data was collected through an interview administered questionnaire by trained interviewers. The confidentiality and anonymity of the participants were protected throughout the study.
Data Analysis
Data were entered and analyzed by using the Statistical Package for the Social Sciences (SPSS) version 24. Descriptive analysis, along with appropriate inferential statistics, were applied. Cross-tabulation was then carried out to look for a possible association between SMA and the independent variables. Multivariate Logistic regression was used to determine the predictors of SMA within the study population and in this analysis, the prevalence of SMA was considered as the outcome. Whereas, participant’s demographics were considered as exposure variables (gender, age, income, education, job type, and health insurance). Finally, univariate and multivariate logistic regression at 95% CI were computed. All factors which achieved a p-value of less than 0.05 at the univariate level were considered fit to be included in the multivariable model to determine the predictors SMA and statistical significance for all analyses was set at p < 0.05.
Ethical Approval
Before the data collection, ethical approval was sought for this from the Ethical Committee, International Islamic University Malaysia (reference number IREC 2019-004O).
Results
Sociodemographic Characteristics of the Study Participants
Four hundred and eighty adult participants were surveyed, 29.8% participants aged between 21–30, while 41.9% aged between 31–40 years and 28.3% of participants who were aged above 40 years. Whereas, 45.8% of participants polled male. The majority of participants belonged to the Malay community 46.7%. Only 2.3% of participants had completed primary education, 16.3% had gone through secondary school education, 30.4% had a diploma certificate, 42.1% had completed undergraduate degree/bachelor degree, while 9.0% had postgraduate degrees. 24.6% of participants had a monthly income of less than 3000 Malaysian Ringgit [RM] (US$ 720.70), while 39.2% had incomes in the range of 3000–5000 RM (US$720.7–1201.1) and 36.3% of participants had higher incomes than 5000 RM (US$ 1201.1). All sociodemographic characteristics were presented in Table 1.
Table 1.
Sociodemographic Characteristics of Study Participants
| Variables | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Male | 220 | 45.8% |
| Female | 260 | 54.2% |
| Age (Years) | Frequency | Percentage |
| 21–25 | 49 | 10.2% |
| 26–30 | 94 | 19.6% |
| 31–40 | 201 | 41.9% |
| Above 40 | 136 | 28.3% |
| Race | Frequency | Percentage |
| Malay | 224 | 46.7% |
| Chinese | 109 | 22.7% |
| Tamil | 51 | 10.6% |
| Others | 96 | 20% |
| Marital status | Frequency | Percentage |
| Single | 155 | 32.3% |
| Married | 325 | 67.7% |
| Education | Frequency | Percentage |
| Primary school | 11 | 2.3% |
| Secondary school | 78 | 16.2% |
| Certificate/Diploma | 146 | 30.4% |
| Undergraduate degree/Bachelor degree | 202 | 42.1% |
| Postgraduate education | 43 | 9.0% |
| Household monthly income | Frequency | Percentage |
| Under RM 3000 | 118 | 24.6% |
| RM 3000–5000 | 188 | 39.2% |
| Over RM 5000 | 174 | 36.3% |
| Health Insurance | Frequency | Percentage |
| Yes | 227 | 47.3% |
| No | 186 | 38.7% |
| Not sure | 67 | 14% |
| Occupation | Frequency | Percentage |
| Professional | 56 | 11.7% |
| Skilled labour | 16 | 3.3% |
| Manual labour | 80 | 16.7% |
| Administrative | 76 | 15.8% |
| Self-employed | 124 | 25.8% |
| Home duties | 5 | 1.0% |
| Unemployed | 112 | 23.4% |
| Pensioner | 10 | 2.1% |
| Others | 1 | 0.2% |
Frequency of Antibiotics Consumption in Past and Their Source of Information
Results showed that 13.5% of participants used antibiotics in the last month, 23.1% of participants indicated that they used antibiotics at least once in the last six months, 17.7% of participants used antibiotics last year and 11% of participants used antibiotics more than a year ago. At the same time, 24.4% of participants said that they did not remember when they used antibiotics the last time. Furthermore, 51% of participants claimed that they got advice from a doctor, pharmacist, or nurse on how to take them. While 40.4% of participants indicate that they did not get any advice from them and 36% did not remember any details about this.
Reliability
Internal Consistency
Internal consistency was determined for practice towards SMA and factors contributing to SMA and Cronbach’s alpha value was 0.90. While Cronbach’s alpha for the public-reported outcomes domain was 0.670.
Test-Retest Reliability
Results obtained from the test-retest analysis indicate satisfactory reliability and stability. For domain practice towards SMA and factors contributing SMA and public-reported outcomes were 0.891, and 0.787 respectively (p < 0.05).
Prevalence of SMA and Common Sources of Antibiotics
The prevalence of SMA concerning demographic characteristics was reported in Table 2. The overall prevalence of SMA was 15.1%. The rate of SMA was higher in males (8.8%) as compared to females (6.3%). Regarding age distribution, the highest prevalence was among the age groups of 31–40 years old (7.9%) followed by people aged above 40 years (3.5%), and then by people aged between 26–30 years old (2.3%). In contrast, the lowest prevalence of SMA was noted in the younger age group 21–25 years old, where only 1.3% of participants obtained antibiotics without prescription.
Table 2.
Prevalence of SMA
| Characteristics | Prevalence of SMA | P-value | ||
|---|---|---|---|---|
| Gender | Antibiotics without prescription | Antibiotics with prescription | Cannot remember | 0.051* |
| Male | 42 (8.8%) | 97 (20.2%) | 81 (16.9%) | |
| Female | 30 (6.2%) | 135 (28.1%) | 95 (19.8%) | |
| Age (years) | Antibiotics without prescription | Antibiotics with prescription | Cannot remember | P-value |
| 21–25 | 6 (1.2%) | 25 (5.2%) | 18 (3.8%) | 0.293 |
| 26–30 | 11 (2.3%) | 43 (9%) | 40 (8.3%) | |
| 31–40 | 38 (7.9%) | 89 (18.5%) | 74 (15.4%) | |
| Above 40 | 17 (3.5%) | 75 (15.6%) | 44 (9.2%) | |
| Race | Antibiotics without prescription | Antibiotics with prescription | Cannot remember | P-value |
| Malay | 35 (7.3%) | 114 (23.8%) | 75 (15.6%) | 0.799 |
| Chinese | 16 (3.3%) | 55 (11.5%) | 38 (7.9%) | |
| Tamil | 4 (0.8%) | 22 (4.6%) | 25 (5.2%) | |
| Others | 17 (3.5%) | 41 (8.5%) | 38 (7.9%) | |
| Income | Antibiotics without prescription | Antibiotics with prescription | Cannot remember | P-value |
| Under 3000 | 23 (4.8%) | 51 (10.6%) | 44 (9.2%) | 0.327 |
| 3000 to 5000 | 28 (5.8%) | 88 (18.3%) | 72 (15%) | |
| Above 5000 | 21 (4.4%) | 93 (19.4%) | 60 (12.5%) | |
| Education | Antibiotics without prescription | Antibiotics with prescription | Cannot remember | P-value |
| Primary school | 1 (0.2%) | 4 (0.8%) | 6 (1.3%) | 0.001*** |
| Secondary school | 10 (2.1%) | 39 (8.1%) | 29 (6%) | |
| Certificate/Diploma | 36 (7.5%) | 63 (13.1%) | 47 (9.8%) | |
| Undergraduate degree | 21 (4.4%) | 99 (20.6%) | 82 (17.1%) | |
| Postgraduate education | 4 (0.8%) | 27 (5.6%) | 12 (2.5%) | |
| Marital status | Antibiotics without prescription | Antibiotics with prescription | Cannot remember | P-value |
| Married | 55 (11.5%) | 160 (33.3%) | 110 (22.9%) | 0.284 |
| Single | 17 (3.6%) | 72 (14.9%) | 66 (13.8%) | |
| Health Insurance | Antibiotics without prescription | Antibiotics with prescription | Cannot remember | P-value |
| No | 48 (10%) | 75 (15.6%) | 63 (13.1%) | 0.001*** |
| Yes | 22 (4.6%) | 128 (26.7%) | 77 (16%) | |
| Occupation | Antibiotics without prescription | Antibiotics with prescription | Cannot remember | P-value |
| Professional | 7 (1.5%) | 34 (7.1%) | 15 (3.1%) | 0.009** |
| Skilled labour | 4 (0.8%) | 5 (1%) | 7 (1.5%) | |
| Manual labour | 18 (3.8%) | 28 (5.8%) | 34 (7.1%) | |
| Administrative | 11 (2.3%) | 40 (8.3%) | 25 (5.2%) | |
| Self-employed | 23 (4.8%) | 60 (12.5%) | 41 (8.5%) | |
| Home duties | 2 (0.4%) | 2 (0.4%) | 1 (0.2%) | |
| Unemployed | 6 (1.3%) | 55 (11.5%) | 51 (10.6%) | |
| Pensioner | 1 (0.2%) | 8 (1.7%) | 1 (0.2%) | |
| Others | Nil | Nil | 1 (0.2%) | |
Notes: p<0.05 Significant; While ***p < 0.001, **p < 0.01, * p < 0.05.
A notable difference was also seen among married participants 11.5% and unmarried participants 3.6%. The factor that was significantly associated with SMA was education level (p=0.001), occupation (p=0.009) and the presence of health insurance (p=0.001). Other sociodemographic characteristics, such as gender, age, race, income, and marital status were not significantly associated with the SMA. Moreover, 64.8% of participants indicated that they bought their antibiotics from pharmacies. Whereas, other common sources included stall/hawker, internet and friend/family, and relatives, 2.1%, 1.3%, 3.1%, respectively. Only 3.3% of participants utilized leftover antibiotics; they saved these antibiotics from their previous prescription.
Frequently Used Antibiotics and Common Reasons for SMA
Out of 480 participants, 20.6% indicated that they always use amoxicillin-clavulanate antibiotic if ever they have a cough or cold, runny nose, either flu or sore throat, diarrhea or fever followed by ampicillin/cloxacillin 14.2% and levofloxacin 8.3%. While metronidazole, ampicillin, ciprofloxacin, moxifloxacin, erythromycin, azithromycin, tetracycline, ceftriaxone, and doxycycline were used by a small number of participants scoring 6.9%, 5%, 4.8%, 4%, 3.8%, 2.9%, 2.3%, 1.5%, and 1% respectively. The most common reasons for SMA were highlighted in Figure 1. Results showed that 19.2% of participants did not go to see doctors when they were sick because of the high cost either for medicine or checkup. While 7.3% of participants stated that they face difficulties in communication with doctors and 11.3% said that they face difficulties in transportation to health clinics or hospitals. At the same time, 6.3% said that they do not implicitly trust doctors and 23.1% of participants said that they do not have enough time to visit doctors.
Figure 1.
Common reasons for self-medication with antibiotics.
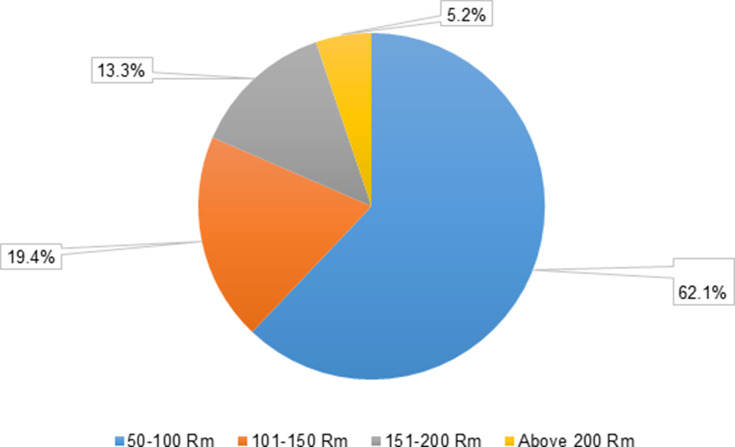
Money-Saving
Figure 2 presents how much money participants were saving at one time while purchasing antibiotics. According to the results, the majority of the participants (62.1%), saved RM 50–100 as compared to participants (5.2%) who saved above RM 200. While 13.3% of participants saved 151–200, and 19.4% of participants saved 101–151 RM.
Figure 2.
Saving of money in one time in Malaysian Ringgit (RM).
Knowledge, Attitude, and Practice of the Respondents
Less than half (48.3%) of participants completed their course of treatment as recommended and 31.7% stopped it when they felt better. Whereas, 40.6% of participants had indicated that it’s okay to use antibiotics that were given to a friend or family member if they were used to treat the same illness regardless of the outcome. More than half of the study participants (51.5%) wrongly identified that antibiotics can be used to treat cold and flu. While 57.7% believed that antibiotics are used to treat fever followed by the sore throat (41.5%), skin or wound infection (27.7%, diarrhea (27.3%) and body aches (22.3%), etc. (Table 3).
Table 3.
The Participant’s Responses Regarding the Knowledge and Attitude Questions
| Questions | Frequency | Percentage |
|---|---|---|
| Q. When do you think you should stop taking antibiotics once you have begun treatment? | ||
| When I feel better | 152 | 31.7% |
| When I have taken all the antibiotics as directed | 232 | 48.3% |
| Do not know | 96 | 20% |
| Q. It is okay to use antibiotics that were given to a friend or family member if they were used to treat the same illness | ||
| Yes | 195 | 40.6% |
| No | 178 | 37.1% |
| Do not know | 107 | 22.3% |
| Q. It is okay to buy the same antibiotics, or request the same antibiotics from a doctor if I am sick and they helped me get better when I had the same symptoms before | ||
| Yes | 169 | 35.2% |
| No | 180 | 37.5% |
| Do not know | 131 | 27.3% |
| Q. Do you think these conditions can be treated with antibiotics? (Mark more than one if applicable) | ||
| HIV/AIDS | 63 | 13.1% |
| Gonorrhea | 54 | 11.3% |
| Bladder or UTI | 93 | 19.4% |
| Diarrhea | 131 | 27.3% |
| Cold and Flu | 247 | 51.5% |
| Fever | 277 | 57.7% |
| Malaria | 76 | 15.8% |
| Measles | 44 | 9.2% |
| Skin or wound infection | 133 | 27.7% |
| Sore throat | 199 | 41.5% |
| Body aches | 107 | 22.3% |
| Headaches | 77 | 16.0% |
Predictors of SMA
Being male (adjusted OR=0.513; 95% CI: 0.300–0.877), unemployed (adjusted OR = 1.146; 95% CI: 0.122–10.797) with no health insurance (adjusted OR=0.108; 95% CI: 0.025–0.472) and having low education (adjusted OR = 0.259; 95% CI: 0.084–0.800) were more likely to use antibiotics for self-medication. All the results of multivariate logistic regression analysis of predictors of SMA were mention in Table 4.
Table 4.
Multivariate Logistic Regression Analysis of Predictors of SMA
| Variable | COR (CI 95%) | P-value | AOR (CI 95%) | P-value |
|---|---|---|---|---|
| Gender | ||||
| Male | 0.513 (0.300–0.877) | 0.015** | 0.502 (0.269–0.935) | 0.030* |
| Female | Ref | Ref | ||
| Income | COR (CI 95%) | P-value | AOR (CI 95%) | P-value |
| Under 3000 | 0.501 (0.253–0.991) | 0.047* | 0.849 (0.371–1.945) | 0.699 |
| 3000 to 5000 | 0.710 (0.376–1.341) | 0.291 | 1.416 (0.573–2.978) | 0.359 |
| Above 5000 | Ref | Ref | ||
| Health insurance | COR (CI 95%) | P-value | AOR (CI 95%) | P-value |
| No | 0.108 (0.025–0.472) | 0.003** | 0.136 (0.029–0.649) | 0.012** |
| Yes | 0.401 (0.89–1.803) | 0.234 | 0.404 (0.083–1.958) | 0.260 |
| Not-sure | Ref | Ref | ||
| Occupation | COR (CI 95%) | P-value | AOR (CI 95%) | P-value |
| Professional | 0.607 (0.065–5.660) | 0.661 | 0.699 (0.60621–8.024) | 0.773 |
| Skilled labour | 0.156 (0.013–1.828) | 0.139 | 0.299 (0.020–4.454) | 0.381 |
| Manual labour | 0.194 (0.022–1.689) | 0.138 | 0.349 (0.032–3.822) | 0.389 |
| Administrative | 0.455 (0.051–4.034) | 0.479 | 0.528 (0.048–5.765) | 0.600 |
| Self-employed | 0.326 (0.039–2.754) | 0.303 | 0.570 (0.057–5.707) | 0.633 |
| Home duties | 0.125 (0.007–2.176) | 0.154 | 0.178 (0.008–3.968) | 0.276 |
| Unemployed | 1.146 (0.122–10.797) | 0.051* | 1.203 (0.105–13.834) | 0.058* |
| Pensioner | Ref | Ref | ||
| Age | COR (CI 95%) | P-value | AOR (CI 95%) | P-value |
| 21–25 | 0.944 (0.336–2.659) | 0.914 | 0.771 (0.231–2.576) | 0.673 |
| 26–30 | 0.886 (0.380–2.065) | 0.779 | 0.617 (0.231–1.643) | 0.334 |
| 31–40 | 0.531 (0.277–1.016) | 0.056* | 0.555 (0.264–1.166) | 0.120 |
| Above 40 | Ref | Ref | ||
| Education | COR (CI 95%) | P-value | AOR (CI 95%) | P-value |
| Primary school | 0.593 (0.052–7.731) | 0.673 | 1.770 (0.0.121–25.990) | 0.677 |
| Secondary school | 0.578 90.164–2.035) | 0.393 | 0.888 (0.208–3.787) | 0.827 |
| Certificate/Diploma | 0.259 (0.084–0.800) | 0.019** | 0.429 (0.110–1.673) | 0.023* |
| Undergraduate degree | 0.698 (0.221–2.208) | 0.541 | 0.868 (0.238–3.163) | 0.830 |
| Postgraduate education | Ref | Ref | ||
Notes: **p < 0.01, *p < 0.05.
Abbreviations: AOR, Adjusted Odd’s Ratio; CI, confidence interval; COR, Crude Odd’s Ratio; Ref, Reference category.
Public Reported Outcome
In this part of the study, several questions were asked from participants to estimate their experience on the outcomes after taking antibiotics. A slightly greater than one-quarter of participants (32.9%) indicated that they will use antibiotics without prescription in the future if the same symptoms of a disease appear again. While 49.5% said that they will not utilize antibiotics in the future if the same symptoms appear, and only 20.6% were not sure about this. Gender, income, duration of stay in Malaysia, place of birth, and ethnicity were the characteristics that showed a significant association (p= 0.001) with future use of SMA (participants said yes, “we will use antibiotics in future without a prescription”). On the other hand, the male gender (20.4%) was most prone towards SMA in the future as compared to females (12.5%). While the participants who were the local residents (34.6%) and participants whose income (22.9%) was above 5000 Rm said ‘no” they will not utilize antibiotics without prescription in the future.
Overall 81.6% of participants indicated that after taking antibiotics they feel better and whereas 2.3% of participants indicated that their symptoms become worse. While 37.32% of participants admitted that treating their symptoms with SMA antibiotics proves economical and interestingly 33.8% were “not sure” about this. Furthermore, 137 (28.2%) quoted “yes” and 37.8% quoted “no” recommendation of SMA for self-health care. While the rest (34%) of participants were unsure about this (Table 5).
Table 5.
Public Reported Outcomes
| Demographic Characteristic | Statement | ||||
|---|---|---|---|---|---|
| Do you plan to self-medicate again if the same symptoms will appear again in the future? | |||||
| Gender | Yes | No | Not sure | P-value | |
| Male | 98 (20.4%) | 85 (17.7%) | 37 (7.7%) | 0.001 | |
| Female | 60 (12.5%) | 138 (28.8%) | 62 (12.9%) | ||
| Ethnicity | Yes | No | Not sure | P-value | |
| Malay | 61 (12.7%) | 110 (22.9%) | 53 (11%) | 0.001 | |
| Chinese | 34 (7.1%) | 53 (11%) | 22 (4.6%) | ||
| Tamil | 10 (2.1%) | 32 (14.3%) | 9 (1.9%) | ||
| Others | 53 (11%) | 28 (5.8%) | 15 (3.1) | ||
| Income | Yes | No | Not sure | P-value | |
| Under 3000 RM | 45 (9.4%) | 33 (6.9%) | 39 (8.1%) | 0.001 | |
| 3000 to 50,000 RM | 75 (15.6%) | 80 (16.7%) | 33 (6.9%) | ||
| Over 50,000 RM | 38 (7.9%) | 110 (22.9%) | 27 (5.6%) | ||
| Education | Yes | No | Not sure | P-value | |
| Primary school | 4 (0.8%) | 4 (0.8%) | 3 (0.6%) | 0.033 | |
| Secondary school | 29 (6%) | 29 (6%) | 19 (4%) | ||
| Certificate/Diploma | 56 (11.7%) | 56 (11.7%) | 40 (8.3%) | ||
| Undergraduate degree | 62 (12.9%) | 111 (23.1%) | 29 (6%) | ||
| Postgraduate education | 12 (2.5%) | 23 (4.8%) | 8 (1.7%) | ||
| Place of Birth | Yes | No | Not sure | P-value | |
| Born in Malaysia | 84 (17.5%) | 166 (34.6%) | 72 (15%) | 0.001 | |
| Not Born in Malaysia | 74 (15.4%) | 57 (11.9%) | 27 (5.6%) | ||
| How do you evaluate your symptoms after taking antibiotics? | |||||
| Better | Worse | Same as before | |||
| 392 (81.6%) | 11 (2.3%) | 77 (16.1%) | |||
| Do you feel that treating your symptoms by yourself with antibiotics proves economical? | |||||
| Yes | No | Not sure | |||
| 179 (37.32%) | 139 (29%) | 162 (33.8%) | |||
| Do you feel that self-medication with antibiotics should be recommended for self-health care? | |||||
| Yes | No | Not sure | |||
| 135 (28.2%) | 182 (37.8%) | 163 (34%) | |||
Discussion
To the best of our knowledge, this is the first population-based study performed in Malaysia (Kuala Lumpur) examining the practices towards SMA. The prevalence rate among the general population was 15.1% and similar findings were also reported from another study carried out in Spain (15.2%).21 A study performed in Hungary reported less prevalence of SMA (7.8%).22 Whereas, previous studies performed in Kedah (50%) and Putrajaya (16.5%) (Malaysia) also showed a higher rate of SMA as compared to the current study.19,23 While studies carried out in developed countries including Macedonia (17.8%), Lithuania (31%), Poland (41.1%) showed a slightly higher prevalence rate when compared with the results of the current study.24–26 The low rate of SMA in Malaysia indicates a robust healthcare system in Malaysia. Results from the current study indicate that SMA is significantly associated with participant’s education level (P=0.001), health insurance (P=0.001), and job type (P=0.009). Whereas, findings from multivariate logistic analysis also found that males with a low level of education are most prone towards SMA. A study performed in Eritrea and Uganda also confirmed these findings.27,28 In the current study participants having lower education are most likely to use antibiotics without prescription. A study performed in France and Lebanon also confirmed that low education level has a significant impact on SMA.29,30 This low level of education leads people towards the misconception that cough or cold, runny nose, either flu or throat, diarrhea or fever treated through antibiotics, or antibiotics only, and the results from the current study confirmed that 20.6% of participants used amoxicillin when these symptoms appear. Studies performed in Saudi Arabia31 and Cameroon32 showed almost similar results, where amoxicillin was the most commonly chosen antibiotic by participants (22.3%, 26.4%, respectively). More than half of the participants from the current study claimed that they got advice from healthcare professionals (including pharmacists) about who to use antibiotics. So the pharmacist can play an important role to stop this inappropriate practice and a study performed in Hungary confirmed this finding.33 The majority of participants who previously utilized antibiotics with a prescription or without prescription obtained their antibiotics from a medical store or pharmacy. Results obtained from other studies performed in Mozambique, Malaysia, and Jordan showed that pharmacies serve as the most common source to get antibiotics without prescription.34–36 The results of the current study also indicate that cost is the most common reason for SMA and these findings are consistent with other studies performed in Saudi Arabia, Jordan, and Pakistan, where SMA among adult populations was significantly associated with financial constraints.3,37,38 When the right time to stop taking antibiotics was studied, it was noted that 31.7% of participants were most likely to stop taking antibiotics when they felt better. This finding is consistent with another study conducted in Jordan and results from this study showed that 32% of the respondents who used antibiotics but did not complete the recommended course of treatment.39 While another study performed in Sindh (Pakistan) also reported that more than two-thirds (74.7%) of the study population had no idea about the possible inadequate use of antibiotics.38 Results from these studies showed that such kind of bad practices or malpractice including non-compliance led to the spread of resistant pathogens, which can be countered by the appropriate or rational use of antibiotics. Furthermore, more than half of the participants from the current study (51.5%) wrongly identified that antibiotics can be used to treat colds and flu. Studies performed in Penang and Putrajaya (Malaysia) reported that more than 80% of participants misunderstood that antibiotics can treat viral infections.19,23 Another study performed in Poland revealed that 40% of participants believed that antibiotics can be used to treat flu.40 The last part of the study consists of public reported outcomes. In this part, participants answered several questions specially designed to estimate their thoughts after taking antibiotics. Interestingly, 32.9% of participants said they would utilize antibiotics in the future, and this rate is higher than the original SMA rate. Future use of antibiotics for self-medication is significantly associated with the participants’ gender (P=0.001), income (P=0.001), duration of stay in Malaysia (P=0.001), place of birth (P=0.001), and ethnicity (P=0.009). Males are most likely to resort to SMA in the future as compared to females. Results also showed that future use of antibiotics was associated with low income, and participants thought that treating their symptoms/illness with non-prescription antibiotics proved economical. A higher percentage of participants were agreed that their symptoms become better after taking antibiotics.
The limitations of the study must be taken into consideration. Data were collected during the daytime in different public places, including malls, supermarkets, parks, and from outside of hospitals, where mostly young male and female abundance is higher at this time. Thus, a higher number of young participants were included in this study. In addition to this, data was collected through face-to-face interviews using a validated questionnaire and people were usually reluctant to admit wrong practices (social desirability bias).
Conclusion
Results indicate that despite the strict antibiotic policy, people still using antibiotics and in addition to this, more people are planning to do SMA in the future. At the same time, people with a low level of education are at risk of using antibiotics without prescription, therefore, health policymakers should implement awareness programs to educate people about the implications of SMA. The majority of the population who used antibiotics for themself buy their antibiotics from pharmacies, so health authorities should restrict the over-the-counter (OTC) availability of antibiotics. Given the growing global resistance to antibiotics and other health issues linked to the improper use of antibiotics, findings from this study have suggested major public health policy implications from concerned authorities. To make the lay public more aware the WHO organizes antibiotics awareness days and the aims of this are to increase the awareness of global antimicrobial resistance and to encourage best practices among the general public. So by following the WHO guidelines by the concerned health authorities and policymakers to develop new policies to avoid the further emergence and spread of drug-resistant infections. Lastly, policymakers should also consider the structural problems pointed out in this study, including self-medication which is a result of easy availability or accessibility, and practices around sharing medications which is potentially a result of self-diagnosis and misinformation at the level of the supplier, be this at the hospital or pharmacy. Moreover, the study highlights that more multi-center, well-designed prospective research studies along with in-depth studies are urgently required to confirm the issue and to find the exact reasons behind SMA.
Abbreviations
SMA, Self-medication with antibiotics; OTC, Over the counter; WHO, World Health Organization.
Data Sharing Statement
The anonymized datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
AD, SIA, and MG collected and analyzed the data, and wrote the manuscript. CSZ, SJ and NSBR conceptualized and designed the study, guided data analysis and interpretation, and critically reviewed the manuscript. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declared no potential conflicts of interest for this work, nor concerning the research, authorship, and publication of this article.
References
- 1.WHO. Antibiotic resistance; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance. Accessed August 31, 2021.
- 2.Cambaco O, Menendez YA, Kinsman J, et al. Community knowledge and practices regarding antibiotic use in rural Mozambique: where is the starting point for prevention of antibiotic resistance? BMC Public Health. 2020;20(1):1–15. doi: 10.1186/s12889-020-09243-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nusair MB, Al‐azzam S, Alhamad H, Momani MY. The prevalence and patterns of self‐medication with antibiotics in Jordan: a community‐based study. Int J Clin Pract. 2021;75(1):e13665. doi: 10.1111/ijcp.13665 [DOI] [PubMed] [Google Scholar]
- 4.Nepal G, Bhatta S. Self-medication with antibiotics in WHO Southeast Asian Region: a systematic review. Cureus. 2018;10(4):e2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mukattash TL, Alkhatatbeh MJ, Andrawos S, Jarab AS, AbuFarha RK, Nusair MB. Parental self-medication of antibiotics for children in Jordan. J Pharm Health Serv Res. 2020;11(1):75–80. [Google Scholar]
- 6.Shehadeh M, Suaifan G, Darwish RM, Wazaify M, Zaru L, Alja’fari S. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J. 2012;20(2):125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gajdács M, Bátori Z, Ábrók M, Lázár A, Burián K. Characterization of resistance in gram-negative urinary isolates using existing and novel indicators of clinical relevance: a 10-year data analysis. Life (Basel, Switzerland). 2020;10:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harbarth S, Samore M. Antimicrobial resistance determinants and future control. Emerg Infect Dis. 2005;11(6):794–801. doi: 10.3201/eid1106.050167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Bakri AG, Bustanji Y, Yousef A. Community consumption of antibacterial drugs within the Jordanian population: sources, patterns and appropriateness. Intel J Antimicrob Agents. 2005;26(5):389–395. doi: 10.1016/j.ijantimicag.2005.07.014 [DOI] [PubMed] [Google Scholar]
- 10.Berzanskyte A, Valinteliene R, Haaijer-Ruskamp F, Gurevicius R, Lj G. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. 2006;19(4):246–253. [DOI] [PubMed] [Google Scholar]
- 11.Aslam A, Gajdács M, Zin CS, et al. Evidence of the practice of self-medication with antibiotics among the lay public in low-and middle-income countries: a scoping review. Antibiotics. 2020;9(9):597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torres NF, Solomon VP, Middleton L. Patterns of self-medication with antibiotics in Maputo City: a qualitative study. Antimicrob Resist Infect Control. 2019;8(1):1–12. doi: 10.1186/s13756-019-0618-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auta A, Hadi MA, Oga E, et al. Global access to antibiotics without prescription in community pharmacies: a systematic review and meta-analysis. J Infect. 2019;78(1):8–18. doi: 10.1016/j.jinf.2018.07.001 [DOI] [PubMed] [Google Scholar]
- 14.Oh AL, Hassali MA, Al-Haddad MS, Sulaiman S, Shafie AA, Awaisu A. Public knowledge and attitudes towards antibiotic usage: a cross-sectional study among the general public in the state of Penang, Malaysia. J Infect Dev Ctries. 2011;5(05):338–347. [DOI] [PubMed] [Google Scholar]
- 15.Lim KK, Teh CC. A cross sectional study of public knowledge and attitude towards antibiotics in Putrajaya, Malaysia. South Med Rev. 2012;5(2):26–33. [PMC free article] [PubMed] [Google Scholar]
- 16.Ying TJ, Zainal ZA, Wahab IA, Zamri F, Huri HZ. Knowledge, attitude and self-medication practice on antibiotic use amongst general public in AlorSetar, Kedah, Malaysia. Madridge J Pharm Res. 2018;1(3):40–46. doi: 10.18689/mjpr-1000107 [DOI] [Google Scholar]
- 17.Department of Statistics M. Federal Territory of Kuala Lumpur; 2019. Available form: https://www.dosm.gov.my/v1/index.php?r=column/cone&menu_id=bjRlZXVGdnBueDJKY1BPWEFPRlhIdz09. Accessed December 1, 2020.
- 18.Oxford Dictionary learners dictionary; 2020. Available from: https://www.oxfordlearnersdictionaries.com/definition/english/layperson?q=layperson. Accessed December 1, 2020.
- 19.Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35(2):121. doi: 10.4103/0253-7176.116232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aslam A, Gajdács M, Zin CS, Binti Abd Rahman NS, Ahmed SI, Jamshed SQ. Public awareness and practices towards self-medication with antibiotics among the Malaysian population. A development of questionnaire and pilot-testing. Antibiotics (Basel). 2020;9(2):97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guinovart MC, Figueras A, Llop JC, Llor C. Obtaining antibiotics without prescription in Spain in 2014: even easier now than 6 years ago. J Antimicrob Chemother. 2015;70(4):1270–1271. [DOI] [PubMed] [Google Scholar]
- 22.Gajdács M, Paulik E, Szabó AJAPH. Public knowledge, attitude and practices towards antibiotics and antibiotic resistance: a cross-sectional study in Szeged District, Hungar. Antibiotics (Basel). 2020;90(1):5–14. [Google Scholar]
- 23.OH LA, Hassali MA, Al-Haddad MS, Syed Sulaiman SA, Shafie AA, Awaisu A. Public knowledge and attitudes towards antibiotic usage: a cross-sectional study among the general public in the state of Penang, Malaysia. J Infect Dev Ctries. 2011;5(5):338–347. doi: 10.3855/jidc.1502 [DOI] [PubMed] [Google Scholar]
- 24.Pavydė E, Veikutis V, Mačiulienė A, Mačiulis V, Petrikonis K, Stankevičius E. Public knowledge, beliefs and behavior on antibiotic use and self-medication in Lithuania. Int J Environ Res Public Health. 2015;12(6):7002–7016. doi: 10.3390/ijerph120607002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ivanovska V, Zdravkovska M, Bosevska G, Angelovska B. Antibiotics for upper respiratory infections: public knowledge, beliefs and self-medication in the Republic of Macedonia. Pril. 2013;34(2):59–70. [PubMed] [Google Scholar]
- 26.Muras M, Krajewski J, Nocun M, Godycki-Cwirko M. A survey of patient behaviours and beliefs regarding antibiotic self-medication for respiratory tract infections in Poland. Arch Med Sci. 2013;9(5):854–857. doi: 10.5114/aoms.2012.29217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ateshim Y, Bereket B, Major F, et al. Prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea: a descriptive cross sectional survey. BMC Public Health. 2019;19(1):726. doi: 10.1186/s12889-019-7020-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ocan M, Bwanga F, Bbosa GS, et al. Patterns and predictors of self-medication in northern Uganda. PLoS One. 2014;9(3):e92323. doi: 10.1371/journal.pone.0092323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jamhour A, El-Kheir A, Salameh P, Hanna PA, Mansour H. Antibiotic knowledge and self-medication practices in a developing country: a cross-sectional study. Am J Infect Control. 2017;45(4):384–388. doi: 10.1016/j.ajic.2016.11.026 [DOI] [PubMed] [Google Scholar]
- 30.Demoré B, Mangin L, Tebano G, Pulcini C, Thilly N. Public knowledge and behaviours concerning antibiotic use and resistance in France: a cross-sectional survey. Infection. 2017;45(4):513–520. doi: 10.1007/s15010-017-1015-2 [DOI] [PubMed] [Google Scholar]
- 31.Al Rasheed A, Yagoub U, Alkhashan H, et al. Prevalence and predictors of self-medication with antibiotics in Al Wazarat Health Center, Riyadh City, KSA. Biomed Res Intel. 2016;2016. doi: 10.1155/2016/3916874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ngu RC, Feteh VF, Kika BT, et al. Prevalence and determinants of antibiotic self-medication among adult patients with respiratory tract infections in the Mboppi Baptist Hospital, Douala, Cameroon: a cross-sectional study. Diseases (Basel, Switzerland). 2018;6:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gajdács M, Paulik E, Szabó A. Knowledge, attitude and practice of community pharmacists regarding antibiotic use and infectious diseases: a cross-sectional survey in Hungary (KAPPhA-HU). Antibiotics (Basel). 2020;9(2):41. doi: 10.3390/antibiotics9020041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jawahir S, Aziz NA. Self-medication among adult population in Selangor, Malaysia. Intel J Pharm Pharm Sci. 2017;9(5):268–274. doi: 10.22159/ijpps.2017v9i5.16445 [DOI] [Google Scholar]
- 35.Sawair FA, Baqain ZH, Abu Karaky A, Abu Eid R. Assessment of self-medication of antibiotics in a Jordanian population. Med Princ Pract. 2009;18(1):21–25. doi: 10.1159/000163041 [DOI] [PubMed] [Google Scholar]
- 36.Torres NF, Solomon VP, Middleton LE. Pharmacists’ practices for non-prescribed antibiotic dispensing in Mozambique. Pharm Pract (Granada). 2020;18(3):1965. doi: 10.18549/PharmPract.2020.3.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alghadeer S, Aljuaydi K, Babelghaith S, Alhammad A, Alarifi MN. Self-medication with antibiotics in Saudi Arabia. Saudi Pharm J. 2018;26(5):719–724. doi: 10.1016/j.jsps.2018.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bilal M, Haseeb A, Khan MH, et al. Self-medication with antibiotics among people dwelling in rural areas of Sindh. JCDR. 2016;10(5):Oc08–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yusef D, Babaa AI, Bashaireh AZ, et al. Knowledge, practices & attitude toward antibiotics use and bacterial resistance in Jordan: a cross-sectional study. Infect Dis Health. 2018;23(1):33–40. doi: 10.1016/j.idh.2017.11.001 [DOI] [PubMed] [Google Scholar]
- 40.Mazińska B, Strużycka I, Hryniewicz W. Surveys of public knowledge and attitudes with regard to antibiotics in Poland: did the European Antibiotic Awareness Day campaigns change attitudes? PLoS One. 2017;12(2):e0172146. doi: 10.1371/journal.pone.0172146 [DOI] [PMC free article] [PubMed] [Google Scholar]