Abstract
Objective:
The aim of this study was to evaluate the initial impact of the COVID-19 pandemic on individuals with systemic lupus erythematosus (SLE).
Methods:
Patients with SLE participating in a multi-center longitudinal cohort study in New York and Boston were invited to complete a supplemental web-based questionnaire in the summer of 2020. Participants completed standardized patient-reported outcome (PRO) measures and a combination of Likert scale and open-ended questions exploring the impact of the COVID-19 pandemic on their health and access to health care. Changes in PROs were evaluated with paired t-tests and frequencies of worsened symptoms were calculated. A thematic qualitative analysis was conducted on free text responses.
Results:
Of 97 patients invited, 63 (65%) completed a supplemental questionnaire. Nearly 50% of respondents exhibited increases in anxiety (47.5%) and depression (48.3%) and over 40% scored worse in measures of pain interference, fatigue, and cognitive abilities. Respondents with pre-existing diagnoses of anxiety did not differ from other participants in PRO scores, but were more than three times as likely to report worsened health status. Patients denied difficulties accessing medications (85%) or medical care (84%) and over 50% participated in telehealth visits. Anxiety and increased health risks due to immunosuppression were recurring themes in free text responses.
Conclusions:
SLE patients experienced a significant physical and emotional toll in the initial months of the COVID-19 pandemic. Comprehensive patient-centered care, including monitoring and addressing anxiety and health-related quality of life, is critical to improving health outcomes in this population during the ongoing health crisis.
Keywords: systemic lupus erythematosus, COVID-19, patient reported outcomes, anxiety, telemedicine
Introduction
The COVID-19 pandemic has had a profound impact on physical and emotional health with uncertainty and isolation fueling a parallel epidemic of fear, anxiety, and depression(1). Individuals with systemic lupus erythematosus (SLE), a chronic autoimmune condition, are particularly vulnerable to pandemic-related physical and emotional distress. SLE patients face prognostic uncertainty in the setting of their underlying immunosuppression and have high rates of comorbid mood disorders, including anxiety. Perceived stress, anxiety, and depression have been associated with an increased burden of SLE symptoms, greater disease activity, and worse outcomes(2-5). Disruption of health care services and shortages of hydroxychloroquine, the linchpin of most SLE treatment regimens, may have had additional adverse effects on this medically complex population.
To date little is known about the impact of the COVID-19 pandemic on individuals with SLE. Understanding the experiences of these patients and their perceptions of health, health-related quality of life, and access to health care during the pandemic is necessary to inform comprehensive patient-centered approaches to addressing the sequelae of this public health crisis.
The objective of this study was to evaluate the impact of the first wave of the COVID-19 pandemic on individuals with SLE. We investigated changes in standardized patient-reported outcomes (PROs) and queried the experiences of SLE patients living in New York City and Boston, two major metropolitan areas with high COVID-19 rates early in the pandemic.
Materials and Methods
Population:
The study population was derived from participants in a multi-center longitudinal cohort study of the clinical implementation of PRO measures in outpatient SLE care. English-speaking patients aged 18 years or older who met 1997 American College of Rheumatology SLE criteria and received ongoing care at Tufts Medical Center (TMC) in Boston, MA or the Hospital for Special Surgery (HSS) in New York, NY were invited to enroll in the cohort at the time of clinic visits between February and August 2019. The overall cohort had an enrollment rate of 88% and was representative of the diverse population of SLE outpatients cared for at both centers, with declining patients not differing from participants with regard to socio-demographic or SLE characteristics. Participants in the cohort completed web-based PRO measures as part of routine outpatient clinical encounters and were included in this analysis if they responded to a supplemental COVID-19 questionnaire, along with repeat PRO measures, in July or August 2020. The study was reviewed and approved by the Tufts Health Sciences Institutional Review Board (IRB# 13159).
Data Collection:
Socio-demographic information, including age, sex, race, ethnicity, insurance type, and disability status, co-morbidities, and baseline PRO measures and SLE disease duration, activity, and related damage were collected at the time of enrollment in the cohort. Disease activity and damage were measured by treating physicians with the Safety of Estrogens in Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index (SELENA-SLEDAI) and the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index (SLICC/ACR-DI) respectively(6,7). PROs were measured with Patient-Reported Outcome Measurement Information System (PROMIS®) Computerized Adaptive Tests (CATs), which are normalized around a general population mean T-score of 50 and have demonstrated validity in outpatients with SLE.(8) PROMIS CATs included were physical function, pain interference, fatigue, ability to participate in social roles and activities, applied cognition-abilities, sleep disturbance, anxiety, depression, and self-efficacy for managing chronic conditions--manage medications/treatment.
In July 2020, participants were contacted by research staff by phone and/or email and invited to complete a supplemental COVID-19 survey exploring their experience in the early months of the pandemic. The supplemental survey included a questionnaire exploring the impact of the pandemic on SLE patients’ health, access to medications, and access to health care through a combination of Likert-scale and open-ended questions. Participants were asked about their telemedicine experiences with questions adapted from the Telehealth Usability Questionnaire(9). They were also asked to repeat all PROMIS CATs done at the time of enrollment in the cohort and to complete an additional PROMIS CAT assessing social isolation that was not included with the initial surveys.
All study questionnaires were in English. Patients were emailed a link to the web-based survey, which was then completed remotely. Surveys were administered using REDCap, an electronic data capture system hosted by the Tufts Clinical and Translational Science Institute.
Quantitative Analysis:
Descriptive statistics were reported for demographic and clinical variables. Differences between COVID-19 questionnaire respondents and non-respondents were assessed with t-tests for continuous variables and chi-squared tests for categorical variables. Changes in PROMIS scores were evaluated with paired t-tests. In addition, frequencies of score changes of 3 or more points were calculated. A T-score change of 2 to 3 points has been shown to be the minimal important difference in several PROMIS domains(10-12). Differences in clinical and socio-demographic characteristics among those with and without clinically meaningful increases in anxiety, defined as T-score changes of 5 or more,(13) were examined with univariate analyses (t-tests and chi-squared or Fisher’s exact tests). We conducted a sub-group analysis of PROMIS score changes and COVID-19 questionnaire responses in participants with and without baseline self-reported diagnoses of anxiety using t-tests and Fisher’s exact tests respectively. All statistical analyses were performed with SAS version 9.4 (Cary, NC).
Qualitative Analysis:
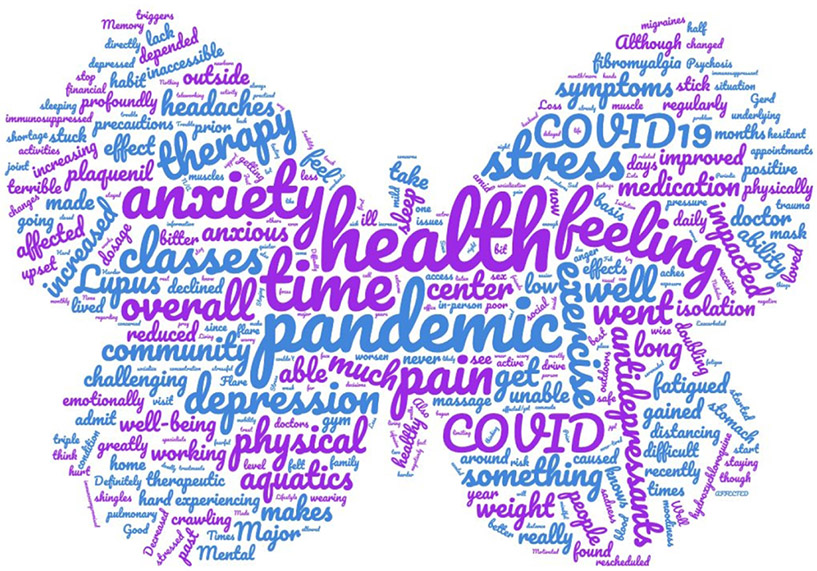
Free-text responses were independently reviewed and coded by two authors (SK, VP). They met to review and refine codes and performed a thematic analysis organizing codes into salient themes. A word cloud, in which the relative size of each word represents the frequency with which it appeared in the free-text responses, was created using Wordclouds.com.
Results
A total of 63 of 97 eligible subjects (65%) completed a COVID-19 questionnaire between July 24, 2020 and August 22, 2020 (Table 1). There were no significant differences in age, sex, race, ethnicity, insurance type, disability status, geographic location, SLE disease duration, SLE activity, SLE-related damage, or baseline history of diagnosed anxiety, depression or fibromyalgia between those who completed the survey and those who did not. Nearly all respondents were female and about 50% were non-white. Duration of disease varied significantly among participants, but mean baseline disease activity and disease-related damage scores were low.
Table 1.
Baseline Characteristics of Study Participants
| Characteristic | Participants (n = 63) |
|---|---|
| Age: mean ± SD years (range) | 42.5 ± 13.5 (21.0 – 78.0) |
| Female: n (%) | 62 (98.4) |
| Race: n (%) | |
| White | 31 (49.2) |
| Black | 15 (23.8) |
| Asian | 9 (14.3) |
| More than One Race | 5 (7.9) |
| Not Reported | 3 (4.8) |
| Ethnicity: n (%) | |
| Hispanic/Latino | 10 (15.9) |
| Insurance: n (%) | |
| Medicaid | 14 (22.2) |
| Medicare | 7 (11.1) |
| Commercial | 42 (66.7) |
| On Disability (by patient self-report): n (%) | 17 (27.0) |
| Geographic Location: n (%) | |
| Boston | 23 (36.5) |
| New York | 40 (63.5) |
| SLE Characteristics | |
| SLE Disease Duration: mean ± SD years (range) | 10.9 ± 9.2 (0.5 – 44) |
| SELENA-SLEDAI: mean ± SD (range) [Range 0 to 105, higher worse] | 3.3 ± 3.3 (0 – 14) |
| SLICC/ACR Damage Index: mean ± SD (range) [Range 0 to 46, higher worse] | 1.0 ± 2.0 (0 – 13) |
| Co-Morbid Conditions (by patient self-report) | |
| Anxiety: n (%) | 14 (22.2) |
| Depression: n (%) | 13 (20.6) |
| Fibromyalgia: n (%) | 11 (17.5) |
PRO Measures:
PROMIS CAT T-scores at the time of completion of the supplemental COVID-19 questionnaire and changes from the pre-pandemic baseline are shown in Table 2. Participants’ physical function, pain interference, fatigue, and anxiety T-scores during the pandemic were worse than US general population mean of 50 by a half standard deviation or more. PROMIS social isolation scores in our study participants during the early phase of the pandemic were comparable to the US general population (mean T-score 49.9 +/− 10.4). Physical function, pain interference, anxiety, and depression T-scores showed significant deterioration from their pre-pandemic levels, while other domains, including sleep disturbance and self-efficacy, did not demonstrate significant changes. Nearly fifty percent of participants exhibited increased anxiety (48%) and depression (48%) and over forty percent demonstrated worsened fatigue, pain interference, and cognitive abilities T-scores (Table 2).
Table 2.
PROMIS® Computerized Adaptive Test (CAT) Scores during the COVID-19 Pandemic
| PROMIS® CAT | N | T-Scorea Mean ± SD |
Change in T-Score from pre-pandemic Mean ± SD |
p-valueb | % with Worsened T-Scoresc |
|---|---|---|---|---|---|
| Physical Function | 63 | 45.0 ± 11.3 | −2.0 ± 7.4 | 0.03 | 39.7 |
| Pain Interference | 63 | 56.5 ± 10.8 | 2.3 ± 6.7 | 0.01 | 41.3 |
| Fatigue | 63 | 56.7 ± 11.6 | 1.8 ± 8.3 | 0.09 | 42.9 |
| Sleep Disturbance | 63 | 53.0 ± 11.9 | 0.1 ± 8.5 | 0.94 | 33.3 |
| Social Participation | 60 | 47.1 ± 11.0 | −1.3 ± 7.8 | 0.21 | 40.0 |
| Applied Cognition- Abilities | 60 | 47.4 ± 8.8 | −1.6 ± 7.5 | 0.10 | 43.3 |
| Anxiety | 59 | 55.4 ± 10.8 | 2.9 ± 8.3 | 0.01 | 47.5 |
| Depression | 58 | 52.1 ± 10.3 | 2.7 ± 7.9 | 0.01 | 48.3 |
| Self-Efficacy (Medication Management) | 61 | 48.8 ± 7.4 | −0.2 ± 6.2 | 0.84 | 26.2 |
| Social Isolation | 62 | 49.9 ± 10.4 | N/A | N/A | N/A |
T-scores are normalized around a mean of 50 and standard deviation of 10 in the general population, with higher scores indicating more of the measured domain.
p-value indicates statistical significance of changes in T-scores based on paired t-tests.
Worsening as defined by T-score change ≥ 3.
One third of participants (21/63) demonstrated increases in PROMIS anxiety scores of 5 or more points. These participants with increased anxiety did not differ from other respondents with regard to sociodemographic characteristics, baseline disease activity and damage, and co-morbid diagnoses of anxiety, depression, or fibromyalgia. Participants with baseline diagnoses of anxiety did not have significantly different changes in T-scores compared to the rest of the cohort.
Fifty-one participants (81%) noted that their responses to the PROMIS surveys were at least partly influenced by their SLE. At the same time, 39 (62%) reported that other factors also played a role, with most citing the pandemic in free-text responses.
COVID-19 Questionnaire:
The majority of participants (60%) reported that their health was “about the same” since the start of the COVID-19 pandemic. Fourteen respondents (22%) reported some worsening of health status while 11 (18%) reported some improvement. Those with a baseline diagnosis of anxiety were 3.3 times more likely to report worsening of their health since the start of the pandemic than those without (50% vs.15%, p=0.03).
Most respondents did not report challenges in accessing healthcare (Figure 1). Few patients endorsed difficulty getting medications (15%) or medical care (16%). Over three quarters reported that they had a visit with their rheumatologist since the start of the pandemic, with 32 patients (51%) receiving care via telehealth and 16 (25%) attending in-person visits. Among those who had a telehealth visit, the vast majority were satisfied with the quality of the experience (Figure 2). Twenty-four patients (75%) agreed or strongly agreed that telehealth was an acceptable way to receive healthcare services and over 90% felt comfortable communicating with their rheumatologists during the visits. Nearly everyone (91%) felt that the lack of physical contact during visits was not a problem. However, several noted in free text responses that while telehealth was a good option during the pandemic, in-person visits were generally preferable particularly when lupus symptoms were active or if laboratory studies needed to be drawn.
Figure 1.
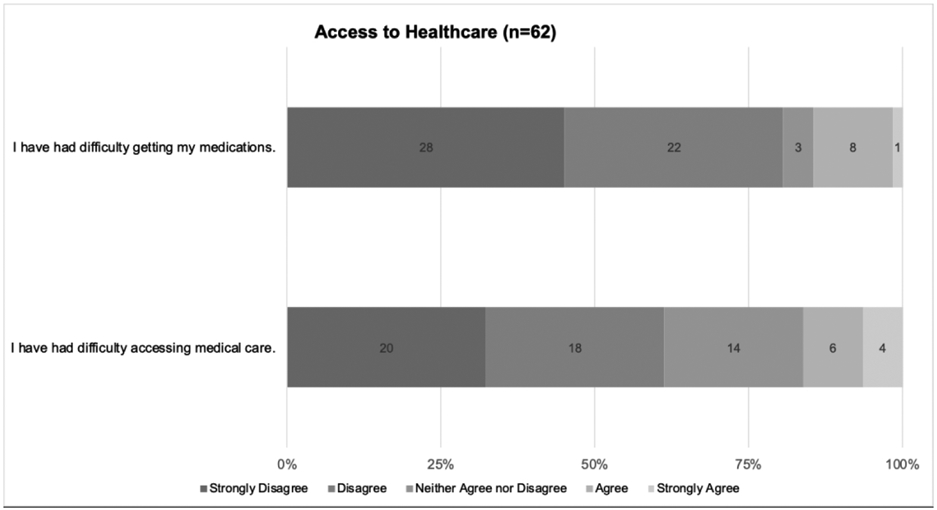
Access to Healthcare Survey Results
Figure 2.
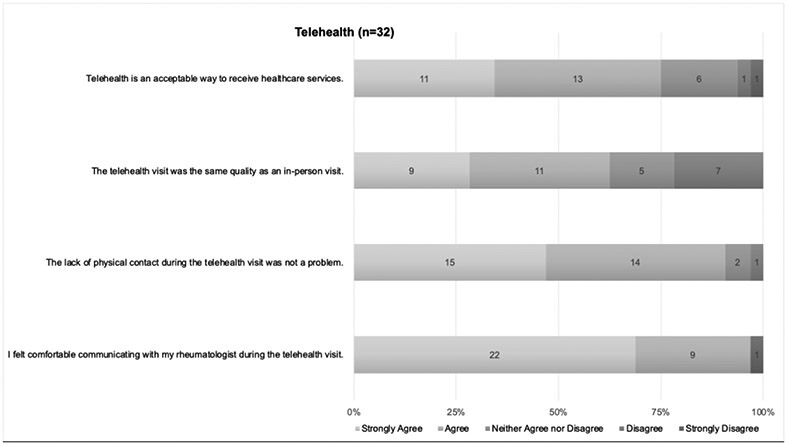
Telehealth Survey Results
Qualitative Analysis:
Several major themes were identified from participants’ free-text responses to the prompt “please explain how the COVID-19 pandemic has affected your health” (Table 3 and Figure 3). Increased anxiety, depression, and isolation were common themes in over 40% of responses. Patients also cited concerns about health risks due to immunosuppression, noting that both their underlying SLE and the medications they were taking increased their vulnerability and stress. Physical activity was a challenge for many (>20%), with respondents reporting significant physical and emotional consequences including declining function, weight gain, and increased pain and stress as a result of being unable to exercise. Challenges accessing health care were noted by a few who mentioned rescheduled medical, physical therapy, and infusion treatment appointments. Four patients specifically cited difficulties obtaining hydroxychloroquine. A fifth of participants (21%) noted that the pandemic had no significant impact on their health, and a few (8%) even reported a positive impact from having more time and being able to work remotely.
Table 3.
Themes and Illustrative Quotations from Free-Text Responses on the Impact of the COVID-19 Pandemic
| Theme | Quotation |
|---|---|
| Anxiety/Depression | “It has increased my anxiety, and I've had trouble sleeping, even though I am already over-tired from having a newborn.” “Covid has caused anxiety, depression and overall sadness.” “Stress and anxiety mostly. Don't know what information to trust.” |
| Isolation | “Periodic feelings of isolation. Sad at times that I cannot socialize with friends and family.” “Isolation has caused depression and exacerbated symptoms” “Some isolation … Less support because of distancing.” |
| Health risk due to immunosuppression | “Because I have Lupus and have been on the medication I take for over 40 years, I am concerned about being immunocompromised. Covid-19 and health concerns have impacted the decisions I make regarding my exposure to others during this time.” “The stress over being immunosuppressed amid a pandemic has been challenging at times.” |
| Decreased physical activity | “Doing aquatics classes at a community center greatly improved my health in the year prior to the pandemic - both physically and emotionally. I had few symptoms, reduced pain, and went down in dosage on my antidepressants. I am unable to go to the community center for these classes or get my therapeutic massage therapy, so my pain has increased, my overall health and physical ability has declined, and I am crawling out of a terrible depression after increasing my antidepressants and doubling down on therapy.” “I have practiced extreme social distancing. Prior to the pandemic I used to go for walks for exercise. In the first two months of the pandemic I stayed inside which has negatively impacted my health and well-being. I try to increase my time outdoors.” “Inability to exercise outdoors, weight gain.” “Not being able to go to the gym has been very hard on me. I have gained too much weight which makes my pulmonary issues worsen as well as pain.” |
| Decreased access to medications/health care | “There was a shortage of one of my medications—hydroxychloroquine.” “I was unable to receive monthly infusion treatments, delayed appointments for specialists as office was closed.” “an in-person visit with my doctor had to be rescheduled.” “Harder to go to physical therapy” |
| Financial strain | "I had to stop working, that affected my financial situation." |
| Positive impact | “It did not affect my health in a negative way. In fact, I was feeling better than what I had been feeling before Covid19.” “Not having to commute has allowed me to rest more.” “I was having a lupus flare right before pandemic began. My health has improved since I started teleworking back in Feb 2020.” “Living in a quieter place has reduced my stress and increased my health.” |
| No impact | “Not much has changed in my health due to Covid19” |
Figure 3.
Impact of COVID-19 Pandemic on Health Free Text Response Word Cloud
Discussion
This prospective cohort study found that individuals with SLE living in the northeast United States experienced a significant physical and emotional toll in the initial months of the COVID-19 pandemic. Close to fifty percent of respondents had increased symptoms of anxiety and depression, and over forty percent demonstrated worsened pain interference, fatigue, cognitive abilities and social participation on standardized measures. Participants described stress amplified by the fear and uncertainty of being chronically immunosuppressed. Notably, despite widespread disruptions to health care, a majority of patients denied worsened health or difficulties accessing medical care.
Our findings of increased psychological distress in persons with SLE are consistent with what has been reported more generally in the United States and globally during the pandemic(14-17). As immunosuppressed individuals who rely on frequent medical care, SLE patients may be particularly susceptible to pandemic stressors and have been shown to exhibit increased symptoms of anxiety and depression even compared to those with other rheumatic diseases(18). Nearly half of our cohort had a significant increase in anxiety and depression, a larger proportion than what has been previously been reported in SLE populations during the pandemic to the best of our knowledge. One abstract paradoxically found improvements in PROs in an SLE cohort living in Georgia, while another found increased anxiety and depression in 15% of a national sample of SLE patients(18,19). The geographic location of participants and timing of data collection may be important contextual factors contributing to the variability of these findings.
Our study, in a cohort of patients with SLE living in early epicenters of the pandemic in the United States, may provide important insight into the impact of the pandemic on those with SLE more broadly as caseloads grow both nationally and internationally. Our findings, while significant, may underestimate the full burden of symptoms related to the pandemic as COVID-19 surveys were completed in mid-summer 2020, when cases were decreasing and communities were re-opening after the initial surge in the northeast United States. Even so, the increase in physical and emotional symptoms we observed may have significant consequences if sustained through subsequent phases of the pandemic. Ongoing anxiety and stress are associated with worse outcomes in SLE, including increased perceived disease activity and symptom severity(3,20). It is notable that those with pre-existing diagnoses of anxiety in our study were more than three times as likely to report worsened health as other participants. As the pandemic continues, screening for symptoms of anxiety and depression and providing appropriate treatment will be of particular importance in providing comprehensive care for SLE.
Surprisingly, the majority of SLE patients in our study denied difficulty accessing health care despite disruptions to in-person care and widely reported shortages of hydroxychloroquine related to increased demand for the drug early in the pandemic(21). This finding may reflect the high self-efficacy of members of this particular cohort, who elected to participate in a longitudinal research study and who had had SLE for an average of over 10 years. PROMIS self-efficacy scores of participants were comparable to general population norms and remained largely unchanged from the pre-pandemic baseline, suggesting most respondents were adept at managing their illness. Social isolation PROMIS scores were similarly comparable to general population norms despite widespread social distancing, and may also indicate a population accustomed to coping with SLE and the social isolation that often accompanies the diagnosis(22). Certain sub-groups of those with SLE, including individuals with newly diagnosed disease, those without established outpatient rheumatologists, and those with poor self-efficacy in chronic disease management, may be more susceptible to lapses in care than those in our study. In addition, although our cohort includes patients from diverse racial and socio-economic backgrounds, our patients were all insured and received care at tertiary care academic medical centers. Our findings may not be representative of the experience of the most vulnerable SLE patients. Specific attention to these populations is critical as the already pronounced existing health care disparities in SLE may be exacerbated by the COVID-19 pandemic, which has had disproportionate impact on minorities and individuals from lower socio-economic backgrounds(23).
Our study also provides important initial insight into the feasibility and acceptability of telehealth care in SLE. The majority of respondents who attended a telehealth visit felt it was an acceptable way to receive healthcare services and appreciated the convenience of saved travel time. As the benefits of telemedicine continue to be recognized, virtual visits may evolve into a complementary form of health care for SLE patients that outlives the pandemic. However, investigation of barriers to participating in telehealth will be important, as nearly 50% of patients in our study did not have a virtual visit in the first three months of the pandemic despite universal access to a smartphone and/or computer in this cohort. Concerns expressed about the adequacy of telemedicine to evaluate lupus flares and the need to present in person anyway for blood draws are consistent with what others have found(24) and warrant further evaluation. Strengths of our study include its longitudinal design and use of quantitative and qualitative analyses that provide a nuanced picture of SLE patients’ experiences in the early months of the pandemic. The study population, diverse individuals with verified SLE living in an initial hot spot of the pandemic in the United States, and the use of validated outcome measures are additional strengths. This is unlike many observational studies which are cross-sectional and include individuals with self-reported SLE among a number of other autoimmune conditions(18,25-27).
Certain limitations are important to note. There may be selection bias in patients participating in the cohort and completing the supplemental survey despite robust enrollment and response rates. This may account for the relatively few males in this study. We did not identify any socio-demographic or clinical differences between respondents and the overall cohort, but we may have been underpowered to detect such differences. We also lacked statistical power to conduct multivariable models to evaluate the relative impact of socio-demographics, SLE disease characteristics, baseline comorbidities, and baseline PRO scores on the evaluated outcomes. We were unable to obtain SELENA-SLEDAI scores at the time of the supplemental survey as patients completed the surveys remotely and asynchronously with clinical care. In addition, pre-pandemic PROMIS social isolation scores were unavailable, which limited our ability to assess if there was any significant change in perceived social isolation due to the pandemic. Finally, the experience of our participants, who were treated at two urban academic medical centers may not be generalizable to other populations receiving care in community or rural settings.
In summary, SLE patients in New York City and Boston experienced a significant increase in anxiety, depression, and physical symptoms at the start of the COVID-19 pandemic. Patients described stress from the pandemic intensified by fear and uncertainty related to their chronic immunosuppression. Now more so than ever, SLE patients require comprehensive patient-centered care that is tailored to their holistic needs. As this study demonstrates, standardized PRO measures can be useful tools for identifying domains that require attention on individual and population levels. Use of these measures to monitor and address health-related quality of life is critically important to improving outcomes for individuals with SLE as the pandemic continues to unfold.
COVID-19 Supplemental Questionnaire.
Since the start of the COVID-19 pandemic:
My health is:
[Much better; somewhat better; about the same; somewhat worse; much worse]
I have had difficulty accessing medical care.
[Strongly agree; agree; neither agree nor disagree; disagree; strongly disagree]
I have had difficulty accessing my medications.
[Strongly agree; agree; neither agree nor disagree; disagree; strongly disagree]
Please explain how the COVID-19 pandemic has affected your health.
[Free text]
Have you had an appointment with your rheumatologist since the start of the pandemic?
[Yes/No]
My recent rheumatology visit was conducted:
a) in person; b) remotely by telehealth
If b):
Please indicate your agreement with the following statements.
[Strongly disagree; disagree; neither agree nor disagree; agree; strongly agree]:
I felt comfortable communicating with my rheumatologist during the telehealth visit.
The lack of physical contact during the telehealth visit was not a problem.
The telehealth visit was the same quality as an in-person visit.
Telehealth is an acceptable way to receive healthcare services.
Acknowledgements
The authors would like to thank Serena Weber, Shreya Shetty, Neena Patel, Dina Sheira, and Robyn Lipshultz for assistance with data collection.
Funding:
This work was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, Award Numbers 1KL2TR002545 and UL1TR002544, and the Michael D. Lockshin Fellowship of the Barbara Volcker Center for Women and Rheumatic Disease at the Hospital for Special Surgery. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Declaration of Conflicting Interests: The authors have no conflicts of interest to declare.
References
- 1.Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peralta-Ramírez Ml, Jiménez-Alonso J, Godoy-García JF, Perez-García M, Jáimez L, Guzmán Úbeda M, et al. The effects of daily stress and stressful life events on the clinical symptomatology of patients with lupus erythematosus. Psychosom Med. 2004;66:788–94. [DOI] [PubMed] [Google Scholar]
- 3.Adams SG, Dammers PM, Saia TL, Brantley PJ, Gaydos GR. Stress, depression, and anxiety predict average symptom severity and daily symptom fluctuation in systemic lupus erythematosus. J Behav Med. 1994;17:459–77. [DOI] [PubMed] [Google Scholar]
- 4.Martz CD, Allen AM, Fuller-Rowell TE, Spears EC, Lim SS, Drenkard C, et al. Vicarious racism stress and disease activity: the Black Women’s Experiences Living with Lupus (BeWELL) study. J Racial Ethn Heal Disparities. 2019;6:1044–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tisseverasinghe A, Peschken C, Hitchon C. Anxiety and mood disorders in systemic lupus erythematosus: current insights and future directions. Curr Rheumatol Rep. 2018;20(12). [DOI] [PubMed] [Google Scholar]
- 6.Petri M, Kim MY, Kalunian KC, Grossman J, Hahn BH, Sammaritano LR, et al. Combined oral contraceptives in women with systemic lupus erythematosus. N Engl J Med 2005;353:2550–8. [DOI] [PubMed] [Google Scholar]
- 7.Gladman DD, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, et al. The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. 1996;39:363–9. [DOI] [PubMed] [Google Scholar]
- 8.Kasturi S, Szymonifka J, Burket JC, Berman JR, Kyriakos A, Levine AB, et al. Validity and reliability of Patient Reported Outcomes Measurement Information System computerized adaptive tests in systemic lupus erythematosus. J Rheumatol. 2017;44:1024–31. [DOI] [PubMed] [Google Scholar]
- 9.Parmanto B, Lewis AN, Graham KM, Bertolet MH. Development of the Telehealth Usability Questionnaire (TUQ). Int J Telerehabilitation. 2016;8:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hays RD, Spritzer KL, Fries JF, Krishnan E. Responsiveness and minimally important difference for the Patient-Reported Outcomes Measurement Information System (PROMIS) 20-item physical functioning short form in a prospective observational study of rheumatoid arthritis. Ann Rheum Dis. 2015;74:104–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee AC, Driban JB, Price LL, Harvey WF, Rodday AM, Wang C. Responsiveness and minimally important differences for 4 Patient-Reported Outcomes Measurement Information System short forms: physical function, pain interference, depression, and anxiety in knee osteoarthritis. J Pain. 2017;18:1096–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz P, Pedro S, Alemao E, Yazdany J, Dall’Era M, Trupin L, et al. Estimates of responsiveness, minimally important differences, and patient acceptable symptom state in five Patient-Reported Outcomes Measurement Information System short forms in systemic lupus erythematosus. ACR Open Rheumatol. 2020;2:53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Swanholm E, Mcdonald W, Makris U, Noe C, Gatchel R. Estimates of Minimally Important Differences (MIDs) for two Patient-Reported Outcomes Measurement Information System (PROMIS) computer-adaptive tests in chronic pain patients. J Appl Biobehav Res. 2014;19:217–32. [Google Scholar]
- 14.Alison Holman E, Thompson RR, Garfin DR, Silver RC. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Sci Adv. 2020;6:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. Published 2020 September 1. doi: 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi L, Lu Z-A, Que J-Y, Huang X-L, Liu L, Ran M-S, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the Coronavirus Disease 2019 pandemic. JAMA Netw Open. 2020;3(7):e2014053. Published 2020 July 1. doi: 10.1001/jamanetworkopen.2020.14053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson CN, Baumgartner J, Pichardo C, Toro B, Li L, Arciuolo R, et al. COVID-19 outbreak — New York City, February 29 – June 1 , 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1725–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katz P, Pedro S, Wip K, Simon T, Shaw Y, Cornish A. Changes in mental health during the COVID-19 pandemic among individuals with rheumatic disease [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/changes-in-mental-health-during-the-covid-19-pandemic-among-individuals-with-rheumatic-disease/. Accessed April 28, 2021. [Google Scholar]
- 19.Lim SS, Theis K, Dunlop-Thomas C, Bao G, Helmick C, Gordon C, et al. Unexpected changes in physical and psychological measures among Georgia lupus patients during the early weeks of the COVID-19 pandemic in the United States, March 30 – April 21, 2020 [abstract]. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/unexpected-changes-in-physical-and-psychological-measures-among-georgia-lupus-patients-during-the-early-weeks-of-the-covid-19-pandemic-in-the-united-states-march-30-april-21-2020/. Accessed April 28, 2021. [Google Scholar]
- 20.Roberts AL, Malspeis S, Kubzansky LD, Feldman CH, Chang SC, Koenen KC, et al. Association of trauma and posttraumatic stress disorder with incident systemic lupus erythematosus in a longitudinal cohort of women. Arthritis Rheumatol. 2017;69:2162–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mendel A, Bernatsky S, Askanase A, Bae SC, Clarke AE, Costedoat-Chalumeau N, et al. Hydroxychloroquine shortages among patients with systemic lupus erythematosus during the COVID-19 pandemic: Experience of the Systemic Lupus International Collaborating Clinics. Ann Rheum Dis. 2020;80:272–4. [DOI] [PubMed] [Google Scholar]
- 22.Sutanto B, Singh-grewal D, Mcneil HP, Neill SO, Craig JC, Jones J, et al. Experiences and perspectives of adults living with systemic lupus erythematosus: thematic synthesis of qualitative Studies. Arthritis Care Res. 2013;65:1752–65. [DOI] [PubMed] [Google Scholar]
- 23.Feldman CH, Ramsey-Goldman R. Widening disparities among patients with rheumatic diseases in the COVID-19 era: an urgent call to action. Arthritis Rheumatol. 2020;72:1409–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.So H, Szeto CC, Tam LS. Patient acceptance of using telemedicine for follow-up of lupus nephritis in the COVID-19 outbreak [published online ahead of print, 2020 Jun 24]. Ann Rheum Dis. 2020;annrheumdis-2020-218220. doi: 10.1136/annrheumdis-2020-218220 [DOI] [PubMed] [Google Scholar]
- 25.Michaud K, Wipfler K, Shaw Y, Simon TA, Cornish A, England BR, et al. Experiences of patients with rheumatic diseases in the United States during early days of the COVID-19 Pandemic . ACR Open Rheumatol. 2020;2:335–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.George MD, Venkatachalam S, Banerjee S, Baker JF, Merkel PA, Gavigan K, et al. Concerns, healthcare use, and treatment interruptions in patients with common autoimmune rheumatic diseases during the COVID-19 pandemic [published online ahead of print, 2020 Nov 15]. J Rheumatol. 2020;jrheum.201017. doi: 10.3899/jrheum.201017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rathi M, Singh P, Bi HP, Shivanna A, Kavadichanda C, Tripathy SR, et al. Impact of the COVID-19 pandemic on patients with systemic lupus erythematosus: Observations from an Indian inception cohort. Lupus. 2021;30(1):158–164. [DOI] [PubMed] [Google Scholar]