Abstract
Pancreatic cancer surgery continues to be associated with a high operative morbidity rate, poor long‐term survival outcomes, and various challenges in obtaining high‐level evidence. Not only is the early postoperative morbidity rate high, but also late morbidity involves lifelong nutritional support for long‐term survivors. Due to poor survival outcomes even after curative surgery, pancreatic surgeons have doubts about the role of surgery as the definitive treatment for pancreatic cancer. Additionally, conducting clinical trials to obtain high‐level evidence in the field of pancreatic surgery is difficult, and the results have only had a moderate impact on clinical practice due to skepticism regarding their quality. Therefore, quality evidence regarding the extent of resection, mode of approach to dissection, reconstruction methods for pancreatico‐enteric anastomosis, determination of resectability, timing of surgery, and the definition of the resection margin is lacking. However, numerous innovative pancreatic surgical procedures have been developed, which may aptly have been called “art” when they were first introduced, regardless of whether they subsequently were supported by scientific evidence. In this review, we provide recent examples of the integration of art and science in the field of pancreatic surgery, which illustrate how the creative ideas of pancreatic surgeons evolved into generally accepted clinical practice. Pancreatic surgeons should be considered “surgical artists,” “surgical scientists,” and “surgical practitioners.” We look forward to more “surgical artists” educating future “surgical artists and scientists” to create a richer “spirit of innovation,” leading to a more beautiful integration of art and science in the field of pancreatic surgery.
Keywords: evidence‐based medicine, inventions, neoplasms, pancreas, pancreatectomy
Numerous innovative pancreatic surgical procedures have been developed, which may aptly have been called “art” when they were first introduced, regardless of whether they subsequently were supported by scientific evidence. In this review, we provide recent examples of the integration of art and science in the field of pancreatic surgery, which illustrate how the creative ideas of pancreatic surgeons evolved into generally accepted clinical practice. Pancreatic surgeons should be considered “surgical artists,” “surgical scientists,” and “surgical practitioners.”

1. INTRODUCTION
Compared to other malignancies of the gastrointestinal tract, pancreatic cancer surgery is unique in terms of its associated high operative morbidity rate, poor long‐term survival outcomes, and challenges in terms of obtaining high‐level evidence based on randomized clinical trials (RCTs). Until recently, the pancreas has been referred to as “no man's land,” which may explain why even the brightest thinkers in the East and West did not describe the pancreas in their anatomical diagrams (Figure 1).
FIGURE 1.
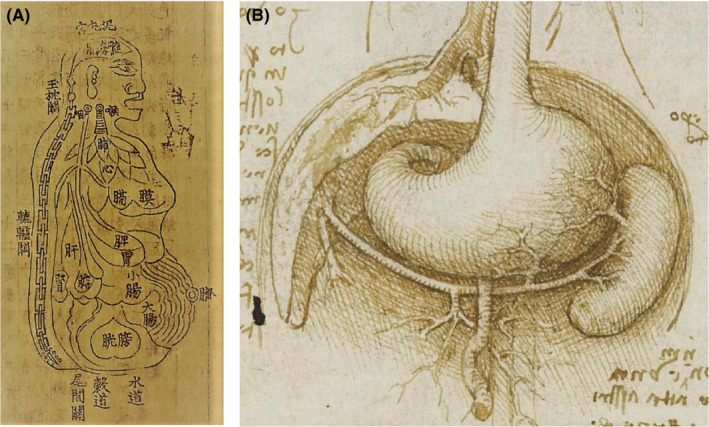
Understanding abdominal viscera as represented in classics from the Orient and the Occident. A. Drawing of the overall body, viscera, and bowel (Sinhyeongjangbudo) in Donguibogam, (Principles and Practice of Eastern Medicine; Memory of the World, UNESCO, Reproduced from Cultural Heritage Administration of the Republic of Korea according to Korea Open Government License, available from https://www.cha.go.kr/unescoGallery/selectUnescoGalleryView.do?id=189978). B. Abdominal anatomy according to Leonardo da Vinci (Reproduced from “Recto: The gastrointestinal tract and the bladder. Verso: The gastrointestinal tract, and the stomach, liver, and spleen c.1508” by Leonardo da Vinci with permission from the Royal Collection Trust, Royal Collection Trust/© Her Majesty Queen Elizabeth II 2021, available from https://www.rct.uk/collection/919031/recto‐the‐gastrointestinal‐tract‐and‐the‐bladder‐verso‐the‐gastrointestinal‐tract)
After pancreatectomy, early morbidity is associated with pancreatic leakage, bleeding, delayed gastric emptying, and local sepsis, which often result from complex surgical procedures requiring multiple anastomoses. 1 , 2 , 3 In addition, surgery‐related and systemic complications are more frequent due to the long operation time and, compared to other gastrointestinal malignancies, the general preoperative condition of patients with pancreatic cancer is worse. Late operative morbidity consists of exocrine and endocrine pancreatic insufficiency due to the loss of pancreatic parenchyma and marginal ulcers or the development of afferent loop syndrome attributable to gastrointestinal tract reconstruction. 4 These late complications give rise to nutritional disorders demanding lifelong nutritional support in long‐term survivors. 5 Therefore, the history of pancreatectomy procedures and treatments lead to the constant efforts currently made to reduce postoperative complications.
Moreover, survival outcomes for pancreatic cancer remain low and have not improved significantly over the past few decades. 6 Only 20%‐30% of patients at the time of pancreatic cancer diagnosis are considered candidates for surgery, while 70%‐80% of patients eventually fail to receive curative treatment mainly due to systemic metastasis. 6 Moreover, due to poor survival outcomes even after curative resection, pancreatic surgeons have doubts about the role of surgery as the definitive treatment for pancreatic cancer. For these reasons, pancreatic cancer is considered a systemic disease; however, surgeons should also focus on achieving safer and more complete local control of the tumor through surgery.
Nevertheless, there is a lack of high‐level evidence in the field of pancreatic surgery. Consequently, we do not yet have detailed guidelines for pancreatic surgical procedures, partly due to limitations in conducting RCTs, especially those focused on pancreatic cancer. Despite a noticeable increase in the quantity and quality of RCTs focused on pancreatic surgery, many are limited in their design and reporting, including selective reporting, limited assessment of long‐term effects, and the risk of small sample bias. 7 , 8 Specifically, given small differences in the expected effect of pancreatic surgery, the sample size can be “prohibitively large” while the number of pancreatic cancer patients is insufficient for case recruitment. 9 Moreover, standardization of surgical techniques is difficult due to the complexity of the procedures. 10 As a result of deep‐rooted skepticism, RCTs for pancreatic surgery have had only a moderate impact on daily clinical practice. For this reason, neither a synthesis of evidence nor a systematic review of filtered evidence is easily obtainable for pancreatic cancer surgery. 11
2. CURRENT ISSUES IN PANCREATIC SURGERY
As previously mentioned, a number of issues regarding pancreatic surgical procedures, especially those for pancreatic cancer, still need to be addressed (Table 1). However, authoritative in‐depth guidelines, including those from the National Comprehensive Cancer Network (NCCN), 12 American Society of Clinical Oncology (ASCO), 13 European Society for Medical Oncology (ESMO), 14 Japan Pancreas Society (JPS), 15 and the International Study Group for Pancreatic Surgery (ISGPS), 16 have yet to be provided for pancreatic surgery. Each of the current issues in pancreatic surgery will be discussed below.
TABLE 1.
Current issues in pancreatic surgery
| Extent of surgery |
| Organ |
| Observation vs surgery |
| Excision vs pancreatectomy |
| Partial vs total pancreatectomy |
| Pancreaticoduodenectomy: standard Whipple vs pylorus preservation vs pylorus resection |
| Organ preservation (duodenum, spleen, or splenic vessels) |
| Lymph node dissection: standard vs extended |
| Nerve plexus dissection: preservation vs half‐circumferential removal vs 360° removal |
| Major vessels resection |
| Portal vein or superior mesenteric vein: technical amenability in relation to the first or second jejunal vein and duodenal inferior margin |
| Superior mesenteric artery: under trials in some centers |
| Common hepatic artery |
| Celiac artery: distal pancreatectomy with celiac artery resection (DPCAR) |
| Meso‐pancreas excision |
| Definition of the area |
| Level of dissection |
| Mode of approach for dissection |
| Various superior mesenteric artery first approach |
| Infra‐colic (mesenteric) vs supra‐colic |
| Right or left vs supra‐pancreatic |
| Radical ante‐grade modular pancreato‐splenectomy (RAMPS): anterior and posterior |
| No touch isolation technique |
| En bloc dissection |
| Minimally invasive surgery |
| Reconstruction method (pancreatic anastomosis) |
| Pancreaticojejunostomy vs pancreaticogastrostomy |
| Dunking/invaginating method vs duct‐to‐mucosa anastomosis |
| Internal vs external vs no stent |
| Many innovative modifications of pancreatic restoration |
| Usage and duration of surgical drain |
| Transection and stump management |
| Stapling vs hand sewing |
| With or without use of sealant, type of sealant |
| With or without use of somatostatin |
| Determination of resectability |
| Criteria |
| Various criteria: National Comprehensive Cancer Network (NCCN) criteria, etc. |
| International Association of Pancreatology (IAP) consensus criteria (+ biologic/conditional criteria) |
| Tools and their reliability: CT, MRI, PET, cytology, etc. |
| Determination after neoadjuvant treatment |
| Response evaluation by CT tumor marker, PET, etc. |
| Timing of Surgery |
| Upfront surgery, surgery after neoadjuvant therapy |
| Timing and indication of conversion surgery |
| Resection margin and residual tumor |
| Significance of multiple margins |
| Concept of residual tumor (tumor at the margin vs 1‐mm margin) |
First, there is much debate regarding the appropriate extent of resection, which includes observation vs surgery, excision vs partial pancreatectomy, partial vs total pancreatectomy, the extent of gastric resection during pancreaticoduodenectomy ([PD]; standard Whipple operation, pylorus preservation, or pylorus resection), and organ preservation (duodenum, spleen, or splenic vessels; detailed in the “spleen‐preserving distal pancreatectomy” section), depending on the nature and extent of the disease. 17 , 18 Additionally, the extent of lymphadenectomy, resection of major vessels, and nerve plexus dissection can be controversial for several reasons; for example, whether to include the resection or dissection of remote site lymph nodes, the portomesenteric vein, and major arteries including the celiac axis (detailed in the “modified Appleby operation for advanced pancreatic body cancer” section), superior mesenteric artery (SMA), and hepatic arteries. Previous RCTs have confirmed that prophylactic hemi‐circumferential peri‐SMA nerve plexus dissection was not beneficial for survival gain. 19 , 20 , 21 , 22 However, even though R0 resection can be achieved by adjusting the dissection level, no consensus has been achieved on the systematic criteria for the extent of resection according to the extent of the patient's primary disease. 23 Finally, although the definition remains controversial, the mesopancreas should also be considered when determining the extent of surgery (detailed in the “meso‐pancreas excision” section). 24
Second, the various modes of approaching dissection require further discussion, which include different types of SMA (first) approaches mainly for pancreatic head cancer, 25 , 26 , 27 , 28 , 29 , 30 , 31 radical ante‐grade modular pancreato‐splenectomy for pancreatic body and tail cancer, 32 , 33 the no‐touch isolation technique, 28 en bloc dissection, 34 , 35 and minimally invasive surgery. 36 , 37 , 38 Recently, the Miami International Evidence‐based Guidelines strongly recommended minimally invasive distal pancreatectomy for benign and low‐grade malignant tumors over open surgery; however, data on the advantages of minimally invasive PD over open surgery are insufficient. Minimally invasive pancreatectomy is recommended in high‐volume centers, and the requirement for a structured training program for minimally invasive pancreatectomy must also be emphasized. 38
Third, a major factor contributing to morbidity after pancreatectomy is the leakage of pancreatic juice from the pancreatico‐enterostomy or pancreatic stump. Therefore, pancreatic surgeons are continuously searching for the best techniques for anastomosis and stump closure, which include various methods of reconstruction, the site and route of anastomosis, the use and type of stent or surgical drain, the use of surgical tissue adhesives, and other innovative techniques to restore pancreatico‐enteric continuity. 39 , 40
Fourth, the criteria and tools for determining resectability are constantly evolving. To date, several resectability criteria have been proposed by various institutions and academic societies. Since its first introduction in 2002, the NCCN resectability criteria have been the most widely adopted. 12 Particularly, diagnostic criteria for borderline resectable pancreatic cancer have primarily evolved with a focus on technical resectability. 16 However, the concept of this disease entity includes oncological curability supported by neoadjuvant treatment. 41 Consequently, the criteria for determining tumor resectability are expanding beyond only anatomical or technical perspectives. Recently, the biological criteria proposed by the MD Anderson Cancer Center and the International Association of Pancreatology (IAP) have been validated. 42 , 43 Criteria for imaging and non‐anatomical criteria such as tumor markers, patient condition, and genetic profiling are also being developed. 44 In particular, establishing criteria for biological markers and morphological and functional imaging after neoadjuvant therapy is challenging. 45 Furthermore, the appropriate timing of surgery (upfront or after neoadjuvant therapy) and conversion surgery is fiercely debated. 46
Lastly, the appropriate definition and assessment of the resection margin of the surgical specimen is controversial. PD specimens for pancreatic cancer have the most resection margins among the gastrointestinal malignancies, with seven margin evaluations recommended, including transection (pancreatic neck, proximal and distal gastrointestinal tract, bile duct, and vessel segment [if present]) and circumferential margins (portomesenteric groove, SMA margin [or retroperitoneal margin], posterior margin, and anterior surface). 12 In addition, a consensus regarding the definition of “positive resection margin” has not been reached. In 1977, the American Joint Committee on Cancer defined a positive resection margin as the presence of tumor cells on the margin. 47 However, the alternative definition presented in 2006 by the Royal College of Pathologists included the presence of tumor cells within 1 mm of the resection margin. 48 , 49 Since this new definition was introduced, the prognostic implications and real‐world practicality have been debated. 50 , 51
3. WHAT IS “ART,” “SCIENCE,” AND THEIR INTEGRATION?
Some of the abovementioned current issues have reached some level of consensus, while others are still under debate. As evidence accumulates over time, the level of consensus will likely increase in the future. However, by reflecting on past experiences, we can speculate on how this process will unfold in the future; the process required not only the mechanical accumulation of evidence, but also innovation and imagination that could be described as "art" beyond the boundaries of science.
Based on these concepts, a sample diagram integrating “art” and “science” in the field of surgery is presented in Figure 2. Surgeons recognize problems and raise questions based on their observations and experiences in clinical practice. Surgeons’ reasoning based on their knowledge and imagination can lead to the development of innovative and creative ideas, which result in theories and hypotheses that enable surgeons to conduct RCTs to establish evidence for future clinical applications. This process exists as an iterative cycle because new practice cannot be perfect.
FIGURE 2.
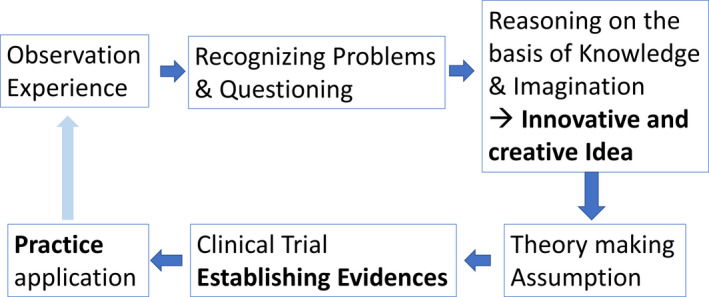
A sample diagram of the integration of art and science in the field of surgery
Most surgeons would claim they know what science is; however, what is art? The following are representative quotes about art that set it apart from science: “Art is not based on evidence, but on experience. Art does not confine to logic, it is an expression of feeling. Art does not work with hypothesis and does not need evidence and hence art is separate from science” 52 and “art is the solution of a problem which cannot be expressed explicitly until it is solved. Art is the creative process and it goes through all fields.” 53
There have been numerous creative and innovative surgical procedures in the history of pancreatic surgery that deserve to be called “art.” Most of the procedures belong to the realm of “art” when they are first introduced, regardless of whether they have been supported by scientific evidence or have become general practice. Likewise, there are many concepts and techniques applied to pancreatic surgery that are still considered “art.” Consequently, a few recent examples of “art, science, and their integration” are presented below. The first example demonstrates an experience in which an innovative technique, introduced by a need derived from clinical experience, continued to evolve through the integration of art and science. The second example illustrates how an innovative procedure adopted from other surgical disciplines overcame problems specific to pancreatic surgery. The third example shows the continuous integration of art and science regarding the meso‐pancreas, whose concept has not yet been fully established; the innovative concept, along with the development of a variety of surgical approaches in the area, is being evidenced through ongoing trials. The last example describes the integration of physiology and pancreatic surgery, which goes beyond the limits of the anatomical or technical perspective of surgery, often overlooked by surgeons.
3.1. Spleen‐preserving distal pancreatectomy
Overwhelming post‐splenectomy infection (OPSI) is a rare but fatal complication after distal pancreatectomy with splenectomy (Figure 3a). 54 The first solution introduced to manage this problem was the Warshaw procedure, in which the spleen is preserved (though not the splenic vessels) during distal pancreatectomy. 55 However, many surgeons had concerns about splenic infarction and gastric varix, which can develop after splenic vessel resection. 55 , 56 Therefore, the Kimura procedure, which involves the preservation of both the spleen and splenic vessels, was proposed. 57 Many surgeons have attempted both the Warshaw and Kimura procedures and have demonstrated their feasibility in clinical practice. Although initial reports appealed for improved technical reliability and safety compared to traditional distal pancreatectomy with splenectomy, 57 a recent systematic review and meta‐analysis have revealed that the incidence of splenic infarction and secondary splenectomy associated with the Kimura procedure is significantly lower than that of the Warshaw procedure. 58
FIGURE 3.
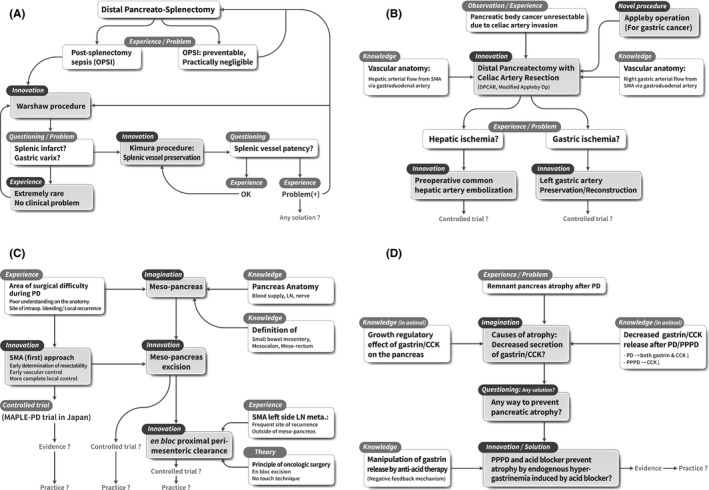
Cascade of knowledge, experience, questioning, hypothesis, and building evidence triggered by imagination and innovation. A. Spleen‐preserving distal pancreatectomy. B. Modified Appleby operation for advanced pancreatic body cancer. C. Meso‐pancreas excision. D. Preventing atrophy of the remnant pancreas after pancreatic head resection
However, OPSI were discovered to be more rare and preventable than expected, and splenic infarction and gastric varices were also rare, with little clinical significance. 59 , 60 Moreover, the benefits of splenic vessel preservation are not clear, since long‐term patency of the preserved vessels is uncertain. 61 As a result, surgeons are currently performing all three procedures (conventional splenectomy and spleen preservation with or without splenic vessel preservation) based on clinical experience and value judgments regarding the risk of complications. As “practitioners,” surgeons can choose between these options based on their own experience, their feasibility, and on evidence provided by the “surgical scientists.”
3.2. Modified Appleby operation for advanced pancreatic body cancer
Pancreatic body cancers frequently infiltrate the celiac artery due to its proximity to the tumor. Originally designed for advanced gastric cancer, the Appleby operation includes a total gastrectomy and celiac artery resection (Figure 3‐b). 62 The modified Appleby procedure, which involves preserving the right gastric artery and right gastroepiploic vessel to preserve the entire stomach, has been proposed and shown to be technically feasible as a treatment for pancreatic body cancer. 63 , 64 Additionally, hepatic and gastric blood flow is expected to be preserved by collateral blood flow from the SMA through the gastroduodenal and pancreaticoduodenal arteries after celiac and common hepatic artery resections. However, understandably, many pancreatic surgeons are concerned about hepatic and gastric ischemia, which have been reported but are extremely rare. 65 Therefore, innovative procedures have been developed to address these issues, including preoperative common hepatic artery embolization to ensure hepatic blood flow 34 , 66 and the preservation or reconstruction of the left gastric artery to prevent gastric ischemia. 67 , 68 Since these innovative techniques have only been reported in a limited number of cases, RCTs are required to confirm their technical feasibility and safety.
3.3. Meso‐pancreas excision
Based on our understanding of pancreatic anatomy and the definition of the mesentery, meso‐colon, and meso‐rectum, the concept of the meso‐pancreas has emerged (Figure 3‐c). 69 Although the anatomical concept of the meso‐pancreas is still controversial, some surgeons perform meso‐pancreas excision during PD for pancreatic head cancer to remove all soft tissue from this area since tumor involvement of retroperitoneal resection margin (R1 resection) and local recurrence is frequently reported after surgery. 70 , 71 In addition, innovative SMA‐first approaches that emphasize the principles of oncological surgery have been introduced to facilitate meso‐pancreas excision. One example is the MAPLE‐PD (mesenteric approach versus conventional approach for pancreatic cancer during Pancreaticoduodenectomy) trial currently in progress in Japan. 72 Another example is the concept of “en bloc proximal peri‐mesenteric clearance,” which was proposed due to cancer recurrence at the SMA left‐side lymph node, located outside of the meso‐pancreas, and for which RCT‐based evidence is expected in the future. 35 Through the above process, we can speculate how art and science are integrated to refine the establishment of innovative surgical procedures. All surgeons who have proposed this concept and attempted meso‐pancreas excision should be considered “surgical artists” as well as “surgical scientists.”
3.4. Preventing atrophy of the remnant pancreas after pancreatic head resection
Atrophy of the distal remnant pancreas is a frequently observed phenomenon after PD due to pancreaticojejunostomy stricture, postoperative radiation therapy, or the presence of an altered route for food passage, among others (Figure 3‐d). 73 Additionally, the physiological change in gastrin/cholecystokinin (CKK) secretion has emerged as another potential cause of atrophy. This is based on the understanding that gastrin/CCK secretion is reduced after PD or pylorus‐preserving PD (PPPD) and through the growth‐stimulating effect that gastrin/CCK has on the pancreas that has clearly been identified in animal models. 74 Therefore, it has been theorized that one of the causes of remnant pancreatic atrophy after PD/PPPD could be a decrease in gastrin/CCK secretion after PD and a decrease in CCK secretion after PPPD. Gastrin is secreted from the gastric antrum, and CCK is secreted from the duodenum; therefore, a consequence of both PD and PPPD is the removal of the source of these hormones. 75
Therefore, we wondered if there was any way to prevent pancreatic atrophy. The extent of post‐PPPD atrophy was hypothesized to be less than that of post‐PD atrophy because PPPD preserves the gastrin secretion zone. In addition, a significant level of preserved gastrin/CCK response was observed in post‐PPPD patients but not in post‐PD patients. 76 , 77 Based on the knowledge that gastrin secretion can be manipulated by acid blockers through physiological negative feedback mechanisms, 78 an innovative idea emerged; it was hypothesized that acid blockers may prevent or reduce the extent of atrophy of the remnant pancreas after PPPD by stimulating endogenous gastrin secretion. Subsequently, an RCT of patients after PPPD with induced hypergastrinemia showed a significant reduction in the extent of atrophy of the distal pancreas, along with an increased level of stool elastase. 73 Although long‐term administration of acid blockers after PD has not become general practice due to potential side effects, it was an innovation that should be considered an “art,” since a solution was proposed from a new perspective based on the surgeon's observation and experience. Pancreatic exocrine insufficiency that occurs immediately after PD/PPPD in association with pancreatic tissue loss and gastrin/CCK regulation gradually returns to normal functional levels within 6 months. 4 , 79 Therefore, the current version of the ISGPS position paper recommends that pancreatic enzyme replacement therapy should be routinely initiated and continued for at least 6 months postoperatively in patients who undergo PD. 5
4. CONCLUSION
This review illustrates how the creative ideas of pancreatic surgeons have evolved into generally accepted clinical practice. Surgeons should be considered “surgical artists,” “surgical scientists,” and “surgical practitioners” due to their capacity to combine art and science in clinical practice. We look forward to witnessing more “surgical artists” educating future “surgical artists and scientists” to continue the rich “spirit of innovation” in pancreatic surgery, which will lead to more innovative ideas and the development of more efficient methods of establishing high levels of evidence, and, thus, a more beautiful integration of art and science in the field of pancreatic surgery.
DISCLOSURE
Funding: The authors received no specific funding for this study.
Conflict of interest: The authors have no conflicts of interest or financial ties to disclose.
Author Contribution: Mee Joo Kang: conceptualization (supporting), formal analysis (supporting), methodology (supporting), visualization (equal), writing – original draft preparation (equal), writing – review & editing (equal). Sun‐Whe Kim: conceptualization (lead), formal analysis (lead), methodology (lead), supervision (lead), visualization (equal), writing – original draft preparation (equal), writing – review & editing (equal).
ACKNOWLEDGMENTS
The figure work was supported by the Creative Media Service of the National Cancer Center Korea. We would like to thank Editage (www.editage.co.kr) for English language editing.
Kang MJ, Kim S‐W. Current status and perspectives of the future of pancreatic surgery: Establishment of evidence by integration of “art” and “science”. Ann Gastroenterol Surg. 2021;5:738–746. 10.1002/ags3.12494
REFERENCES
- 1. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161:584–91. [DOI] [PubMed] [Google Scholar]
- 2. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma D, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20–5. [DOI] [PubMed] [Google Scholar]
- 3. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8. [DOI] [PubMed] [Google Scholar]
- 4. Park JW, Jang JY, Kim EJ, Kang MJ, Kwon W, Chang YR, et al. Effects of pancreatectomy on nutritional state, pancreatic function and quality of life. Br J Surg. 2013;100:1064–70. [DOI] [PubMed] [Google Scholar]
- 5. Gianotti L, Besselink MG, Sandini M, Hackert T, Conlon K, Gerritsen A, et al. Nutritional support and therapy in pancreatic surgery: A position paper of the International Study Group on Pancreatic Surgery (ISGPS). Surgery. 2018;164:1035–48. [DOI] [PubMed] [Google Scholar]
- 6. Mizrahi JD, Surana R, Valle JW, Shroff RT. Pancreatic cancer. Lancet. 2020;395:2008–20. [DOI] [PubMed] [Google Scholar]
- 7. Huttner FJ, Capdeville L, Pianka F, Ulrich A, Hackert T, Büchler MW, et al. Systematic review of the quantity and quality of randomized clinical trials in pancreatic surgery. Br J Surg. 2019;106:23–31. [DOI] [PubMed] [Google Scholar]
- 8. Kaido T. Recent randomized controlled trials in pancreaticoduodenectomy. Pancreas. 2006;33:228–32. [DOI] [PubMed] [Google Scholar]
- 9. Pawlik TM, Abdalla EK, Barnett CC, Ahmad SA, Cleary KR, Vauthey JN, et al. Feasibility of a randomized trial of extended lymphadenectomy for pancreatic cancer. Arch Surg. 2005;140(6):589–91;discussion 589–591. [DOI] [PubMed] [Google Scholar]
- 10. Katz MH, Merchant NB, Brower S, Branda M, Posner MC, William Traverso L, et al. Standardization of surgical and pathologic variables is needed in multicenter trials of adjuvant therapy for pancreatic cancer: results from the ACOSOG Z5031 trial. Ann Surg Oncol. 2011;18:337–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Probst P, Huttner FJ, Meydan O, Kalkum E, Kretschmer R, Jensen K, et al. Evidence map of pancreatic surgery: protocol for a living systematic review and meta‐analysis. BMJ Open. 2019;9:e032353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Comprehensive Cancer Network . NCCN Clinical Practice Guidelines in Oncology: Pancreatic Adenocarcinoma, Version 2.2021 [Internet]. Plymouth Meeting, PA: National Comprehensive Cancer Network; c2021 [cited 2021 Apr 7]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf [Google Scholar]
- 13. Khorana AA, McKernin SE, Berlin J, Hong TS, Maitra A, Moravek C, et al. Potentially curable pancreatic adenocarcinoma: ASCO clinical practice guideline update. J Clin Oncol. 2019;37:2082–8. [DOI] [PubMed] [Google Scholar]
- 14. Ducreux M, Cuhna AS, Caramella C, Hollebecque A, Burtin P, Goéré D, et al. Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow‐up. Ann Oncol. 2015;26(Suppl 5):v56–68. [DOI] [PubMed] [Google Scholar]
- 15. Japan Pancreas Society . Classification of pancreatic carcinoma (4th edn). Tokyo: Kanehara & Co., Ltd.; 2017. [Google Scholar]
- 16. Bockhorn M, Uzunoglu FG, Adham M, Imrie C, Milicevic M, Sandberg AA, et al. Borderline resectable pancreatic cancer: a consensus statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2014;155:977–88. [DOI] [PubMed] [Google Scholar]
- 17. Klaiber U, Probst P, Strobel O, Michalski CW, Dörr‐Harim C, Diener MK, et al. Meta‐analysis of delayed gastric emptying after pylorus‐preserving versus pylorus‐resecting pancreatoduodenectomy. Br J Surg. 2018;105:339–49. [DOI] [PubMed] [Google Scholar]
- 18. Yang DJ, Xiong JJ, Liu XT, Li J, Dhanushka Layanthi Siriwardena KM, Hu WM. Total pancreatectomy compared with pancreaticoduodenectomy: a systematic review and meta‐analysis. Cancer Manag Res. 2019;11:3899–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kang MJ, Jang JY, Kim SW. Surgical resection of pancreatic head cancer: What is the optimal extent of surgery? Cancer Lett. 2016;382:259–65. [DOI] [PubMed] [Google Scholar]
- 20. Jang JY, Kang MJ, Heo JS, Choi SH, Choi DW, Park SJ, et al. A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg. 2014;259:656–64. [DOI] [PubMed] [Google Scholar]
- 21. Inoue Y, Saiura A, Yoshioka R, Ono Y, Takahashi M, Arita J, et al. Pancreatoduodenectomy with systematic mesopancreas dissection using a supracolic anterior artery‐first approach. Ann Surg. 2015;262:1092–101. [DOI] [PubMed] [Google Scholar]
- 22. Yamada S, Satoi S, Takami H, Yamamoto T, Yoshioka I, Sonohara F, et al. Multicenter randomized phase II trial of prophylactic right‐half dissection of superior mesenteric artery nerve plexus in pancreatoduodenectomy for pancreatic head cancer. Ann Gastroenterol Surg. 2021;5:111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Inoue Y, Saiura A, Oba A, Kawakatsu S, Ono Y, Sato T, et al. Optimal extent of superior mesenteric artery dissection during pancreaticoduodenectomy for pancreatic cancer: balancing surgical and oncological safety. J Gastrointest Surg. 2019;23:1373–83. [DOI] [PubMed] [Google Scholar]
- 24. Ramia JM, De‐la‐Plaza R, Manuel‐Vazquez A, Lopez‐Marcano A, Morales R. Systematic review of the mesopancreas: concept and clinical implications. Clin Transl Oncol. 2018;20:1385–91. [DOI] [PubMed] [Google Scholar]
- 25. Nakao A, Takagi H. Isolated pancreatectomy for pancreatic head carcinoma using catheter bypass of the portal vein. Hepatogastroenterology. 1993;40:426–9. [PubMed] [Google Scholar]
- 26. Pessaux P, Varma D, Arnaud JP. Pancreaticoduodenectomy: superior mesenteric artery first approach. J Gastrointest Surg. 2006;10:607–11. [DOI] [PubMed] [Google Scholar]
- 27. Shukla PJ, Barreto G, Pandey D, Kanitkar G, Nadkarni MS, Neve R, et al. Modification in the technique of pancreaticoduodenectomy: supracolic division of jejunum to facilitate uncinate process dissection. Hepatogastroenterology. 2007;54:1728–30. [PubMed] [Google Scholar]
- 28. Hirota M, Kanemitsu K, Takamori H, Chikamoto A, Tanaka H, Sugita H, et al. Pancreatoduodenectomy using a no‐touch isolation technique. Am J Surg. 2010;199:e65–8. [DOI] [PubMed] [Google Scholar]
- 29. Weitz J, Rahbari N, Koch M, Buchler MW. The "artery first" approach for resection of pancreatic head cancer. J Am Coll Surg. 2010;210:e1–4. [DOI] [PubMed] [Google Scholar]
- 30. Kurosaki I, Minagawa M, Takano K, Takizawa K, Hatakeyama K. Left posterior approach to the superior mesenteric vascular pedicle in pancreaticoduodenectomy for cancer of the pancreatic head. JOP. 2011;12:220–9. [PubMed] [Google Scholar]
- 31. Sanjay P, Takaori K, Govil S, Shrikhande SV, Windsor JA. 'Artery‐first' approaches to pancreatoduodenectomy. Br J Surg. 2012;99:1027–35. [DOI] [PubMed] [Google Scholar]
- 32. Mitchem JB, Hamilton N, Gao F, Hawkins WG, Linehan DC, Strasberg SM. Long‐term results of resection of adenocarcinoma of the body and tail of the pancreas using radical antegrade modular pancreatosplenectomy procedure. J Am Coll Surg. 2012;214:46–52. [DOI] [PubMed] [Google Scholar]
- 33. Chun YS. Role of radical antegrade modular pancreatosplenectomy (RAMPS) and pancreatic cancer. Ann Surg Oncol. 2018;25:46–50. [DOI] [PubMed] [Google Scholar]
- 34. Hirano S, Kondo S, Hara T, Ambo Y, Tanaka E, Shichinohe T, et al. Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic body cancer: long‐term results. Ann Surg. 2007;246:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kang MJ, Kim SW. En bloc proximal peri‐mesenteric clearance for pancreatic head cancer surgery. Ann Hepatobiliary Pancreat Surg. 2020;24:389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. de Rooij T, van Hilst J, van Santvoort H, Boerma D, van den Boezem P, Daams F, et al. Minimally Invasive Versus Open Distal Pancreatectomy (LEOPARD): A Multicenter Patient‐blinded Randomized Controlled Trial. Ann Surg. 2019;269:2–9. [DOI] [PubMed] [Google Scholar]
- 37. van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD‐2): a multicentre, patient‐blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 2019;4:199–207. [DOI] [PubMed] [Google Scholar]
- 38. Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, et al. The Miami International Evidence‐based Guidelines on Minimally Invasive Pancreas Resection. Ann Surg. 2020;271:1–14. [DOI] [PubMed] [Google Scholar]
- 39. Kawaida H, Kono H, Hosomura N, Amemiya H, Itakura J, Fujii H, et al. Surgical techniques and postoperative management to prevent postoperative pancreatic fistula after pancreatic surgery. World J Gastroenterol. 2019;25:3722–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jang JY, Chang YR, Kim SW, Choi SH, Park SJ, Lee SE, et al. Randomized multicentre trial comparing external and internal pancreatic stenting during pancreaticoduodenectomy. Br J Surg. 2016;103:668–75. [DOI] [PubMed] [Google Scholar]
- 41. Kang MJ, Jang JY, Kwon W, Kim SW. Clinical significance of defining borderline resectable pancreatic cancer. Pancreatology. 2018;18:139–45. [DOI] [PubMed] [Google Scholar]
- 42. Katz MH, Pisters PW, Evans DB, Sun CC, Lee JE, Fleming JB, et al. Borderline resectable pancreatic cancer: the importance of this emerging stage of disease. J Am Coll Surg. 2008;206(5):833–46;discussion 846–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Isaji S, Mizuno S, Windsor JA, Bassi C, Fernández‐del Castillo C, Hackert T, et al. International consensus on definition and criteria of borderline resectable pancreatic ductal adenocarcinoma 2017. Pancreatology. 2018;18:2–11. [DOI] [PubMed] [Google Scholar]
- 44. Kato H, Horiguchi A, Ito M, Asano Y, Arakawa S. Essential updates 2019/2020: Multimodal treatment of localized pancreatic adenocarcinoma: Current topics and updates in survival outcomes and prognostic factors. Ann Gastroenterol Surg. 2021;5:132–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wang ZJ, Arif‐Tiwari H, Zaheer A, Ameli S, Bhosale PR, Do RK, et al. Therapeutic response assessment in pancreatic ductal adenocarcinoma: society of abdominal radiology review paper on the role of morphological and functional imaging techniques. Abdom Radiol (NY). 2020;45:4273–89. [DOI] [PubMed] [Google Scholar]
- 46. Satoi S, Yamamoto T, Yamaki S, Sakaguchi T, Sekimoto M. Surgical indication for and desirable outcomes of conversion surgery in patients with initially unresectable pancreatic ductal adenocarcinoma. Ann Gastroenterol Surg. 2020;4:6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. American Joint Committee for Cancer Staging and End Results Reporting . Manual for Staging of Cancer 1977. Chicago, Ill: American Joint Committee on Cancer; 1977. [Google Scholar]
- 48. Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A. Redefining the R1 resection in pancreatic cancer. Br J Surg. 2006;93:1232–7. [DOI] [PubMed] [Google Scholar]
- 49. The Royal College of Pathologists . Standards and minimum datasets for reporting cancers. Minimum dataset for the histopathological reporting of pancreatic, ampulla of Vater and bile duct carcinoma. 2002. The Royal College of Pathologists. [Google Scholar]
- 50. Campbell F, Smith RA, Whelan P, Sutton R, Raraty M, Neoptolemos JP, et al. Classification of R1 resections for pancreatic cancer: the prognostic relevance of tumour involvement within 1 mm of a resection margin. Histopathology. 2009;55:277–83. [DOI] [PubMed] [Google Scholar]
- 51. Demir IE, Jager C, Schlitter AM, Konukiewitz B, Stecher L, Schorn S, et al. R0 Versus R1 Resection Matters after Pancreaticoduodenectomy, and Less after Distal or Total Pancreatectomy for Pancreatic Cancer. Ann Surg. 2018;268:1058–68. [DOI] [PubMed] [Google Scholar]
- 52. Chandra R. Being at Home. Lulu.com. 2014.
- 53. Hein P. [Quoted in] Duane Preble. Man creates art creats man 1973:14.
- 54. Waghorn DJ, Mayon‐White RT. A study of 42 episodes of overwhelming post‐splenectomy infection: is current guidance for asplenic individuals being followed? J Infect. 1997;35:289–94. [DOI] [PubMed] [Google Scholar]
- 55. Warshaw AL. Conservation of the spleen with distal pancreatectomy. Arch Surg. 1988;123:550–3. [DOI] [PubMed] [Google Scholar]
- 56. Miura F, Takada T, Asano T, Kenmochi T, Ochiai T, Amano H, et al. Hemodynamic changes of splenogastric circulation after spleen‐preserving pancreatectomy with excision of splenic artery and vein. Surgery. 2005;138:518–22. [DOI] [PubMed] [Google Scholar]
- 57. Kimura W, Inoue T, Futakawa N, Shinkai H, Han I, Muto T. Spleen‐preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery. 1996;120:885–90. [DOI] [PubMed] [Google Scholar]
- 58. Nakata K, Shikata S, Ohtsuka T, Ukai T, Miyasaka Y, Mori Y, et al. Minimally invasive preservation versus splenectomy during distal pancreatectomy: a systematic review and meta‐analysis. J Hepatobiliary Pancreat Sci. 2018;25:476–88. [DOI] [PubMed] [Google Scholar]
- 59. Malleo G, Damoli I, Marchegiani G, Esposito A, Marchese T, Salvia R, et al. Laparoscopic distal pancreatectomy: analysis of trends in surgical techniques, patient selection, and outcomes. Surg Endosc. 2015;29:1952–62. [DOI] [PubMed] [Google Scholar]
- 60. Yoon YS, Lee KH, Han HS, Cho JY, Ahn KS. Patency of splenic vessels after laparoscopic spleen and splenic vessel‐preserving distal pancreatectomy. Br J Surg. 2009;96:633–40. [DOI] [PubMed] [Google Scholar]
- 61. Yoon YS, Lee KH, Han HS, Cho JY, Jang JY, Kim S‐W, et al. Effects of laparoscopic versus open surgery on splenic vessel patency after spleen and splenic vessel‐preserving distal pancreatectomy: a retrospective multicenter study. Surg Endosc. 2015;29:583–8. [DOI] [PubMed] [Google Scholar]
- 62. Appleby LH. The coeliac axis in the expansion of the operation for gastric carcinoma. Cancer. 1953;6:704–7. [DOI] [PubMed] [Google Scholar]
- 63. Hishinuma S, Ogata Y, Matusui J, et al. Two cases of cancer of the pancreatic body undergoing gastric preservation with distal pancreatectomy combined with resection of the celiac axis. Jpn J Gastroenterol Surg. 1991;24:2782–6. [Google Scholar]
- 64. Nagino M, Nimura Y, Hayakawa N, Kamiya J, Kondo S. Appleby's operation for pancreas cancer. Tan to Sui. 1991;12:1361–8. [Google Scholar]
- 65. Mollberg N, Rahbari NN, Koch M, Hartwig W, Hoeger Y, Büchler MW, et al. Arterial resection during pancreatectomy for pancreatic cancer: a systematic review and meta‐analysis. Ann Surg. 2011;254:882–93. [DOI] [PubMed] [Google Scholar]
- 66. Kondo S, Katoh H, Shimizu T, Omi M, Hirano S, Ambo Y, et al. Preoperative embolization of the common hepatic artery in preparation for radical pancreatectomy for pancreas body cancer. Hepatogastroenterology. 2000;47:1447–9. [PubMed] [Google Scholar]
- 67. Kimura A, Yamamoto J, Aosasa S, Hatsuse K, Nishikawa M, Nishiyama K, et al. Importance of maintaining left gastric arterial flow at Appleby operation preserving whole stomach for central pancreatic cancer. Hepatogastroenterology. 2012;59:2650–2. [DOI] [PubMed] [Google Scholar]
- 68. Sato T, Saiura A, Inoue Y, Takahashi Y, Arita J, Takemura N. Distal Pancreatectomy with En Bloc Resection of the Celiac Axis with Preservation or Reconstruction of the Left Gastric Artery in Patients with Pancreatic Body Cancer. World J Surg. 2016;40:2245–53. [DOI] [PubMed] [Google Scholar]
- 69. Gockel I, Domeyer M, Wolloscheck T, Konerding MA, Junginger T. Resection of the mesopancreas (RMP): a new surgical classification of a known anatomical space. World J Surg Oncol. 2007;5:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Peparini N, Chirletti P. Mesopancreas: a boundless structure, namely R1 risk in pancreaticoduodenectomy for pancreatic head carcinoma. Eur J Surg Oncol. 2013;39:1303–8. [DOI] [PubMed] [Google Scholar]
- 71. Kawabata Y, Tanaka T, Ishikawa N, Hayashi H, Tajima Y. Modified total meso‐pancreatoduodenum excision with pancreaticoduodenectomy as a mesopancreatic plane surgery in borderline resectable pancreatic cancer. Eur J Surg Oncol. 2016;42:698–705. [DOI] [PubMed] [Google Scholar]
- 72. Hirono S, Kawai M, Okada KI, Fujii T, Sho M, Satoi S, et al. MAPLE‐PD trial (Mesenteric Approach vs. Conventional Approach for Pancreatic Cancer during Pancreaticoduodenectomy): study protocol for a multicenter randomized controlled trial of 354 patients with pancreatic ductal adenocarcinoma. Trials. 2018;19(1):613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Jang JY, Kim SW, Han JK, Park S‐J, Park Y‐C, Joon Ahn Y, et al. Randomized prospective trial of the effect of induced hypergastrinemia on the prevention of pancreatic atrophy after pancreatoduodenectomy in humans. Ann Surg. 2003;237:522–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kim SW, Kim KH, Park SJ, Her HH, Jang JY, Park YH. Endogenous gastrin stimulates regeneration of remnant pancreas after partial pancreatectomy. Dig Dis Sci. 2001;46:2134–9. [DOI] [PubMed] [Google Scholar]
- 75. Kim SW, Kim KH, Han JK, Park YH. Pylorus‐preservation decreases the extent of atrophy of the remnant pancreas after pancreatoduodenectomy. HPB. 1999;1:65–70. [Google Scholar]
- 76. Takada T, Yasuda H, Shikata J, Watanabe S, Shiratori K, Takeuchi T. Postprandial plasma gastrin and secretin concentrations after a pancreatoduodenectomy. A comparison between a pylorus‐preserving pancreatoduodenectomy and the Whipple procedure. Ann Surg. 1989;210:47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Tangoku A, Nishikawa M, Adachi A, Suzuki T. Plasma gastrin and cholecystokinin response after pylorus‐preserving pancreatoduodenectomy with Billroth‐I type of reconstruction. Ann Surg. 1991;214:56–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Xu G, Sumi S, Koike M, Tanigawa K, Nio Y, Tamura K. Role of endogenous hypergastrinemia in regenerating endocrine pancreas after partial pancreatectomy. Dig Dis Sci. 1996;41:2433–9. [DOI] [PubMed] [Google Scholar]
- 79. Ohtsuka T, Yamaguchi K, Chijiiwa K, Kinukawa N, Tanaka M. Quality of life after pylorus‐preserving pancreatoduodenectomy. Am J Surg. 2001;182:230–6. [DOI] [PubMed] [Google Scholar]


