Abstract
Eosinophils are leukocytes which reside in the gastrointestinal tract under homeostatic conditions, except for the esophagus which is normally devoid of eosinophils. Research on eosinophils has primarily focused on anti-helminth responses and type 2 immune disorders. In contrast, the search for a role of eosinophils in chronic intestinal inflammation and fibrosis has been limited. With a shift in research focus from adaptive to innate immunity and the fact that the eosinophilic granules are filled with inflammatory mediators, eosinophils are becoming a point of interest in inflammatory bowel diseases. In the current review we summarize eosinophil characteristics and recruitment as well as the current knowledge on presence, inflammatory and pro-fibrotic functions of eosinophils in inflammatory bowel disease and other chronic inflammatory conditions, and we identify research gaps which should be covered in the future.
Keywords: eosinophils, IBD, inflammation, fibrosis, gastrointestinal disorders
1 Introduction
Inflammatory bowel diseases (IBD), further subdivided into Crohn’s disease (CD) and ulcerative colitis (UC), are idiopathic, heterogeneous disorders characterized by a relapsing and remitting disease course (1). Both disorders are believed to result from an inappropriate immune response towards the intestinal microbiota in genetically predisposed patients (1). Although certain genetic risk factors, e.g. polymorphisms in nucleotide-binding oligomerization domain-containing 2 (NOD-2) and autophagy related protein like 1 (ATGL1) have been identified, the exact pathogenesis remains elusive (1, 2).
An excessive immune reaction occurs in response to a loss of the epithelial barrier integrity and damage to tissues, thereby further leading to inflammation (3, 4). This repetitive inflammatory response in IBD patients is considered to contribute to the development of excessive extracellular matrix (ECM) deposition resulting in intestinal fibrosis, especially in CD, due to its transmural character. Stricture formation through fibrosis resulting in complications like intestinal obstruction is the most common indication for surgery in CD patients (5).
Intestinal fibrosis manifests itself only in previously or actively inflamed regions of the gastrointestinal (GI) tract, indicating that inflammation is a sine qua non condition to develop fibrosis (6, 7). Hence, research primarily focused on the inflammatory process, but not on the resulting fibrosis. Repetitive inflammatory injury to the intestine can result in the release of growth factors, thereby stimulating fibroblast proliferation and the differentiation from fibroblasts to myofibroblasts which will ultimately result in excessive deposition of ECM (8). However, the characterization of the key immune cells and their mediators involved in gut fibrogenesis awaits further investigation.
Most studies on the pathogenesis of inflammatory disorders have focused on excessive adaptive immune responses, although recently the focus has shifted to innate immunity (9). In this context, the search for a potential role for involvement of eosinophils in inflammation and fibrosis recently became relevant again (10, 11). Already several decades ago, eosinophils were identified as important contributing cells to the immune cell infiltration in IBD, e.g. with the inclusion of eosinophil infiltration in the lamina propria in the Geboes histological score for UC (12, 13). Furthermore, eosinophilia-associated basal plasmacytosis is considered a hallmark in early diagnosis of IBD and strongly correlated with histological diagnosis (14). Additionally, important eosinophil infiltration in the lamina propria of colonic biopsies in UC patients was previously demonstrated to be the most significant predictor of poor response to medical therapy (15). Moreover, the extensive presence of pre-formed mediators in the eosinophilic granules, known to be involved in inflammation or fibrosis, makes these innate immune cells particularly interesting in the context of fibrostenosis in IBD and in the search of novel treatment targets (9). Although several reports already suggested the eosinophilic granulocytes to be associated with increased levels of inflammation and fibrosis development, a causal role or mechanism has not yet emerged.
In the current review we summarize eosinophil characteristics and recruitment as well as the current knowledge on presence, inflammatory and pro-fibrotic function of eosinophils in IBD and other chronic inflammatory conditions, and we identify research gaps which should be covered in the future.
2 Gastrointestinal Eosinophils
2.1 General Characteristics
Eosinophils are leukocytes that reside in the lamina propria of the gastrointestinal (GI) tract (16, 17). They are normal resident immune cells in the entire GI tract, with exception of the esophagus, where eosinophils are only present under inflammatory conditions such as gastro-esophageal reflux disease and eosinophilic esophagitis (18). Under the influence of interleukin (IL)-3, IL-5 and granulocyte-macrophage colony stimulating factor (GM-CSF), accompanied with a decrease in transcription factor FOG-1 and increased presence of the transcription factors GATA-1, ID2 and XBP1, eosinophils differentiate from pluripotent hematopoietic stem cells in the bone marrow to mature eosinophils ( Figure 1A ) (19–22). In response to IL-5, eosinophils are released into the peripheral circulation ( Figure 1B ), after which they can migrate to the GI tract after binding of chemoattractant molecules, in particular C-C motif ligand 11 (CCL11, eotaxin-1), CCL24 (eotaxin-2), CCL26 (eotaxin-3), CCL5 [Regulated upon activation, normal T cell expressed and secreted (RANTES)], CCL7 [Monocyte chemoattractant protein-3 (MCP-3)] and CCL13 (MCP-4), to their C-C chemokine receptors (CCR) (CCR1, CCR3 and CCR4) ( Figure 1C ) (23). The activation of these receptors triggers both eosinophil recruitment and activation, and thereby induces the production of several cytokines [IL-4, IL-5, IL-13, interferon-gamma (IFN-γ) etc.] and chemokines (CCL3, CCL5, CCL11 etc.) (20). Upon stimulation with cytokines, e.g. IL-4, IL-5 and IL-13, eosinophils will become activated ( Figure 1D ) (24). Eosinophil activation causes degranulation, possibly resulting in damage to the tissue by the release of, amongst others, toxic oxygen radicals, eosinophil cationic protein (ECP) and transforming growth factor β (TGF-β) (11, 25). Eosinophil degranulation therefore contributes to the inflammatory process, in synergy with other inflammatory cells. Among those, the most important ones are Th2 lymphocytes which express the CCR3 membrane receptor and cluster with eosinophils during inflammation (26). It was long believed that eosinophils worked purely as effector cells of the Th2 immune reaction. More recently however, it was discovered eosinophils have their own functionality while still being strongly intertwined with the Th2 lymphocytes (27). In this context, Th2 lymphocytes produce IL-4, IL-5, IL-13 and eotaxins and thereby contribute to the activation and recruitment of eosinophils (28). Eosinophils, on the other hand, produce IL-4 and IL-5, thereby stimulating differentiation of naïve Th0 to Th2 lymphocytes and stimulating Th2 lymphocytes as well (28).
Figure 1.
Pluripotent hematopoeitic stem cells differentiate from the bone marrow to eosinophil progenitors in response to GM-CSF, IL-3, IL-5, a decrease in transcription factor FOG-1 and increased presence of the transcription factors GATA-1, ID2 and XBP1 (A). Under the influence of IL-5 the eosinophil progenitor will be released in the peripheral circulation and further develop into mature eosinophils in the blood (B). By the binding of the chemoattractants (eotaxin-1, eotaxin-2, eotaxin-3, MCP-3, MCP-4 and RANTES) to the chemoattractant receptors (CCR1, CCR3 and CCR4) a chemoattractant gradient is created and the mature eosinophils are recruited to the GI tract (C). The binding of the cytokines IL-4, IL-5 and IL-33, primarily produced by the Th2 cells and ILC2s, to their respective receptor (IL-4R or CD124, IL-5R or CD125 and ST2) causes eosinophil activation and subsequent degranulation releasing TGF-ß, ECP, EPX, EDN and MBP. These factors possibly influence fibroblast activation and differentiation from fibroblasts to myofibroblasts (D). This figure was created via biorender.com.
2.2 Eosinophil Recruitment
Eosinophil recruitment to the GI tract occurs during active inflammation in IBD. In this process, chemoattractant molecules bind to their receptors present on the eosinophil membrane. Besides playing a pivotal role in eosinophil recruitment, the chemoattractant molecules partly serve as eosinophil activators as well (11). Below, we will provide an overview of the known eosinophil chemotaxis pathways.
2.2.1 Eotaxin-1, -2 and -3 – CCR3 Axis
Eotaxin is a potent eosinophil chemoattractant, secreted by eosinophils, macrophages, epithelial cells, mast cells, basophils, Th2 lymphocytes and fibroblasts (29). Eotaxin-1 is believed to be a pivotal chemotactic factor and is constitutively expressed in the small intestine and colon (30–34). Besides its binding capacity to CCR3, eotaxin-1 can furthermore bind to the receptors CCR2, CCR5 and with high affinity to CXCR3, with the latter possibly acting as a decoy receptor by sequestering eotaxin-1 (35, 36). Eotaxin-1 was first established in a guinea-pig model of allergic airway inflammation (37–39). Eotaxin-2 and -3 were later discovered to carry similar functionality concerning eosinophil recruitment (40, 41).
Colonic eotaxin-1,-2 and -3 and CCR3 mRNA expression levels in IBD patients are significantly increased compared to healthy controls (42). Furthermore, serum and tissue eotaxin-1 protein levels correlated with IBD disease severity and eosinophil infiltration (16, 17). The crucial role of eotaxin-1 was confirmed in eotaxin deficient mice, which showed impaired eosinophil recruitment to the colon (42, 43).
Studies in eotaxin-1 deficient mice, however, revealed the chemoattractant not to be essential for the development of airway eosinophilia (44). Moreover, eotaxin-1 knockout mice had only partial eosinophil depletion indicating other chemokines might overcome this deficiency and eotaxin-1 alone is not sufficient to support eosinophil recruitment (45). It is therefore believed that eotaxin-1 mediated eosinophil recruitment is maintained by Th2 lymphocytes by generating IL-4 and IL-5, thereby serving as eosinophil growth and stimulating factors (46).
2.2.2 RANTES, MCP-3 and MCP-4 Mediated Chemotaxis
Besides binding eotaxin-1, 2 and 3, the chemoattractant receptor CCR3 similarly binds RANTES, MCP-3 and MCP-4, resulting in eosinophil chemotaxis (47–49).
Apart from being an eosinophilic chemoattractant, RANTES is a chemotactic for T lymphocytes and basophils as well. The chemokine plays an active role in leukocyte recruitment to inflammatory sites and, together with IL-2 and IFN-gamma, released by T-lymphocytes, it is also responsible for proliferation and activation of natural killer (NK) cells (47). Other than binding to the CCR3 receptor, RANTES also has a binding affinity to CCR1 and CCR4 (48). Protein and mRNA levels of RANTES were demonstrated to be elevated in both UC and CD patients (49).
MCP-3 does not only attract eosinophils, but also functions as a monocyte and neutrophil chemoattractant and regulates macrophage functioning. Apart from binding to CCR3, MCP-3 can also bind to CCR1 (48). Increased MCP-3 expression has been associated with inflammatory diseases, such as allergic inflammation (50). In vivo, MCP-3 antibody mediated neutralization in mouse lung derived endothelial cells resulted in significantly decreased eosinophil accumulation, indicating that MCP-3 is an important and potent chemotactic factor (51).
MCP-4 is a chemoattractant for several cells such as eosinophils, basophils, monocytes, macrophages, immature dendritic cells and T-lymphocytes (48). This chemokine is considered to play a pivotal role in many chronic inflammatory diseases, including allergic airway inflammation and rheumatoid arthritis, by recruiting several cell types to the inflamed tissue followed by activation (52).
Because of the variety of chemoattractants, all with their unique and common features, it is likely that eosinophil chemotaxis is not induced by binding of a single chemoattractant to its receptor, but rather a complex interplay of multiple of the factors described (48).
3 Role of Eosinophils in Inflammation
3.1 Eosinophil Activation
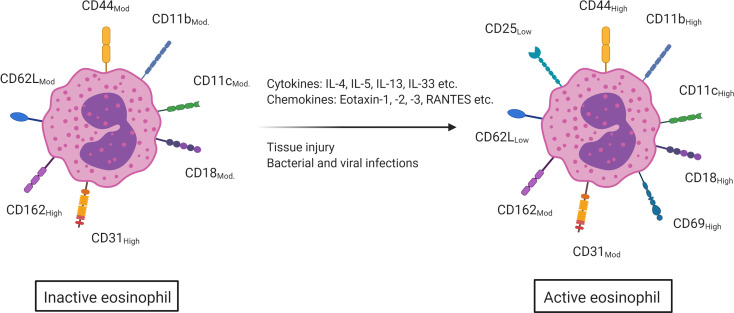
Upon stimulation, activated eosinophils will degranulate and subsequently release their preformed granular content in the environment. Several eosinophil activating mechanisms have been described such as tissue damage, bacterial and viral infections, the binding of cytokines (IL-4, IL-5, IL-13, IL-33, etc.) and the binding of certain chemokines (eotaxin, RANTES, etc.) (53, 54). In humans, this eosinophil activation is characterized by an upregulated expression of the surface markers CD44, CD11c, CD11b and CD18. CD31 and CD162, however, are highly expressed on inactive eosinophils, but become moderately expressed upon activation. While CD25 and CD69 are not present on quiescent eosinophils, they are, respectively, lowly and highly expressed on activated eosinophils. Lastly, the surface marker CD62L is moderately expressed on eosinophils and becomes lowly expressed upon activation ( Figure 2 ) (11, 55). As eosinophil activation is strongly dependent on the cytokine milieu, these markers can help enlighten the not fully understood role of eosinophils in intestinal inflammation (56).
Figure 2.
Upon contact with several cytokines (IL-4, IL-5, IL-13, IL-33, etc.), chemokines (eotaxin-1,2 and -3, RANTES etc.) and via tissue damage and bacterial and viral infections, eosinophils will become activated. This activation is marked by an increased surface expression of CD18, CD44, CD11b and CD11c (moderate to high expression). CD25 and CD69 are not present on inactive eosinophils, but are on active eosinophils (low and high expression respectively). CD162 and CD31 on the other hand are highly expressed on inactive eosinophils but only moderately on active eosinophils and CD62L is moderately expressed on inactive eosinophils but becomes lowly expressed once the eosinophil is activated. This figure was created via biorender.com.
3.1.1 IL-4
IL-4 is a cytokine that is mainly produced by basophils, mast cells, T-lymphocytes, type 2 innate lymphoid cells (ILC2s), eosinophils and neutrophils (57). This cytokine drives differentiation from naïve Th0 to Th2 lymphocytes, which in turn will produce IL-4, thereby creating a positive feedback loop, thereby further enhancing the differentiation of Th2 lymphocytes (58). This pro-inflammatory cytokine is also known to stimulate eosinophil transmigration across the endothelium and the differentiation of Th2 lymphocytes, resulting in cytokine release (59, 60). By increasing eotaxin expression, IL-4 also promotes eosinophil accumulation and eosinophil chemotaxis (61). IL-4 has been linked to several inflammatory disorders, such as asthma and allergic inflammation. The role of IL-4 has already been investigated in the pathogenesis of IBD, where it is suggested to play a pivotal role in inflammation and immune response activation, mainly in UC patients in whom increased expression has been shown (62). Indeed, IL-4 deficiency can prevent the development of colitis in IL-10 knock out mice, which spontaneously develop colitis (63). Additionally, the dextran sodium sulphate (DSS) induced colitis and T cell transfer model also suggest that IL-4 can promote colitis (64–66). Recently, an IL-4/IL-13 dual antagonist was developed and evaluated in a murine model of oxazolone-induced colitis, where it showed to ameliorate overall disease activity (67, 68). IL-4 and IL-13 can also be targeted trough a shared receptor, comprising the IL-4Rα and IL-13α1 chains (69). In this model, blocking IL-4 and IL-13 ameliorated disease severity (70–72). Mice lacking IL-4Rα did not develop disease in this model, further indicating a potential role for IL-4 in the development of colitis and inflammation (73). In contrast, IL-4 mRNA expression levels in CD patients’ intestinal tissue were reduced, corresponding to lower numbers of IL-4 producing cells in mucosal biopsies (74).
3.1.2 IL-5
IL-5 is a chemotactic agent which promotes the differentiation of eosinophils in the bone marrow and can activate eosinophils. In addition, eosinophils produce and secrete IL-5 upon degranulation, thereby promoting their own differentiation and activation, and contributing to their own expansion (75). IL-5 is mainly produced by Th2 lymphocytes and ILC2s, and in lower quantities by NKT cells, mast cells and eosinophils (76–80). ILC2s contribute to the activation of eosinophils by producing IL-4, IL-5, also shown to synergize with eotaxins, and IL-13 (81–83). Specific inhibition of IL-5, by mepolizumab or reslizumab, or specifically blocking the IL-5 receptor, by benralizumab, has been shown to attenuate the type 2 immune response and overall disease severity of eosinophilic asthma patients indicating an important role of IL-5 in eosinophil related disorders (84).
During active inflammation, eosinophils increase IL-4, IL-5 and IL-13 expression, indicating a shift to the Th2 response. Elevated IL-5 levels were found in rectal perfusion fluid from UC patients (85). Mice with DSS induced colitis receiving anti-IL-5 treatment exhibited lower eosinophil expression, more severe weight loss and higher hemoccult scores indicating that IL-5, and eosinophils, may possibly play a protective role in colitis development as well (86). A case report describing a beneficial role of benralizumab in an UC patient shows additional evidence for an advantageous effect of blocking the IL-5 receptor in UC patients (87).
3.1.3 IL-13
The cytokine IL-13 is produced by Th2 lymphocytes, CD4 cells, NKT cells, mast cells, basophils and eosinophils (88). It has been linked to airway hyperresponsiveness and fibrosis development before, as a mediator of allergic inflammation, and therefore linked to diseases such as asthma (88).
IL-13 and IL-4 share some functionality due to a shared receptor, formed by IL-4Rα and IL-13Rα1. Activation of this shared receptor results in STAT6 signaling and stimulation of the type 2 immunity (89). IL-13 can also bind to IL-13Rα2, which acts as a decoy receptor and therefore inhibits IL-13 signaling (90, 91). IL-13 binds IL-13Rα2 with an affinity about 400-fold higher than IL-4Rα/IL-13Rα1, thereby inhibiting STAT6 signaling and dampening the subsequent type 2 immunity response (92). Other studies, however, do suggest a signaling functionality for IL-13Rα2. Strober et al. described IL-13Rα2 signaling to result in TGF-β1 production thereby possibly providing a contribution to fibrosis in a model of bleomycin induced pulmonary fibrosis and oxazolone colitis. Later, this functionality was proven in a trinitrobenzene sulfonic acid (TNBS) colitis model as well (93).
IL-13Rα2 knockout mice were protected from the induction of colitis in a DSS induced colitis model. This was confirmed by IL-13Rα2 antibody mediated neutralization in 8-12-week-old BALB/c mice which showed significant amelioration in colon health, based on colon pathology score and colon length, compared to wild type (wt) mice after DSS induced colitis (92). However, a previous report demonstrated that IL-13Rα2 knock out mice were not protected from colitis development, but recovered and restored the mucosal layer faster (91). Elevated IL13Rα2 mRNA expression levels in mucosal biopsies from both UC as CD patients during active disease have been reported and have been suggested as a potential biomarker for anti-TNF non-responsiveness (94–96). Although IL-13 has been implicated in the inflammatory response in UC patients, results from clinical trials are disappointing: tralokinumab and anrukinzumab, a human and humanized monoclonal anti-IL13 antibody respectively, did not show any therapeutic benefit (62). Therefore, it is still unclear which role IL-13 plays in the development of IBD, but it seems likely that it could serve as a potential therapeutic target in IBD (70, 97).
3.1.4 IL-33
IL-33 is a pro-inflammatory cytokine secreted by several intestinal cells such as ILC2s, Th2 lymphocytes, epithelial cells, etc. that binds to suppression of tumorigenicity 2 (ST2), present on the eosinophilic membrane, and thereby activating the ST2/IL-33 signaling pathway (98). Upon epithelial damage IL-33 will be released and can directly expand ILC2s, Th2 cells and eosinophils. Via the production of IL-5 and IL-13 and the production of IL-4 and IL-5, the ILC2 and Th2 cells, respectively, can furthermore contribute to the expansion of the eosinophil population (99).
Several studies already proposed a potential involvement for IL-33 in the development of colitis: activated eosinophils, together with increased colonic IL-33 mRNA expression levels which correlated with increased colonic eotaxin-1 expression have been demonstrated in UC patients (100). In both intestinal biopsies from IBD patients as in the colon of SAMP/YitFc mice, which spontaneously develop colitis resembling human CD, ST2/IL-33 signaling caused an eosinophilic infiltration and activation coinciding with a Th2 mediated immune response resulting in the release of IL-4, IL-5 and IL-13 (101–103). Antibody mediated blocking of ST2 in these SAMP/YitFc mice diminished the production of Th2 cytokines, and decreased eosinophil recruitment to the ileum (102). In addition, ST2 knockout in C57BL/6 mice alleviated disease symptoms. This was confirmed in a C57BL/6 mouse model with antibody-mediated blocking of ST2 (104).
3.2 Eosinophil Degranulation
Upon eosinophil activation and subsequent eosinophil degranulation, toxic substances can be released into the environment. Release of the eosinophil specific proteins eosinophil cationic protein (ECP), eosinophil peroxidase (EPO), eosinophil derived neurotoxin (EDN) and eosinophil major basic protein (MBP) were described to cause tissue damage via its cytotoxic activity, resulting in the destruction of the epithelial layer and thereby contributing to, amongst others, airway damage and possible lung dysfunction (105). Furthermore, the protein TGF-β1, released from the eosinophil granules, has been described to contribute to inflammation and fibrosis as well (106).
MBP is located in the core of the eosinophilic granule while ECP, EPO and EDN are stored in the surrounding matrix (107). Eosinophil degranulation occurs via four different mechanisms; classical exocytosis, compound exocytosis, piecemeal degranulation and cytolysis (107). It is also known that asthmatic patients’ eosinophils tend to produce more reactive oxygen species compared to healthy controls. Nitric oxide levels, believed to be a marker for the level of eosinophilic inflammation in the lower airways, are elevated in bronchial asthmatic patients and are used in diagnosis of asthma (107).
The contribution of these proteins in the development of intestinal inflammation are discussed below.
3.2.1 Transforming Growth Factor β1 (TGF-β1)
TGF-β is a cytokine produced by fibroblasts, epithelial cells and immune cells (108). Three different human isoforms exist: TGF-β1, which is the most abundant form in the GI tract, TGF-β2 and TGF-β3 (109).
The role of TGF-β1, present in the eosinophilic granules, in acute intestinal inflammation is still elusive with contradictory results in the literature (110). While some studies reported increased TGF-β1 levels during active inflammation, others reported decreased levels or no significant differences at all (111, 112). In addition, TGF-β1 deficient mice spontaneously developed colitis (113, 114). Although TGF-β has been linked to inflammation before, its more important role is attributed to chronic inflammation and subsequent fibrosis which is discussed in detail in the next section (115).
3.2.2 Eosinophil Cationic Protein (ECP)
Upon eosinophil degranulation, the eosinophil specific ECP, also known as ribonuclease 3, is released. The protein with a molecular weight ranging from 18 to 22 kDa is encoded by the Ribonuclease A family member 3 gene (116). ECP can damage cell membranes by the formation of pores into transmembrane channels through which toxic molecules can enter the cell (117, 118). Eosinophils house large amounts of ECP that are released upon degranulation and therefore no de novo synthesis is required at the time of degranulation (118).
Patients with active CD or UC had elevated serum ECP levels compared to healthy individuals or IBD patients in remission (119). This study furthermore revealed faecal ECP (fECP) to be elevated in both CD and UC patients. The diagnostic accuracy for differentiating IBD patients with active from inactive disease however was lower for fECP compared to fecal calprotectin (fCal). High fECP levels nevertheless did correlate with a necessity for treatment alteration or surgical intervention indicating fECP could be used as a diagnostic tool for remission of the IBD patients (120). Furthermore, increased ECP and MBP deposition was demonstrated in the small bowel of eosinophilic gastroenteritis patients and correlated with disease severity (118). Even though reports have shown increased ECP levels during active inflammation in IBD and related conditions, a causal relationship and conclusive evidence for ECP as a mediator in inflammation is lacking.
3.2.3 Eosinophil Peroxidase (EPO)
The toxic cationic EPO forms hypohalous, hypobromous and hypochlourous acid by using hydrogen peroxide, halide ions and bromide via the formation of these acids, EPO can cause cellular damage (121, 122).
Colonic mucosal biopsies from CD patients and colonic perfusion fluids from UC patients express elevated EPO levels during active disease (123–125). Further evidence suggests EPO to be significantly upregulated in tissue of IBD patients at diagnosis, but decreased again during the disease course (126). EPO causes damage to structures via nitrate oxidation, and thereby producing toxic reactive oxygen species (127, 128). These reactive oxygen species have previously been linked to renal inflammation and fibrosis (129). A murine DSS colitis model furthermore revealed EPO release into the lumen of the colon and EPO deficient mice showed amelioration in colitis after induction of experimental colitis via DSS, suggesting a potential role of EPO in chronic intestinal inflammation (130).
3.2.4 Eosinophil Derived Neurotoxin (EDN)
Unlike the name would suggest, EDN is not neurotoxic for humans. The protein received its name because intracerebral EDN injection showed neuropathological responses in a murine model (122).
Amcoff et al. reported increased fecal EDN protein levels in UC patients not only during but also three months prior to relapse. Therefore, faecal EDN has been proposed as a biomarker or predictor of relapse (131). This prognostic role for EDN in eosinophil mediated intestinal inflammation has also been suggested in pediatric patients (132). EDN might therefore possibly serve as a diagnostic tool or biomarker for gastrointestinal inflammation. Whether the protein additionally contributes directly to inflammation or fibrosis development is still up for debate.
3.2.5 Eosinophil Major Basic Protein (MBP)
MBP, often called proteoglycan2 (PRG2) is encoded by the PRG2 gene and has two homologues, MBP1 and MBP2. While MBP1 can be detected in eosinophils, basophils and mast cells, MBP2 is only present in eosinophils (133). Due to its cationic nature, MBP can disturb permeability and cell membrane functioning as well (117).
It is believed MBP directly increases the epithelial layer permeability via its toxicity (134). In vitro co-culture of eosinophils and epithelial cells decreased the integrity of the epithelial barrier, which has been attributed to MBP (135). MBP knock out mice do not develop colitis upon oxazolone exposure, indicating a potential role for MBP in intestinal inflammation (135).
In summary (compiled in Table 1 ), eosinophils have been implicated in the inflammatory process in IBD patients (11). Studies have demonstrated an increased number of activated eosinophils in both active and inactive UC compared to healthy controls (25). As the presence of activated eosinophils was more pronounced in quiescent UC compared to active UC, eosinophils have also been suggested to be involved in tissue repair and remodeling mechanisms (25). Moreover, an increased number of degranulated eosinophils and eosinophil granule protein levels has been demonstrated in tissue samples from IBD patients (136). Peripheral blood eosinophilia was furthermore associated with worse clinical outcomes and more severe disease in UC patients (137, 138). In vivo, IL-4 production by eosinophils has been shown to promote colitis in both the chemically induced dextran sodium sulphate (DSS), as well as in the T cell transfer model (139). Even though several reports suggest a role for eosinophils in inflammation, conclusive evidence is lacking and therefore requires further investigation.
Table 1.
Role of eosinophil activating mediators and compounds from eosinophil specific granules in intestinal inflammation.
| Pre-clinical evidence | Clinical evidence | |
|---|---|---|
| IL-4 | ◊ IL-4 blocking in IL-10 deficient mice: protected from colitis development (63) ◊ No IL-4Rα: no disease development (73) |
◊ UC patients: ↑ IL-4 expression levels in inflamed mucosa (62) ◊ CD patients: ↓ IL-4 levels in intestinal tissue due to lower numbers of IL-4 producing cells in mucosal biopsies (74) |
| ◊ IL-4/IL-13 dual antagonist in oxazolone colitis model (67, 68) - Reduced overall disease activity ◊ IL-4/IL-13 blocking trough a shared receptor (69, 71) - Reduced overall disease severity |
||
| IL-13 | ◊ CD and UC patients: ↑ IL-13Rα2 in mucosal biopsies (94, 95) ◊ Potential biomarker for anti-TNF non-responsiveness (96) ◊ Clinical trial with Tralokinumab and Anrukinzumab: no therapeutic effects (62) |
|
◊ {IL-13Rα2 KO model
 DSS model: mice protected ssssss from colitis introduction (92) DSS model: mice protected ssssss from colitis introduction (92)◊ IL-13Rα2 KO model: not protected from colitis development but recovered faster (91) |
||
| IL-5 | ◊ {Mepolizumab & Reslizumab Benralizumab  Attenuates type 2 response + used and shown effective in eosnophl eosinophilic asthma patients Attenuates type 2 response + used and shown effective in eosnophl eosinophilic asthma patients◊ UC patients’ rectal perfusion fluids (84): - ↑ IL-5 levels |
|
| IL-33 | ◊ SAMP/YitFc colitis model and antibody mediated ST2 blocking (102): - ↓ Th2 cytokine production and ↓ eosinophil recruitment into the ileum ◊ C57BL/6 ST2 KO mice (104) and ST2 antibody mediated depletion in C57BL/6 mice alleviated disease symptoms |
◊ UC patients: ↑ colonic IL-33 mRNA levels and activated eosinophils (100) ◊ IBD patients’ intestinal biopsies (101–103): - ST2/IL-33 signaling - Eosinophil infiltration which coincided with Th2 mediated immune response - IL-4, IL-5 and IL-13 release |
| TGF-β1 | ◊ TGF-β1 deficient mice: spontaneously develop colitis (113, 114) | ◊ Active inflammation in IBD patients: ↑ }TGF-β1 protein levels ↓ (111, 112) = |
| EDN | ◊ UC patients: ↑ f(EDN) protein levels during and 3 months prior to relapse: possible prognostic role (131) ◊ Suggested as a prognostic marker in paediatric patients (132) |
|
| ECP | ◊ Active CD and UC: ↑ serum ECP compared to HC (118) | |
| ◊ Eosinophil gastroenteritis: ECP and MBP deposition in small bowel (119) | ||
| MBP | ◊ MBP KO mice: no colitis development upon oxazolone exposure (135) ◊ In vitro co-culture of eosinophils and epithelial cells decreased functioning of the epithelial barrier - attributed to MBP (135) |
|
| ◊ MBP directly increases epithelial layer permeability via its toxicity (134) | ||
| EPX | ◊ DSS colitis model: ↑ EPX release in colonic lumen (130) ◊ EPX-/- mice: colitis amelioration (130) |
◊ CD patients’ colonic mucosal biopsies and UC patients’ colonic perfusion fluids - ↑ EPX levels during active disease (123–125) ◊ IBD patients: EPX ↑ at diagnosis but decreased again during disease course (126) |
4 Role of Eosinophils in Fibrosis
Because eosinophil infiltration was already shown in other fibrotic diseases, such as endomyocardial fibrosis, idiopathic retroperitoneal fibrosis and pulmonary fibrosis, targeting eosinophils may prove to be beneficial in a number of other fibrotic implications (89, 140). Little is known, however, about the eosinophilic involvement in the development of intestinal fibrosis in IBD. Therefore, the exact mechanism or functioning of the eosinophils in these fibrotic diseases requires further investigation. The involvement of the previously described eosinophil activators and proteins from eosinophil granules in fibrosis will be described below.
4.1 IL-4
IL-4, a potent inducer of TGF-β1, stimulates fibroblast expression and release of inflammatory cytokines, thereby stimulating inflammation and lung remodeling and repair in chronic asthma patients (141). Increased IL-4 expression has been linked to pulmonary fibrosis. In this study, IL-4 deficient mice developed significantly less pulmonary fibrosis than wt mice. On the other hand, the same study showed that IL-4 did not directly stimulate collagen type I expression and alpha smooth muscle actin (α-SMA) proliferation (142). While IL-4 has been associated with idiopathic pulmonary fibrosis (IPF), hepatic fibrosis and cardiac fibrosis (143–146), little is known about the role of IL-4 in the development of intestinal fibrosis.
4.2 IL-5
This cytokine has also been investigated in a variety of chronic fibrotic diseases, such as hepatic fibrosis (89). By using IL-5 knock out C57BL/6 mice, Reiman et al. were able to show a significant reduction in the development of hepatic fibrosis, determined via histopathological analysis, suggesting IL-5 is a potent player in this condition (89). The study demonstrated that IL-5 stimulated the Th2 lymphocyte response and indirectly upregulated IL-13, shown to be a key mediator in the development of fibrosis, indicating IL-5 could have both a direct and an indirect effect on eosinophil mediated liver fibrosis (89). The importance of this Th2 response was later demonstrated in experimental models of pulmonary, renal and intestinal fibrosis (147–149). Moreover, anti-IL-5 mediated treatment depleted the intestinal eosinophils, and suppressed the development of radiation induced intestinal fibrosis (RIF) in mice, demonstrating the importance of eosinophils and IL-5 in the development of RIF (150). Research on IL-5 involvement in the development of intestinal fibrosis however is still limited, highlighting the need for additional research to shed light on the exact pathogenesis.
4.3 IL-13
IL-13 has also been implicated in several fibrotic diseases such as pulmonary, renal, hepatic and intestinal fibrosis and was identified as a possible inducer of airway remodeling in asthma patients (151–154). IL-13, together with IL-4, is responsible for eosinophil activation and additionally can activate and proliferate fibroblasts (155). This cytokine was shown to promote lung fibrosis, and IPF patients exhibited increased IL-4 and IL-13 receptors on lung fibroblasts (155). IL-13 has also been implicated in intestinal fibrosis. Fibrosis in chronic TNBS treated mice seemed driven by IL-13 via TGF-β1 production, and IL-13 blocking resulted in the prevention of intestinal fibrosis (156, 157). Increased IL-4Rα, IL-13Rα1 and IL-13Rα2 levels were found in ileal strictures in CD patients, indicating IL-13 might be involved (62). Even though IL-13 has been implicated in wound repair, tissue remodeling and fibrosis formation, it is not completely understood how it contributes to the development of strictures in CD patients (92). Even if anti-IL13 treatment was not successful to suppress inflammation in UC patients (cf. 2.1.3), its effect on inflammation and especially fibrosis in CD has not been investigated (62).
4.4 IL-33
The co-culture of fibroblasts with eosinophils, activated via IL-33, led to the production and release of components that were associated with chronic intestinal fibrosis, including TGF-β (25). Activating eosinophils via IL-33 and subsequently co-culturing the activated eosinophils with intestinal fibroblasts resulted in the increase of IL-13Rα2, the pro-inflammatory cytokines TNF-α, IL-1β and IL-6 and the chemokines CCL24 and CCL26 (158). The release of these latter two eosinophil chemoattractant molecules possibly results in additional eosinophil recruitment. Co-cultured fibroblasts were isolated and subsequently cultured with IL-13, leading to the production of fibronectin, collagen 1α2 and periostin, which are pro-fibrotic elements. The role of eosinophils in inflammation and fibrosis might therefore be a two-step mechanism (158). Interestingly, IL-33 is also increased in the ileal specimens of paediatric CD patients compared to healthy controls (158).
4.5 TGF-β
TGF-β has been shown to stimulate fibrosis in several organs (1, 159–161). This pro-fibrotic cytokine can affect structural airway cells such as fibroblasts, smooth muscle cells and epithelial cells, and has been implicated in fibrotic diseases such as airway remodeling in asthmatic patients (154). It stimulates fibroblast to myofibroblast activation, and thereby fibrosis (154). In vitro culturing of mucosal fibroblasts derived from UC patients during active disease showed increased production of both TGF-β1 as TGF-β3, while mucosal fibroblasts derived from CD patients during active disease showed increased production of TGF-β1, but less TGF-β3 (162). Increased TGF-β1 levels are similarly observed in mucosal biopsies from CD patients (163). TGF-β,however, is produced by a subset of cells, such as epithelial cells, fibroblasts and immune cells, therefore not specifically indicating a role for eosinophils (108). Future research in which eosinophils and their secreted products, such as TGF-β, are blocked could further help to unravel the specific role of eosinophil derived TGF-β in fibrosis development.
4.6 ECP
This protein has recently been proposed as a possible mediator in tissue remodeling in allergic asthma patients and in patients with eosinophilic esophagitis (164). In the lungs, tissue remodeling occurs via collagen and proteoglycan release from the interstitial fibroblasts. Eosinophils, and ECP in particular, further mediate this process by the production and release of TGF-β (164, 165). Additionally, ECP also causes collagen gel contraction and accumulation of intracellular proteoglycan. ECP might therefore have an indirect effect on fibroblast activation (164). However, conclusive evidence is lacking and additional research is necessary. Moreover, a role for ECP in the development of intestinal fibrosis has not yet been described.
4.7 EPO
EPO knockout mice showed decreased renal fibrosis development (129). These EPO knockout mice also show decreased α-SMA expression and collagen I deposition, indicating a possible involvement in fibrosis development (129). Eosinophils, the source of EPO, also accumulated in the renal interstitium of mice with unilateral ureteral obstruction. Pulmonary epithelial cell exposure to both EPO and MBP resulted in increased mRNA levels of TGF-α, TGF-β1, epidermal growth factor receptor, platelet derived growth factor and tenascin (166). These factors are all associated with fibroblast activation, indicating EPO might be involved in fibrosis development. Again, conclusive evidence is lacking.
5 Other Factors Shaping Eosinophil Function
Neutrophil extracellular traps (NETs), a complex mesh of extracellular fibers primarily consisting of neutrophil DNA have been implicated in inflammatory and fibrotic disorders. Thereby, an excess NET production was suggested to be involved in several pulmonary disorders (167). In that context, NETs have been implicated in the activation of lung fibroblasts and differentiation towards myofibroblasts, correlating to an increased collagen and connective tissue growth factor (CTGF) production (168). Similar to what has been proposed in neutrophils, the potential involvement of eosinophil extracellular traps (EET), already indicated to be involved in tissue damage in the airways of patients suffering from asthma, should be further explored in the context of fibrosis development (169).
Additionally, several studies have indicated a link between the microbiome and intestinal eosinophils. Previously, a significantly higher abundance of eosinophils was shown in germ-free mice compared to pathogen-free mice, suggesting that the microbiome dampens eosinophil proliferation (170). Furthermore, when germ-free mice were exposed to a complex microbiome, a significant decrease in eosinophil numbers was shown (170). Moreover, recent data has shown that high eosinophil presence, resulting from helminth infections, can lead to tissue fibrosis (171). The microbiome therefore clearly has a direct effect on eosinophil numbers and possibly eosinophil functioning.
Lastly, as eosinophils are generally present in the GI tract under homeostatic conditions, they are believed to have a beneficial role in the maintenance of tissue homeostasis. This beneficial role is believed to occur via the preserving of IgA producing plasma B cells, thereby promoting Peyer’s patch development and regulating intestinal microbiota composition. Furthermore, eosinophils are considered to enhance intestinal mucus secretion, thereby supporting the epithelial barrier integrity. Lastly, eosinophils have been described to secrete the IL-1 receptor antagonist IL-1Rα thereby inhibiting IL-1β production resulting in decreased Th17 differentiation. As Th17 cells are the main producers of the profibrotic cytokine IL-17A, eosinophils can fulfill an anti-fibrotic role as well (172).
6 Treatment Options: Targeting Eosinophils in IBD
At diagnosis, patients with IBD are often treated with corticosteroids in a tapering schedule to quickly improve symptoms ( Table 2 ) (189, 190). Corticosteroids prevent eosinophil accumulation, reduce eosinophil chemotaxis and can block other eosinophil factors, including in vitro eosinophil adherence (173, 174). Corticosteroids also have a known anti-fibrotic function by reducing collagen synthesis, which is also related to their negative effect on wound healing (175). This anti-fibrotic effect has been demonstrated in several diseases such as idiopathic pulmonary fibrosis, systemic sclerosis and retroperitoneal fibrosis (176–180). However, long-term corticosteroid exposure is not recommended due to systemic side effects (189).
Table 2.
Conventional treatment options for IBD patients.
| Treatment | Influence on eosinophil presence | Influence on fibrostenosis development |
|---|---|---|
| Corticosteroids | Prevent eosinophil accumulation and reduce eosinophil chemotaxis and can block other eosinophil factors (173, 174). | Demonstrated in idiopathic pulmonary fibrosis, systemic sclerosis and retroperitoneal fibrosis: affects wound healing and reduces collagen synthesis (175–180). |
| Anti-α4β7 integrin (Vedolizumab) | Possible ↓ in influx of eosinophils, but inconclusive evidence (181) ◊ Vedolizumab: no effect on eosinophil circulation ◊ Natalizumab:
|
No effects described in literature. |
| Anti-TNF (infliximab and adalimumab) | No effect described in literature. | Infliximab: suggested to be effective in the early stages of fibrosis development - ↓ in bFGF and VEGF levels in serum (182). - In vitro exposure of myofibroblasts, isolated from CD patients, to infliximab: ↓ collagen production (183). Adalimumab: CREOLE study - CD patients with small bowel strictures: beneficial effect (184) |
| Anti-IL-12/IL-23 (Ustekinumab) | No effect described in literature. | No effect described in literature. |
| JAK inhibitor (Tofacitinib) | Effective in several eosinophil related disorders (185–187) - ↓ in eosinophil numbers - ↓ in disease symptoms |
|
| BAL (Bronchoalveolar lavage) fluid in mice treated with Tofacitinib (188): - eosinophil presence reduced (188). - ↓ in [TGF-β] - ↓ myofibroblasts deposited in pulmonary arteries | ||
The IBD therapeutic landscape has changed entirely with the availability of several biological agents and small molecules in the past two decades ( Table 2 ). However, the direct effect of these biologicals on eosinophil presence, activation and degranulation is still largely unknown. Mucosal addressin cell adhesion molecule 1 (MadCAM-1), expressed on the vascular endothelium in the intestinal tract, will bind α4β7-integrin, present on the eosinophil surface. This α4β7-integrin/MadCAM-1 binding causes eosinophilic recruitment to the GI tract (191). It would therefore be expected that anti-α4β7-integrin treatment would affect intestinal eosinophil recruitment. However, only inconclusive evidence is available in literature: while Bochner and colleagues reported no effect on eosinophil circulation after vedolizumab treatment (181), natalizumab, a humanized anti-α4β1 and α4β7-integrin antibody approved for treatment of systemic sclerosis, caused an increase in circulating eosinophils and a decreased accumulation of eosinophils at the site of inflammation (181). Non-responders to vedolizumab treatment had higher baseline colonic mucosal mean eosinophil counts. Whether this increased baseline eosinophil count could be used as a predictor for non-response to the humanized antibody vedolizumab should be further investigated (192). While no effects of infliximab treatment on eosinophil presence and activation status have been described, infliximab has been suggested to be effective in the early stages of fibrosis development. Patients treated with infliximab, a chimeric antibody targeting TNF-α, exhibited a decrease in serum levels of basic fibroblast growth factor (bFGF) and vascular endothelial growth factor (VEGF) (182). These factors are known to be involved in the development of intestinal fibrosis; bFGF promotes fibroblast proliferation and VEGF stimulates fibroblast activation and ECM synthesis (193, 194). In vitro exposure of myofibroblasts, isolated from CD patients’ active lesions, to infliximab moreover reduced collagen production (183). In the CREOLE study, 97 CD patients with small bowel strictures were treated with the human anti-TNF-α therapy adalimumab. Two thirds (63.9%) of CD patients responded successfully (defined as adalimumab continuation without prohibited treatment, endoscopic dilatation or bowel resection) to adalimumab with a sustained response of 45.7% after 3.8 years, indicating that anti-TNF therapy might have a beneficial effect on intestinal strictures (184).
Tofacitinib, the first JAK-inhibitor approved for moderate-to-severe UC, has shown to be an effective therapeutic in several eosinophil related disorders such as hypereosinophilic syndrome, drug-induced hypersensitivity syndrome and eosinophilic esophagitis ( Table 2 ) (185–187). In a pulmonary eosinophilic vasculitis model, the eosinophil abundance in BAL fluid was reduced in 8-week-old C57BL/6 mice treated with tofacitinib. Moreover, decreased TGF-β concentrations were measured in the BAL fluid and less myofibroblasts were deposited in the pulmonary arteries, indicating tofacitinib might not only affect eosinophil infiltration, but could also serve as an anti-fibrotic treatment (188). Nevertheless, tofacitinib failed phase II drug development in patients with luminal CD, and thus no further investigation is scheduled (195). In contrast, the JAK-1 inhibitor filgotinib did show promising efficacy in CD, including a significant decrease in VEGF (196, 197).
Because the eosinophilic role in inflammation and fibrosis is still so little understood, treatments specifically targeting eosinophils are not currently used in IBD patients. Treatments targeting eosinophils in murine models of colitis, however, have shown to decrease inflammation and tissue architecture remodeling (158). Targeting CCR3 or eotaxin seems a potential therapeutic option because of its role in the accumulation of eosinophils, and indeed reduced inflammation in the Samp1/SkuS1c mouse model (198, 199). Targeting eotaxin-1 via an anti-eotaxin-1 monoclonal antibody (mAb) in a chemically induced model of colitis also reduced the overall disease severity, and has proven its efficacy in a RAG1 deficient mouse model of allergic inflammation (200–202). Bertilimumab, a human anti-eotaxin-1 mAb was initially developed for the treatment of allergic disorders (203, 204). The same mAb demonstrated a clear beneficial effect in a DSS colitis, suggesting that it should be considered for development in the treatment of IBD (205).
Benralizumab, a humanized anti-IL-5R mAb causing eosinophil depletion, already proved its efficacy in asthma patients (206). A similar mAb was designed and showed to significantly ameliorate radiation-induced intestinal fibrosis in mice, and could therefore be a potential therapeutic target in a specific subset of IBD patients (150).
Targeting the ST2/IL-33 pathway might alleviate disease symptoms for IBD patients. Several IL-33 blocking antibodies are currently under evaluation for asthma and for chronic obstructive pulmonary disease (COPD). Interfering with ST2, however, should be handled with caution because ST2 is involved in the activation of other cell types such as ILC2s, T lymphocytes, mast cells, basophils and several other immune cells and could thereby indirectly affect other pathways (98).
Lastly, as previously mentioned, a study revealed severe eosinophil infiltration in the lamina propria of colonic biopsies to be the most significant predictor of poor response to medical therapy in UC patient, highlighting once more the importance of eosinophil monitoring in IBD patients (15).
7 Conclusion
Eosinophils and their granular components have been suggested as pivotal players in several inflammatory and fibrotic diseases including IBD. Although various important mediators of eosinophil recruitment and activation are upregulated in IBD patients, an exact pathogenesis or mechanism through which eosinophils would fulfill their function is still not clear. The specific contribution of eosinophil derived proteins, i.e. ECP, EPO, EDN and MBP, is even less understood. However, pro-fibrotic TGF-β released from eosinophils could potentially contribute to intestinal fibrosis in IBD. Published studies mainly provide descriptive data, rather than demonstrating a clear causative role. Further research will therefore be needed in order to determine the role of eosinophil activation and degranulation in inflammation and fibrosis, specifically in the intestine, and to possibly identify novel anti-inflammatory and anti-fibrotic treatments in IBD.
Author Contributions
The original draft was written by IJ. All authors contributed equally in the conceptualization and revising. All authors approved the final version of the review.
Funding
IJ is supported by a KU Leuven grant (ZKD2906-C14/17/097). CB and BV are supported by the Clinical Research Fund KOOR (University Hospitals Leuven, Leuven, Belgium). TV is a Senior Clinical Investigator and LW a doctoral researcher supported by the Research Foundation Flanders (FWO), Belgium.
Conflict of Interest
CB reports consultancy fees from Ablynx. SV reports financial support for research from MSD, AbbVie, Takeda, Pfizer, J&J, lecture fees from MSD AbbVie, Takeda, Ferring, Centocor, Hospira, Pfizer, J&J, Genentech/Roche, consultancy fees from MSD, AbbVie, Takeda, Ferring, Centocor, Hospira, Pfizer, J&J, Genentech/Roche, Celgene, Mundipharma, Celltrion, Second Genome, Prometheus, Shire, Prodigest, Gilead and Galapagos. BV reports financial support for research from Pfizer lecture fees from Abbvie, Biogen, Chiesi, Falk, Ferring, Galapagos, Janssen, MondayNightIBD, MSD, Pfizer, R-Biopharm, Takeda and Truvion, consultancy fees from Applied Strategic, Atheneum, Bristol Myers Squibb, Guidepont, Ipsos, Janssen, Progenity, Sandoz and Takeda. TV reports financial support for research from Danone and MyHealth, has served on the Speaker bureau for Abbott, Fresenius Kabi, Kyowa Kirin, Menarini, Remedus, Takeda and Will Pharma, consultancy fees from Baxter, Dr. Falk Pharma, Takeda, Tramedico, Truvion, VectivBio and Zealand Pharma.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Glossary
| α-SMA | alpha smooth muscle actin |
| ATGL1 | Autophagy related protein like 1 |
| BAL | Bronchoalveolar lavage |
| bFGF | basic fibroblast growth factor |
| CCL | C-C motif ligand |
| CCR | C-C chemokine receptor |
| CD | Crohn’s disease |
| CD | Cluster of differentiation |
| CTGF | Connective tissue growth factor |
| CXCR | C-X-C chemokine receptor |
| DSS | Dextran sodium sulphate |
| ECM | Extracellular matrix |
| ECP | Eosinophil cationic protein |
| EDN | Eosinophil derived neurotoxin |
| EET | Eosinophil extracellular traps |
| EPO | Eosinophil peroxidase |
| fECP | faecal eosinophil peroxidase |
| fCal | faecal calprotectin |
| GI | Gastrointestinal |
| GM-CSF | Granulocyte-macrophage colony-stimulating factor |
| IBD | Inflammatory bowel disease |
| IFN | Interferon |
| IL | Interleukin |
| ILC | Innate lymphoid cell |
| IPF | Idiopathic pulmonary fibrosis |
| IRGM | Immunity related GTPase M |
| JAK | Janus kinase |
| mAb | Monoclonal antibody |
| MadCam | Mucosal addressin cell adhesion molecule |
| MBP | Eosinophil major basic protein |
| MCP | Monocyte chemoattractant protein |
| mRNA | messenger ribonucleic acid |
| NETs | Neutrophil extracellular traps |
| NK | Natural killer |
| NKT | Natural killer T |
| NOD-2 | Nucleotide-binding oligomerization domain-containing protein 2 |
| PRG2 | Proteoglycan 2 |
| RANTES | Regulated upon activation, normal T cell expressed and secreted |
| RIF | Radiation induced fibrosis |
| ST2 | Suppression of tumorigenicity 2 |
| STAT | Signal transducer and activator of transcription |
| TGF | Transforming growth factor |
| TNBS | Trinitrobenzene sulfonic acid |
| TNF | Tumor necrosis factor |
| Th | T helper |
| UC | Ulcerative colitis |
| VEGF | Vascular endothelial growth factor |
| wt | wild type |
References
- 1. De Souza HSP, Fiocchi C. Immunopathogenesis of IBD: Current State of the Art. Nat Rev Gastroenterol Hepatol (2016) 13:13–27. doi: 10.1038/nrgastro.2015.186 [DOI] [PubMed] [Google Scholar]
- 2. Mirkov MU, Verstockt B, Cleynen I. Genetics of Inflammatory Bowel Disease: Beyond NOD2. Lancet (2017) 2:224–34. doi: 10.1016/S2468-1253(16)30111-X [DOI] [PubMed] [Google Scholar]
- 3. Zhang M, Sun K, Wu Y, Yang Y, Tso P, Wu Z. Interactions Between Intestinal Microbiota and Host Immune Response in Inflammatory Bowel Disease. Front Immunol (2017) 8:942. doi: 10.3389/fimmu.2017.00942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coskun M. Intestinal Epithelium in Inflammatory Bowel Disease. Front Med (2014) 1:24. doi: 10.3389/fmed.2014.00024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rieder F, Fiocchi C. Intestinal Fibrosis in IBD - A Dynamic, Multifactorial Process. Nat Rev Gastroenterol Hepatol (2009) 6:228–35. doi: 10.1038/nrgastro.2009.31 [DOI] [PubMed] [Google Scholar]
- 6. Rieder F, Fiocchi C, Rogler G. Mechanisms, Management, and Treatment of Fibrosis in Patients With Inflammatory Bowel Diseases. Gastroenterology (2017) 152:340–50. doi: 10.1053/j.gastro.2016.09.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Henderson NC, Rieder F, Wynn TA. Fibrosis: From Mechanisms to Medicines. Nature (2020) 587:555–66. doi: 10.1038/s41586-020-2938-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Herrera J, Henke CA, Bitterman PB, Herrera J, Henke CA, Bitterman PB. Extracellular Matrix as a Driver of Progressive Fibrosis. J Clin Invest (2018) 128:45–53. doi: 10.1172/JCI93557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shah K, Ignacio A, McCoy KD, Harris NL. The Emerging Roles of Eosinophils in Mucosal Homeostasis. Mucosal Immunol (2020) 13:574–83. doi: 10.1038/s41385-020-0281-y [DOI] [PubMed] [Google Scholar]
- 10. Uhlig HH, Powrie F. Translating Immunology Into Therapeutic Concepts for Inflammatory Bowel Disease. Annu Rev Immunol (2018) 36:755–81. doi: 10.1146/annurev-immunol-042617-053055 [DOI] [PubMed] [Google Scholar]
- 11. Filippone RT, Sahakian L, Apostolopoulos V, Nurgali K. Eosinophils in Inflammatory Bowel Disease. Inflamm Bowel Dis (2019) 25:1140–51. doi: 10.1093/ibd/izz024 [DOI] [PubMed] [Google Scholar]
- 12. Coppi LC, Thomazzi SM, de Ayrizono MLS, Coy CSR, Fagundes WJJ, Goes JRN, et al. Comparative Study of Eosinophil Chemotaxis, Adhesion, and Degranulation In Vitro in Ulcerative Colitis and Crohn’s Disease. Inflamm Bowel Dis (2007) 13:211–8. doi: 10.1002/ibd.20018 [DOI] [PubMed] [Google Scholar]
- 13. Geboes K, Riddell R, Ost A, Jensfelt B, Persson T, Löfberg R. A Reproducible Grading Scale for Histological Assessment of Inflammation in Ulcerative Colitis. Gut (2000) 47:404–9. doi: 10.1136/gut.47.3.404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Canavese G, Villanacci V, Antonelli E, Cadei M, Sapino A, Rocca R, et al. Eosinophilia – Associated Basal Plasmacytosis: An Early and Sensitive Histologic Feature of Inflammatory Bowel Disease. Apmis (2017) 125:179–83. doi: 10.1111/apm.12639 [DOI] [PubMed] [Google Scholar]
- 15. Zezos P, Patsiaoura K, Nakos A, Mpoumponaris A, Vassiliadis T, Giouleme O, et al. Severe Eosinophilic Infiltration in Colonic Biopsies Predicts Patients With Ulcerative Colitis Not Responding to Medical Therapy. Color Dis (2014) 16:O420–30. doi: 10.1111/codi.12725 [DOI] [PubMed] [Google Scholar]
- 16. Mir A, Minguez M, Tatay J, Pascual I, Pena A, Sanchiz V, et al. Elevated Serum Eotaxin Levels in Patients With Inflammatory Bowel Disease. Am J Gastroenterol (2002) 97:1452–7. doi: 10.1111/j.1572-0241.2002.05687.x [DOI] [PubMed] [Google Scholar]
- 17. Chen W, Paulus B, Shu D, Wils I. Increased Serum Levels of Eotaxin in Patients With Inflammatory Bowel Disease. Scand J Gastroenterol (2001) 36:515–20. doi: 10.1080/00365520120163 [DOI] [PubMed] [Google Scholar]
- 18. Runge TM, Dellon ES. Do We Know What Causes Eosinophilic Esophagitis? A Mechanistic Update. Curr Gastroenterol Rep (2015) 176:139–48. doi: 10.1007/s11894-015-0458-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Johnston LK, Bryce PJ. Understanding Interleukin 33 and Its Roles in Eosinophil Development. Front Med (2017) 4:51. doi: 10.3389/fmed.2017.00051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rosenberg HF, Dyer KD, Foster PS. Eosinophils: Changing Perspectives in Health and Disease. Nat Rev Immunol (2013) 13:9–22. doi: 10.1038/nri3341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rothenberg ME, Mishra A, Brandt EB, Hogan SP. Gastrointestinal Eosinophils. Immunol Rev (2001) 179:139–55. doi: 10.1034/j.1600-065X.2001.790114.x [DOI] [PubMed] [Google Scholar]
- 22. Daugherty BL, Siciliano SJ, DeMartino JA, Malkowitz L, Sirotina A, Springer MS. Cloning, Expression, and Characterization of the Human Eosinophil Eotaxin Receptor. J Exp Med (1996) 183:2349–54. doi: 10.1084/jem.183.5.2349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Weller PF, Spencer LA. Functions of Tissue-Resident Eosinophils. Nat Rev Immunol (2017) 17:746–60. doi: 10.1038/nri.2017.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McBrien CN, Menzies-Gow A. The Biology of Eosinophils and Their Role in Asthma. Front Med (2017) 4:93. doi: 10.3389/fmed.2017.00093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Al-Haddad S, Riddell RH. The Role of Eosinophils in Inflammatory Bowel Disease. Gut (2005) 54:1674–5. doi: 10.1136/gut.2005.072595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gerber BO, Zanni MP, Uguccioni M, Loetscher M, Mackay CR, Pichler WJ, et al. Functional Expression of the Eotaxin Receptor CCR3 in T Lymphocytes Co-Localizing With Eosinophils. Curr Biol (1997) 7:836–43. doi: 10.1016/S0960-9822(06)00371-X [DOI] [PubMed] [Google Scholar]
- 27. Spencer LA, Weller PF. Eosinophils and Th2 Immunity: Contemporary Insights. Immunol Cell Biol (2010) 88(3):250–6. doi: 10.1038/icb.2009.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ohta K, Nagase H, Suzukawa M, Ohta S. Antibody Therapy for the Management of Severe Asthma With Eosinophilic Inflammation. Int Immunol (2017) 29:337–43. doi: 10.1093/intimm/dxx045 [DOI] [PubMed] [Google Scholar]
- 29. Rothenberg ME. Eotaxin: An Essential Mediator of Eosinophil Trafficking Into Mucosal Tissues. Am J Respir Cell Mol Biol (1999) 21:291–5. doi: 10.1165/ajrcmb.21.3.f160 [DOI] [PubMed] [Google Scholar]
- 30. Ahrens R, Waddell A, Seidu L, Blanchard C, Carey R, Forbes E, et al. Intestinal Macrophage/Epithelial Cell-Derived CCL11/Eotaxin-1 Mediates Eosinophil Recruitment and Function in Pediatric Ulcerative Colitis. J Immunol (2008) 181(10):7390–9. doi: 10.4049/jimmunol.181.10.7390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kitaura M, Nakajima T, Imai T, Harada S, Combadiere C, Tiffany HL, et al. Molecular Cloning of Human Eotaxin, an Eosinophil-Selective CC Chemokine, and Identification of a Specific Eosinophil Eotaxin Receptor, CC Chemokine Receptor 3. J Biol Chem (1996) 271:7725–30. doi: 10.1074/jbc.271.13.7725 [DOI] [PubMed] [Google Scholar]
- 32. Uguccioni M, Baggiolini M, Dahinden CA. High Expression of the Chemokine Receptor CCR3 in Human Blood Basophils. Role in Activation by Eotaxin, MCP-4, and Other Chemokines. J Clin Invest (1997) 100(5):1137–43. doi: 10.1172/JCI119624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Romagnani P, Paulis A, Beltrame C, Annunziato F, Dente V, Maggi E, et al. Tryptase-Chymase Double-Positive Human Mast Cells Express the Eotaxin Receptor CCR3 and Are Attracted by CCR3-Binding Chemokines. Am J Pathol (1999) 155:1195–204. doi: 10.1016/S0002-9440(10)65222-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sallusto F, Mackay CR, Lanzavecchia A. Selective Expression of the Eotaxin Receptor CCR3 by Human T Helper 2 Cells. Science (80) (1997) 277:2005–8. doi: 10.1126/science.277.5334.2005 [DOI] [PubMed] [Google Scholar]
- 35. Ogilvie P, Bardi G, Clark-lewis I, Baggiolini M, Uguccioni M. Eotaxin Is a Natural Antagonist for CCR2 and an Agonist for CCR5. Blood (2001) 97:1920–4. doi: 10.1182/blood.V97.7.1920 [DOI] [PubMed] [Google Scholar]
- 36. Xanthou G, Duchesnes E, Williams TJ, Pease JE. CCR3 Functional Responses Are Regulated by Both CXCR3 and Its Ligands CXCL9, CXCL10 and CXCL11. Eur J Immunol (2003) 33:2241–50. doi: 10.1002/eji.200323787 [DOI] [PubMed] [Google Scholar]
- 37. Jose BPJ, Grif DA, Collins PD, Walsh DT, Moqbel R, Totty NF, et al. Eotaxin: A Potent Eosinophil Chemoattractant Cytokine Detected in a Guinea Pig Model of Allergic Airways Inflammation. J Exp Med (1994) 179:881–7. doi: 10.1084/jem.179.3.881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rothenberg BME, Luster AD, Lilly CM, Drazen JM, Leder P. Constitutive and Allergen-Induced Expression of Eotaxin mRNA in the Guinea Pig Lung. J Exp Med (1995) 181:1211–6. doi: 10.1084/jem.181.3.1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rankin SM, Conroy DM, Williams TJ. Eotaxin and Eosinophil Recruitment: Implications for Human Disease. Mol Med Today (2000) 6:20–7. doi: 10.1016/S1357-4310(99)01635-4 [DOI] [PubMed] [Google Scholar]
- 40. Petering H, Höchstetter R, Kimmig D, Smolarski R, Kapp A, Elsner J. Detection of MCP-4 in Dermal Fibroblasts and Its Activation of the Respiratory Burst in Human Eosinophils. J Immunol (1998) 160:555–8. [PubMed] [Google Scholar]
- 41. Forssmann U, Uguccioni M, Loetscher P, Dahinden CA, Langen H, Thelen M, et al. Eotaxin-2, a Novel CC Chemokine That Is Selective for the Chemokine Receptor CCR3, and Acts Like Eotaxin on Human Eosinophil and Basophil Leukocytes. J Exp Med (1997) 185:2171–6. doi: 10.1084/jem.185.12.2171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Manousou P, Kolios G, Valatas V, Drygiannakis I, Bourikas L, Pyrovolaki K, et al. Increased Expression of Chemokine Receptor CCR3 and Its Ligands in Ulcerative Colitis: The Role of Colonic Epithelial Cells in In Vitro Studies. Clin Exp Immunol (2010) 162:337–47. doi: 10.1111/j.1365-2249.2010.04248.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Saitoh O, Kojima K, Sugi K, Matsuse R, Uchida K, Tabata K, et al. Fecal Eosinophil Granule-Derived Proteins Reflect Disease Activity in Inflammatory Bowel Disease. Am J Gastroenterol (1999) 94:3513–20. doi: 10.1016/S0002-9270(99)00699-1 [DOI] [PubMed] [Google Scholar]
- 44. Tomkinson A, Duez C, Cieslewicz G, Gelfand E. Eotaxin-1-Deficient Mice Develop Airway Eosinophilia and Airway Hyperresponsiveness. Int Arch Allergy Immunol (2001) 126:119–25. doi: 10.1159/000049502 [DOI] [PubMed] [Google Scholar]
- 45. Rothenberg ME, MacLean JA, Pearlman E, Luster AD, Leder P. Targeted Disruption of the Chemokine Eotaxin Partially Reduces Antigen- Induced Tissue Eosinophilia. J Exp Med (1997) 185:785–90. doi: 10.1084/jem.185.4.785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Amin K, Kristjansson G, Rorsman F, Sangfelt P, Sa B. Eosinophil Granulocytes Are Activated During the Remission Phase of Ulcerative Colitis. Gut (2005) 54(12):1714–20. doi: 10.1136/gut.2005.066423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Donlon T, Krensky A, Wallace M, FS C, Lovett M, Clayberger C. Localization of a Human T-Cell-Specific Gene, RANTES (D17S136E), to Chromosome 17q11.2-q12. Genomics (1990) 553:548–53. doi: 10.1016/0888-7543(90)90485-D [DOI] [PubMed] [Google Scholar]
- 48. Ying S, Meng Q, Zeibecoglou K, Douglas S, Macfarlane A, Humbert M, et al. Eosinophil Chemotactic Chemokines (Eotaxin, Eotaxin-2, RANTES, Monocyte Chemoattractant Protein-3 (MCP-3), and MCP-4), and C-C Chemokine Receptor 3 Expression in Bronchial Biopsies From Atopic and Nonatopic (Intrinsic) Asthmatics. J Immunol (1999) 163:6321–9. [PubMed] [Google Scholar]
- 49. Ansari N, Abdulla J, Zayyani N, Brahmi U, Taha S, Satir AA. Comparison of RANTES Expression in Crohn’s Disease and Ulcerative Colitis: An Aid in the Differential Diagnosis? J Clin Pathol (2006) 59:1066–72. doi: 10.1136/jcp.2005.034983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ford J, Hughson A, Lim K, Bardina SV, Lu W, Charo IF, et al. CCL7 Is a Negative Regulator of Cutaneous Inflammation Following Leishmania Major Infection. Front Immunol (2019) 9:3063. doi: 10.3389/fimmu.2018.03063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Shang XZ, Chiu BC, Stolberg V, Lukacs NW, Kunkel SL, Murphy HS, et al. Eosinophil Recruitment in Type-2 Hypersensitivity Pulmonary Granulomas: Source and Contribution of Monocyte Chemotactic Protein-3 (CCL7). Am J Pathol (2002) 161:257–66. doi: 10.1016/S0002-9440(10)64177-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Mendez-Enriquez E, García-Zepeda EA. The Multiple Faces of CCL13 in Immunity and Inflammation. Inflammopharmacology (2013) 21:397–406. doi: 10.1007/s10787-013-0177-5 [DOI] [PubMed] [Google Scholar]
- 53. Samitas K, Rådinger M, Bossios A. Current Update on Eosinophilic Lung Diseases and Anti-IL-5 Treatment. Recent Pat Antiinfect Drug Discov (2011) 6:189–205. doi: 10.2174/157489111796887855 [DOI] [PubMed] [Google Scholar]
- 54. Soman KV, Stafford SJ, Pazdrak K, Wu Z, Luo X, White WI, et al. Activation of Human Peripheral Blood Eosinophils by Cytokines in a Comparative Time-Course Proteomic/Phosphoproteomic Study. J Proteome Res (2017) 16:2663–79. doi: 10.1021/acs.jproteome.6b00367 [DOI] [PubMed] [Google Scholar]
- 55. Bochner BS. Systemic Activation of Basophils and Eosinophils: Markers and Consequences. J Allergy Clin Immunol (2000) 106:292–302. doi: 10.1067/mai.2000.110164 [DOI] [PubMed] [Google Scholar]
- 56. Lampinen M, Backman M, Winqvist O, Rorsman F, Rönnblom A, Sangfelt P, et al. Different Regulation of Eosinophil Activity in Crohn’s Disease Compared With Ulcerative Colitis. J Leukoc Biol (2008) 84:1392–9. doi: 10.1189/jlb.0807513 [DOI] [PubMed] [Google Scholar]
- 57. Paul WE. History of Interleukin-4. Cytokine (2015) 176:139–48. doi: 10.1016/j.physbeh.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Sokol CL, Barton GM, Farr AG, Medzhitov R. A Mechanism for the Initiation of Allergen-Induced T Helper Type 2 Responses. Nat Immunol (2008) 9:310–8. doi: 10.1038/ni1558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Seder RA, Paul WE, Davis MM, Fazekas de St. Groth B. The Presence of Interleukin 4 During In Vitro Priming Determines the Lymphoklne-Producing Potential of CD4+ T Cells From T Cell Receptor Transgenic Mice. J Exp Med (1992) 176:1091–8. doi: 10.1084/jem.176.4.1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hsieh C, Heimberger A, Gold J, O’Garra A, Murphy K. Differential Regulation of T Helper Phenotype Development by Interleukins 4 and 10 in an Alpha Beta T-Cell-Receptor Transgenic System. Proc Natl Acad Sci (1992) 89:6065–9. doi: 10.1073/pnas.89.13.6065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Dubois GR, Bruijnzeel PL. IL-4-Induced Migration of Eosinophils in Allergic Inflammation. Ann NY Acad Sci (1994) 725:268–73. doi: 10.1111/j.1749-6632.1994.tb39809.x [DOI] [PubMed] [Google Scholar]
- 62. Giuffrida P, Caprioli F, Facciotti F, Di Sabatino A. The Role of Interleukin-13 in Chronic Inflammatory Intestinal Disorders. Autoimmun Rev (2019) 18:549–55. doi: 10.1016/j.autrev.2019.03.012 [DOI] [PubMed] [Google Scholar]
- 63. Specht S, Arriens S, Hoerauf A. Induction of Chronic Colitis in IL-10 Deficient Mice Requires IL-4. Microbes Infect (2006) 8:694–703. doi: 10.1016/j.micinf.2005.09.006 [DOI] [PubMed] [Google Scholar]
- 64. Reichman H, Moshkovits I, Itan M, Pasmanik-Chor M, Vogl T, Roth J, et al. Transcriptome Profiling of Mouse Colonic Eosinophils Reveals a Key Role for Eosinophils in the Induction of s100a8 and s100a9 in Mucosal Healing. Sci Rep (2017) 7:7117. doi: 10.1038/s41598-017-07738-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Griseri T, Arnold IC, Pearson C, Krausgruber T, Schiering C, Franchini F, et al. Granulocyte Macrophage Colony-Stimulating Factor-Activated Eosinophils Promote Interleukin-23 Driven Chronic Colitis. Immunity (2015) 43:187–99. doi: 10.1016/j.immuni.2015.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Waddell A, Ahrens R, Tsai Y-T, Sherrill JD, Denson LA, Steinbrecher KA, et al. Intestinal CCL11 and Eosinophilic Inflammation Is Regulated by Myeloid Cell–Specific RelA/p65 in Mice. J Immunol (2013) 190:4773–85. doi: 10.4049/jimmunol.1200057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kasaian MT, Page KM, Fish S, Brennan A, Cook TA, Moreira K, et al. Therapeutic Activity of an Interleukin-4/Interleukin-13 Dual Antagonist on Oxazolone-Induced Colitis in Mice. Immunology (2014) 143:416–27. doi: 10.1111/imm.12319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kojima R, Kuroda S, Ohkishi T, Nakamaru K, Hatakeyama S. Oxazolone-Induced Colitis in BALB/C Mice: A New Method to Evaluate the Efficacy of Therapeutic Agents for Ulcerative Colitis. J Pharmacol Sci (2004) 96:307–13. doi: 10.1254/jphs.FP0040214 [DOI] [PubMed] [Google Scholar]
- 69. Wills-Karp M, Finkelman FD. Untangling the Complex Web of IL-4-and IL-13-Mediated Signaling Pathways. Sci Signal (2008) 1:1–4. doi: 10.1126/scisignal.1.51.pe55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Heller F, Fuss IJ, Nieuwenhuis EE, Blumberg RS, Strober W. Oxazolone Colitis, a Th2 Colitis Model Resembling Ulcerative Colitis, Is Mediated by IL-13-Producing NK-T Cells. Immunity (2002) 17:629–38. doi: 10.1016/S1074-7613(02)00453-3 [DOI] [PubMed] [Google Scholar]
- 71. Weigmann B, Lehr HA, Yancopoulos G, Valenzuela D, Murphy A, Stevens S, et al. The Transcription Factor NFATc2 Controls IL-6-Dependent T Cell Activation in Experimental Colitis. J Exp Med (2008) 205:2099–110. doi: 10.1084/jem.20072484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Boirivant M, Fuss IJ, Chu A, Strober W. Oxazolone Colitis: A Murine Model of T Helper Cell Type 2 Colitis Treatable With Antibodies to Interleukin 4. J Exp Med (1998) 188:1929–39. doi: 10.1084/jem.188.10.1929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Hoving JC, Kirstein F, Nieuwenhuizen NE, Fick LCE, Hobeika E, Reth M, et al. B Cells That Produce Immunoglobulin E Mediate Colitis in BALB/c Mice. Gastroenterology (2012) 142:96–108. doi: 10.1053/j.gastro.2011.09.044 [DOI] [PubMed] [Google Scholar]
- 74. Karttunnen R, Breese EJ, Walker-Smith JA, MacDonald TT. Decreased Mucosal Interleukin-4 (IL-4) Production in Gut Inflammation. J Clin Pathol (1994) 47:1015–8. doi: 10.1136/jcp.47.11.1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Wallaert B, Desreumaux P, Copin MC, Tillie I, Benard A, Colombel JF, et al. Immunoreactivity for Interleukin 3 and 5 and Granulocyte/Macrophage Colony-Stimulating Factor of Intestinal Mucosa in Bronchial Asthma. J Exp Med (1995) 182:1897–904. doi: 10.1084/jem.182.6.1897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Woodruff PG, Modrek B, Choy DF, Jia G, Abbas AR, Ellwanger A, et al. T-Helper Type 2-Driven Inflammation Defines Major Subphenotypes of Asthma. Am J Respir Crit Care Med (2009) 180:388–95. doi: 10.1164/rccm.200903-0392OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Smith SG, Chen R, Kjarsgaard M, Huang C, Oliveria JP, O’Byrne PM, et al. Increased Numbers of Activated Group 2 Innate Lymphoid Cells in the Airways of Patients With Severe Asthma and Persistent Airway Eosinophilia. J Allergy Clin Immunol (2016) 137:75–86. doi: 10.1016/j.jaci.2015.05.037 [DOI] [PubMed] [Google Scholar]
- 78. Shakoory B, Fitzgerald SM, Lee SA, Chi DS, Krishnaswamy G. The Role of Human Mast Cell-Derived Cytokines in Eosinophil Biology. J Interf Cytokine Res (2004) 24:271–81. doi: 10.1089/107999004323065057 [DOI] [PubMed] [Google Scholar]
- 79. Sakuishi K, Oki S, Araki M, Porcelli SA, Miyake S, Yamamura T. Invariant NKT Cells Biased for IL-5 Production Act as Crucial Regulators of Inflammation. J Immunol (2007) 179:3452–62. doi: 10.4049/jimmunol.179.6.3452 [DOI] [PubMed] [Google Scholar]
- 80. Hogan SP, Rosenberg HF, Moqbel R, Phipps S, Foster PS, Lacy P, et al. Eosinophils: Biological Properties and Role in Health and Disease. Clin Exp Allergy (2008) 38:709–50. doi: 10.1111/j.1365-2222.2008.02958.x [DOI] [PubMed] [Google Scholar]
- 81. Ebbo M, Crinier A, Vély F, Vivier E. Innate Lymphoid Cells: Major Players in Inflammatory Diseases. Nat Rev Immunol (2017) 17:665–78. doi: 10.1038/nri.2017.86 [DOI] [PubMed] [Google Scholar]
- 82. Park SW, Kim DJ, Chang HS, Park SJ, Lee YM, Park JS, et al. Association of Interleukin-5 and Eotaxin With Acute Exacerbation of Asthma. Int Arch Allergy Immunol (2003) 131:283–90. doi: 10.1159/000072140 [DOI] [PubMed] [Google Scholar]
- 83. Fulkerson PC, Rothenberg ME. Targeting Eosinophils in Allergy, Inflammation and Beyond. Nat Rev Drug Discov (2013) 12:117–29. doi: 10.1038/nrd3838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Pelaia C, Paoletti G, Puggioni F, Racca F, Pelaia G, Canonica GW, et al. Interleukin-5 in the Pathophysiology of Severe Asthma. Front Physiol (2019) 10:1514. doi: 10.3389/fphys.2019.01514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Lampinen M, Carlson M, Sangfelt P, Taha Y, Thõrn M, Lõõf L, et al. IL-5 and TNF-α Participate in Recruitment of Eosinophils to Intestinal Mucosa in Ulcerative Colitis. Dig Dis Sci (2001) 46:2004–9. doi: 10.1023/A:1010659803912 [DOI] [PubMed] [Google Scholar]
- 86. Kobayashi T, Iijima K, Kita H. Beneficial Effects of Eosinophils in Colitis Induced by Dextran Sulfate Sodium. J Allergy Clin Immunol (2004) 113:S172. doi: 10.1016/j.jaci.2004.01.053 [DOI] [Google Scholar]
- 87. Sugimoto K, Fujita S, Miyazu T, Ishida N, Tani S, Yamade M, et al. Improvement in Ulcerative Colitis by Administration of Benralizumab for Comorbid Refractory Bronchial Asthma: A Novel Clinical Observation. Inflamm Bowel Dis (2021) 27:E3–4. doi: 10.1093/ibd/izaa225 [DOI] [PubMed] [Google Scholar]
- 88. Rael E, Lockey R. Interleukin-13 Signaling and Its Role in Asthma. World Allergy Organ J (2011) 4:54–64. doi: 10.1097/WOX.0b013e31821188e0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Reiman RM, Thompson RW, Feng CG, Hari D, Knight R, Cheever AW, et al. Interleukin-5 (IL-5) Augments the Progression of Liver Fibrosis by Regulating IL-13 Activity. Infect Immun (2006) 74:1471–9. doi: 10.1128/IAI.74.3.1471-1479.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Kawakami K, Taguchi J, Murata T, Puri RK. The Interleukin-13 Receptor Alpha2 Chain: An Essential Component for Binding and Internalization But Not for Interleukin-13-Induced Signal Transduction Through the STAT6 Pathway. Blood (2001) 97:2673–9. doi: 10.1182/blood.v97.9.2673 [DOI] [PubMed] [Google Scholar]
- 91. Verstockt B, Perrier C, De Hertogh G, Cremer J, Creyns B, Van Assche G, et al. Effects of Epithelial IL-13rα2 Expression in Inflammatory Bowel Disease. Front Immunol (2018) 9:2983. doi: 10.3389/fimmu.2018.02983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Karmele EP, Pasricha TS, Ramalingam TR, Thompson RW, Knilans KJ, Hegen M, et al. Anti-IL-13Ra2 Therapy Promotes Recovery in a Murine Model of Inflammatory Bowel Disease. Mucosal Immunol (2019) 12:1174–86. doi: 10.1038/s41385-019-0189-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Strober W, Kitani A, Fichtner-Feigl S, Fuss IJ. The Signaling Function of the IL-13Ralpha2 Receptor in the Development of Gastrointestinal Fibrosis and Cancer Surveillance. Curr Mol Med (2009) 9:740–50. doi: 10.2174/156652409788970652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Arijs I, Li K, Toedter G, Quintens R, Van Lommel L, Van Steen K, et al. Mucosal Gene Signatures to Predict Response to Infliximab in Patients With Ulcerative Colitis. Gut (2009) 58:1612–9. doi: 10.1136/gut.2009.178665 [DOI] [PubMed] [Google Scholar]
- 95. Arijs I, Quintens R, Van Lommel L, Van Steen K, De Hertogh G, Lemaire K, et al. Predictive Value of Epithelial Gene Expression Profiles for Response to Infliximab in Crohn’s Disease. Inflamm Bowel Dis (2010) 16:2090–8. doi: 10.1002/ibd.21301 [DOI] [PubMed] [Google Scholar]
- 96. Verstockt B, Verstockt S, Creyns B, Tops S, Van Assche G, Gils A, et al. Mucosal IL13RA2 Expression Predicts Nonresponse to Anti-TNF Therapy in Crohn’s Disease. Aliment Pharmacol Ther (2019) 49:572–81. doi: 10.1111/apt.15126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Reinisch W, Panés J, Khurana S, Toth G, Hua F, Comer GM, et al. Anrukinzumab, an Anti-Interleukin 13 Monoclonal Antibody, in Active UC: Efficacy and Safety From a Phase IIa Randomised Multicentre Study. Gut (2015) 64:894–900. doi: 10.1136/gutjnl-2014-308337 [DOI] [PubMed] [Google Scholar]
- 98. Griesenauer B, Paczesny S. The ST2/IL-33 Axis in Immune Cells During Inflammatory Diseases. Front Immunol (2017) 8:475. doi: 10.3389/fimmu.2017.00475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Jonckheere AC, Bullens DMA, Seys SF. Innate Lymphoid Cells in Asthma: Pathophysiological Insights From Murine Models to Human Asthma Phenotypes. Curr Opin Allergy Clin Immunol (2019) 19:53–60. doi: 10.1097/ACI.0000000000000497 [DOI] [PubMed] [Google Scholar]
- 100. Lampinen M, Fredricsson A, Vessby J, Martinez JF, Wanders A, Rorsman F, et al. Downregulated Eosinophil Activity in Ulcerative Colitis With Concomitant Primary Sclerosing Cholangitis. J Leukoc Biol (2018) 104:173–83. doi: 10.1002/JLB.3MA0517-175R [DOI] [PubMed] [Google Scholar]
- 101. Schmitz J, Owyang A, Oldham E, Song Y, Murphy E, McClanahan TK, et al. IL-33, an Interleukin-1-Like Cytokine That Signals via the IL-1 Receptor-Related Protein ST2 and Induces T Helper Type 2-Associated Cytokines. Immunity (2005) 23:479–90. doi: 10.1016/j.immuni.2005.09.015 [DOI] [PubMed] [Google Scholar]
- 102. De Salvo C, Wang XM, Pastorelli L, Mattioli B, Omenetti S, Buela KA, et al. IL-33 Drives Eosinophil Infiltration and Pathogenic Type 2 Helper T-Cell Immune Responses Leading to Chronic Experimental Ileitis. Am J Pathol (2016) 186:885–98. doi: 10.1016/j.ajpath.2015.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Meisel C, Bonhagen K, Löhning M, Coyle AJ, Gutierrez-Ramos J-C, Radbruch A, et al. Regulation and Function of T1/ST2 Expression on CD4+ T Cells: Induction of Type 2 Cytokine Production by T1/ST2 Cross-Linking. J Immunol (2001) 166:3143–50. doi: 10.4049/jimmunol.166.5.3143 [DOI] [PubMed] [Google Scholar]
- 104. Sedhom MAK, Pichery M, Murdoch JR, Foligné B, Ortega N, Normand S, et al. Neutralisation of the Interleukin-33/ST2 Pathway Ameliorates Experimental Colitis Through Enhancement of Mucosal Healing in Mice. Gut (2013) 62:1714–23. doi: 10.1136/gutjnl-2011-301785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Kita H. Eosinophils: Multifaceted Biologic Propterties and Roles in Health and Disease. Immunol Rev (2011) 242:161–77. doi: 10.1111/j.1600-065X.2011.01026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Egesten A, Calafat J, Knol EF, Janssen H, Walz TM. Subcellular Localization of Transforming Growth Factor-α in Human Eosinophil Granulocytes. Blood (1996) 87:3910–8. doi: 10.1182/blood.v87.9.3910.bloodjournal8793910 [DOI] [PubMed] [Google Scholar]
- 107. Lacy P. Eosinophil Cytokines in Allergy. In: Foti M, editor. Cytokine Effector Functions in Tissues. Edmonton: Elsevier. p. 173–218. [Google Scholar]
- 108. Ihara S, Hirata Y, Koike K. TGF-β in Inflammatory Bowel Disease: A Key Regulator of Immune Cells, Epithelium, and the Intestinal Microbiota. J Gastroenterol (2017) 52:777–87. doi: 10.1007/s00535-017-1350-1 [DOI] [PubMed] [Google Scholar]
- 109. Roberts AB, Heine UI, Flanders KC, Sporn MB. Transforming Growth Factor-Beta. Major Role in Regulation of Extracellular Matrix. Ann NY Acad Sci (1990) 580:225–32. doi: 10.1111/j.1749-6632.1990.tb17931 [DOI] [PubMed] [Google Scholar]
- 110. Diny NL, Rose NR, Čiháková D. Eosinophils in Autoimmune Diseases. Front Immunol (2017) 8:484. doi: 10.3389/fimmu.2017.00484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Chowdhury A, Fukuda R, Fukumoto S. Growth Factor mRNA Expression in Normal Colorectal Mucosa and in Uninvolved Mucosa From Ulcerative Colitis Patients. J Gastroenterol (1996) 31:353–60. doi: 10.1007/BF02355024 [DOI] [PubMed] [Google Scholar]
- 112. Babyatsky MW, Rossiter G, Podolsky DK. Expression of Transforming Growth Factors Alpha and Beta in Colonic Mucosa in Inflammatory Bowel Disease. Gastroenterology (1996) 110:975–84. doi: 10.1053/gast.1996.v110.pm8613031 [DOI] [PubMed] [Google Scholar]
- 113. Shull MM, Ormsby I, Kier AB, Pawlowski S, Diebold RJ, Yin M, et al. Targeted Disruption of the Mouse Transforming Growth Factor-Beta 1 Gene Results in Multifocal Inflammatory Disease. Nature (1992) 359:693–9. doi: 10.1038/359693a0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Seamons A, Treuting PM, Brabb T, Maggio-Price L. Characterization of Dextran Sodium Sulfate-Induced Inflammation and Colonic Tumorigenesis in Smad3(-/-) Mice With Dysregulated Tgfβ. PloS One (2013) 8(11):e79182. doi: 10.1371/journal.pone.0079182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Shomyseh S, Zenewicz L, Masahito K, Flavell R. Anti- and Pro-Inflammatory Roles of TGF-β, IL-10, and IL-22 In Immunity and Autoimmunity. Curr Opin Pharmacol (2010) 9:447–53. doi: 10.1016/j.coph.2009.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Mastrianni DM, Eddy RL, Rosenberg HF, Corrette SE, Shows TB, Tenen DG, et al. Localization of the Human Eosinophil Charcot-Leyden Crystal Protein (Lysophospholipase) Gene (CLC) to Chromosome 19 and the Human Ribonuclease 2 (Eosinophil-Derived Neurotoxin) and Ribonuclease 3 (Eosinophil Cationic Protein) Genes (RNS2 and RNS3) to Chromosome 14. Genomics (1991) 13:240–2. doi: 10.1016/0888-7543(92)90237-M [DOI] [PubMed] [Google Scholar]
- 117. Simon D, Simon H-U. Chapter 12 - Eosinophils. In: Barnes P, Drazen J, Rennard S, Thomson N, editors. Asthma and COPD. Oxford: Elsevier; (2008). p. 145–56. [Google Scholar]
- 118. Zuo L, Rothenberg ME. Chapter 46 Eosinophil-Associated Gastrointestinal Disorders (EGID). In: Rich R, Fleisher T, Shearer W, Schroeder H, Frew A, Weyand C, editors. Clinical Immunology: Principles and Practice. Edinburgh: Elsevier; (2008). p. 691–9. [Google Scholar]
- 119. Wędrychowicz A, Tomasik P, Pieczarkowski S, Grzenda-Adamek Z, Kowalska-Duplaga K, Fyderek K. Clinical Value of Serum Eosinophilic Cationic Protein Assessment in Children With Infflammatory Bowel Disease. Arch Med Sci (2014) 10:1142–6. doi: 10.5114/aoms.2013.34415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Abedin N, Seemann T, Kleinfeld S, Ruehrup J, Röseler S, Trautwein C, et al. Fecal Eosinophil Cationic Protein Is a Diagnostic and Predictive Biomarker in Young Adults With Inflammatory Bowel Disease. J Clin Med (2019) 8:2025. doi: 10.3390/jcm8122025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Wang J, Slungaard A. Role of Eosinophil Peroxidase in Host Defense and Disease Pathology. Arch Biochem Biophys (2006) 445:256–60. doi: 10.1016/j.abb.2005.10.008 [DOI] [PubMed] [Google Scholar]
- 122. Kovalszki A, Weller PF. Chapter 24: Eosinophils and Eosinophilia. In: Rich R, Fleisher T, Shearer W, Schroeder H, Frew A, Weyand C, editors. Clinical Immunology. London: Elsevier; (2013). p. 349–61. [Google Scholar]
- 123. Carlson M, Raab Y, Peterson C, Hällgren R, Venge P. Increased Intraluminal Release of Eosinophil Granule Proteins EPO, ECP, EPX, and Cytokines in Ulcerative Colitis and Proctitis in Segmental Perfusion. Am J Gastroenterol (1999) 94:1876–83. doi: 10.1111/j.1572-0241.1999.01223 [DOI] [PubMed] [Google Scholar]
- 124. Carvalho ATP, Elia CCS, de Souza HSP, Elias PRP, Pontes EL, Lukashok HP, et al. Immunohistochemical Study of Intestinal Eosinophils in Inflammatory Bowel Disease. J Clin Gastroenterol (2003) 36:120—125. doi: 10.1097/00004836-200302000-00006 [DOI] [PubMed] [Google Scholar]
- 125. Woodruff SA, Masterson JC, Fillon S, Robinson ZD, Furuta GT. Role of Eosinophils in Inflammatory Bowel and Gastrointestinal Diseases. J Pediatr Gastroenterol Nutr (2011) 52:650–61. doi: 10.1097/MPG.0b013e3182128512 [DOI] [PubMed] [Google Scholar]
- 126. Levy AM, Gleich GJ, Sandborn WJ, Tremaine WJ, Steiner BL, Phillips SF. Increased Eosinophil Granule Proteins in Gut Lavage Fluid From Patients With Inflammatory Bowel Disease. Mayo Clin Proc (1997) 72:117–23. doi: 10.4065/72.2.117 [DOI] [PubMed] [Google Scholar]
- 127. Wu W, Chen Y, Hazen SL. Eosinophil Peroxidase Nitrates Protein Tyrosyl Residues. Implications for Oxidative Damage by Nitrating Intermediates in Eosinophilic Inflammatory Disorders. J Biol Chem (1999) 274:25933–44. doi: 10.1074/jbc.274.36.25933 [DOI] [PubMed] [Google Scholar]
- 128. Kruidenier L, Verspaget HW. Oxidative Stress as a Pathogenic Factor in Inflammatory Bowel Disease -Radicals or Ridiculous? Aliment Pharmacol Ther (2002) 16:1997–2015. doi: 10.1046/j.1365-2036.2002.01378 [DOI] [PubMed] [Google Scholar]
- 129. Colon S, Luan H, Liu Y, Meyer C, Gewin L, Bhave G. Peroxidasin and Eosinophil Peroxidase, But Not Myeloperoxidase, Contribute to Renal Fibrosis in the Murine Unilateral Ureteral Obstruction Model. Am J Physiol Ren Physiol (2019) 316:360–71. doi: 10.1152/ajprenal.00291.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Forbes E, Murase T, Yang M, Matthaei KI, Lee JJ, Lee NA, et al. Immunopathogenesis of Experimental Ulcerative Colitis Is Mediated by Eosinophil Peroxidase. J Immunol (2004) 172:5664–75. doi: 10.4049/jimmunol.172.9.5664 [DOI] [PubMed] [Google Scholar]
- 131. Amcoff K, Cao Y, Zhulina Y, Lampinen M, Halfvarson J, Carlson M. Prognostic Significance of Faecal Eosinophil Granule Proteins in Inflammatory Bowel Disease. Scand J Gastroenterol (2019) 54:1237–44. doi: 10.1080/00365521.2019.1670251 [DOI] [PubMed] [Google Scholar]
- 132. Roca M, Varela AR, Donat E, Cano F, Hervas D, Armisen A, et al. Fecal Calprotectin and Eosinophil-Derived Neurotoxin in Healthy Children Between 0 and 12 Years. J Pediatr Gastroenterol Nutr (2017) 65:394–8. doi: 10.1097/MPG.0000000000001542 [DOI] [PubMed] [Google Scholar]
- 133. Plager DA, Loegering DA, Checkel JL, Tang J, Kephart GM, Caffes PL, et al. Major Basic Protein Homolog (MBP2): A Specific Human Eosinophil Marker. J Immunol (2006) 177:7340–5. doi: 10.4049/jimmunol.177.10.7340 [DOI] [PubMed] [Google Scholar]
- 134. Choe MM, Sporn PHS, Swartz MA. An In Vitro Airway Wall Model of Remodeling. Am J Physiol - Lung Cell Mol Physiol (2003) 285:427–33. doi: 10.1152/ajplung.00005.2003 [DOI] [PubMed] [Google Scholar]
- 135. Furuta GT, Nieuwenhuis EES, Karhausen J, Gleich G, Blumberg RS, Lee JJ, et al. Eosinophils Alter Colonic Epithelial Barrier Function: Role for Major Basic Protein. Am J Physiol - Gastrointest Liver Physiol (2005) 289:890–7. doi: 10.1152/ajpgi.00015.2005 [DOI] [PubMed] [Google Scholar]
- 136. Kato M, Kephart GM, Talley NJ, Wagner JM, Sarr MG, Bonno M, et al. Eosinophil Infiltration and Degranulation in Normal Human Tissue. Anat Rec (1998) 252:418–25. doi: [DOI] [PubMed] [Google Scholar]
- 137. Click B, Anderson AM, Koutroubakis IE, Rivers CR, Babichenko D, Machicado JD, et al. Peripheral Eosinophilia in Patients With Inflammatory Bowel Disease Defines an Aggressive Disease Phenotype. Am J Gastroenterol (2017) 112:1849–58. doi: 10.1038/ajg.2017.402 [DOI] [PubMed] [Google Scholar]
- 138. Barrie A, Mourabet M, Weyant K, Clarke K, Gajendran M, Rivers C, et al. Recurrent Blood Eosinophilia in Ulcerative Colitis Is Associated With Severe Disease and Primary Sclerosing Cholangitis. Dig Dis Sci (2013) 58:222–8. doi: 10.1007/s10620-012-2329-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Jung Y, Rothenberg ME. Roles and Regulation of Gastrointestinal Eosinophils in Immunity and Disease. J Immunol (2014) 193:999–1005. doi: 10.4049/jimmunol.1400413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Neuberger J. Eosinophils and Primary Biliary Cirrhosis - Stoking the Fire? Hepatology (1999) 30:335–7. doi: 10.1002/hep.510300150 [DOI] [PubMed] [Google Scholar]
- 141. Doucet C, Brouty-Boyé D, Pottin-Clemenceau C, Jasmin C, Canonica GW, Azzarone B. IL-4 and IL-13 Specifically Increase Adhesion Molecule and Inflammatory Cytokine Expression in Human Lung Fibroblasts. Int Immunol (1998) 10:1421–33. doi: 10.1093/intimm/10.10.1421 [DOI] [PubMed] [Google Scholar]
- 142. Huaux F, Liu T, McGarry B, Ullenbruch M, Phan SH. Dual Roles of IL-4 in Lung Injury and Fibrosis. J Immunol (2003) 170:2083–92. doi: 10.4049/jimmunol.170.4.2083 [DOI] [PubMed] [Google Scholar]
- 143. Roselló-Lletí E, Rivera M, Bertomeu V, Cortés R, Jordán A, González-Molina A. Interleukin-4 and Cardiac Fibrosis in Patients With Heart Failure. Rev Española Cardiol (2007) 60:777–80. doi: 10.1016/s1885-5857(08)60014-6 [DOI] [PubMed] [Google Scholar]
- 144. Ong C, Wong C, Roberts CR, Teh HS, Jirik FR. Anti-IL-4 Treatment Prevents Dermal Collagen Deposition in the Tight-Skin Mouse Model of Scleroderma. Eur J Immunol (1998) 28:2619–29. doi: [DOI] [PubMed] [Google Scholar]
- 145. Cheever A, Williams M, Wynn T, Finkelman F, Seder R, Cox T, et al. Anti-IL-4 Treatment of Schistosoma Mansoni-Infected Mice Inhibits Development of T Cells and non-B, Non-T Cells Expressing Th2 Cytokines While Decreasing Egg-Induced Hepatic Fibrosis. J Immunol (1994) 53:1689–99. doi: 10.1017/CBO9781107415324.004 [DOI] [PubMed] [Google Scholar]
- 146. Wynn T. Cellular and Molecular Mechanisms of Fibrosis. J Pathol (2008) 214:199–210. doi: 10.1002/path [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Wynn TA, Ramalingam TR. Mechanisms of Fibrosis: Therapeutic Translation for Fibrotic Disease. Nat Med (2012) 18:1028–40. doi: 10.1038/nm.2807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Wick G, Grundtman C, Mayerl C, Wimpissinger TF, Feichtinger J, Zelger B, et al. The Immunology of Fibrosis. Annu Rev Immunol (2013) 31:107–35. doi: 10.1146/annurev-immunol-032712-095937 [DOI] [PubMed] [Google Scholar]
- 149. Speca S, Giusti I, Rieder F, Latella G. Cellular and Molecular Mechanisms of Intestinal Fibrosis. World J Gastroenterol (2012) 18:3635–61. doi: 10.3748/wjg.v18.i28.3635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Takemura N, Kurashima Y, Mori Y, Okada K, Ogino T, Osawa H, et al. Eosinophil Depletion Suppresses Radiation-Induced Small Intestinal Fibrosis. Sci Transl Med (2018) 10:333. doi: 10.1126/scitranslmed.aan0333 [DOI] [PubMed] [Google Scholar]
- 151. Kaviratne M, Hesse M, Leusink M, Cheever AW, Davies SJ, McKerrow JH, et al. IL-13 Activates a Mechanism of Tissue Fibrosis That Is Completely TGF-Beta Independent. J Immunol (2004) 173:4020–9. doi: 10.4049/jimmunol.173.6.4020 [DOI] [PubMed] [Google Scholar]
- 152. Lee CG, Homer RJ, Zhu Z, Lanone S, Wang X, Koteliansky V, et al. Interleukin-13 Induces Tissue Fibrosis by Selectively Stimulating and Activating Transforming Growth Factor β1. J Exp Med (2001) 194:809–21. doi: 10.1084/jem.194.6.809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Alegre . Select Effects of IL-13 in Driving Tissue Repair and Fibrosis. Am J Transplant (2016) 16:2771. doi: 10.1111/ajt.14027 [DOI] [Google Scholar]
- 154. Hur GY, Broide DH. Genes and Pathways Regulating Decline in Lung Function and Airway Remodeling in Asthma. Allergy Asthma Immunol Res (2019) 11:604–21. doi: 10.4168/aair.2019.11.5.604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Passalacqua G, Mincarini M, Colombo D, Troisi G, Ferrari M, Bagnasco D, et al. IL-13 and Idiopathic Pulmonary Fibrosis: Possible Links and New Therapeutic Strategies. Pulm Pharmacol Ther (2017) 45:95–100. doi: 10.1016/j.pupt.2017.05.007 [DOI] [PubMed] [Google Scholar]
- 156. Burrello C, Garavaglia F, Cribiù FM, Ercoli G, Lopez G, Troisi J, et al. Therapeutic Faecal Microbiota Transplantation Controls Intestinal Inflammation Through IL10 Secretion by Immune Cells. Nat Commun (2018) 9(1):5184. doi: 10.1038/s41467-018-07359-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Fichtner-Feigl S, Kesselring R, Martin M, Obermeier F, Ruemmele P, Kitani A, et al. IL-13 Orchestrates Resolution of Chronic Intestinal Inflammation via Phosphorylation of Glycogen Synthase Kinase-3β. J Immunol (2014) 192:3969–80. doi: 10.4049/jimmunol.1301072 [DOI] [PubMed] [Google Scholar]
- 158. Masterson JC, Capocelli KE, Hosford L, Biette K, McNamee EN, De Zoeten EF, et al. Eosinophils and IL-33 Perpetuate Chronic Inflammation and Fibrosis in a Pediatric Population With Stricturing Crohn’s Ileitis. Inflamm Bowel Dis (2015) 21:2429–40. doi: 10.1097/MIB.0000000000000512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Isaka Y. Targeting TGF-β Signaling in Kidney Fibrosis. Int J Mol Sci (2018) 19:1–13. doi: 10.3390/ijms19092532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Ojiaku CA, Yoo EJ, Panettieri RA. Transforming Growth Factor β1 Function in Airway Remodeling and Hyperresponsiveness: The Missing Link? Am J Respir Cell Mol Biol (2017) 56:432–42. doi: 10.1165/rcmb.2016-0307TR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Dewidar B, Soukupova J, Fabregat I, Dooley S. TGF-β in Hepatic Stellate Cell Activation and Liver Fibrogenesis: Updated. Curr Pathobiol Rep (2019) 3:291–305. doi: 10.1007/s40139-015-0089-8 [DOI] [Google Scholar]
- 162. McKaig BC, Hughes K, Tighe PJ, Mahida YR. Differential Expression of TGF-Beta Isoforms by Normal and Inflammatory Bowel Disease Intestinal Myofibroblasts. Am J Physiol Cell Physiol (2002) 282:172–82. doi: 10.1152/ajpcell.00048.2001 [DOI] [PubMed] [Google Scholar]
- 163. di Mola FF, Friess H, Scheuren A, Di Sebastiano P, Graber H, Egger B, et al. Transforming Growth Factor-Betas and Their Signaling Receptors Are Coexpressed in Crohn’s Disease. Ann Surg (1999) 229:67–75. doi: 10.1097/00000658-199901000-00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Bystrom J, Amin K, Bishop-Bailey D. Analysing the Eosinophil Cationic Protein - A Clue to the Function of the Eosinophil Granulocyte. Respir Res (2011) 12:10. doi: 10.1186/1465-9921-12-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Zagai U, Dadfar E, Lundahl J, Venge P, Sköld CM. Eosinophil Cationic Protein Stimulates TGF-β1 Release by Human Lung Fibroblasts in vitro . Inflammation (2007) 30:153–60. doi: 10.1007/s10753-007-9032-4 [DOI] [PubMed] [Google Scholar]
- 166. Pégorier S, Wagner LA, Gleich GJ, Pretolani M. Eosinophil-Derived Cationic Proteins Activate the Synthesis of Remodeling Factors by Airway Epithelial Cells. J Immunol (2006) 177:4861–9. doi: 10.4049/jimmunol.177.7.4861 [DOI] [PubMed] [Google Scholar]
- 167. Porto BN, Stein RT. Neutrophil Extracellular Traps in Pulmonary Diseases: Too Much of a Good Thing? Front Immunol (2016) 7:311. doi: 10.3389/fimmu.2016.00311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Chrysanthopoulou A, Mitroulis I, Apostolidou E, Arelaki S, Mikroulis D, Konstantinidis T, et al. Neutrophil Extracellular Traps Promote Differentiation and Function of Fibroblasts. J Pathol (2014) 233:294–307. doi: 10.1002/path.4359 [DOI] [PubMed] [Google Scholar]
- 169. Choi Y, Le Pham D, Lee DH, Lee SH, Kim SH, Park HS. Biological Function of Eosinophil Extracellular Traps in Patients With Severe Eosinophilic Asthma. Exp Mol Med (2018) 50(8):1–8. doi: 10.1038/s12276-018-0136-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Sutherland DB, Fagarasan S. Gut Reactions: Eosinophils Add Another String to Their Bow. Immunity (2014) 40:455–7. doi: 10.1016/j.immuni.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 171. McManus DP, Dunne DW, Sacko M, Utzinger J, Vennervald BJ, Zhou XN. Schistosomiasis. Nat Rev Dis Prim (2018) 4:1–19. doi: 10.1038/s41572-018-0013-8 [DOI] [PubMed] [Google Scholar]
- 172. Gurtner A, Gonzalez-Perez I, Arnold IC. Intestinal Eosinophils, Homeostasis and Response to Bacterial Intrusion. Semin Immunopathol (2021) 43:295–306. doi: 10.1007/s00281-021-00856-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Altman LC, Hill JS, Hairfield WM, Mullarkey MF. Effects of Corticosteroids on Eosinophil Chemotaxis and Adherence. J Clin Invest (1981) 67:28–36. doi: 10.1172/JCI110024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Loymans RJB, Gemperli A, Cohen J, Rubinstein SM, Sterk PJ, Reddel HK, et al. Comparative Effectiveness of Long Term Drug Treatment Strategies to Prevent Asthma Exacerbations: Network Meta-Analysis. BMJ (2014) 348:1–16. doi: 10.1136/bmj.g3009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Oikarinen AI, Vuorio EI, Zaragoza EJ, Palotie A, Mon-Li C, Uitto J. Modulation of Collagen Metabolism by Glucocorticoids. Biochem Pharmacol (1988) 37:1451–62. doi: 10.1016/0006-2952(88)90006-8 [DOI] [PubMed] [Google Scholar]
- 176. Vaglio A, Palmisano A, Corradi D, Salvarani C, Buzio C. Retroperitoneal Fibrosis: Evolving Concepts. Rheum Dis Clin North Am (2007) 33:803–17. doi: 10.1016/j.rdc.2007.07.013 [DOI] [PubMed] [Google Scholar]
- 177. Vaglio A, Maritati F. Idiopathic Retroperitoneal Fibrosis. J Am Soc Nephrol (2016) 27:1880–9. doi: 10.1681/ASN.2015101110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Badea I, Taylor M, Rosenberg A, Foldvari M. Pathogenesis and Therapeutic Approaches for Improved Topical Treatment in Localized Scleroderma and Systemic Sclerosis. Rheumatology (2009) 48:213–21. doi: 10.1093/rheumatology/ken405 [DOI] [PubMed] [Google Scholar]
- 179. Peikert T, Daniels CE, Beebe TJ, Meyer KC, Ryu JH. Assessment of Current Practice in the Diagnosis and Therapy of Idiopathic Pulmonary Fibrosis. Respir Med (2008) 102:1342–8. doi: 10.1016/j.rmed.2008.03.018 [DOI] [PubMed] [Google Scholar]
- 180. Rogliani P, Mura M, Assunta Porretta M, Saltini C. New Perspectives in the Treatment of Idiopathic Pulmonary Fibrosis. Ther Adv Respir Dis (2008) 2:75–93. doi: 10.1177/1753465808089363 [DOI] [PubMed] [Google Scholar]
- 181. Bochner BS. Novel Therapies for Eosinophilic Disorders. Immunol Allergy Clin North Am (2015) 35(3):577–98. doi: 10.1016/j.iac.2015.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Di Sabatino A, Ciccocioppo R, Benazzato L, Sturniolo GC, Corazza GR. Infliximab Downregulates Basic Fibroblast Growth Factor and Vascular Endothelial Growth Factor in Crohn’s Disease Patients. Aliment Pharmacol Ther (2004) 19:1019–24. doi: 10.1111/j.1365-2036.2004.01927 [DOI] [PubMed] [Google Scholar]
- 183. Di Sabatino A, Pender SLF, Jackson CL, Prothero JD, Gordon JN, Picariello L, et al. Functional Modulation of Crohn’s Disease Myofibroblasts by Anti-Tumor Necrosis Factor Antibodies. Gastroenterology (2007) 133:137–49. doi: 10.1053/j.gastro.2007.04.069 [DOI] [PubMed] [Google Scholar]
- 184. Bouhnik Y, Carbonnel F, Laharie D, Stefanescu C, Hébuterne X, Abitbol V, et al. Efficacy of Adalimumab in Patients With Crohn’s Disease and Symptomatic Small Bowel Stricture: A Multicentre, Prospective, Observational Cohort (CREOLE) Study. Gut (2018) 67:53–60. doi: 10.1136/gutjnl-2016-312581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Damsky WE, Vesely MD, Lee AI, Choi J, Meyer AC, Chen M, et al. Drug-Induced Hypersensitivity Syndrome With Myocardial Involvement Treated With Tofacitinib. JAAD Case Rep (2019) 5:1018–26. doi: 10.1016/j.jdcr.2019.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. King B, Lee AI, Choi J. Treatment of Hypereosinophilic Syndrome With Cutaneous Involvement With the JAK Inhibitors Tofacitinib and Ruxolitinib. Physiol Behav (2017) 176:139–48. doi: 10.1016/j.physbeh.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Mendoza Alvarez LB, Liu X, Glover S. Treatment-Resistant Eosinophilic Oesophagitis Successfully Managed With Tofacitinib. BMJ Case Rep (2019) 12:10–2. doi: 10.1136/bcr-2019-232558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Matsumoto A, Sasaki N, Nagashima H, Akiyama M, Niisato M, Yamauchi K, et al. Tofacitinib Suppressed Remodeling of Pulmonary Eosinophilic Vasculitis in a Murine Model. J Transl Sci (2019) 6:1–7. doi: 10.15761/JTS.1000355 [DOI] [Google Scholar]
- 189. Torres J, Bonovas S, Doherty G, Kucharzik T, Gisbert JP, Raine T, et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Medical Treatment. J Crohn’s Colitis (2020) 14:4–22. doi: 10.1093/ecco-jcc/jjz180 [DOI] [PubMed] [Google Scholar]
- 190. Harbord M, Eliakim R, Bettenworth D, Karmiris K, Katsanos K, Kopylov U, et al. Third European Evidence-Based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 2: Current Management. J Crohn’s Colitis (2017) 11:769–84. doi: 10.1093/ecco-jcc/jjx009 [DOI] [PubMed] [Google Scholar]
- 191. Kim HJ, Jung Y. The Emerging Role of Eosinophils as Multifunctional Leukocytes in Health and Disease. Immune Netw (2020) 20:1–14. doi: 10.4110/in.2020.20.e24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Kim EM, Randall C, Betancourt R, Keene S, Lilly A, Fowler M, et al. Mucosal Eosinophilia Is an Independent Predictor of Vedolizumab Efficacy in Inflammatory Bowel Diseases. Inflamm Bowel Dis (2020) 26:1232–8. doi: 10.1093/ibd/izz251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Lee BJ, Moon HG, Shin TS, Jeon SG, Lee EY, Gho YS, et al. Protective Effects of Basic Fibroblast Growth Factor in the Development of Emphysema Induced by Interferon-γ. Exp Mol Med (2011) 43:169–78. doi: 10.3858/emm.2011.43.4.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Larsson-Callerfelt A-K, Andersson Sjöland A, Hallgren O, Bagher M, Thiman L, Löfdahl C-G, et al. VEGF Induces ECM Synthesis and Fibroblast Activity in Human Lung Fibroblasts. Eur Respir J (2017) 50. doi: 10.1183/1393003 [DOI] [Google Scholar]
- 195. Panés J, Sandborn WJ, Schreiber S, Sands BE, Vermeire S, D’Haens G, et al. Tofacitinib for Induction and Maintenance Therapy of Crohn’s Disease: Results of Two Phase IIb Randomised Placebo-Controlled Trials. Gut (2017) 66:1049–59. doi: 10.1136/gutjnl-2016-312735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Vermeire S, Schreiber S, Petryka R, Kuehbacher T, Hebuterne X, Roblin X, et al. Clinical Remission in Patients With Moderate-to-Severe Crohn’s Disease Treated With Filgotinib (the FITZROY Study): Results From a Phase 2, Double-Blind, Randomised, Placebo-Controlled Trial. Lancet (2017) 389:266–75. doi: 10.1016/S0140-6736(16)32537-5 [DOI] [PubMed] [Google Scholar]
- 197. Roblin X, Serone A, Yoon OK, Zhuo L, Grant E, Woo J, et al. Effects of the Janus Kinase 1 (JAK1)-Selective Inhibitor Filgotinib on Circulating Cytokines and Whole-Blood Genes/Pathways of Patients With Moderately to Severely Active Crohn’s Disease (CD). J Crohn’s Colitis (2018) 14:S457–8. doi: 10.1093/ecco-jcc/jjz203.663 [DOI] [Google Scholar]
- 198. Ben S, Li X, Xu F, Xu W, Li W, Wu Z, et al. Treatment With Anti-CC Chemokine Receptor 3 Monoclonal Antibody or Dexamethasone Inhibits the Migration and Differentiation of Bone Marrow CD34+ Progenitor Cells in an Allergic Mouse Model. Allergy Eur J Allergy Clin Immunol (2008) 63:1164–76. doi: 10.1111/j.1398-9995.2008.01747 [DOI] [PubMed] [Google Scholar]
- 199. Masterson JC, McNamee EN, Jedlicka P, Fillon S, Ruybal J, Hosford L, et al. CCR3 Blockade Attenuates Eosinophilic Ileitis and Associated Remodeling. Am J Pathol (2011) 179:2302–14. doi: 10.1016/j.ajpath.2011.07.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Adar T, Shteingart S, Ben-Ya’acov A, Shitrit AB-G, Livovsky DM, Shmorak S, et al. The Importance of Intestinal Eotaxin-1 in Inflammatory Bowel Disease: New Insights and Possible Therapeutic Implications. Dig Dis Sci (2016) 61:1915–24. doi: 10.1007/s10620-016-4047 [DOI] [PubMed] [Google Scholar]
- 201. Vieira AT, Fagundes CT, Alessandri AL, Castor MGM, Guabiraba R, Borges VO, et al. Treatment With a Novel Chemokine-Binding Protein or Eosinophil Lineage-Ablation Protects Mice From Experimental Colitis. Am J Pathol (2009) 175:2382–91. doi: 10.2353/ajpath.2009.090093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Gonzalo JA, Lloyd CM, Kremer L, Finger E, Martinez AC, Siegelman MH, et al. Eosinophil Recruitment to the Lung in a Murine Model of Allergic Inflammation: The Role of T Cells, Chemokines, and Adhesion Receptors. J Clin Invest (1996) 98:2332–45. doi: 10.1172/JCI119045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Ding C, Li J, Zhang X. Bertilimumab Cambridge Antibody Technology Group. Curr Opin Investig Drugs (2004) 5:1213—1218. [PubMed] [Google Scholar]
- 204. Main S, Handy R, Wilton J, Smith S, Williams L, Fou L, et al. A Potent Human Anti-Eotaxin1 Antibody, CAT-213: Isolation by Phage Display and In Vitro and In Vivo Efficacy. J Pharmacol Exp Ther (2006) 319:1395–404. doi: 10.1124/jpet.106.110734 [DOI] [PubMed] [Google Scholar]
- 205. Adar T, Shteingart S, Livovsky DM, Shitrit ABG, Mahamid BK M. And EG. Inhibition of Eotaxin-1 (CCL-11) Ameliorates DSS-Induced Colitis - A Novel Potential Therapeutic Approach for Inflammatory Bowel Disease. United Eur Gastroenterol J (2013) 1:A135–587. doi: 10.1177/2050640613502900 [DOI] [Google Scholar]
- 206. Mukherjee M, Sehmi R, Nair P. Anti-IL5 Therapy for Asthma and Beyond. World Allergy Organ J (2014) 7:32. doi: 10.1186/1939-4551-7-32 [DOI] [PMC free article] [PubMed] [Google Scholar]