Abstract
Objective
Months after the declaration of the coronavirus disease of 2019 (COVID-19) national emergency, visits among children remained suppressed for unclear reasons, which we sought to understand by examining child visit rates.
Methods
Using de-identified claims data for children <18 years old from OptumLabs® Data Warehouse, a large commercial claims database, we compared monthly primary care visit and vaccination rates from January–October 2020 to January–October 2018 and 2019. Visit rates were analyzed by visit reason and by the month after (eg, month +1) the COVID-19 public health emergency declaration using a series of child-level Poisson regression models.
Results
There were 3.4, 3.4, and 3.1 million children in 2018, 2019, and 2020 cohorts, respectively. Compared to the same months in prior years, primary care visits in 2020 were 60% lower in month +1 (incidence rate ratio [IRR] 0.40, 99% confidence interval [CI] 0.40–0.40) and 17% lower in month +7 (IRR 0.83, 99% CI 0.83–0.83). Preventive visit rates were 53% lower in month +1 (IRR 0.47, 99% CI 0.47–0.47), but 8% higher than prior years in month +7 (IRR 1.08, 99% CI 1.08–1.08). Monthly rates of vaccine administration followed a similar pattern. Problem-focused visits remained 31% lower in month +7 (IRR 0.69, 99% CI 0.68–0.69), with notably fewer infection-related visits (acute respiratory tract infections IRR 0.37, 99% CI 0.36–0.37; gastroenteritis IRR 0.20, 99% CI 0.20–0.20).
Conclusion
Seven months after the COVID-19 emergency declaration, receipt of pediatric care remained suppressed due to fewer problem-focused visits, with notably fewer infection-related visits. By October 2020, rates of preventive visits and vaccination exceeded rates in prior years.
Keywords: ambulatory pediatrics, health services research
What's New.
Among commercially insured children, the persistent reduction in primary care visits as of October 2020 was due to fewer problem-focused visits. Though rates of preventive visits and vaccination rebounded as the pandemic progressed, as of October 2020 a cumulative deficit remained.
Alt-text: Unlabelled box
Introduction
The coronavirus disease of 2019 (COVID-19) pandemic has had a staggering impact on outpatient medical practice volume. In the United States, the volume of visits across all outpatient settings declined by almost 60% in early April 2020.1, 2, 3 Since that time a substantial rebound in visit volume has been reported, with visits to many specialties close to prepandemic volume by October 2020.4 Pediatric care is a notable exception.5 Among children younger than 5 years old, multiple reports found visits remained below prepandemic volume while visits for other age groups recovered.4, 5, 6, 7 Factors contributing to lower visit volume specifically for children during this time are unclear. Possibly during the COVID-19 pandemic, parents and physicians became more hesitant to bring children to clinic visits due to of concerns about safety, which could impact volume of both preventive and problem-focused visits.8 , 9 Another possibility is that decreased circulation of respiratory viruses (eg, influenza, respiratory syncytial virus)10, 11, 12 due to the extensive public health measures aimed at reducing COVID-19 transmission resulted in fewer children experiencing illnesses requiring primary care visits.10, 11, 12 Alternatively, fewer children may have presented for preventive visits in the absence of childcare, school, and sports-associated need for visit documentation.
A continued decrease in pediatric visits has important implications for the financial viability of pediatric practices, the opportunity for adequate education of pediatric trainees, and the clinical needs of children including preventive, chronic illness, and acute care. For example, among pediatric Medicaid beneficiaries there were 3 million fewer total vaccinations ordered by mid-April 2020 compared to prior years with the largest deficits among children greater than 2 years old.13 To further understand the impact of the pandemic on children's receipt of care, we examined trends in pediatric primary care preventive visits, problem-focused visits, and overall vaccination rates among a national sample of commercially insured children during the first 10 months of 2020 compared to the first 10 months of 2018 and 2019.
Methods
Study Sample
Our study utilized de-identified claims data from 2018 to 2020 in the OptumLabs® Data Warehouse, which includes medical claims and enrollment records for commercial enrollees covered under a range of health plan products which currently cover an estimated 13% of commercially insured US individuals nationally. We created 3 cohorts of children for these three years (2018, 2019, and 2020), with each cohort including all enrolled children <18 years old who had 10 months of continuous enrollment (from January through October of the cohort year) and children ≤1 year old with continuous enrollment since birth (from birth through October of the cohort year).
Due to potential lag in claims data, we tested the completeness of claims by calculating weekly rates of childbirths per 1000 female enrollees between 15 and 44 years old and confirmed that the weekly rate of childbirth in the data remained stable from January 1 through October 6, 2020.14 , 15 To evaluate whether the substantial rise in unemployment during the pandemic was associated with increased insurance drop-out rates during 2020 compared to prior years, we examined insurance drop-out rates across the 3 years and found the drop-out rate was similar for each year.
Our 2020 data spanned January 1 through October 6, 2020. We defined the three 4-week intervals from January 1 through March 24, 2020 as the “pre-pandemic” period (3 months) and the seven 4-week intervals from March 25 through October 6, 2020 as the “pandemic” period (7 months). Thus month +1 of the pandemic period (March 25–April 21, 2020) directly followed the proclamation of national public health emergency on March 13, 2020 as well as the Centers for Medicare and Medicaid Services statements on telehealth and non-essential care on March 17 and 18, respectively.16, 17, 18
Enrollee Characteristics
Enrollee characteristics included child age (categorized into 4 groups: <1, 1–4, 5–11, 12–<18 years old), sex, rural-urban commuting area 4-category US Census designation, and enrollee county median household income (categorized into quartiles from the 2010 US Census).19 To further describe the sample, we determined child medical complexity using the Pediatric Medical Complexity Algorithm, which categorizes patients into 3 levels of medical complexity based on administrative claims data: complex chronic disease (eg, cystic fibrosis or technology dependence), noncomplex chronic disease (eg, asthma), and no chronic disease.20 To do so, we used the 12-month period prior to the cohort year (eg, 2018 data were used for the 2019 cohort). Because not all children were enrolled consistently during the prior 12 months, this approach may underestimate the percentage of children identified as having a chronic disease. However, any underestimate should occur consistently across each year, as the percentage of children enrolled for the prior 12 months was similar for each year. Of note, rates of chronic disease were similar to prior studies.21
Visit Setting and Visit Reason Categorization
Our main analyses focused on primary care physician (PCP) visits. To identify these visits, we first identified emergency department visits and urgent care visits using Current Procedural Terminology (CPT) codes, physician specialty codes, place of service codes, and CPT modifiers as described previously.21 , 22 Among the remaining visits, we identified PCP visits based on the physician specialty code for the visit (family medicine, pediatrics).
We then categorized the PCP visits using CPT codes: preventive visits (99381–99384, 99391–99394) and problem-focused visits (99201–99215). Telemedicine visits were identified via CPT codes (99441–99449), CPT modifiers (GT, GQ and 95), or place of service code (02); the remaining visits were categorized as in-person. Audio-only telemedicine CPT codes made up 4% (n = 27,604) of total telemedicine visits during the study period; therefore, we analyzed audio-only and audio-video telemedicine together.
Among the remaining non-PCP visits, visits were categorized as visits to physician specialists (eg, cardiologist, otorhinolaryngologist) or nonphysician clinicians (eg, social worker, psychologist, physical therapist).
Diagnoses and Vaccine Identification
To describe trends within primary care problem-focused visits, we selected 8 common conditions which included both acute and chronic conditions and varied in their likelihood of disease burden being impacted by the pandemic and pandemic-related public health measures. Specifically, we selected 2 acute conditions with infectious etiology which we hypothesized would occur less frequently due to public health interventions in place to reduce coronavirus transmission (acute respiratory tract infection (ARTI); gastroenteritis)10 , 11 and 2 acute conditions which we hypothesized would have stable and nondeferrable need for care (hyperbilirubinemia; urinary tract infections [UTIs]). Among chronic conditions, we selected one where we hypothesized that public health interventions may have reduced exacerbations (asthma),23 one where school closures may have altered management plans (attention deficit-hyperactivity disorder), and one where it was less likely that pandemic-related factors would impact disease control (eczema). Finally, we selected one group of diagnoses where we anticipated an increase in acute and chronic needs (anxiety and depression) due to pandemic-related societal changes.24 , 25 We identified visits based on the primary International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code on the visit (listed in Appendix Table 1).26, 27, 28, 29, 30, 31, 32, 33 Consistent with prior work, the ARTI condition group is composed of both bacterial and viral diagnoses including sinusitis, acute otitis media, streptococcal pharyngitis, viral upper respiratory infection, bronchiolitis, and others.26 Gastroenteritis also included both viral and bacterial etiologies.27 Visits for these 8 conditions along with preventive visits accounted for 63% of all pediatric primary care visits in these data.
Vaccinations were identified by CPT administration codes. We examined total volume of all childhood vaccines administered per month, with the exception of influenza (due to seasonal administration), consistent with recent CDC reports of overall volume.13
Statistical Analysis
We describe enrollee characteristics and visit trends for the 2018, 2019, and 2020 cohorts using descriptive statistics.
To estimate the relative change in visit rates during early and later months of the pandemic, we compare 2020 to 2018 and 2019 visits using a series of child-level Poisson regression models. We specifically examined the first month during the defined pandemic period (March 25–April 21; hereafter referred to month +1) and seventh month during the defined pandemic period (September 9–October 6; hereafter referred to as month +7) to examine the early and later pandemic period compared to the same months in prior years. For each PCP visit category, the dependent variable was visit counts with the independent variable being an indicator variable for 2020 versus prior years (2018 and 2019), with standard errors adjusted for child-level clustering. Separate models were fitted to data for all PCP visits, preventive PCP visits (total and stratified by child age), problem-focused PCP visits (total and for the 8 selected conditions), telemedicine PCP visits, and overall noninfluenza vaccine administration.
Finally, to provide context about changes in primary care visits, we determined volume of visits outside of primary care for children to the emergency department, urgent care, physician specialists, and nonphysician clinicians (eg, social work, physical therapist), in 2020 compared to prior years.
All analyses were conducted in SAS software, Version 9.4 (SAS Institute, Inc., Cary, NC) with significance assessed using an alpha level of .05.
Ethical Considerations
This analysis was determined to be exempt by the Harvard Longwood Campus Institutional Review Board.
Results
There were 3.4, 3.4, and 3.1 million children in the 2018, 2019, and 2020 cohorts, respectively. Patient characteristics were similar across all 3 cohorts, with 51% male enrollees, similar age distribution and medical complexity, and a majority (90%) from an urban location (Table 1 ).
Table 1.
Characteristics of Children in the Study Cohorts (2018, 2019, and 2020)
| Characteristic, No. (%) | 2018 | 2019 | 2020 | |
|---|---|---|---|---|
| Total cohort, No. | 3,447,599 | 3,362,729 | 3,114,291 | |
| Age category, y | Under 1 | 143,292 (4) | 137,268 (4) | 120,151 (4) |
| 1–5 | 673,391 (20) | 653,377 (19) | 598,734 (19) | |
| 5–12 | 1,345,079 (39) | 1,309,673 (39) | 1,214,142 (39) | |
| 12–<18 | 1,285,837 (37) | 1,262,411 (38) | 1,181,264 (38) | |
| Sex | Male | 1,758,110 (51) | 1,716,339 (51) | 1,588,937 (51) |
| Female | 1,689,278 (49) | 1,646,095 (49) | 1,523,934 (49) | |
| Census division | New England | 129,107 (4) | 123,701 (4) | 107,632 (4) |
| Middle Atlantic | 308,272 (9) | 298,555 (9) | 274,541 (9) | |
| East North Central | 565,832 (17) | 537,376 (17) | 493,169 (16) | |
| West North Central | 380,930 (11) | 395,662 (12) | 385,669 (13) | |
| South Atlantic | 661,503 (20) | 647,464 (20) | 597,592 (20) | |
| East South Central | 136,947 (4) | 129,776 (4) | 122,339 (4) | |
| West South Central | 542,275 (16) | 518,826 (16) | 475,745 (16) | |
| Mountain | 329,173 (10) | 308,055 (10) | 285,742 (10) | |
| Pacific | 312,832 (9) | 291,976 (9) | 259,744 (9) | |
| Urban/rural designation | Urban | 3,033,003 (90) | 2,923,818 (90) | 2,696,593 (90) |
| Large rural | 185,804 (6) | 182,382 (6) | 169,935 (6) | |
| Small rural | 95,039 (3) | 92,401 (3) | 85,944 (3) | |
| Rural isolated | 53,416 (2) | 52,996 (2) | 49,212 (2) | |
| County Median Household Income, Quartile* | Quartile 1 (<$41,042) | 481,365 (14) | 466,904(14) | 429,004 (14) |
| Quartile 2 ($41,042–52,197) | 817,611 (24) | 791,937 (24) | 735,088 (25) | |
| Quartile 3 ($52,198–69,240) | 877,161 (26) | 835,579 (26) | 778,536 (26) | |
| Quartile 4 (>$69,240) | 1,187,161 (35) | 1,153,410 (36) | 1,056,200 (35) | |
| Pediatric Medical Complexity† | Complex chronic conditions | 2,979,244 (86) | 2,905,266 (86) | 2,673,865 (86) |
| Noncomplex chronic conditions | 376,788 (11) | 366,632 (11) | 351,792 (11) | |
| No chronic conditions | 91,567 (3) | 90,831 (3) | 88,634 (3) |
Determined based on the 2010 US Census.
Categorized using the Pediatric Medical Complexity Algorithm.20
Total primary care visit rates in 2020, compared to 2018 and 2019, were 60% lower during month +1 (incidence rate ratio [IRR] 0.40, 99% confidence interval [CI] 0.40–0.40; Table 2 ). Total primary care visit rates partially rebounded by the end of the study period (month +7) at which time 2020 visit rates were 17% below prior years (IRR 0.83, 99% CI 0.83–0.83).
Table 2.
Change in Primary Care Visit Rates Overall, by Enrollee Age, and by Specific Conditions, During the COVID-19 Pandemic (March 25–October 6, 2020) Compared to Average Rates of the Same 1-Month Intervals in 2018 and 2019
| Fraction of all Pediatric Primary Care Visits in January–October 2019, % | First Month of the COVID-19 Pandemic IRR (99% CI)* | Seventh Month of the COVID-19 Pandemic IRR (99% CI)* | |
|---|---|---|---|
| Total primary care visits | 100 | 0.40 (0.40–0.40) | 0.83 (0.83–0.83) |
| Preventive visits | 37 | 0.47 (0.47–0.47) | 1.08 (1.08–1.08) |
| Preventive visits by child age, y | |||
| 0–1 | 6 | 0.99 (0.99–0.99) | 1.00 (1.00–1.00)† |
| 1–4 | 13 | 0.57 (0.57–0.57) | 1.01 (1.01–1.01) |
| 5–11 | 9 | 0.22 (0.22–0.22) | 1.17 (1.17–1.17) |
| 12–<18 | 8 | 0.21 (0.21–0.21) | 1.26 (1.26–1.26) |
| Problem-focused visits | 63 | 0.37 (0.37–0.37) | 0.69 (0.68–0.69) |
| Problem-focused visits for selected conditions | |||
| Acute respiratory tract infection | 20 | 0.18 (0.18–0.19) | 0.37 (0.36–0.37) |
| Anxiety and depression | 1 | 0.88 (0.88–0.88) | 1.13 (1.13–1.13) |
| Asthma | 1 | 0.44 (0.44–0.44) | 0.40 (0.40–0.40) |
| Attention deficit hyperactivity disorder | 2 | 0.76 (0.76–0.76) | 0.89 (0.89–0.89) |
| Eczema | 0.4 | 0.73 (0.73–0.73) | 0.95 (0.95–0.95) |
| Gastroenteritis | 1 | 0.14 (0.14–0.14) | 0.20 (0.20–0.20) |
| Neonatal hyperbilirubinemia | 0.2 | 0.84 (0.84–0.84) | 0.87 (0.87–0.87) |
| Urinary tract infection | 0.3 | 0.64 (0.64–0.64) | 0.78 (0.77–0.78) |
| Administration of total noninfluenza vaccinations | N/A | 0.52 (0.52–0.52) | 1.04 (1.04–1.04) |
IRR indicates incidence rate ratio; COVID-19, coronavirus of 2019; and CI, confidence interval.
Child visit counts for specified 1-month intervals modeled using a series of individual-level Poisson regressions with an indicator variable for 2020 versus prior years and with standard errors adjusted for child-level clustering.
Rate 0.995 with 99% CI 0.995 to 0.996, displayed as 1.00 due to rounding.
Trends in Primary Care Preventive Visits
Preventive visits in 2020 abruptly declined after the start of the pandemic and then rebounded. In 2020, preventive visit rates across all ages in month + 1 were 53% lower than prior years (IRR 0.47, 99% CI 0.47–0.47; Table 2). By month +7, preventive visit rates in 2020 exceeded prior years by 8% (IRR 1.08, 99% CI 1.08–1.08; Table 2).
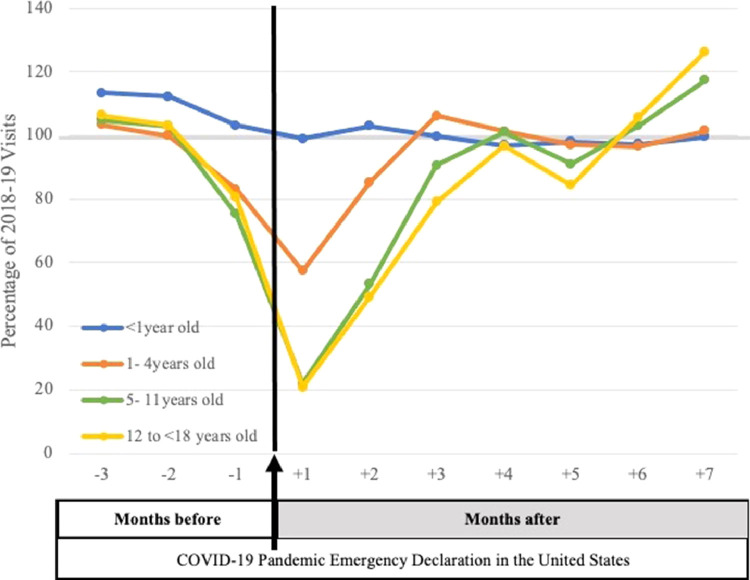
Preventive visit rates during this time period varied by child age group (Fig. 1 ). During month +1, larger declines in preventive visits in 2020 compared to prior years occurred for children aged 5 and older (5–11 year olds: IRR 0.22, 99% CI 0.22–0.22; 12–<18 year olds: IRR 0.21, 99% CI 0.21–0.21; Table 2). In contrast, children under 1 year of age experienced only a 1% relative decline in rates of preventive visits in month +1 compared to prior years (IRR 0.99, 99% CI 0.99–0.99).
Figure 1.
Preventive visits conducted by primary care clinicians by child age, 2020 volume as percentage of prior years 2018 to 2019. Rates of visits for the year 2020 as percentage of the rates from the same 1-month interval in prior years (averaged for 2018–2019) to a primary care clinician for preventive visits for various child ages. The vertical line indicates the beginning of the period defined as the COVID-19 pandemic period (March 25, 2020). Note: This study uses 2018 to 2020 claims data from the OptumLabs® Data Warehouse. The panels include individuals who had 10 months of continuous enrollment during the cohort year.
During month +7, the rates of preventive visits in 2020 matched or exceeded the rates in prior years for all age groups with a larger increase observed for older children (5–11 year olds: IRR 1.17, 99% CI 1.17–1.17; 12–<18 year olds IRR 1.26, 99% CI 1.26–1.26).
The cumulative number of preventive visits from January 1 to October 6, 2020 was 10% below usual (deficit of 69 preventive visits per 1000 children). During the studied pandemic period of 2020, telemedicine was used for 0.5% of all preventive visits.
Trends in Primary Care Problem-Focused Visits
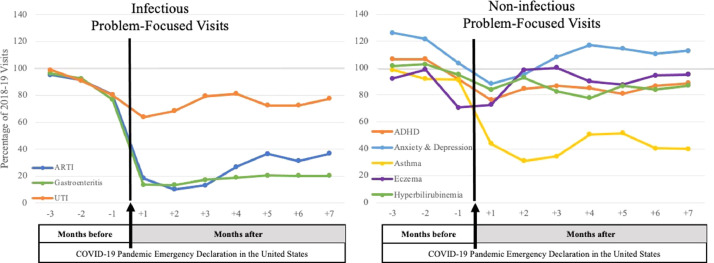
While problem-focused visits declined similarly to preventive visits early in the pandemic, problem-focused visit rates remained well below rates of prior years into the seventh month of the pandemic. Compared to 2018 and 2019 rates, problem-focused visit rates in 2020 were 63% lower during month +1 (IRR 0.37, 99% CI 0.37–0.37; Table 2) and 31% lower during month +7 (IRR 0.69, 99%CI 0.68–0.69).
We compared 2020 to 2018 and 2019 for 8 problem-focused conditions in month +7 (Fig. 2 ). In month + 7, visit rates in 2020 were substantially lower for ARTI (−63%, IRR 0.37, 99% CI 0.36–0.37), gastroenteritis (−80%, IRR 0.20, 99% CI 0.20–0.20), and asthma (−60%, IRR 0.40, 99% CI 0.40–0.40, Table 2). At the other extreme, visit rates for anxiety and depression were 13% higher than prior years during month +7 (IRR 1.13, 99% CI 1.13–1.13). The remaining conditions had 2020 visit rates ranging from 5% to 22% lower than prior years, including eczema (−5%), attention deficit-hyperactivity disorder (−11%), neonatal hyperbilirubinemia (−13%), and UTI (−22%). ARTIs accounted for 20% of total primary care visits in 2019; the other 7 conditions in total accounted for about 6% of total primary care visits in 2019.
Figure 2.
Problem-focused visits for 8 selected conditions conducted by primary care clinicians in 2020 as a percentage of prior years 2018 to 2019. Rates of visits for the year 2020 as percentage of the rates from the same 1-month interval in prior years (averaged for 2018–2019) to a primary care clinician for problem-focused visits for 8 selected conditions. The vertical line indicates the beginning of the period defined as the COVID-19 pandemic period (March 25, 2020). Note: This study uses 2018 to 2020 claims data from the OptumLabs® Data Warehouse. The panels include individuals who had 10 months of continuous enrollment during the cohort year.
Telemedicine was utilized for 24% of problem-focused visits in primary care during the studied pandemic period, ranging from 44% of visits in month +1 to 15% of visits in month +7.
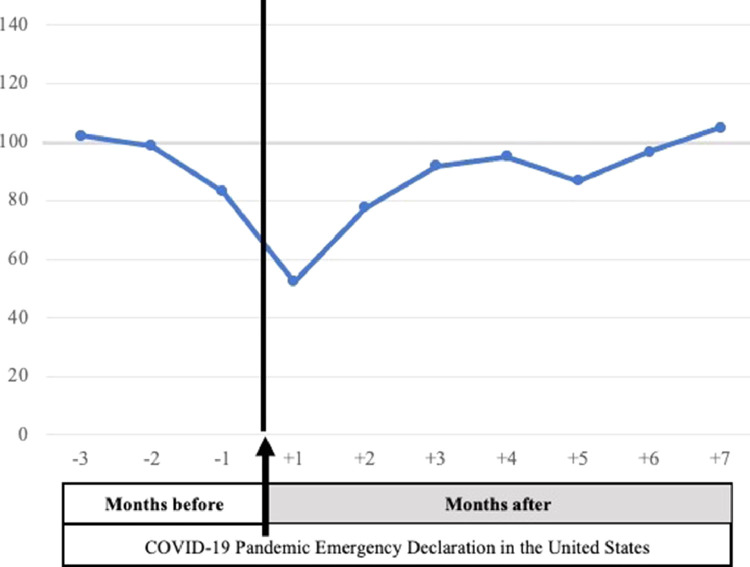
Vaccination Rates
Overall vaccine administration fluctuated with preventive visit rates (Fig. 3 ). Overall vaccine administration rates during month +1 were 48% below prior years (IRR 0.52, 99% CI 0.52–0.52) and by month +7 exceeded prior years by 4% (IRR 1.04, 99% CI 1.04–1.04). The cumulative vaccine deficit as of October 2020 was 10% below prior years (deficit of 43 vaccines per 1000 children), improved from a cumulative vaccine deficit as large as 17% in month +4.
Figure 3.
Noninfluenza immunizations administered in 2020 as percentage of prior years 2018 to 2019. Rates of immunizations administered for the year 2020 as percentage of the rates from the same 1-month interval in prior years (averaged for 2018–2019). The vertical line indicates the beginning of the period defined as the COVID-19 pandemic period (March 25, 2020). Note: This study uses 2018 to 2020 claims data from the OptumLabs® Data Warehouse. The panels include individuals who had 10 months of continuous enrollment during the cohort year.
Overall Pediatric Visits During Pandemic Period
Focusing on the 7-month pandemic period, there were 30% fewer primary care visits compared to the same period of 2018 and 2019. Compared to 2018 and 2019, visits to all other settings were also lower, with 38% fewer ED visits, 41% fewer urgent care visits, 25% fewer physician specialist visits, and 16% fewer non-physician clinician visits (Table 3 ). During the pandemic period, telemedicine was used for 12% of primary care visits, 2% of ED visits, 5% of urgent care visits, 23% of physician specialist visits, and 21% of nonphysician clinician visits (Table 3 ).
Table 3.
Distribution of Total Pediatric Visits per 1000 Child Enrollees by Visit Setting and Specialty During the COVID-19 Period (March 25–October 6, 2020)
| Visits per 1000 Child Enrollees |
||||
|---|---|---|---|---|
| 2018 | 2019 | 2020 | ||
| Primary care | In-person | 1282 | 1293 | 790 |
| Telemedicine | 4 | 7 | 111 | |
| Emergency department | In-person | 229 | 235 | 143 |
| Telemedicine | 2 | 2 | 4 | |
| Urgent care | In-person | 31 | 33 | 18 |
| Telemedicine | 0 | 0 | 1 | |
| Physician specialists | In-person | 395 | 398 | 231 |
| Telemedicine | 1 | 1 | 68 | |
| Nonphysician clinicians* | In-person | 90 | 108 | 66 |
| Telemedicine | 0 | 0 | 18 | |
COVID-19 indicates coronavirus of 2019.
Nonphysician clinicians include social workers, psychologists, physical therapists, etc.
Discussion
Among a national sample of commercially insured children, primary care visits were 60% below prior years in the first month of the pandemic and remained 17% below prior years in the seventh month of the pandemic. After the third month of the pandemic, lower visit rates were largely due to fewer problem-focused visits with notably fewer visits for infectious conditions such as ARTI and gastroenteritis. In contrast, by the seventh month of the pandemic, preventive visits and overall vaccine administration exceeded rates of prior years, although a cumulative deficit of preventive visits and vaccine administration remained as of October 2020.
Given the extensive public health efforts in place to reduce transmission of COVID-19, it would not be surprising that school and childcare center closures, universal masking, and physical distancing may have also reduced the number of children becoming ill with other viral infections, such as ARTIs and gastroenteritis. Fewer viral illnesses could also contribute to fewer acute asthma visits.23 Thus, the changes we describe in pediatric primary care settings provides outpatient context to complement recent studies describing the substantial reduction in pediatric influenza-related hospitalizations and deaths in 2020.10, 11, 12
We also observed modest reductions in visits for conditions such as UTIs and hyperbilirubinemia, conditions for which we would not expect the pandemic or associated public health measures to have a substantial impact on incidence of disease. This suggests that other factors, such as changes in family care-seeking behaviors or clinician recommendations, may have contributed. For example, families may choose not to seek care during this time because of concerns about exposure to COVID-19 in the clinic. Alternatively, clinicians may be increasingly coordinating care without clinic visits (eg, home nursing visits for hyperbilirubinemia, or specimen collection without a visit for dysuria) to support physical distancing. As the pandemic progressed and local responses evolved, there may have been further shifts in parent and clinician perceptions of the risks inherent in an in-person clinic visit. Specifically, local stay-at-home orders lifted over time and clinics worked to institute a range of strategies to support physical distancing in the office (eg, restricting the number of appointments, utilizing telemedicine visits, limiting types of conditions seen, maintaining adequate supply of personal protective equipment)17 , 34, 35, 36 which may contribute to the increased visit rates during the later pandemic period studied.
The modest increase in visits for depression and anxiety during month +7 is notable. Prior studies report increased mental health needs for children and adolescents during and after natural disasters in general and during the COVID-19 pandemic specifically.24 , 25 , 37, 38, 39, 40 Similarly, we found that visits for these diagnoses exceeded prior years for month +3 through month +7. One key question remaining is whether the observed increase in mental health visits met the demand or if substantial unmet need remained.
While it is reassuring that rates of preventive visits and vaccinations began to exceed rates of prior years by October 2020, it is important to acknowledge the cumulative deficit of the deferred care during the early months of the pandemic. For every 1000 children, we found a cumulative deficit of 43 vaccines not given between January and October 2020 relative to prior years. This finding in a national sample echoes findings from others about decreases in vaccine administration,41, 42, 43 and supports concerns that we may observe increases in vaccine-preventable diseases in the future if this deficit remains unaddressed.44 , 45
Our analysis has key limitations. Our sample was limited to a commercially insured population, and therefore may not generalize to children with other health insurance, commercial or public, or children without insurance. As Medicaid data become available, it will be important to examine the impact of the pandemic on utilization in this population. Additionally, our analysis also focused on volume of care, and cannot assess quality or outcomes of care received (or deferred). Further work will need to address the impact of these trends on clinical outcomes.
Conclusion
Among a national sample of commercially insured children, we found that decreased primary care visits by children from March 25 to October 6, 2020 were due primarily to fewer problem-focused visits. Among specific conditions examined, visits for ARTI and gastroenteritis were most substantially lower than prior years. Despite dramatic reductions early in the pandemic, rates of preventive visits, and vaccine administration rebounded and by the seventh month of the pandemic exceeded rates in prior years. However, as of October 2020, an unaddressed cumulative deficit remained for both preventive visits and vaccinations.
Acknowledgments
Financial statement: This work was supported in part by a Health Resources and Services Administration (HRSA) NRSA for Primary Care Research Award (T32 HP22240; KS), the National Institute of Mental Health Award Number (T32MH019733; SYP), the National Institute of Allergy and Infectious Diseases (R01AI148159; KNR), and the Commonwealth Fund (AM). The content is solely the responsibility of the authors and does not necessarily represent the official views of, nor an endorsement by, HRSA, HHS, the NIH, or the US Government.
Footnotes
The authors have no conflicts of interest to disclose.
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.acap.2021.04.031.
Appendix. SUPPLEMENTARY DATA
References
- 1.Mehrotra A, Chernew M, Linetsky D, et al. 2020. The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges. Accessed October 21, 2020. [DOI] [Google Scholar]
- 2.Epic Health Research Network . 2020. Expansion of Telehealth during COVID-19 Pandemic. Available at: https://ehrnprd.blob.core.windows.net/wordpress/pdfs/Expansions-in-Telehealth-COVID-19.pdf. Accessed October 26, 2020. [Google Scholar]
- 3.Martin K, Kurowski D, Given P, et al. Health Care Cost Institute; 2020. The Impact of COVID-19 on the Use of Preventive Health Care. Available at: https://healthcostinstitute.org/hcci-research/the-impact-of-covid-19-on-the-use-of-preventive-health-care. Accessed October 26, 2020. [Google Scholar]
- 4.Mehrotra A, Chernew M, Linetsky D, et al. 2020. The Impact of the COVID-19 Pandemic on Outpatient Care: Visits Return to Prepandemic Levels, But Not for All Providers and Patients. Accessed October 21, 2020. [DOI] [Google Scholar]
- 5.Mehrotra A, Chernew M, Linetsky D, et al. 2021. The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases. Accessed February 23, 2021. [DOI] [Google Scholar]
- 6.Gold J. Pediatric practices struggle to adapt and survive amid covid-19. The Washington Post. 2020 https://www.washingtonpost.com/health/pediatric-practices-struggle-to-adapt-and-survive-amid-covid-19/2020/04/10/1ec26648-78fc-11ea-a130-df573469f094_story.html Available at: Accessed June 11, 2021. [Google Scholar]
- 7.Goza SH, Wietecha M. American Academy of Pediatrics and Children's Hospital Association Letter to the Honorable Alex M. Azar, Secretary of the US Department of Health and Human Services. 2020.
- 8.Feemster K, Localio R, Grundmeier R, et al. Incidence of healthcare-associated influenza-like illness after a primary care encounter among young children. J Pediatr Infect Dis Soc. 2019;8:191–196. doi: 10.1093/jpids/piy023. [DOI] [PubMed] [Google Scholar]
- 9.Macy ML, Smith TL, Cartland J, et al. Parent-reported hesitancy to seek emergency care for children at the crest of the first wave of COVID-19 in Chicago. Acad Emerg Med. 2021 doi: 10.1111/acem.14214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S. Centers for Disease Control and Prevention . 2021. FluView: A Weekly U.S. Influenza Surveillance Report.https://www.cdc.gov/flu/weekly/index.htm#S3 Available at: Accessed February 17, 2021. [Google Scholar]
- 11.U.S. Centers for Disease Control and Prevention . 2021. The National Respiratory and Enteric Virus Surveillance System: Respiratory Syncytial Virus Surveillance. Available at: https://www.cdc.gov/surveillance/nrevss/rsv/natl-trend.html. Accessed February 23, 2021. [Google Scholar]
- 12.BioFire Syndromic Trends: Respiratory Pathogens Trends. syndromictrends.com. Accessed February 9, 2021.
- 13.Santoli J, Lindley M, DeSilva M. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:591–593. doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 14.Tseng P, Kaplan RS, Richman BD, et al. Administrative costs associated with physician billing and insurance-related activities at an academic health care system. JAMA. 2018;319:691–697. doi: 10.1001/jama.2017.19148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson JBA. The benefit of using both claims data and electronic medical record data in health care analysis. Optum. Available at:https://www.optum.com/content/dam/optum/resources/whitePapers/Benefits-of-using-both-claims-and-EMR-data-in-HC-analysis-WhitePaper-ACS.pdf. Accessed June 11, 2021
- 16.Centers for Medicare & Medicaid Services . 2020. List of Telehealth Services. Available at: https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes. Accessed July 15, 2020. [Google Scholar]
- 17.Centers for Medicare & Medicaid Services . Centers for Medicare & Medicaid Services; 2020. CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response. [Google Scholar]
- 18.Trump DJ. 2020. Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak. [Google Scholar]
- 19.WWAMI RUCA Rural Health Research Center. Four Category Classification, Census Division. Accessed July 15, 2020. Available at: http://depts.washington.edu/uwruca/ruca-maps.php
- 20.Simon TD, Haaland W, Hawley K, et al. Development and validation of the pediatric medical complexity algorithm (PMCA) version 3.0. Acad Pediatr. 2018;18:577–580. doi: 10.1016/j.acap.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ray KN, Shi Z, Ganguli I, et al. Trends in pediatric primary care visits among commercially insured US children, 2008-2016. JAMA Pediatr. 2020;174:350–357. doi: 10.1001/jamapediatrics.2019.5509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poon SJ, Schuur JD, Mehrotra A. Trends in visits to acute care venues for treatment of low-acuity conditions in the United States from 2008 to 2015. JAMA Intern Med. 2018;178:1342–1349. doi: 10.1001/jamainternmed.2018.3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheehan WJ, Patel SJ, Margolis RHF, et al. Pediatric asthma exacerbations during the COVID-19 pandemic: absence of the typical fall seasonal spike in Washington, DC. J Allergy Clin Immunol Pract. 2021 doi: 10.1016/j.jaip.2021.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 25.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4:421. doi: 10.1016/s2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ray KN, Shi Z, Gidengil CA, et al. Antibiotic prescribing during pediatric direct-to-consumer telemedicine visits. Pediatrics. 2019;143 doi: 10.1542/peds.2018-2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jagai JS, Smith GS, Schmid JE, et al. Trends in gastroenteritis-associated mortality in the United States, 1985-2005: variations by ICD-9 and ICD-10 codes. BMC Gastroenterol. 2014;14:211. doi: 10.1186/s12876-014-0211-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akmatov MK, Steffen A, Holstiege J, et al. Trends and regional variations in the administrative prevalence of attention-deficit/hyperactivity disorder among children and adolescents in Germany. Sci Rep. 2018;8:17029. doi: 10.1038/s41598-018-35048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ni J, Friedman H, Boyd BC, et al. Early antibiotic exposure and development of asthma and allergic rhinitis in childhood. BMC Pediatr. 2019;19:225. doi: 10.1186/s12887-019-1594-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thyssen JP, Corn G, Wohlfahrt J, et al. Retrospective markers of paediatric atopic dermatitis persistence after hospital diagnosis: a nationwide cohort study. Clin Exp Allergy. 2019;49:1455–1463. doi: 10.1111/cea.13487. [DOI] [PubMed] [Google Scholar]
- 31.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 32.Karaca Z, Moore BJ. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2006. Costs of emergency department visits for mental and substance use disorders in the United States, 2017: statistical brief #257. [PubMed] [Google Scholar]
- 33.Germanos G, Light P, Zoorob R, et al. Validating use of electronic health data to identify patients with urinary tract infections in outpatient settings. Antibiotics (Basel) 2020;9 doi: 10.3390/antibiotics9090536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Academy of Pediatrics; 2020. Caring for Children With Acute Illness in the Ambulatory Care Setting During the Public Health Emergency. Available at: https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/caring-for-children-with-acute-illness-in-the-ambulatory-care-setting-during-the-public-health-emergency/. Accessed February 17, 2021. [Google Scholar]
- 35.Livingston E, Desai A, Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020;323:1912–1914. doi: 10.1001/jama.2020.5317. [DOI] [PubMed] [Google Scholar]
- 36.Mehrotra A, Ray K, Brockmeyer DM, et al. Rapidly converting to “virtual practices”: outpatient care in the era of COVID-19. NEJM Catal Innov Care Deliv. 2020;1 doi: 10.1056/cat.20.0091. [DOI] [Google Scholar]
- 37.Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146 doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- 38.Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health-related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1675–1680. doi: 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Substance Abuse and Mental Health Services Administration . Disaster Technical Assistance Center Supplemental Research Bulletin; 2018. Behavioral Health Conditions in Children and Youth Exposed to Natural Disasters. Available at: https://www.samhsa.gov/sites/default/files/srb-childrenyouth-8-22-18.pdf. Accessed February 23, 2021. [Google Scholar]
- 40.Schweiberger K, Hoberman A, Iagnemma J, et al. Practice-level variation in telemedicine use in a pediatric primary care network during COVID-19. J Med Internet Res. 2020 doi: 10.2196/24345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bramer C, Kimmins L, Swanson R, et al. Decline in child vaccination coverage during the COVID-19 Pandemic—Michigan Care Improvement Registry, Mary 2016-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:630–631. doi: 10.15585/mmwr.mm6920e1. [DOI] [PubMed] [Google Scholar]
- 42.Blue Cross Blue Shield Association; 2020. The Blue Cross Blue Shield Association Reports Steep Decline in Childhood Vaccinations Due to COVID-19 Pandemic, Putting Community Protection at Risk. Available at: https://www.bcbs.com/press-releases/the-blue-cross-blue-shield-association-reports-steep-decline-childhood-vaccinations. Accessed February 17, 2021. [Google Scholar]
- 43.O'Leary ST, Trefren L, Roth H, et al. Number of childhood and adolescent vaccinations administered before and after the COVID-19 outbreak in Colorado. JAMA Pediatr. 2021;175:305–307. doi: 10.1001/jamapediatrics.2020.4733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feldman AG, O'Leary ST, Isakov LD. The risk of resurgence in vaccine preventable infections due to COVID-related gaps in immunization. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.At least 80 million children under one at risk of diseases such as diphtheria, measles and polio as COVID-19 disrupts routine vaccination efforts, warn Gavi, WHO and UNICEF. News Release. 2020. Available at:https://www.who.int/news/item/22-05-2020-at-least-80-million-children-under-one-at-risk-of-diseases-such-as-diphtheria-measles-and-polio-as-covid-19-disrupts-routine-vaccination-efforts-warn-gavi-who-and-unicef. Accessed February 22, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.