Abstract
Objective
To understand the impact of the coronavirus disease 2019 (COVID-19) pandemic on parental perceptions of health behaviors and food insecurity among children with overweight and obesity living in San Francisco and to assess the relationship between food insecurity and dietary intake during the pandemic.
Methods
Parents of children ages 4 to 12 in San Francisco with body mass index ≥85th percentile measured at a clinic visit at a Federally Qualified Health Center or academic practice from January 1st to March 15th, 2020 were eligible to participate. Parents completed a survey reporting on child health behaviors and household food insecurity prior to and since the start of the pandemic. Survey items were abstracted from validated surveys with adaptations. Regression models evaluated associations between food insecurity and dietary intake variables.
Results
Most participants (n = 145) were publicly insured (90%), Latino (77%), and spoke Spanish at home (70%). Parents perceived that child mean daily nonacademic screen time was higher during the pandemic compared to before (3.8 hours vs 1.6 hours). Mean daily physical activity was reported to be lower compared to prior to the pandemic (1 hour vs 1.8 hours). On average, reported bedtime shifted 1.6 hours later. Food insecurity increased significantly but was not associated with intake of fruits, vegetables, sugar-sweetened beverages, or foods with added sugar during the pandemic.
Conclusions
Parents of children with overweight or obesity in San Francisco perceive increased child screen time, decreased physical activity and later bedtimes during the COVID-19 pandemic. Findings suggest a need for policies that support healthy lifestyle behaviors among low-income children during the pandemic.
Keywords: COVID-19 pandemic, dietary intake, physical activity, screen time, sleep
What's New.
During the coronavirus disease 2019 pandemic, children with overweight and obesity living in San Francisco, CA have increased screen time, decreased physical activity, and are going to bed later. This population has also experienced a large increase in food insecurity.
Alt-text: Unlabelled box
While children are at low risk of serious morbidity or death from coronavirus disease 2019 (COVID-19) disease,1 pandemic mitigation strategies may have negative effects on child health. Childhood obesity is highly prevalent in the United States2 and increases risk for hypertension,3 dyslipidemia,4 and type 2 diabetes.5 Pandemic containment strategies that result in the closure of schools, recreational programs, and playgrounds may worsen obesity and children's cardiovascular health.6, 7, 8, 9 School attendance is protective against increases in obesity,10 and both physical activity and adequate sleep are critical for preventing excess weight gain; earlier bedtimes are also associated with lower child body mass index (BMI).11, 12, 13 Children's BMI percentiles tend to decrease or plateau during the school year and increase over the summer break.14, 15, 16 Furthermore, summer time effects on BMI are most prominent in children with overweight or obesity10 and among Latino and African-American children.16 These groups, which already shoulder disproportionate direct effects of COVID-19,17 may be at highest risk of obesity related health disparities due to school closures.1
The reasons why school attendance promotes healthier weight trajectories among children are not entirely clear, but likely include increased opportunities for structured physical activity, decreased screen time, healthier meal options at school, fewer opportunities for snacking, and earlier school day bedtimes.13 , 18 , 19 Shelter-in-place orders may have a greater impact on children's cardiovascular and metabolic health than summer time school closures alone because of the concurrent closures of schools, parks, and recreational facilities.20 In addition, widespread job loss resulting in higher rates of household food insecurity may lead to lower consumption of fruits and vegetables and higher consumption of processed foods and beverages.21, 22, 23 Understanding how pandemic mitigation approaches affect child health behaviors including physical activity, screen time, sleep and diet as well as the impact on household food insecurity is critical to creating policies that protect the community while doing the least harm to children.
Studies to date have documented parental perceptions that school age children have decreased their daily physical activity and increased sedentary time during the pandemic24 , 25 and have also revealed increased intake of high-calorie nutrient foods and beverages.26 In addition, a multinational study of adolescent dietary behavior found increased intake of fried foods and sweets compared to before the pandemic, as well as increased consumption of fruits, vegetables, and legumes.27 A key limitation of the current literature on the relationship between COVID mitigation strategies and child health behaviors is the paucity of data on low-income and racial-ethnic minority children in the United States.
To address the current gap, we conducted a study among a mainly low-income sample of children ages 4 to 12 years in San Francisco, CA with BMI ≥ 85th percentile. Our objectives were to determine parents’ perceptions of patterns of child screen time, physical activity, dietary intake, and bedtime during the COVID-19 pandemic compared to prior to the imposition of shelter-in-place orders in mid-March 2020 which led to closures of schools, playgrounds and recreational facilities. Second, we evaluated the prevalence of food insecurity before and after the start of shelter-in-place orders and determined whether food insecurity was associated with reported child intake of fruits and vegetables, sugar-sweetened beverages (SSBs), and foods high in added sugar during the pandemic.
Methods
Study Design
This was a cross-sectional study. Data were collected via a one-time survey. Parents reported on family demographics, child health behaviors before and after the start of the pandemic and family food insecurity before and after the start of the pandemic. Parents were given the option of completing the survey verbally by phone with a research assistant or on their own via an e-mailed link to an electronic survey.
Recruitment and Procedures
Eligibility criteria included the child being between the ages of 4 and 12 at the start of the study and having a BMI ≥ 85th percentile measured at a clinic visit at either the Zuckerberg San Francisco General Hospital Children's Health Center, a federally qualified health center, or 1 of 4 University of California San Francisco Health primary care sites in San Francisco between January 1st and March 15th 2020. The Zuckerberg San Francisco General Hospital Children's Health Center serves publicly insured children only, while University of California San Francisco Health primary sites serve both private and publicly insured children. Exclusion criteria included parents speaking a language other than English or Spanish, the child having a medical condition that predisposes to obesity, or the child taking medications that cause weight gain (ie, antipsychotics). Potential participants were identified via medical records search. Primary care providers of each potential participant were then contacted to confirm that the child met eligibility criteria. Research staff called parents and briefly explained the study to them. If parents were interested, research staff provided full details of the study and obtained a verbal consent. An information sheet was then mailed to all parents who consented. The survey was available for completion in English and Spanish and research staff were bilingual. Parents received a $25 gift card in the mail after completing the survey. All recruitment took place in June, July and August 2020. The study was approved by the IRB of the University of California San Francisco.
Study Variables
Child nonacademic screen time: To assess screen time, parents were asked “About how much time did your child spend on screen time on a typical weekday before the start of the shelter-in-place order on March 16th, 2020? Please include any time that your child spent watching television shows, watching videos or movies, and playing video games on a TV, laptop, cell phone, iPad/tablet, or videogame system. Please do not include time spent doing school work.” Response options included “0 minutes,” “30 minutes,” “1 hour,” “2 hours,” “3 hours,” “4 hours,” “5 hours,” “6 hours,” “7 hours,” “8 hours,” and “greater than 8 hours.” The question was then asked again about a typical weekday since March 16th, 2020. This question was adapted from a question from the National Health and Nutrition Examination Survey to include a broader array of different nontelevision screen time options and to specifically exclude academic screen time.28
Child physical activity: To assess physical activity, parents were asked “On a typical day before the start of shelter-in-place on March 16th 2020, about how much total time did your child spend doing physical activity? Add up all the time he or she spent in any kind of physical activity that increased his/her heart rate and made him/her breathe hard some of the time.” The response options included: “0 minutes,” “15 minutes,” “30 minutes,” “45 minutes,” “1 hour,” “2 hours,” “3 hours,” “4 hours,” and “greater than 4 hours.” The question was then repeated to ask about physical activity on a typical day since March 16, 2020. This question was adapted from a question in the National Health and Nutrition Examination Survey 2019–2020 survey.28 We used the same wording to describe physical activity but asked parents to specify the amount of physical activity on a typical day rather than the number of days per week that the child exceeds 60 minutes of physical activity. We made this change as we anticipated that some children may fail to ever meet the 60-minute threshold but may still do regular physical activity. Parents were then asked whether their child had done any of the following since the start of the shelter-in-place order: 1) “gone outside to walk, run, or ride a bike?” 2) “played outside,” or 3) “done any exercise videos.” If parents answered yes, they were asked how often the child engaged in the activity with the following response options: “less than once a week,” “1 to 2 × per week,” “3 to 4 × per week,” “5 to 6 × per week,” and “every day.” Finally, parents were asked “Do you have an outdoor space that is part of your home or apartment building where your child can play during shelter-in-place?”
Child bedtime: To assess child bedtime, parents were asked “On a typical weekday before the start of the shelter-in-place order, about what time did your child go to bed at night?” The response options were in half hour increments from “6:00 pm” to “midnight” and “after midnight.” Parents were then asked about their child's bedtime on a typical weekday since March 16, 2020.
Child dietary intake: We asked parents to quantify child dietary intake in servings during the pandemic only. We also assessed parents’ overall perception of change in intake for each category of food and beverages from prior to the pandemic. To assess SSB intake, we asked “In the past 7 days, on how many days has your child had a beverage with added sugar including soda, sweetened fruit drinks like Snapple and Capri Sun, sports drinks, lemonade, or agua fresca?.” They were then asked “On the days that your child drank beverages with added sugar, how many servings did he/she have? A serving is 8 ounces.”29 Parents were then asked whether they thought their child was drinking “more” “less” or “the same” amount of SSBs compared to prior to the start of the shelter-in-place order. To assess fruit intake, parents were asked on how many days their child consumed fruit in the previous week and how many servings they consumed on the days they ate fruit, with a serving defined as 1 piece of fruit or 1 cup of chopped fruit. Vegetable intake was determined with an identical question. A serving of vegetables was defined as 1 cup of raw or cooked vegetables.30 Parents were then asked whether their child was eating “more,” “less,” or “the same” amount of fruits and vegetables compared to prior to the shelter-in-place order. Finally, intake of foods high in added sugar was assessed via the following question: “In the past 7 days, on how many days has your child eaten foods with added sugar including cookies, ice cream, cake, chocolate, candy, pan dulce, and pastries?” Parents were then asked whether their child was eating “more” “less” or “the same” amount of foods with added sugar compared to prior to the start of the pandemic.
Food insecurity: We assessed household food insecurity prior to March 16th 2020 and since March 16th 2020 using the 2-item Hunger Vital Sign 31 which asks participants to listen to or read 2 statements describing food insecurity and reply with “often true” “sometimes true” or “never true.” In addition, the survey asked if children had received free or reduced price lunch at school prior to the pandemic and whether they had been receiving schools meals since schools closed. We also asked whether the family had received food from local food banks.
Demographics: Parents reported on basic child demographics including the child's sex, grade level in March 2020, type of school (public, charter, or private), insurance type, and race-ethnicity. Parents reported their own highest educational level, country of origin, the primary language spoken in the home, whether they were employed prior to the start of the pandemic and impacts of the pandemic on their employment and household income. The complete survey was piloted with 2 parents prior to starting the study to ensure clarity of the questions.
Analysis
We used descriptive statistics to analyze demographic data, types of child physical activity during the pandemic, presence or absence of an outdoor space where children can play, child intake of fruits, vegetables, SSBs, and foods with added sugar. Children were considered to engage in outside physical activity if parents reported that they were either “going outside to walk, run, or ride a bike” at least once per week or “playing outside” at least once per week. We compared parents’ reports of mean daily screen time on weekdays, mean daily physical activity, and bedtime after 10 pm prior to and during the pandemic. For the most conservative estimates, participants whose parents reported greater than 8 hours of daily screen time were coded as engaging in 8 hours of daily screen time and those whose parents reported greater than 4 hours of daily physical activity were coded as being active for 4 hours each day. Participants were designated as food insecure for a given time period if parents responded “sometimes true” or “often true” to either of the 2 Hunger Vital Sign questions. We used a paired sample t test to test significance in comparison of means and a chi-square for comparisons of proportions.
We used linear regression to test associations between food insecurity during the pandemic and child dietary intake during the pandemic.
Results
There were 322 potential children identified by medical records search and confirmed eligible by their PCPs. The research team was able to reach 200 parents on the phone, of whom 163 consented to participate and 145 completed the survey. Of those, 79% of completed the survey verbally over the phone and 21% of parents completed the survey electronically via an e-mailed survey link provided by the research team. The majority of participants were publicly insured, Latino, and primarily spoke Spanish at home (Table 1 ). Of parents surveyed, 55% reported losing their only job since March 16, 2020 and 81% reported a decrease in their household income as a result of the pandemic.
Table 1.
Child and Parent Demographic Characteristics in a Study of Parent's Perceptions of Child Health Behaviors During the COVID-19 Pandemic Among Children Ages 4–12 in San Francisco, CA (n = 145)
| Child Demographics | % |
| Sex | |
| Male | 45 |
| Female | 55 |
| Grade level at start of shelter-in-place | |
| Not yet in school | 3 |
| Preschool or TK | 22 |
| K–1st | 20 |
| 2–3 | 24 |
| 4–5 | 23 |
| 6–7 | 6 |
| Insurance type | |
| Public | 90 |
| Private | 10 |
| Race-ethnicity | |
| Latino | 77 |
| African-American | 8 |
| Asian | 2 |
| White | 2 |
| Pacific Islander | 0.7 |
| Mixed race-ethnicity | 10 |
| Main language spoken in home | |
| Spanish | 70 |
| English | 27 |
| Other | 3 |
| Parent Demographics | |
| Parent country of origin | |
| United States | 25 |
| Mexico | 30 |
| El Salvador | 22 |
| Guatemala | 9 |
| Honduras | 8 |
| Peru | 4 |
| Other | 6 |
| Parent educational level | |
| Less than high school degree | 36 |
| High school degree | 48 |
| College degree or beyond | 16 |
| Employed outside the home prior to March 16, 2020 | 70 |
COVID-19 indicates coronavirus disease 2019.
Screen time: Parents perceived that mean daily nonacademic screen time on weekdays was more than twice as high during the pandemic compared to prior to the pandemic (Table 2).
Table 2.
Parent Report of Child Health Behaviors, Food Insecurity, and Use of Food Resources Prior to and During the COVID-19 Pandemic Among a Predominantly Low-Income Sample of Children Ages 4–12 in San Francisco, CA (n = 145)
| Variable | Prepandemic | During Pandemic | P Value |
|---|---|---|---|
| Nonacademic screen time | |||
| Mean daily nonacademic screen time | 1.6 h (SD 1.3) | 3.8 h (SD 2.2) | <.001 |
| Mean daily nonacademic screen time ≥4 h per day | 6% | 52% | <.001 |
| Physical activity | |||
| Mean daily physical activity | 1.8 h (SD 1.2) | 1 h (SD 1) | <.001 |
| Bedtime | |||
| Bedtime after 10 pm | 3% | 65% | <.001 |
| Food insecurity and resources | |||
| Household food insecurity | 48% | 71% | <.001 |
| Use of foodbanks | 35% | 54% | <.001 |
| Receive free or reduced price meals from child's school | 78% | 60% | <.001 |
COVID-19 indicates coronavirus disease 2019; SD, standard deviation.
Physical activity: Parents perceived that mean daily physical activity decreased substantially during the pandemic (Table 2). Parents reported that 45% of children had no place to play outdoors at their home or apartment building. Children who did not have an outdoor space to play had lower daily physical activity compared to those who had an outdoor space (52 minutes vs 76 minutes; P = .02). In addition, 28% of children were reported to engage in no outdoor physical activity.
Bedtime: On average, parents reported that bedtime shifted 1.6 hours later during the pandemic and a significantly larger proportion of participants were reported to go to bed after 10 pm (Table 2).
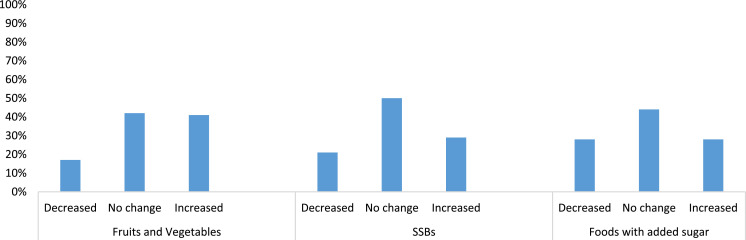
Dietary intake: Parents reported that participants consumed a mean of 16.8 (standard deviation [SD] 8.9) servings per week of fruit, 8.6 (SD 8.9) servings per week of vegetables, and 5.8 (SD 6.7) servings per week of SSBs during the pandemic. Participants consumed foods with added sugar on average 2.5 (SD 2) days each week during the pandemic. Figure depicts parents’ report of change in consumption of fruits and vegetables, SSBs, and foods with added sugar.
Figure.
Percent of parents reporting decrease, no change, and increase in child intake of fruits and vegetables, sugar-sweetened beverages (SSBs), and foods with added sugar during the coronavirus disease 2019 pandemic among children ages 4–12 with overweight and obesity in San Francisco, CA.
Food insecurity: Food insecurity was reported to be high prior to the pandemic with a marked increase during the pandemic (Table 2). Relative to the prepandemic period, more families were accessing food banks, yet fewer children were receiving school meals (Table 2). We found no association between food insecurity during the pandemic and child consumption of fruits and vegetables, SSBs, or foods with added sugar during the pandemic.
Discussion
Our study found a significant shift in parentally perceived health behaviors during the COVID-19 pandemic among children ages 4 to 12 with overweight and obesity in San Francisco, CA. Key findings include parents’ perceptions of greater screen time, less physical activity, and later bedtimes. We also found that 28% of participants were not engaging in any outdoor physical activity and 45% did not have access to a place to play outdoors at home. Children with an outdoor space in which to play at home reported more physical activity. Further, we found a steep increase in food insecurity among study participants. And while the majority of families were accessing food banks, fewer children were receiving school meals during the pandemic relative to the prepandemic period.
Our findings that parents perceived decreased child physical activity and increased screen time are consistent with 2 Internet based-survey studies of parents of mainly white, upper-income children in Canada and the United States. Both studies found generally that parents perceived changes in physical activity and screen time, but did not quantify the changes.24 , 25 A study of health behaviors among Italian children with baseline obesity found much steeper increases in screen time. However, it was conducted during a period of very strict lockdown in Italy in which children were not allowed to leave their homes other than to seek medical care.26
Our finding of a large increase in food insecurity is consistent with national trends, such as an analysis of the Census Household Pulse Survey which found that household food insecurity has doubled overall and tripled in households with children.32 We did not find, however, any association between food insecurity and fruit and vegetable intake during the pandemic as has been seen in previous research.21 We also found that only 17% of families reported decreased intake of fruits and vegetables with 41% actually reporting an increase. This may be because a significant proportion of families were accessing food banks and may receive fresh produce at these sites. School meal distribution sites in San Francisco also provide fresh produce in addition to prepackaged meals. In addition, families of school aged children in California who qualify for free or reduced price school meals were eligible for a one-time $350 food benefit in the Spring and Summer of 2020 (pandemic electronic benefit transfer) which some families may have used to purchase produce. Transnational studies have also found an increase in fruit26 , 27 and vegetable27 intake since the start of the pandemic, which may stem from preparing more meals at home.
It is important to consider our results within the local policy context. All schools were ordered closed for in-person learning in San Francisco beginning on March 16th, 2020 and public schools remained closed until mid-April 2021 when elementary schools began to open. School meals were provided during the closures, but the pick-ups were limited to a narrow time window once or twice per week and only offered at a select number of schools. Thus, families may have had difficulty accessing meals due to transportation barriers and work obligations. The mandate to close also included San Francisco playgrounds and city owned recreational facilities including pools and basketball courts. Playgrounds and basketball courts did not reopen until October 13th, 2020 and city pools remain closed to children under the age of 14 as of May 2021. Summer camps were authorized to open beginning in mid-June 2020. However, capacity at camps that normally serve low-income children was extremely limited, and many organizations only offered on-line options for the summer of 2020.
There are a number of important limitations to our study. The data were based on parental report which is subject to social desirability bias and parents may have had trouble accurately recalling their child's prepandemic behaviors. Furthermore, parents were only surveyed once, and thus we are not able to evaluate how health behaviors evolved. And parents’ perceptions of changes in child health behaviors may have been impacted by their views on mitigation policies. In addition, our survey relied on a single item to assess each outcome rather than using full-length validated tools. This was intentional as we wished to keep the survey short to encourage participation during a period of high stress for parents, but does limit conclusions that can be drawn. In addition, due to our small sample size we were not able to provide meaningful estimates for subgroups within our sample. Finally, our findings may not be applicable to regions of the United States which took a different approach to closures of schools and other services for children and where resources to address food insecurity may not consistently provide fresh produce. Despite these limitations, our study has important implications. Pandemic mitigation approaches appear to have had a negative impact on behaviors that impact cardiovascular and metabolic health in our study population of largely low-income children with overweight and obesity. Our findings raise serious concern that pandemic mitigation strategies will lead to excess weight gain and worsening cardiovascular and metabolic health among a highly vulnerable population of children.
It is critical for policy makers to promote pandemic mitigation approaches that safeguard children's cardiovascular and metabolic health and address disparities in access to recreational activities and outdoor play. Given research on the generally benign impacts of COVID-19 disease on children,33 the safety of outdoor activities,34 the safety of in-person learning with appropriate mitigation strategies,35 , 36 and the efficacy of vaccines in protecting adults from serious illness,37 it is clear that such approaches should include keeping playgrounds and other outdoor recreation spaces open and resuming 5 days per week in-person learning (with opportunities for recess and physical education). In particular, it will be very important to ensure access to camps and recreational programs during the summer as well as options for physical activity and sports during the school year. It is also critical that options for physical activity and recreation be available to low-income children at free or reduced cost. Furthermore, additional measures are needed to address the crisis of food insecurity among households with children including increasing Supplemental Nutrition Assistance Program benefits, expanding Supplemental Nutrition Assistance Program eligibility, and providing additional funds for the pandemic electronic benefit transfer program for children who remain out of school. Pediatric care providers should assess the impacts of pandemic related closures on child health behaviors, refer for food resources and work with families to identify opportunities for increasing physical activity, decreasing screen time, and adjusting child bedtimes. Providers should also provide reassurance regarding the safety of outdoor physical activity with respect to viral transmission. Finally, pediatric care providers and policy makers should assume that there will be an increase in children needing interventions to treat obesity and obesity comorbidities and should plan for increasing services and capacity.
Acknowledgments
Financial statement: This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1K23HD080876-01A1) to A.B., and the National Heart Lung and Blood Institute (1K01HL129087-01A1) to S.M.
Role of sponsors: The study sponsors had no role in study design, collection, analysis, interpretation of data, the writing of the manuscript, and the decision to submit the manuscript for publication.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109:1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skinner AC, Ravanbakht SN, Skelton JA, et al. Prevalence of obesity and severe obesity in US children, 1999-2016. Pediatrics. 2018;141 doi: 10.1542/peds.2017-3459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140 doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 4.Deeb A, Attia S, Mahmoud S, et al. Dyslipidemia and fatty liver disease in overweight and obese children. J Obes. 2018;2018 doi: 10.1155/2018/8626818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pulgaron ER, Delamater AM. Obesity and type 2 diabetes in children: epidemiology and treatment. Curr Diab Rep. 2014;14:508. doi: 10.1007/s11892-014-0508-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rundle AG, Park Y, Herbstman JB, et al. COVID-19 related school closings and risk of weight gain among children. Obesity. 2020;28:1008–1009. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cuschieri S, Grech S. COVID-19: a one-way ticket to a global childhood obesity crisis? J Diabetes Metab Disord. Published online November 6, 2020:1-4. 10.1007/s40200-020-00682-2. [DOI] [PMC free article] [PubMed]
- 8.Storz MA. The COVID-19 pandemic: an unprecedented tragedy in the battle against childhood obesity. Clin Exp Pediatr. 2020;63:477–482. doi: 10.3345/cep.2020.01081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. 2020;9:302–312. doi: 10.1016/j.jshs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baranowski T, O'Connor T, Johnston C, et al. School year versus summer differences in child weight gain: a narrative review. ChildObes Print. 2014;10:18–24. doi: 10.1089/chi.2013.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hills AP, Andersen LB, Byrne NM. Physical activity and obesity in children. Br J Sports Med. 2011;45:866–870. doi: 10.1136/bjsports-2011-090199. [DOI] [PubMed] [Google Scholar]
- 12.Martinez SM, Greenspan LC, Butte NF, et al. Mother-reported sleep, accelerometer-estimated sleep and weight status in Mexican American children: sleep duration is associated with increased adiposity and risk for overweight/obese status. J Sleep Res. 2014;23:326–334. doi: 10.1111/jsr.12114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Venkatapoorna CMK, Ayine P, Selvaraju V, et al. The relationship between obesity and sleep timing behavior, television exposure, and dinnertime among elementary school-age children. J Clin Sleep Med JCSM. 2020;16:129–136. doi: 10.5664/jcsm.8080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moreno JP, Johnston CA, Chen T-A, et al. Seasonal variability in weight change during elementary school. Obes Silver Spring Md. 2015;23:422–428. doi: 10.1002/oby.20977. [DOI] [PubMed] [Google Scholar]
- 15.von Hippel PT, Workman J. From kindergarten through second grade, U.S. children's obesity prevalence grows only during summer vacations. Obes Silver Spring Md. 2016;24:2296–2300. doi: 10.1002/oby.21613. [DOI] [PubMed] [Google Scholar]
- 16.Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014;11:E101. doi: 10.5888/pcd11.130355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Y-H, Glymour MM, Catalano R, et al. Excess mortality in California during the coronavirus disease 2019 pandemic, March to August 2020. JAMA Intern Med. 2021;181:705–707. doi: 10.1001/jamainternmed.2020.7578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weaver RG, Beets MW, Brazendale K, et al. Summer weight gain and fitness loss: causes and potential solutions. Am J Lifestyle Med. 2019;13:116–128. doi: 10.1177/1559827617750576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martinez SM, Tschann JM, McCulloch CE, et al. Temporal associations between circadian sleep and activity patterns in Mexican American children. Sleep Health. 2019;5:201–207. doi: 10.1016/j.sleh.2018.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reuben A, Rutherford GW, James J, et al. Association of neighborhood parks with child health in the United States. Prev Med. 2020;141 doi: 10.1016/j.ypmed.2020.106265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr. 2014;100:684–692. doi: 10.3945/ajcn.114.084525. [DOI] [PubMed] [Google Scholar]
- 22.Eicher-Miller HA, Zhao Y. Evidence for the age-specific relationship of food insecurity and key dietary outcomes among US children and adolescents. Nutr Res Rev. 2018;31:98–113. doi: 10.1017/S0954422417000245. [DOI] [PubMed] [Google Scholar]
- 23.Lee J, Kubik MY, Fulkerson JA. Diet quality and fruit, vegetable, and sugar-sweetened beverage consumption by household food insecurity among 8- to 12-year-old children during summer months. J Acad Nutr Diet. 2019;119:1695–1702. doi: 10.1016/j.jand.2019.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17:85. doi: 10.1186/s12966-020-00987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20:1351. doi: 10.1186/s12889-020-09429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obes Silver Spring Md. 2020;28:1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruiz-Roso MB, de Carvalho Padilha P, Mantilla-Escalante DC, et al. Covid-19 confinement and changes of adolescent's dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020;12 doi: 10.3390/nu12061807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.NHANES, 2019-2020 Questionnaire Instruments. Available at:https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/questionnaires.aspx?BeginYear=2019. Accessed July 22, 2021.
- 29.Beck AL, Tschann J, Butte NF, et al. Association of beverage consumption with obesity in Mexican American children. Public Health Nutr. 2014;17:338–344. doi: 10.1017/S1368980012005514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yaroch AL, Tooze J, Thompson FE, et al. Evaluation of three short dietary instruments to assess fruit and vegetable intake: the National Cancer Institute's food attitudes and behaviors survey. J Acad Nutr Diet. 2012;112:1570–1577. doi: 10.1016/j.jand.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gattu RK, Paik G, Wang Y, et al. The hunger vital sign identifies household food insecurity among children in emergency departments and primary care. Child Basel Switz. 2019;6 doi: 10.3390/children6100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schanzenbach DW, Pitts A. 2020. How much has food insecurity risen? Evidence from the Census Household Pulse Survey.https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-researchreports-pulse-hh-data-10-june-2020.pdf Available at: [Google Scholar]
- 33.Munro APS, Faust SN. COVID-19 in children: current evidence and key questions. Curr Opin Infect Dis. 2020;33:540–547. doi: 10.1097/QCO.0000000000000690. [DOI] [PubMed] [Google Scholar]
- 34.Bulfone TC, Malekinejad M, Rutherford GW, et al. Outdoor transmission of SARS-CoV-2 and other respiratory viruses, a systematic review. J Infect Dis. 2021;223:550–561. doi: 10.1093/infdis/jiaa742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zimmerman KO, Akinboyo IC, Brookhart MA, et al. Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics. 2021;147 doi: 10.1542/peds.2020-048090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Falk A, Benda A, Falk P, et al. COVID-19 cases and transmission in 17 K-12 schools – Wood County, Wisconsin, August 31–November 29, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:136–140. doi: 10.15585/mmwr.mm7004e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384:1412–1423. doi: 10.1056/NEJMoa2101765. [DOI] [PMC free article] [PubMed] [Google Scholar]