Abstract
This review compared the clinical results of transepithelial corneal crosslinking (CXL) to epithelium-off (epi-off) CXL in progressive corneal ectasia using a metaanalysis. The Cochrane databases and Medline were searched for randomized controlled trials (RCTs). Seven RCTs involving 505 eyes that met the eligibility criteria were identified. The epi-off CXL group showed significantly better outcomes in postoperative changes in maximum keratometry (K) during 1-year observation periods. Transepithelial CXL resulted in significantly greater post-treatment central corneal thickness and best spectacle-corrected visual acuity (BSCVA). The presence of a postoperative demarcation line was significantly more frequent after epi-off CXL than that after transepithelial CXL. No statistically significant difference was found between other parameters. Although patients in the transepithelial CXL group demonstrated a greater improvement in BSCVA compared with patients in the epi-off CXL group at the 1 year follow-up, transepithelial CXL had less impact on halting progressive corneal ectasia in terms of maximum K than epi-off CXL.
Keratoconus is characterized as a bilateral, noninflammatory, progressive corneal ectasia.1 It results in corneal thinning and protrusion, progressive myopia, and irregular astigmatism. Although only 26.8% of patients with keratoconus progress to requiring corneal transplantation for visual recovery,2 keratoconus remains the most common indication for corneal transplantation surgery.3
Corneal crosslinking (CXL) was first introduced as a promising technique to slow or stop the progression of corneal ectasia.4 In CXL, riboflavin (vitamin B2) is administered in conjunction with ultraviolet-A (riboflavin–UVA, 365 nm). The riboflavin–UVA interaction leads to the formation of reactive oxygen species, which leads to the formation of additional covalent bonds between collagen molecules, with consequent biomechanical stiffening of the cornea.5 Since the first clinical study was published by Wollensak et al.,4 there has been an increasing number of published studies6–10 reporting the safety and efficacy of the treatment in slowing down or halting the progression of corneal ectasia. However, debriding the epithelium involves the inherent risk for corneal infection, subepithelial haze, sterile corneal infiltrates, corneal scarring, endothelial damage, and herpetic activation. Performing CXL with intact epithelium was proposed to avoid patient discomfort, a delay in visual recovery, and potential risks associated with epithelial removal.11 For transepithelial CXL to work, modification of the standard protocol is required to allow adequate stromal permeation of riboflavin through the epithelial barrier. However, it is presently unknown whether any transepithelial technique is as effective in treating progressive corneal ectasia as the standard epithelium-off (epi-off) technique,12 and there is only a scarcity of randomized controlled trials (RCTs) comparing different techniques in corneal ectasia within the literature.13–19 To provide powerful evidence for the widespread clinical practice of these therapeutic techniques, we undertook this metaanalysis of all published RCTs to compare the clinical effects and safety of transepithelial CXL with epi-off CXL in progressive corneal ectasia.
MATERIALS AND METHODS
This metaanalysis was performed in an academic medical setting in accord with the Preferred Reporting Items for Systematic Reviews and Metaanalyses (PRISMA) guidelines.20 The PRISMA checklist is included in Supplement 1 (available at http://jcrsjournal.org).
Study Selection
Two reviewers searched the Medline, Embase, and the Cochrane Central Register of Controlled Trials databases for publications from January 1, 2003 to May 31, 2018. Our search was performed on June 24, 2018. The first published trial report evaluating the effect of CXL in patients with keratoconus was published in 20034; therefore, the year 2003 was used as the starting point for the literature search. The keywords in our search strategy include corneal crosslinking, corneal collagen crosslinking, collagen crosslinkage, and corneal ectasia. Two reviewers (H.K., S.S.R.) reviewed the titles and abstracts of the search results and retrieved full-text articles if the title or abstract seemed to meet the eligibility criteria for this review.
Inclusion and Exclusion Criteria
Studies were included if they discussed the diagnosis of progressive corneal ectasia disorder such as keratoconus, pellucid marginal degeneration, or postrefractive surgery ectasia.21 The progression of corneal ectasia was defined as an increase of at least 1 diopter (D) in the steepest keratometry (K), a degradation of visual acuity, and an increase of 1 D or more in the manifest cylinder over the preceding 12 months. Studies that had a 1-year minimum follow-up and followed the transepithelial or epi-off technique were included. When the same trial was drawn by a screening, the most recent trial report was used. Only studies including human research participants and published in the English language were included. Animal and ex vivo studies were excluded. Studies in which CXL was performed in combination with other surgical procedures such as intracorneal segment insertion, excimer laser procedures, or iontophoresis techniques were also excluded. This metaanalysis limited selection to RCTs. To confirm the reliability, non-RCTs such as cohort studies, case-control studies, and studies that did not use a random method to prospectively assign participants to 2 groups, were individually analyzed. All articles were carefully reviewed to select those that reported original clinical data preoperatively and postoperatively. Data from previously reported cases included in different articles were omitted to avoid duplication of data.
Risk For Bias Assessment
Two review authors (H.K., S.S.R.) independently assessed the risk for bias of the included studies in accordance with the Cochrane Handbook for Systematic Reviews of Interventions22 using the following parameters: adequacy of sequence generation; allocation concealment; blinding of participants, personnel, and outcome assessors; incomplete outcome data; and selective outcome reporting.
Outcome Measures
Effective outcomes were the changes in the following parameters between the baseline and 1-year follow-up:
Maximum keratometry value: the steepest K value obtained using topographies of a rotating Scheimpflug camera or computerized videokeratography;
Central corneal thickness (CCT): the thickness of the central point using ultrasound pachymetry;
Best spectacle-corrected visual acuity (BSCVA): the visual acuity corrected by only spectacles;
Uncorrected distance visual acuity (UDVA): the visual acuity without correction;
Manifest refraction spherical equivalent (MRSE): the manifest subjective refraction of the SE;
Cylindrical refraction: the manifest subjective refraction of the cylinder.
Corrected distance visual acuity with a contact lens was not included in this analysis because the evaluation of visual acuity was limited to BSCVA or UDVA in most previous trials.
Safety outcomes were endothelial cell density 12 months postoperatively and the number of eyes demarcation line 1 month after CXL. The number of eyes postoperatively got into the adverse events such as infectious keratitis or conjunctivitis, sterile infiltrate though a clear cornea, and delayed epithelial healing was assessed but not statistically analyzed.
Data Extraction
Two reviewers (H.K., S.S.R.) independently extracted data from the included trials using a standardized form. The aforementioned outcome measures and details of the interventions, such as setting, sample size, age, mean baseline maximum K, riboflavin solutions, and follow-up period were collected. The unpublished data was requested from the corresponding authors of the individual trials via email and their replies were awaited on for 3 months.
Heterogeneity Assessment
Assessment of heterogeneity was planned by reviewing the clinical and methodological diversity of the included studies and by examining the forest plots and I-square heterogeneity (I2) statistics as described in the Cochrane Handbook for Systematic Reviews of Interventions.22
Statistical Analysis
Treatment effects were evaluated as the weighted mean difference (WMD) and 95% confidence interval (CI) calculated for absolute changes of the interested outcomes. For individual articles, the WMD was computed by the difference of the mean change in the transepithelial CXL group and that in the epi-off group. The outcomes were measured as means ± SD. For the demarcation line, the data in each study were tabulated into 2 × 2 tables and the odds ratio (OR) and 95% CIs of the results between the 2 techniques were compared. Heterogeneity was also assessed, and an I2 value greater than 50% was considered significant. In this instance, a random-effects model was used because it provides a conservative estimate and is less influenced by the weighting of each study than other methods.23 A fixed model was used when the level of heterogeneity was less than 50%. The metaanalysis was performed using RevMan software (version 5.2, Information Management Systems Group, Cochrane Collaboration). A P value less than 0.05 was considered statistically significant using a 2-sided test.
RESULTS
Results of the Search
There were 1552 articles relevant to the search terms. After screening titles and abstracts, 1541 studies were excluded. Eleven articles13–19,24–27 were initially considered potentially relevant; however, 4 of these were excluded because 3 articles were non-RCT trials and one was a short-term follow-up (Figure 1, and Supplement 2, available at http://jcrsjournal.org). Finally, the remaining seven RCTs involving 505 eyes were included in this metaanalysis.13–19 The unpublished information was obtained from the RCTs by Stojanovic et al.,13 Rossi et al.,14 and Soeters et al.15 No unpublished data was received for Al Fayez et al.16 and Rush and Rush,17 despite inquiries. The article by Al Fayez et al.16 did not show any outcome measures because of the lack of each variable.
Figure 1.
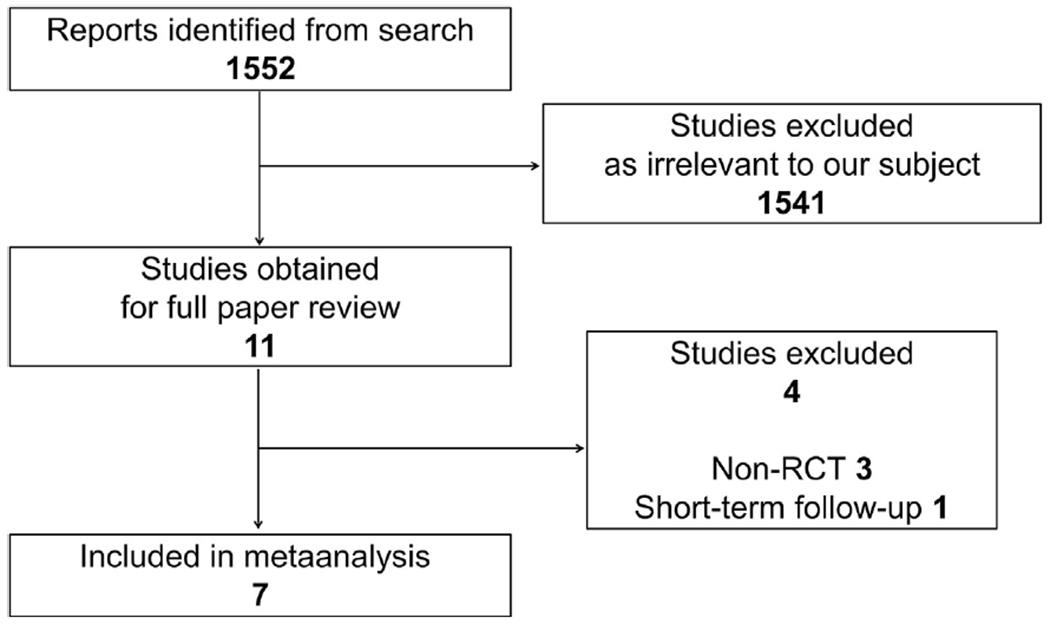
Flow of trial selection (RCT = randomized controlled trial).
Characteristics of the Included Studies
Table 1 shows the main characteristics of the 7 included trials. Seven studies that reported on 272 eyes in the transepithelial CXL group and 233 eyes in the epi-off CXL group provided data for this metaanalysis. Six studies included only keratoconic patients; however, 22% of patients were diagnosed as pellucid marginal degeneration and postcorneal refractive surgery ectasia in a trial by Rush and Rush.17 Table 2 shows the summary of riboflavin profiles of transepithelial CXL and epi-off CXL protocols in the 7 included trials.
Table 1.
Characteristics of 5 randomized controlled trials evaluating transepithelial CXL versus epi-off CXL.
| Study* (Y) | ClinicalTrials.gov | Country | Follow-Up (Mo) | Treated Eyes (N) | Mean Age (Y) | Mean Baseline Kmax (D) | |||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Transepithelial CXL | Epi-Off CXL | Transepithelial CXL | Epi-Off CXL | Transepithelial CXL | Epi-Off CXL | ||||
|
| |||||||||
| Al Fayez16 (2015) | Not registered | Saudi Arabia | 36 | 34 | 36 | 24.8 | 24.1 | N/A | N/A |
| Bikbova18 (2016) | NCT02456961 | Russia | 24 | 76 | 73 | 28.0 | 30.0 | 48.28 | 48.83 |
| Lombardo19 (2017) | NCT02117999 | Italy | 12 | 22 | 12 | 31.0 | 29.4 | 54.7 | 54.7 |
| Rossi14 (2015) | Not registered | Italy | 12 | 10 | 10 | 28.0 | 30.4 | 52.41 | 51.64 |
| Rush17 (2017) | NCT01708538 | United States | 24 | 75 | 56 | 29.8 | 31.5 | 51.34 | 52.03 |
| Soeters15 (2015) | NCT02349165 | Netherlands | 12 | 35 | 26 | 26.91 | 25.85 | 56.4 | 57.8 |
| Stojanovic13 (2014) | NCT01181219 | Norway | 12 | 20 | 20 | 29.45 | 29.45 | 52.68 | 53.59 |
CXL = corneal crosslinking; epi-off = epithelium-off; Kmax = maximum keratometry; N/A = Not available
First author
Table 2.
Summary of riboflavin profiles of CXL protocols.
| Study* (Y) | Transepithelial CXL | Epi-Off CXL | ||
|---|---|---|---|---|
|
| ||||
| Concentration | Impregnation | Concentration | Impregnation | |
|
| ||||
| Al Fayez16 (2015) | 0.1% riboflavin with 20% dextran and 0.02% BAC | Every 3 min for 30 min, then every 3 min during UVA | 0.1% riboflavin with 20% dextran | Every 3 min for 30 min, then every 3 min during UVA |
| Bikbova18 (2016) | Hypotonic 0.1% riboflavin without dextran using an iontophoresis device | Iontophoresis for 10 min, then no riboflavin drop during UVA | 0.1% riboflavin with dextran | Every 2 min for 30 min, then every 2 min during UVA |
| Lombardo19 (2017) | 0.1% riboflavin without dextran using an iontophoresis device | Iontophoresis, then every 2 min during UVA | 0.1% riboflavin with 20% dextran | Every 3 min for 30 min, then every 3 min during UVA |
| Rossi14 (2015) | 0.1% riboflavin with 15% dextran, tris, and EDTA | Every 2 min for 30 min, then every 5 min during UVA | 0.1% riboflavin with 20% dextran | Every 2 min for 30 min, then every 2 min during UVA |
| Rush17 (2017) | 0.25% riboflavin with 1.2% HPMC and 0.01% BAC | Every 2 min for 30 min, then every 2 min during UVA | 0.1% riboflavin with 20% dextran | Every 2 min for 30 min, then every 2 min during UVA |
| Soeters15 (2015) | 0.1% riboflavin with 15% dextran, tris, and EDTA | Every 2 min for 15 min, then every 5 min during UVA | 0.1% riboflavin with 20% dextran | Every 3 min for 30 min, then every 5 min during UVA |
| Stojanovic13 (2014) | Hypotonic 0.5% riboflavin with 0.005% BAC | Every 5 min for 15 min, then stop during UVA | Hypotonic 0.5% riboflavin | Every 5 min for 15 min, then stop during UVA |
BAC = benzalkonium chloride; CXL = corneal crosslinking; EDTA = ethylenediaminetetraacetic acid; epi-off = epithelium off; HPMC = hydroxypropyl methylcellulose; tris = tris(hydroxymethyl)nitromethane; UVA = ultraviolet-A
First author
Quality of the Evidence
Table 3 shows the risks for bias in the included studies. No disagreements were observed between the 2 reviewers. In terms of risk for bias, although all 7 trials were at a low risk for bias for allocation concealment, they were at high risk for bias for masking study participants and personnel. Masking of the investigators collecting the postoperative data was unclear in all trials.
Table 3.
Risk for bias in included studies.
| Study* (Y) | Random Sequence Generation (Selection Bias) | Allocation Concealment (Selection Bias) | Masked Participants and Personnel (Performance Bias) | Masked Outcome Assessment (Detection Bias) | Incomplete Outcome Data (Attrition Bias) | Selective Reporting (Reporting Bias) |
|---|---|---|---|---|---|---|
|
| ||||||
| Al Fayez16 (2015) | Unclear | Low | High | Unclear | Low | Unclear |
| Bikbova18 (2016) | Unclear | Low | High | Unclear | Low | Unclear |
| Lombardo19 (2017) | Unclear | Low | High | Unclear | Low | Unclear |
| Rossi14 (2015) | Unclear | Low | High | Unclear | Low | Unclear |
| Rush17 (2017) | Low | Low | High | Unclear | Low | Low |
| Soeters15 (2015) | Low | Low | High | Unclear | Low | Low |
| Stojanovic13 (2014) | Unclear | Low | High | Unclear | Low | Unclear |
First author
Topographic Results
The maximum K data were reported by 6 of the 7 studies that qualified for inclusion in this study. The maximum K data forest plots showed a significant difference in the change after 1-year follow-up between the 2 groups (WMD, 1.10; 95% CI, 0.97 to 1.22; P < .00001) (Figure 2). No significant heterogeneity was found (P = .10, I2 = 46%). The CCT data were reported by 4 of the 7 studies that qualified for inclusion in this study. The CCT forest plots showed a significant difference in the change after a 1-year follow-up between the 2 groups (WMD, 5.19; 95% CI, 0.79 to 9.59; P = .02) (Figure 3). Heterogeneity was not shown (P = .83, I2 = 0%).
Figure 2.
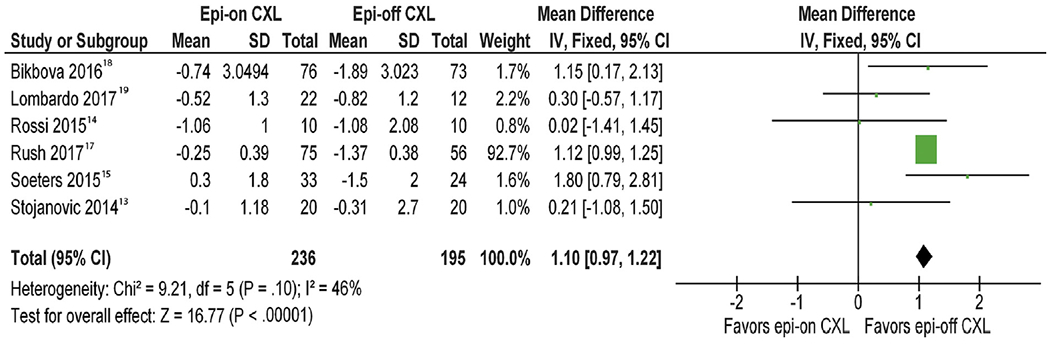
Forest plot comparing change in maximum K of epi-on and epi-off CXL after 1-year follow-up (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; IV = inverse variance; I2 = I-square heterogeneity statistic; Z = Z statistic).
Figure 3.
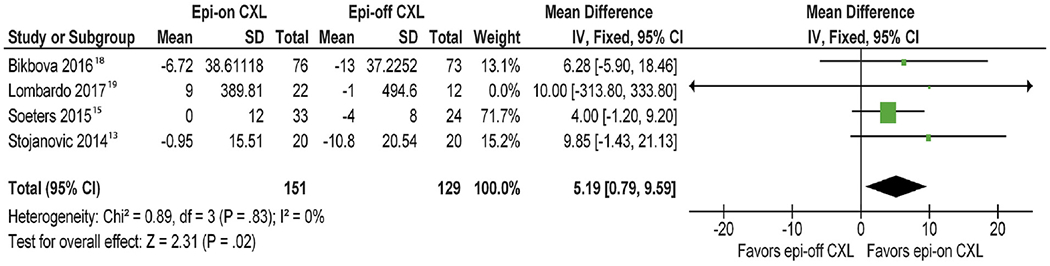
Forest plot comparing change in central corneal thickness of epi-on and epi-off CXL after 1-year follow-up (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; IV = inverse variance; I2 = I-square heterogeneity statistic; Z = Z statistic).
Visual Acuity and Refractive Outcomes
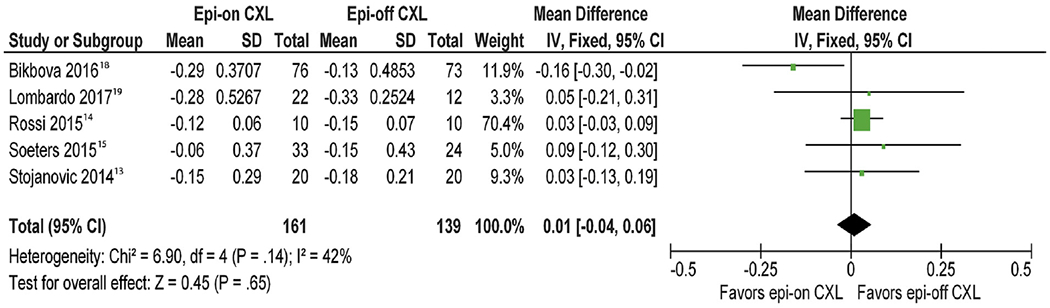
The BSCVA were reported by 6 of 7 studies that qualified for inclusion in this study. Treated eyes in transepithelial CXL group significantly improved in BSCVA in comparison to the epi-off CXL group after a 1-year follow-up (WMD, −0.05; 95% CI, −0.08 to −0.02; P = .002) (Figure 4). Heterogeneity was observed (P = .003, I2 = 57%). The UDVAs were reported by 5 of the 7 studies that qualified for inclusion in this study. The change in UDVA was not significantly different between the 2 groups after 1-year follow-up (WMD, 0.01; 95% CI, −0.04 to 0.06; P = .65) (Figure 5). No statistically significant heterogeneity between studies was identified (P = .14, I2 = 42%). The SE and cylindrical refraction data were reported by 4 of the 7 studies and 2 of the 7 studies that qualified for inclusion in this study, respectively. The change in the MRSE did not differ significantly between the 2 groups after a 1-year follow-up (WMD, −0.04; 95% CI, −0.43 to 0.34; P = .82) (Figure 6). The similar outcomes were obtained in the change in the cylindrical refraction (WMD, −0.18; 95% CI, −0.90 to 0.54; P = .63) (Figure 7). The test suggested no heterogeneity in the 2 outcomes (P = .97, I2 = 0% and P = .93, I2 = 0%, respectively).
Figure 4.
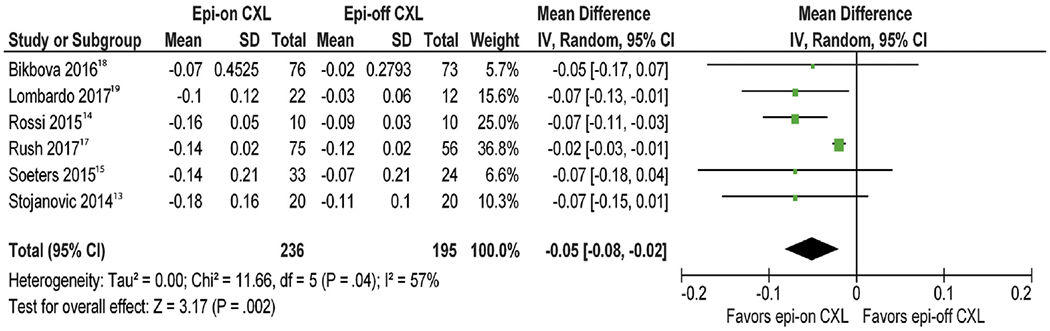
Forest plot comparing change in best spectacle-corrected visual acuity of epi-on and epi-off CXL after 1-year follow-up (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; IV = inverse variance; I2 = I-square heterogeneity statistic; Tau2 = tau-square statistic; Z = Z statistic).
Figure 5.
Forest plot comparing change in uncorrected distance visual acuity of epi-on and epi-off CXL after 1-year follow-up (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; IV = inverse variance; I2 = I-square heterogeneity statistic; Z = Z statistic).
Figure 6.
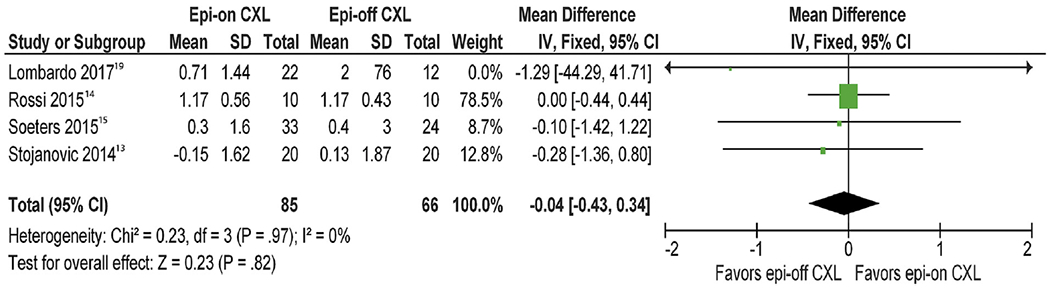
Forest plot comparing change in spherical equivalent refraction of epi-on and epi-off CXL after 1-year follow-up (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; IV = inverse variance; I2 = I-square heterogeneity statistic; Z = Z statistic).
Figure 7.
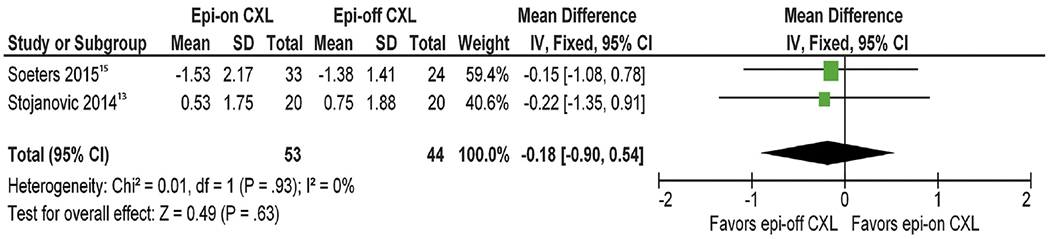
Forest plot comparing change in cylindrical refraction of epi-on and epi-off CXL after 1-year follow-up (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; IV = inverse variance; I2 = I-square heterogeneity statistic; Z = Z statistic).
Safety Outcomes
The endothelial cell density was reported by 5 of 7 studies that qualified for inclusion in this study. No significant differences of endothelial cell density between groups were found at 1 year during follow-up (WMD, −15.82; 95% CI, −40.63 to 8.98; P = .21) (Figure 8). No statistically significant heterogeneity between studies was identified (P = .21, I2 = 40%). A metaanalysis in relation to the demarcation line was performed for 2 of the 7 studies. Forest plots showed that the incidence of demarcation line in patients who had epi-off CXL was significantly more frequent than that in those who had transepithelial CXL (OR, 0.01; 95% CI, 0.00 to 0.18; P = .0009) (Figure 9). The adverse events data were reported by 6 of 7 studies that qualified for inclusion in this study. Table 4 shows the adverse events in the included studies.
Figure 8.
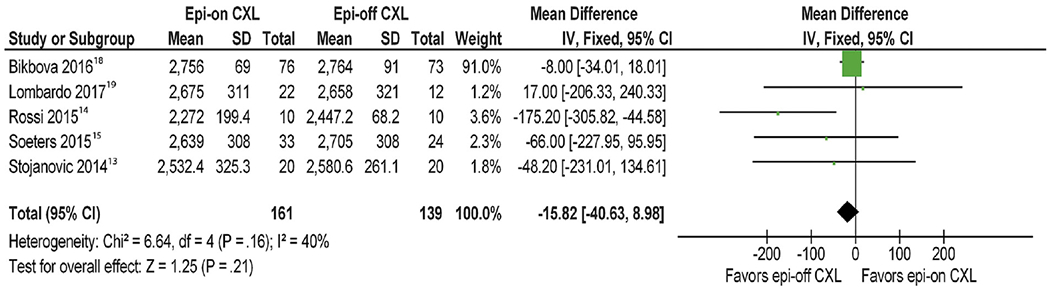
Forest plot comparing endothelial cell density of epi-on and epi-off CXL after 1-year follow-up (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; IV = inverse variance; I2 = I-square heterogeneity statistic; Z = Z statistic).
Figure 9.
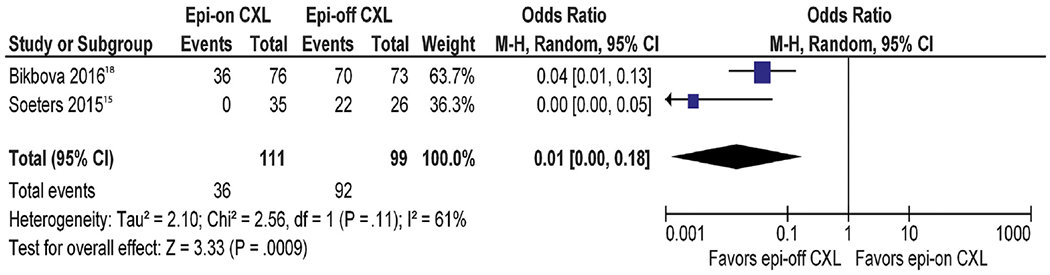
Forest plot comparing the incidence of demarcation line of epi-on and epi-off CXL after 1-month follow-up (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; I2 = I-square heterogeneity statistic; M-H = Mantel-Haenszel; Tau2 = tau-square statistic; Z = Z statistic)
Table 4.
Summary of adverse events of transepithelial CXL and epi-off CXL after 1-year follow-up.
| Study* (Y) | Adverse Events (N) |
Case Presentation | |
|---|---|---|---|
| Transepithelial CXL | Epi-Off CXL | ||
|
| |||
| Bikbova18 (2016) | 0 | 4 | Four eyes developed a permanent haze during 24 months. |
| Lombardo19 (2017) | 2 | 6 | Two eyes and 6 eyes developed stromal edema in transepithelial CXL and epi-off CXL groups, respectively, at both 3 and 7 days postoperatively. |
| Lombardo19 (2017) | 0 | 4 | Mild edema of the most posterior stroma was still found in 4 eyes at 3-month follow-up. |
| Rossi14 (2015) | 0 | 0 | Not reported |
| Rush17 (2017) | 0 | 2 | One eye developed a bacterial conjunctivitis at 1-week follow-up. One eye had delayed epithelial healing at 2-week follow-up. |
| Soeters15 (2015) | 0 | 4 | One eye developed a herpes simplex keratitis at 1-week follow-up. One eye developed a sterile infiltrate at 1-month follow-up. Two eyes had delayed epithelial healing at 1- and 3-week follow-up. |
| Stojanovic13 (2014) | 0 | 0 | Not reported |
CXL = corneal crosslinking; epi-off = epithelium-off
First author
Non-RCT Analysis
Three non-RCTs involving 136 eyes were individually analyzed.24–26 Data were obtained on maximum K, CCT, BSCVA, UDVA, and cylindrical refraction. As shown in the statistical results in Figure 10, there was a significant reduction in maximum K in epi-off CXL at 1 year after surgery compared with transepithelial CXL (WMD, 1.54; 95% CI, 0.39 to 2.68; P = .008). There was a significant deference in CCT between the 2 groups (WMD, 28.76; 95% CI, 4.21 to 53.31; P = .02). As for BSCVA, UDVA, and cylindrical refraction, no statistical significant differences existed.
Figure 10.
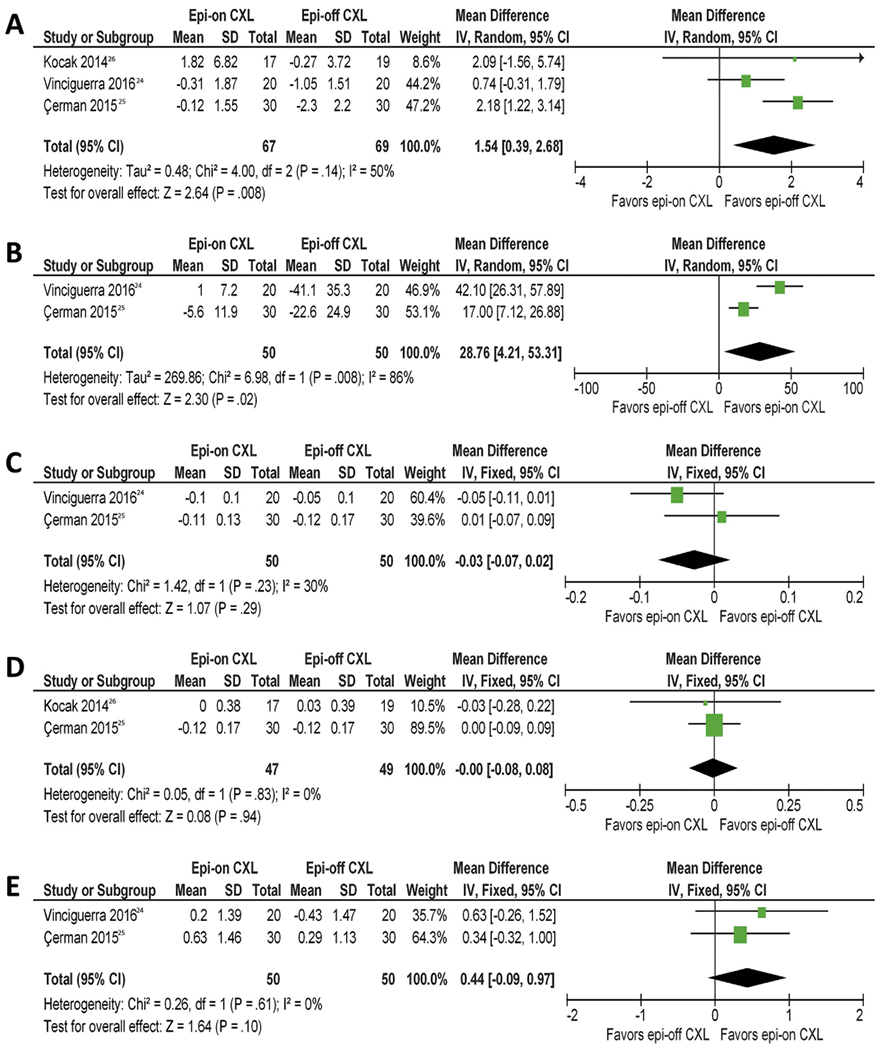
Forest plots comparing change in clinical parameters of epi-on and epi-off CXL after 1-year follow-up in nonrandomized controlled trial. A: Maximum keratometry. B: Central corneal thickness. C: Best spectacle-corrected visual acuity. D: Uncorrected distance visual acuity. E: Cylindrical refraction (Chi2 = chi-square statistic; CI = confidence interval; CXL = corneal crosslinking; df = degrees of freedom; epi-off = epithelium-off; epi-on = epithelium-on; IV = inverse variance; I2 = I-square heterogeneity statistic; Z = Z statistic).
DISCUSSION
In this metaanalysis, we observed changes in topographic, visual, and refractive outcomes after transepithelial CXL and compared these same outcome measures with those in a group of patients who had epi-off CXL treatment in progressive corneal ectasia. This metaanalysis provides evidence that transepithelial CXL had less impact on halting progressive corneal ectasia, in terms of maximum K, than epi-off CXL. Over the 1-year observation period, significant statistical heterogeneity across the 6 studies was noted in BSCVA measurement across the studies with transepithelial CXL, resulting in a greater improvement in BSCVA than epi-off CXL; however, the difference was less than a line on an eye chart and has unclear clinical significance. Li and Wang28 reported on a metaanalysis based on RCTs to compare the efficacy and safety of transepithelial CXL versus epi-off CXL on progressive keratoconus. However, their metaanalysis included only 3 RCTs, making for less evidence and smaller sample sizes. In the present metaanalysis of RCTs, we included 7 studies that had sufficient evidence, although Al Fayez et al.16 did not show outcome measures.
The maximum K data were reported by 6 of the 7 studies that qualified for inclusion in our study. Maximum K is arguably the most popular parameter when considering corneal ectasia progression, although it is not very reproducible. The epi-off CXL group demonstrated a greater change in maximum K when compared with the transepithelial CXL group at 12 months of follow-up in the current metaanalysis. The study by Rush and Rush17 yields 92.7% of the weight in the metaanalysis because of its larger sample size and smaller standard deviation than the other studies. This high weight might be attributed to the differences in the proportion of keratoconic patients because 22% of patients in the Rush and Rush study17 had diagnoses other than keratoconus. The mean difference in maximum K was −1.11 D between the 2 techniques. Similar findings were reported in a previous systematic review assessing the efficacy and safety of transepithelial CXL for the treatment of keratoconus.12 Using the published data from the systematic review article,12 the mean change in maximum K for the 45 articles using an epi-off technique was −1.21 ± 1.29 D. For the 6 articles using a transepithelial technique, they also calculated that the mean change in maximum K was 0.33 ± 1.18 D. In the current study, we observed evidence of no significant statistical heterogeneity as indicated by an I2 of 46%. In terms of maximum K, transepithelial CXL showed a poor potential for halting corneal ectasia progression when compared with regular epi-off CXL.
The demarcation line is useful to ascertain the CXL treatment depth. Two studies included in our metaanalysis15,18 reported that at 1 month postoperatively, the demarcation line after epi-off CXL was more remarkable than after transepithelial CXL. The greater efficacy of epi-off than transepithelial CXL might be associated with the deeper demarcation line observed after treatment.29
Central corneal thickness data were also reported by 4 of the 7 studies that qualified for inclusion in our study. This metaanalysis showed that at the postoperative 12-month visit, the decrease in CCT in the epi-off CXL group was significantly greater than that in the transepithelial CXL group. It is not clear whether this change is clinically meaningful because the WMD (5.19 μm) was small and is within typical test–retest variability.
Data on BSCVA were also reported by 6 of the 7 studies that qualified for inclusion in our study. There was a statistically significant different trend in BSCVA between the transepithelial CXL group and the epi-off CXL group at the 12-month follow-up, with a more favorable outcome in the transepithelial CXL group. Because the WMD (−0.05) is less than 1 line on an eye chart, it is unknown whether this statistically significant difference has an impact on clinical decision-making in the treatment of corneal ectasia. The statistically different trend in BSCVA between the groups might be explained by the higher risk for haze formation in the epi-off group, which was noted after epithelium removal.30 The BSCVA and maximum K readings had opposite outcomes in this metaanalysis in the comparison between the 2 groups. We believe that corneal higher-order aberrations could be useful for the understanding the efficacy of CXL, although each study did not show the change in higher-order aberrations after surgery. Based on the published data from the systematic review,12 the mean changes in BSCVA in the previous studies were −0.08 ± 0.04 and −0.08 ± 0.07 logarithm of the minimum angle of resolution in the transepithelial and epi-off techniques, respectively. We observed evidence of significant statistical heterogeneity between the 4 studies in BSCVA as indicated by an I2 of 57%. We assume that the heterogeneity might be attributable to the differences in patients’ baseline characteristics, such as the mean baseline maximum K.
As for UDVA, SE, and cylindrical refraction, our study showed no significant differences between the transepithelial CXL and epi-off CXL groups at 1-year after surgery. The change in these parameters in the transepithelial CXL group was equivalent to that in the epi-off CXL group. We observed no significant statistical heterogeneity because an I2 in each parameter was less than 50%.
Adverse events data were also reported by 6 of the 7 studies that qualified for inclusion in our study. Our study demonstrated that postoperative complications such as infection, sterile infiltrate, and delayed epithelial healing were reported more frequently with epi-off CXL techniques. However, the postoperative complication rate varied for the 2 RCTs (4% to 15%),15,17 suggesting that a much larger number of study participants would be required to effectively compare the rate of postoperative complications between CXL techniques.
With regard to CXL procedures, we confirmed various concentrations and impregnations of riboflavin in each trial. The heterogeneity between the included trials might be attributed to the discrepancy in surgical protocols as shown in Table 2. The riboflavin solution used in the transepithelial CXL was formulated with benzalkonium chloride 0.005 to 0.02% in the included RCTs. Benzalkonium chloride has been reported to enhance ocular surface penetration by increasing epithelial permeability and bioavailability of topical medication to the corneal stroma.31 However, based on our maximum K outcome, we believe that the ocular surface penetration of riboflavin into the corneal stroma in the transepithelial group was inferior to the epi-off group. The corneal epithelium is itself the critical obstacle to riboflavin permeation into the corneal stroma, and it affects CXL’s effect significantly because a complete and intact epithelial layer is a tough lipophilic barrier to hydrosoluble riboflavin.32 Franch et al.33 found that through an enhancer used in the riboflavin solution, the concentration of riboflavin in an epithelium-on cornea was much lower than in an epi-off cornea in vivo. This can explain, to a large extent, why transepithelial CXL was significantly inferior to epi-off CXL at halting progression of the maximum K value.
We found that the methodology of the transepithelial CXL protocol varied between the included studies. Most studies performed the transepithelial treatment only as the standard treatment without epithelium debridement, with a UVA exposure for 30 minutes, at an irradiance of 3 mW/cm2.13–17 Bikbova and Bikbov18 performed riboflavin soaking using an iontophoresis device to induce absorption. An iontophoresis device was also applied in the study by Lombardo et al.,19 whereas the UVA irradiation was enhanced to shorten the exposure time. However, the total energy density was equal among all studies in the transepithelial CXL. Studies conducted by Stojanovic et al.,13 Rossi et al.,14 Soeters et al.,15 Al Fayez et al.,16 Rush and Rush,17 and Bikbova and Bikbov18 used a 3 mW/cm2 irradiation device for 30 minutes, whereas the study conducted by Lombardo et al.19 used 10 mW/cm2 irradiation for 9 minutes. As for epi-off CXL, each study used the same protocol with 3 mW/cm2 for 30 minutes.13–19 Therefore, the total irradiation dose was approximately 5.4 J/cm2, in transepithelial and epi-off procedures. In the study by Schumacher et al.,34 the effect of crosslinking was related to the total energy, and rapid CXL treatment was regarded as equivalent to the standard procedure. Therefore, we believe that although the procedure parameters used were different, the intensity of the crosslinking effect on the cornea is similar.
Similar results were obtained using data from non-RCTs when we compared the changes in topographic, visual acuity, and cylindrical refraction between transepithelial CXL and epi-off CXL. It has been suggested that transepithelial CXL is less efficient at flattening the maximum K value compared with epi-off CXL, even in a metaanalysis of non-RCTs. However, we assume that quantitative evaluation should be based on RCTs to avoid potential confounding bias.
This metaanalysis has at least 2 limitations that should be taken into account when its results are considered. First, the small number of cases per trial and the total number of cases in this metaanalysis give these analyses low power. It is unknown whether 7 RCTs were adequate for comparing the 2 techniques. Nevertheless, our study provides more powerful evidence than the individual reports alone, and we are unaware of any other similar systematic reviews. It has been reported that heterogeneity between small studies is larger than between larger studies in metaanalyses.35 A further study with greater numbers of RCTs is required to confirm our findings. Second, we could only include data from published articles, and bias could be introduced if studies with small or different effects exist but have not been published.
In summary, epi-off CXL resulted in better maximum K measurements and more frequently induced adverse events compared with the transepithelial CXL technique. Although transepithelial CXL showed superiority over epi-off CXL by exhibiting a better corrected distance visual acuity after 1-year of follow-up, the difference might not be clinically significant. Based on these findings, we recommend that epi-off CXL remains as the standard of care for the treatment of progressive corneal ectasia.
Supplementary Material
WHAT WAS KNOWN
It is unknown whether any method of transepithelial CXL is as effective in treating progressive corneal ectasia as the standard epi-off technique.
WHAT THIS PAPER ADDS
This metaanalysis of randomized controlled trials showed that epi-off CXL might be better than the transepithelial technique for the treatment of progressive corneal ectasia in terms of steepest keratometry.
Footnotes
Presented as a poster at the annual meeting of the American Society of Cataract and Refractive Surgery, Los Angeles, California, USA, May 2017.
Supplemental material available at www.jcrsjournal.org.
Disclosures: None of the authors has a financial or proprietary interest in any material or method mentioned.
REFERENCES
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol 1998; 42:297–319 [DOI] [PubMed] [Google Scholar]
- 2.Javadi MA, Motlagh BF, Jafarinasab MR, Rabbanikhah Z, Anissian A, Souri H, Yazdani S. Outcomes of penetrating keratoplasty in keratoconus. Cornea 2005; 24:941–946 [DOI] [PubMed] [Google Scholar]
- 3.Reeves SW, Stinnett S, Adelman RA, Afshari NA. Risk factors for progression to penetrating keratoplasty in patients with keratoconus. Am J Ophthalmol 2005; 140:607–611 [DOI] [PubMed] [Google Scholar]
- 4.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 2003; 135:620–627 [DOI] [PubMed] [Google Scholar]
- 5.Wollensak G, Spoerl E, Seiler T. Stress-strain measurements of human and porcine corneas after riboflavin-ultraviolet-A-induced cross-linking. J Cataract Refract Surg 2003; 29:1780–1785 [DOI] [PubMed] [Google Scholar]
- 6.Hovakimyan M, Guthoff RF, Stachs O. Collagen cross-linking: Current status and future directions. J Ophthalmol 2012; 2012:406850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spoerl E, Hoyer A, Pillunat LE, Raiskup F. Corneal cross-linking and safety issues. Open Ophthalmol J 2011; 5:14–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhawan S, Rao K, Natrajan S. Complications of corneal collagen cross-linking. J Ophthalmol 2011; 2011:869015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kymionis GD, Portaliou DM, Bouzoukis DI, Suh LH, Pallikaris AI, Markomanolakis M, Yoo SH. Herpetic keratitis with iritis after corneal cross-linking with riboflavin and ultraviolet A for keratoconus. J Cataract Refract Surg 2007; 33:1982–1984 [DOI] [PubMed] [Google Scholar]
- 10.Wollensak G, Iomdina E. Biomechanical and histological changes after corneal crosslinking with and without epithelial debridement. J Cataract Refract Surg 2009; 35:540–546 [DOI] [PubMed] [Google Scholar]
- 11.Pinelli R. BAK: a better alternative to epithelium removal in crosslinking. Ophthalmol Times Europe 2006; 2:36–38 [Google Scholar]
- 12.Shalchi Z, Wang X, Nanavaty MA. Safety and efficacy of epithelium removal and transepithelial corneal collagen crosslinking for keratoconus. Eye (Lond) 2015; 29:15–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stojanovic A, Zhou W, Utheim TP. Corneal collagen cross-linking with and without epithelial removal: a contralateral study with 0.5% hypotonic riboflavin solution. Biomed Res Int 2014; 2014:619398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rossi S, Orrico A, Santamaria C, Romano V, De Rosa L, Simonelli F, De Rosa G. Standard versus trans-epithelial collagen cross-linking in keratoconus patients suitable for standard collagen cross-linking. Clin Ophthalmol 2015; 9:503–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soeters N, Wisse RP, Godefrooij DA, Imhof SM, Tahzib NG. Transepithelial versus epithelium-off corneal cross-linking for the treatment of progressive keratoconus: a randomized controlled trial. Am J Ophthalmol 2015; 159:821–828.e3 [DOI] [PubMed] [Google Scholar]
- 16.Al Fayez MF, Alfayez S, Alfayez Y. Transepithelial versus epithelium-off corneal collagen cross-linking for progressive keratoconus: a prospective randomized controlled trial. Cornea 2015; 34 Suppl 10:S53–S66 [DOI] [PubMed] [Google Scholar]
- 17.Rush SW, Rush RB. Epithelium-off versus transepithelial corneal collagen crosslinking for progressive corneal ectasia: a randomised and controlled trial. Br J Ophthalmol 2017; 101:503–508 [DOI] [PubMed] [Google Scholar]
- 18.Bikbova G, Bikbov M. Standard corneal collagen crosslinking versus transepithelial iontophoresis-assisted corneal crosslinking, 24 months follow-up: randomized control trial. Acta Ophthalmol 2016; 94:e600–e606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lombardo M, Giannini D, Lombardo G, Serrao S. Randomized controlled trial comparing transepithelial corneal cross-linking using iontophoresis with the dresden protocol in progressive keratoconus. Ophthalmology 2017; 124:804–812 [DOI] [PubMed] [Google Scholar]
- 20.Liberati A, Altman DG, Tetzlaff J, Mulrow C, GØtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 2009; 151:W65–W94 [DOI] [PubMed] [Google Scholar]
- 21.Alió JL, Shabayek MH, Artola A. Intracorneal ring segments for keratoconus correction: long-term follow-up. J Cataract Refract Surg 2006; 32:978–985 [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT. Green S, eds, Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. The Cochrane Collaboration, 2011. Available at: http://handbook.cochrane.org/. Accessed August 30, 2018 [Google Scholar]
- 23.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vinciguerra P, Romano V, Rosetta P, Legrottaglie EF, Piscopo R, Fabiani C, Azzolini C, Vinciguerra R. Transepithelial iontophoresis versus standard corneal collagen cross-linking: 1-year results of a prospective clinical study. J Refract Surg 2016; 32:672–678 [DOI] [PubMed] [Google Scholar]
- 25.Çerman E, Toker E, Ozarslan Ozcan D. Transepithelial versus epithelium-off crosslinking in adults with progressive keratoconus. J Cataract Refract Surg 2015; 41:1416–1425 [DOI] [PubMed] [Google Scholar]
- 26.Kocak I, Aydin A, Kaya F, Koc H. Comparison of transepithelial corneal collagen crosslinking with epithelium-off crosslinking in progressive keratoconus. J Fr Ophtalmol 2014; 37:371–376 [DOI] [PubMed] [Google Scholar]
- 27.Nawaz S, Gupta S, Gogia V, Sasikala NK, Panda A. Trans-epithelial versus conventional corneal collagen crosslinking: A randomized trial in keratoconus. Oman J Ophthalmol 2015; 8:9–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li W, Wang B. Efficacy and safety of transepithelial corneal collagen crosslinking surgery versus standard corneal collagen crosslinking surgery for keratoconus: a meta-analysis of randomized controlled trials. BMC Ophthalmol 2017; 17:262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Filippello M, Stagni E, O’Brart D. Transepithelial corneal collagen crosslinking: bilateral study. J Cataract Refract Surg 2012; 38:283–291 [DOI] [PubMed] [Google Scholar]
- 30.Greenstein SA, Fry KL, Bhatt J, Hersh PS. Natural history of corneal haze after collagen crosslinking for keratoconus and corneal ectasia: Scheimpflug and biomicroscopic analysis. J Cataract Refract Surg 2010; 36:2105–2114 [DOI] [PubMed] [Google Scholar]
- 31.Mahaling B, Katti DS. Understanding the influence of surface properties of nanoparticles and penetration enhancers for improving bioavailability in eye tissues in vivo. Int J Pharm 2016; 501:1–9 [DOI] [PubMed] [Google Scholar]
- 32.Spoerl E, Mrochen M, Sliney D, Trokel S, Seiler T. Safety of UVA-riboflavin cross-linking of the cornea. Cornea 2007; 26:385–389 [DOI] [PubMed] [Google Scholar]
- 33.Franch A, Birattari F, Dal Mas G, Lužnik Z, Parekh M, Ferrari S, Ponzin D. Evaluation of Intrastromal Riboflavin Concentration in Human Corneas after Three Corneal Cross-Linking Imbibition Procedures: A Pilot Study. J Ophthalmol 2015; 2015:794256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schumacher S, Oeftiger L, Mrochen M. Equivalence of biomechanical changes induced by rapid and standard corneal cross-linking, using riboflavin and ultraviolet radiation. Invest Ophthalmol Vis Sci 2011; 52:9048–9052 [DOI] [PubMed] [Google Scholar]
- 35.IntHout J, Ioannidis JP, Borm GF, Goeman JJ. Small studies are more heterogeneous than large ones: a meta-meta-analysis. J Clin Epidemiol 2015; 68:860–869 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


