Abstract
Purpose
This study investigated the associations between some factors related to working from home status (WFHS) and positive/negative experiences due to social distancing and their interactions effects on depressive symptoms during the COVID-19 pandemic.
Methods
A random population-based telephone survey interviewed income-earning adults in the Hong Kong general population during April 21–28, 2020 (n = 200).
Results
Mild to severe depression (according to PHQ-9) was reported by 12% of the participants. The prevalence of WFHS categories was 14% for 3–7 days and 13% for ≥ 8 days (past 2 weeks). The multivariable regression analysis showed that, social isolation (β = 0.36; p < 0.001), relaxation feeling in daily life (β = − 0.22; p = 0.002), and WFHS ≥ 8 days (β = 0.15; p = 0.027), but not perceived huge inconvenience and improved family relationship, were associated with depressive symptoms. Statistically significant interaction effects were found. Some positive experiences buffered the potential harms of some negative experiences of social distancing on depressive symptoms; WFHS ≥ 8 days significantly moderated the risk/protective effects of social isolation, improved family relationship, and relaxation feeling on depressive symptoms.
Conclusions
Social distancing is double-edged. Positive experiences should be maximized while negative experiences be minimized, as both were directly and interactively associated with depression. Intensive but not mild to moderate (< 80%) WFHS may impact depressive symptoms negatively via its direct association with depression; it also moderated the associations between positive/negative experiences due to social distancing and depression. Further research is required to discern the inter-relationships among WFHS, positive/negative experiences of social distancing, and depression to better cope with the stressful pandemic.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00127-021-02179-6.
Keywords: Social distancing, Working from home, Depression, Interaction, COVID-19, China
Introduction
Globally, there were over 182 million cases of coronavirus disease 2019 (COVID-19) and around 4 million deaths (July 1, 2021) [1]. As asymptomatic transmission of COVID-19 is common [2, 3], governments have widely adopted comprehensive social distancing measures, including conventional means (e.g., closure of schools and cancelation of public events) used during SARS and H1N1 [4, 5] and unprecedented measures (e.g., mandatory working from home and restriction of gathering size) [6–11]. Although social distancing is an obvious stressor (e.g., threats to employment, inconvenience, and social isolation) that escalates mental distress, the relationship has been scarcely studied. A Germany study documented a 20% increase in the number of helpline contacts received during the first week of the lockdown; the heightened levels of loneliness, anxiety, and suicidal ideation were related to the strictness of the states’ lockdown [12]. Another U.S. study found non-significant associations between implementation of the state-level gathering measures (e.g., home-staying and banning large gatherings) and mental distress (e.g., depression/suicidal attempts) [13].
A dearth of studies has looked at the associations between positive and negative experiences due to social distancing and mental distress. First, social distancing reduces social activities and may result in isolation/disconnection that induces mental distress (e.g., depression and anxiety) [14, 15]. Second, social distancing causes substantial inconvenience (e.g., closure of public facilities and schools/classes, working-from-home, and travel restrictions) that may induce mental distress; such a relationship has not been studied. Third, social distancing has positive impacts. It has slowed down the exhaustive pace of urban lifestyles and spared time/energy for personal and family life. Positive perceptions toward social distancing [e.g., “(it) had not been hard”, and “more time with family members”] have been reported [16]. Relaxation is protective against mental distress [17], while good family relationship/communication are important protective coping resources [18, 19].
Working from home is a modern trend [20, 21] that is likely to expand in the future [22]. In many countries (e.g., the U.K. [23], Germany [24], and the U.S. [25]), working from home during the COVID-19 pandemic had been mandatory; 37.7% of the adults in mainland China worked from home during the COVID-19 pandemic [26]. In Hong Kong where the present study was conducted, civil servants worked from home from early February to May 4, 2020, while many offices followed the suit from March to May. As working from home involves positive (e.g., work-life balance, saving transportation time, and schedule flexibility) and negative attributes (e.g., less sustained motivation, sub-optimal working environment, difficulty in unwinding after work, and longer working hours) [27], its relationship with mental distress is potentially mixed. Previous studies found that those who worked away from offices using digital technologies (‘remote workers’) reported higher levels of loneliness and negative emotions [28, 29]; another report found that ‘remote workers’ were more stressful than their counterparts working at the office [30]. However, other studies reported lower levels of stress among ‘remote workers’ [29] and non-significant associations between working from home and general health/mental health [26].
Besides looking at the direct effects of working from home and experiences due to social distancing, the present study tested a number of interaction effects. First, as working from home has been occurring in the context of social distancing during the COVID-19 pandemic, it may interact with the positive and negative experiences due to social distancing to jointly affect mental distress. A novel hypothesis was tested in this study about whether working from home would modify the potential impacts of positive and negative experiences due to social distancing on depression. For instance, a longer period of working from home might amplify the negative impact of social isolation due to social distancing on depression. Second, the various types of experiences due to social distancing (e.g., social isolation, inconvenience, and change in family relationship) were potential risk and protective factors of depression, they might also interact with each other. In the literature, protective and risk factors sometimes interact with each other to affect mental distress [31, 32]. For instance, a protective factor may buffer the detrimental effect of a risk factor [33], or a risk factor might wash out part of the positive effect of a protective factor [31], or two protective (or risk) factors might interact with each other [34] to affect mental distress. The two sets of interaction hypotheses are novel and have implications on programs promoting mental health during the COVID-19 period.
The present study hence, investigated some objectives that have not been reported in literature: (1) the levels of working from home status (WFHS), positive experiences due to social distancing (improved family relationship and relaxation feeling in daily life), and negative experiences due to social distancing (social isolation and perceived huge inconvenience) among income-earning adults aged 18–65 years in the Chinese Hong Kong general population, (2) potential factors of depressive symptoms including WFHS, positive social distancing experiences, and negative social distancing experiences, (3) the interactions between the positive and negative experiences due to social distancing on depressive symptoms, and (4) the moderation effects of WFHS on the associations between the positive/negative experiences due to social distancing and depressive symptoms. The alternate hypotheses included (a) the positive/negative experiences due to social distancing would be negatively/positively associated with depressive symptoms; (b) WFHS would be positively or negatively associated with depressive symptoms; (c) the positive experiences would interact with the negative experiences to affect depressive symptoms (for instance, the positive experience of improved family relationship due to social distancing would buffer the association between social isolation on depressive symptoms, while improved family relationship and relaxation feeling in daily life would be synergistic in reducing the risk of depression); (d) WFHS would moderate the associations between the positive/negative experiences and depressive symptoms (for instance, the risk effect of social isolation on depressive symptoms would be stronger among those with intensive WFHS than the others).
Methods
Participants and data collection
A random cross sectional population-based telephone survey was conducted among Hong Kong Chinese adults (aged ≥ 18 years) during April 21–28, 2020. Telephone numbers were randomly drawn from the sampling frame of the most updated residential telephone directory. The high penetration rate of household phones in Hong Kong of 84.9% (May, 2020) [35] supports the research design. The household member whose birthday was closest to the interview date was invited to join the study. Unanswered telephone calls were given at least three attempts before being classified as invalid. Unavailable eligible participants were contacted again by appointments. Participants were anonymously interviewed for 10–15 min between 6 and 10:30 pm by some experienced research staff. No incentives were given to the participants. Verbal informed consent was obtained prior to the commencement of the survey. The study was approved by the ethics committee of the corresponding author’s affiliated institution.
Of the 552 contacted eligible persons, 300 completed the interviews (response rate: 300/552 = 54.3%). A paper based on the parent sample (n = 300) has been published [36]. A subsample (n = 200) of all the income-earning participants aged ≤ 65 was selected from the parent sample for this report, as most of those aged > 65 were retired and would find working from home less relevant.
Measures
Background factors
Information about sex, age, current marital status, and educational level was collected.
Depressive symptoms
The 9-item Patient Health Questionnaire (PHQ-9) was used to assess depressive symptoms. It was validated in Chinese populations and showed good psychometric properties [37]. The items asked about the frequencies that specific depressive symptoms (e.g., “little interest or pleasure in doing things” and “feeling down, depressed, or hopeless”) had occurred during the past 2 weeks (0 = not at all to 3 = nearly every day). Summative scores ≥ 5, 10, 15, and 20 were defined as mild, moderate, moderately severe, and severe depression, respectively. In the present study, Cronbach’s alpha of PHQ-9 was 0.84.
Working from home status (WFHS)
The WFHS variable has three categories according to the number of days experiencing working from home in the past 2 weeks: (1) the reference group: WFHS = 0–2 days (including those with self-employment), (2) WFHS = 3–7 days, and (3) WFHS ≥ 8 days.
Experiences due to social distancing
Negative experiences:
Social Isolation due to Social Distancing Scale (SISDS): The 4-item scale assessed the levels of social isolation due to social distancing during the pandemic [ (i) loneliness, (ii) loss of peer’s social support, (iii) less intimate relationship with friends, and (iv) boredom] (five points: 1 = never to 5 = always; Cronbach’s alpha = 0.81).
Perceived huge inconvenience due to social distancing: The item was “Social distancing has caused me huge inconvenience” (1 = extremely disagree to 5 = extremely agree).
Positive experiences:
Improved relationship with family members due to social distancing: The item asked how often the participant had experienced improved relationship with his/her family members due to social distancing” (1 = never to 5 = always).
Relaxation feeling in daily life due to social distancing: An item asked how often the participant felt more relaxed in his/her daily life due to social distancing (1 = never to 5 = always).
Statistical analyses
The sample size planning was conducted using the Tests for One Correlation Module in the PASS 11.0. Assuming power = 0.80 and alpha = 0.05, the sample size of 200 would have the smallest detectable correlation coefficient (r) of 0.20, which represents a small effect size [38]. It deems to be adequate. Three types of regression analyses were performed to investigate the associations between the independent variables (i.e., WFHS and the positive/negative experiences due to social distancing) and depressive symptoms, including (1) simple (bivariate) regression between two variables, (2) regression models involving one of the five independent variables (e.g., WFHS) adjusted for all the studied background variables, and (3) a summary regression model including all the five independent variables simultaneously in the same model (the “Enter” option as the variable selection method in regression analysis).
The interaction effects were tested by using hierarchical linear regression analyses. The direct effect models including two of the independent variables were tested (e.g., WFHS and perceived huge inconvenience), adjusted for background variables; the interaction terms (e.g., WFHS × perceived huge inconvenience) were then added to the direct effect models to test the statistical significance of the interaction term. This is a standard epidemiological approach to test interactions [39]. Structural equation modeling (SEM) method is another option, which in this case yielded almost the same results compared to the regression approach. As this study involved neither latent variables, nor multiple dependent variables, nor complicated pathways, the results of the regression approach, but not SEM, is presented hereby.
All statistical analyses were performed by using SPSS 21.0. Statistically significant levels were defined as p < 0.05.
Results
Descriptive statistics (Table S1)
More than half of the participants were females (67.0%), aged ≤ 55-years old, and being currently married/cohabitating with someone (64.0%). Around one third (33.5%) had received tertiary education or above. The prevalence of mild (PHQ-9 ≥ 5) and moderate-to-severe (PHQ-9 ≥ 10) depression was 8.5% and 3.5%, respectively; the mean (SD; range) PHQ-9 score was 1.7 (3.0; 0–24). The distribution of the WFHS variable was 73.0% (0–2 days), 14.0% (3–7 days), and 13.0% (≥ 8 days) in the past 2 weeks. About 1/4 (26.0%) frequently/always perceived at least one of the four specific social isolation experiences: loneliness (9.0%), loss of peer’s social support (11.0%), less intimate relationship with friends (6.5%), and boredom (23.5%); the mean (SD; range) SISDS score was 7.7 (3.4; 4–20). Furthermore, about 1/3 (34.0%) agreed/extremely agreed that social distancing was hugely inconvenient; about 1/5 frequently/always felt improved relationship with family members (22.0%) and relaxed in daily life (17.7%) due to social distancing.
Correlations among the independent variables (Table S2)
(1) WFHS was positively correlated with perceived huge inconvenience (r = 0.22; p = 0.002), but not with the other three types of positive/negative experiences due to social distancing. (2) Positive correlations were observed between SISDS and perceived huge inconvenience (r = 0.20; p = 0.004) and between improved family relationship and relaxation feeling in daily life (r = 0.33; p < 0.001), respectively. (3) The individual correlations between the negative experiences and positive experiences were statistically non-significant, except for the positive association between SISDS and relaxation feeling in daily life (r = 0.26; p < 0.001).
Associations between the background variables and the independent variables
Participants aged 56–65 years were more likely than others to have perceived huge inconvenience (β = 0.21, p = 0.012) and improved relationship with family members due to social distancing (β = 0.27, p = 0.001). The other associations between the background factors and WFHS/SISDS/relaxation feeling in daily life were statistically non-significant. The results are not presented in the tables.
Factors of depressive symptoms
None of the background factors (sex, age, marital status, and educational level) were significantly associated with depressive symptoms; such data were not presented in the tables. (1) The Pearson correlation coefficients between SISDS/improved family relationship/relaxation in daily life/perceived inconvenience and depressive symptoms were 0.28 (p < 0.001)/ − 0.16 (p = 0.027)/ − 0.17 (p = 0.019)/0.13 (p = 0.065). WFHS was not significantly associated with depressive symptoms according to the overall ANOVA test (p = 0.188); the comparison between WFHS ≥ 8 days versus WFHS = 0–2 days showed a p value of 0.076). (These data are not presented in the tables). Betas of similar bivariate regression models are shown in Table 1. (2) In the adjusted analyses, the four types of positive/negative experiences due to social distancing were all significantly associated with depressive symptoms [(a) SISDS (β = 0.29, p < 0.001), (b) perceived huge inconvenience (β = 0.17, p = 0.013), (c) improved family relationship (β = − 0.15, p = 0.038), (d) relaxation feeling in daily life (β = − 0.16, p = 0.024)], whereas, the associations between WFHS ≥ 8 days / 3–7 days and depressive symptoms were non-significant (β = 0.13, p = 0.073/β = − 0.01, p = 0.919). 3) In the adjusted summary model that contains all the independent variables (Table 1), significant associations with depression were found for the factors of WFHS ≥ 8 days (β = 0.15, p = 0.027; reference group: WFHS = 0–2 days), SISDS (β = 0.36, p < 0.001) and relaxation feeling in daily life (β = − 0.22, p = 0.002), whereas, improved family relationship (β = − 0.13, p = 0.059) and perceived huge inconvenience (β = 0.09, p = 0.196) were statistically non-significant.
Table 1.
Univariate and multivariate linear regression analysis (n = 200)
| Dependent variable: depressive symptoms | ||||||
|---|---|---|---|---|---|---|
| Simple linear regression | Adjusted linear regression modelsa | Summary modelb | ||||
| β (95% CI) | P | β (95% CI) | p | β (95% CI) | p | |
| Working from home status (WFHS) | ||||||
| WFHS = 0–2 days | Ref = 1.0 | Ref = 1.0 | Ref = 1.0 | |||
| WFHS = 3–7 days | − 0.01 (− 0.15 to 0.13) | 0.885 | − 0.01 (− 0.15 to 0.13) | 0.919 | − 0.02 (− 0.15 to 0.11) | 0.773 |
| WFHS ≥ 8 days | 0.13 (− 0.01 to 0.27) | 0.070 | 0.13 (− 0.01 to 0.27) | 0.073 | 0.15 (0.02–0.28) | 0.027 |
| SISDS | 0.28 (0.17–0.41) | < .001 | 0.29 (0.16–0.42) | < 0.001 | 0.36 (0.23–0.49) | < 0.001 |
| Perceived huge inconvenience | 0.13 (− 0.01 to 0.27) | 0.060 | 0.17 (0.04–0.31) | 0.013 | 0.09 (− 0.05 to 0.22) | 0.196 |
| Improved family relationship | − 0.16 (− 0.20 to − 0.11) | 0.023 | −0.15 (− 0.28 to − 0.01) | 0.038 | − 0.13 (− 0.26 to 0.01) | 0.059 |
| Relaxation feeling in daily life | − 0.17 (− 0.30 to − 0.03) | 0.016 | − 0.16 (− 0.29 to − 0.02) | 0.024 | − 0.22 (− 0.35 to − 0.08) | 0.002 |
SISDS the Social Isolation due to Social Distancing Scale, CI confidence interval
aIndividual models that were adjusted for the studied background variables (sex, age, marital status, and educational levels) were fit
bA single multivariable regression model was fit, with all five independent variables being entered into the same model and adjusted for the studied background variables
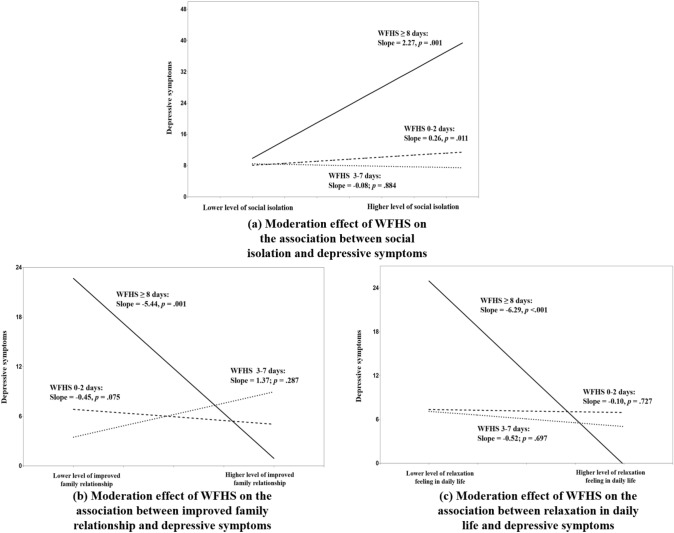
Testing the interaction effects
In Table 2 (Model 2a to 2f), one of the six interaction items between the pairs of positive and negative experiences [i.e., improved family relationship × perceived huge inconvenience (β = − 0.56, p = 0.010)] was statistically significant. In Fig. 1, improved family relationship buffered the risk effect of perceived huge inconvenience on depressive symptoms; the risk effect of perceived huge inconvenience on depressive symptoms was non-significant among those with stronger improved family relationship. In Table 3, three interaction terms [i.e., WFHS ≥ 8 days × SISDS (β = 0.55, p = 0.005), WFHS ≥ 8 days × improved family relationship (β = − 0.49, p = 0.004), and WFHS ≥ 8 days × relaxation in daily life (β = − 0.61, p < 0.001)] were statistically significant, while the interaction between WFHS ≥ 8 days and perceived huge inconvenience and the four interaction between WFHS = 3–7 days and positive/negative experiences (e.g., WFHS = 3–7 days × relaxation feeling in daily life) were statistically non-significant. Figure 2a shows that the positive association between SISDS and depressive symptoms was significant in the WFHS ≥ 8 days group, and was also stronger (a deeper slope) than that of the WFHS = 0–2 days group (the reference group); the corresponding slope was non-significant in the WFHS = 3–7 days group (the interaction effect involving WFHS = 3–7 days was non-significant). Figure 2b and c show that the protective effects of the positive experiences (improved family relationship and relaxation feelings in daily life) on depressive symptoms, as reflected by the negative slopes, were significant in the WFHS ≥ 8 days group, but neither WFHS = 3–7 days nor WFHS = 0–2 days groups. Figure 2b and 2c further show that the WFHS ≥ 8 days group reported much higher levels of depressive symptoms than the WFHS = 3–7 days and WFHS = 0–2 days groups both at lower levels of improved family relationship and relaxation feeling in daily life. In reverse, the level of depressive symptoms was slightly lower in the WFHS ≥ 8 days group than in the WFHS = 3–7 days and WFHS = 0–2 days groups at higher levels of improved family relationship and relaxation feeling in daily life due to social distancing.
Table 2.
Testing the interaction effects between the negative and positive experiences due to social distancing onto depressive symptoms (n = 200)
| Dependent variable: depressive symptoms | ||||
|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | |
| Model 1a | Model 2a | |||
| Improved family relationship | − 0.20 (− 0.33 to − 0.06) | 0.004 | − 0.10 (− 0.04 to 0.20) | 0.504 |
| SISDS | 0.32 (0.19–0.45) | < .001 | 0.40 (0.13–0.68) | 0.004 |
| Improved family relationship × SISDS | − 0.14 (− 0.55 to 0.26) | 0.490 | ||
| Model 1b | Model 2b | |||
| Improved family relationship | − 0.15 (− 0.29 to − 0.02) | 0.028 | 0.26 (− 0.09 to 0.60) | 0.144 |
| Perceived huge inconvenience | 0.18 (0.04–0.32) | 0.009 | 0.49 (0.22–0.76) | < 0.001 |
| Improved family relationship × Perceived huge inconvenience | − 0.56 (− 0.99 to − 0.13) | 0.010 | ||
| Model 1c | Model 2c | |||
| Relaxation feeling in daily life | − 0.26 (− 0.39 to − 0.12) | < .001 | 0.03 (− 0.29 to 0.36) | 0.844 |
| SISDS | 0.36 (0.23–0.49) | < .001 | 0.56 (0.32–0.80) | < 0.001 |
| Relaxation feeling in daily life × SISDS | − 0.41 (− 0.83 to 0.01) | 0.057 | ||
| Model 1d | Model 2d | |||
| Relaxation feeling in daily life | − 0.17 (− 0.30 to − 0.05) | 0.013 | 0.09 (− 0.26 to 0.44) | 0.602 |
| Perceived huge inconvenience | 0.19 (0.05–0.32) | 0.007 | 0.36 (0.11–0.62) | 0.005 |
| Relaxation feeling in daily life × Perceived huge inconvenience | − 0.35 (− 0.77 to 0.08) | 0.111 | ||
| Model 1e | Model 2e | |||
| Improved family relationship | − 0.10 (− 0.25 to 0.05) | 0.177 | − 0.18 (− 0.44 to 0.09) | 0.184 |
| Relaxation feeling in daily life | − 0.12 (− 0.27 to 0.03) | 0.107 | − 0.23 (− 0.57 ~ 0.11) | 0.191 |
| Improved family relationship × Relaxation feeling in daily life | 0.16 (− 0.30 to 0.62) | 0.495 | ||
| Model 1f | Model 2f | |||
| SISDS | 0.26 (0.13–0.40) | < 0.001 | 0.20 (− 0.13 to 0.54) | 0.237 |
| Perceived huge inconvenience | 0.12 (− 0.02 to 0.25) | 0.095 | 0.06 (− 0.25 to 0.38) | 0.712 |
| SISDS × Perceived huge inconvenience | 0.10 (− 0.38 to 0.58) | 0.701 | ||
The models were adjusted for background variables (sex, age, marital status, and educational levels)
SISDS the Social Isolation due to Social Distancing Scale, CI confidence interval
Fig. 1.

Moderation effect of improved family relationship between perceived huge inconvenience and depressive symptoms
Table 3.
Testing the interaction effects between WFHS and positive/negative experiences due to social distancing onto depressive symptoms
| Depressive symptoms | ||||
|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | |
| Model 3a | Model 4a | |||
| WFHS × social isolation | ||||
| SISDS | 0.30 (0.17–0.43) | < 0.001 | 0.26 (0.06–0.46) | 0.010 |
| WFHS = 0–2 days | Ref = 1.0 | Ref = 1.0 | ||
| WFHS = 3–7 days | − 0.02 (− 0.15 to 0.12) | 0.813 | 0.09 (− 0.37 to 0.56) | 0.693 |
| WFHS ≥ 8 days | 0.15 (0.01–0.28) | 0.031 | − 0.21(− 0.61 to 0.19) | 0.302 |
| WFHS = 0–2 days × SISDS | Ref = 1.0 | |||
| WFHS = 3–7 days × SISDS | − 0.14 (− 0.61 to 0.32) | 0.546 | ||
| WFHS ≥ 8 days × SISDS | 0.55 (0.16–0.94) | 0.005 | ||
| Model 3b | Model 4b | |||
| WFHS × perceived huge inconvenience | ||||
| Perceived huge inconvenience | 0.16 (0.02–0.30) | 0.026 | 0.18 (− 0.06 to 0.40) | 0.100 |
| WFHS = 0–2 days | Ref = 1.0 | Ref = 1.0 | ||
| WFHS = 3–7 days | − 0.03 (− 0.17 to 0.11) | 0.651 | − 0.17 (− 0.69 to 0.36) | 0.532 |
| WFHS ≥ 8 days | 0.10 (− 0.05 to 0.24) | 0.196 | 0.03 (− 0.55 to 0.60) | 0.936 |
| WFHS = 0–2 days × perceived huge inconvenience | Ref = 1.0 | |||
| WFHS = 3–7 days × perceived huge inconvenience | 0.11 (− 0.43 to 0.66) | 0.687 | ||
| WFHS ≥ 8 days × perceived huge inconvenience | 0.26 (− 0.32 to 0.84) | 0.390 | ||
| Model 3c | Model 4c | |||
| WFHS × improved family relationship | ||||
| Improved family relationship | − 0.15 (− 0.29 to − 0.01) | 0.030 | − 0.18 (− 0.39 to 0.02) | 0.073 |
| WFHS = 0–2 days | Ref = 1.0 | Ref = 1.0 | ||
| WFHS = 3–7 days | − 0.01 (− 0.15 ~ 0.13) | 0.879 | − 0.28 (− 0.66 to 0.10) | 0.150 |
| WFHS ≥ 8 days | 0.14 (− 0.01 ~ 0.27) | 0.058 | 0.70 (0.39–1.02) | < 0.001 |
| WFHS = 0–2 days × improved family relationship | Ref = 1.0 | |||
| WFHS = 3–7 days × improved family relationship | 0.27 (− 0.12 to 0.66) | 0.176 | ||
| WFHS ≥ 8 days × improved family relationship | − 0.49 (− 0.81 to − 0.16) | .004 | ||
| Model 3d | Model 4d | |||
| WFHS × relaxation feeling in daily life | ||||
| Relaxation feeling in daily life | − 0.16 (− 0.30 to − 0.02) | 0.018 | − 0.04 (− 0.25 to 0.18) | 0.726 |
| WFHS = 0–2 days | Ref = 1.0 | Ref = 1.0 | ||
| WFHS = 3–7 days | 0.01 (− 0.14 to 0.14) | 0.950 | 0.01 (− 0.36 to 0.38) | 0.960 |
| WFHS ≥ 8 days | 0.14 (− 0.01 to 0.28) | 0.052 | 0.80 (0.49–1.12) | < 0.001 |
| WFHS = 0–2 days × relaxation feeling in daily life | Ref = 1.0 | |||
| WFHS = 3–7 days × relaxation feeling in daily life | − 0.06 (− 0.43–0.32) | 0.768 | ||
| WFHS ≥ 8 days × relaxation in daily life | − 0.61 (− 0.94 to − 0.27) | < 0.001 | ||
The models were adjusted for background factors (sex, age, marital status, and educational levels)
WFHS working from home status in the past two weeks, SISDS the Social Isolation due to Social Distancing Scale, CI confidence interval
Fig. 2.
Moderation effect of working from home status (WFHS) on the associations between negative/negative experiences due to social distancing and depressive symptoms
Discussion
About one-eighth of the participants showed mild-to-severe depression. The prevalence of moderate to severe (PHQ-9 ≥ 10) was 3.5%, which was comparable to that of 4.3% in the Hong Kong general population in 2009 [40], but was lower than the 11.2% reported in 2019 when there was violent social unrest that had resulted in over 7000 arrests [41], which has calmed down during the COVID-19 period. Thus, the level of population mental distress might have returned to a ‘normal’ state. Higher prevalence of mild-to-severe depression (also based on PHQ-9) during the COVID-19 pandemic has been reported in some other general populations, such as Nepal (25.3%) [42], Australia (52.1%) [43], Iran (60.2%) [44], Austria (54.6%) [45], and U.K. (63.9%) [45]. The prevalence of depression in this study might have been underestimated, due to potential selection bias caused by the relatively low response rate (< 60%), as non-respondents might have more depressive symptoms than those participating in research studies [46]. However, the differences from that of other countries seem too large to be dismissed. The reasons of the lower prevalence of depression in Hong Kong might be related to the low number of COVID-19 cases and less stringent social distancing measures exercised in Hong Kong, but confirmation is needed.
Social distancing measures are controversial and have met resistance in multiple countries, due to resulting potentially severe financial burden and restriction on personal freedom. Loneliness was one of the key consequences of social distancing [14, 15]. The present study found that 26% of the participants had expressed at least one dimension of social isolation (loneliness, boredom, less intimate social relationship, and loss of peer’s social support) due to social distancing, which can be considered loss of personal and social resources [47]. According to the Conservation of Resource (COR) theory, loss of resources are key mechanisms that trigger stress responses that lead to mental distress [48]. The COR theory has been applied to other studies on mental distress [47, 49, 50] and is supported by our data. Future studies need to look at what extent social isolation could be reduced by means of social media during the COVID-19 period. A Singaporean study found that older people at risk of social isolation were substantially less likely to use devices and technology for social connections during the COVID-19 pandemic [51]. Attention should be paid to potential disparity in accessibility to social media in special social groups. For instance, social media was not used by around 60% of people aged over 65 years in the U.S. [52]. Subsidies to access and enhancement of skills for Internet use among disadvantaged people (e.g., those on social security) may be essential. However, as overuse of social media might also increase loneliness [53], caution about overuse of social media during the pandemic is important.
Another negative consequence of social distancing was perceived huge inconvenience, which was reported by about one-third of the participants. It is noteworthy that older participants (> 55) were more likely than others to report perceived huge inconvenience. They might rely more on offline services than younger people. Perceived huge inconvenience was positively associated with mental distress in the adjusted analysis of single independent variable but not in the summary model after adjusting for other types of positive and negative experiences due to social distancing and WFHS. The turning of the variable of perceived huge inconvenience into non-significance in the latter model may be due to its associations with other negative experiences due to social distancing. It is important to assist people to overcome potential inconvenience encountered during the pandemic by facilitating their adaption to the new expedited electronic era.
It is noteworthy that social distancing is double-edged. The present study is possibly the first one to look at both the positive and negative experiences due to social distancing simultaneously. About 1/3 of the participants reported either improvement in family relationship or perceived more relaxed daily life. Interestingly, relaxation in daily life was positively associated with social isolation. People might have less activities and thus feel less stressful and more relaxed, but at the same time, socially isolated. However, the positive aspects of social distancing might have been under-emphasized in literature. Supporting our hypotheses, the positive experience of relaxation in daily life (and possibly also improvement in family relationship as its association with depressive symptoms was significant in the simple correlation and adjusted association of single independent variable) due to social distancing was protective against mental distress during the pandemic. Other studies have also shown that with social distancing, people may spare more time for themselves and their family members [16], which may lead to the relaxation feeling in daily life and better family relationship that are potentially protective against mental distress [17–19]. There are some interesting findings and implications. First, some of the positive and negative experiences were significantly associated with mental distress. The positive experience of relaxation feeling in daily life and the negative experience of social isolation due to social distancing were both significantly associated with depressive symptoms in the same multivariable summary regression model, adjusted for WFHS and background factors. The findings suggest that some positive and negative experiences due to social distancing might simultaneously and independently influence depressive symptoms in opposite (beneficial and harmful) directions. Second, based on the beta values of the adjusted and summary modes, the positive association between social isolation (a negative experience) and depression was stronger than the negative associations between relaxation feeling in daily life (positive experiences) and depression. Future studies may confirm the relative impact of positive versus negative experiences of social distancing on depression. Third, improved family relationship buffered perceived huge inconvenience; the risk effect of perceived huge inconvenience onto depression even disappeared in the presence of strongly improved family relationship. Future studies should thus investigate the complicated interactions between positive and negative experiences of social distancing on mental distress.
Over one-fourth of the participants had experienced working from home ≥ 3 days, while 13% had WFHS ≥ 8 days in the past 2 weeks. To many participants, working from home due to COVID-19 was a brand-new experience. It may induce mixed positive and negative effects on mental distress but such relationships have not been studied. WFHS ≥ 8 days was significantly associated with depression in the summary model after adjusting for positive/negative experiences due to social distancing and background variables. An important elaboration is that an “mild to moderate” working from home experience might not be significantly associated with mental distress but intensive WFHS did. As high intensity of working from home occurs in many countries where leaving home without a reason has been forbidden (e.g., the U.K. and Canada). It is contended that the impact of intensive working from home in those regions might even be stronger than our case. Further cross-country validation is necessary as cultural differences might matter.
It is interesting that WFHS interacted significantly with the positive and negative experiences due to social distancing to potentially affect mental distress. Again, the interaction involving a high level of WFHS (80%) but not those of a moderate level (30–70%) was significant, reinstating that mild to moderate WFHS might not have a substantial role in determining mental distress. First, intensive working from home might have amplified the risk effects of social isolation, as the intensive working from home experience may isolate people from the normal social environment of the work settings. Besides, it is plausible that both working from home [28, 29] and social isolation [54] may increase loneliness, and create synergistic risk effects on depressive symptoms. Second, the significant protective effect of relaxation feeling on depressive symptoms was only observed among those with a high level of WFHS (≥ 8 days). In words, among those working from home intensively (but not among those with nil/mild to moderate working from home experience), those who felt relaxed in daily life due to social distancing would have lower mental distress than those who did not feel relaxed. The lack of relaxation due to social distancing might also be due to the job nature (e.g., incompatibility to remote work), shortage of know-how (e.g., literacy of electronic communication), and home environment (e.g., disturbance by family members and no working station at home). Thus, it is important to support staff working from home intensively with training and empathy; counseling should also be given to those meeting difficulties and distress during the working from home process. Third, the interaction between WFHS and improved family relationship on depression was very similar to the aforementioned interaction between WFHS and relaxation, as shown by the respective figures. Such comparable findings suggest that the role and inter-relationships between WFHS and positive experiences due to social distancing might follow a general pattern, which warrants further investigation. Furthermore, it is seen from the figures that those having worked from home intensively reported highly elevated depressive symptoms when the level of social isolation was high and when the levels of improved family relationship/relaxation were low. In addition, when family relationships were largely improved or people felt very relaxed, those working from home intensively reported fewer depressive symptoms than those with WFHS = 0–2 days. The findings again reinstate the interactive nature between working from home intensively and other positive/negative experiences due to social distancing. Thus, those with intensive working from home experiences need to pay attention to enhancing positive experiences and minimizing social isolation during social distancing.
This study has several limitations. First, recall bias and social desirability bias may exist. For instance, social desirability bias (a form of reporting bias) might occur when some participants tended to under-report depressive symptoms because the feeling that others might associate their symptoms with personal weaknesses/failures and presentation of such depressive symptoms might result in stigma. Second, causal relationship cannot be made due to the cross sectional design. Third, the measurements of positive/negative experiences due to social distancing were self-constructed as there have been no available related assessments; some other experiences related to social distancing may not have been covered (e.g., financial loss). Fourth, the response rate was relatively low (54.3%) although it was comparable to other population-based telephone surveys in Hong Kong [55, 56]. In Hong Kong, landline phones are easy to obtain and inexpensive. However, we infer that single-person households are less likely than others to install such phones as no one would answer the phone when he/she is not at home. Data are not available to compare those with and without landline phones. Comparing the characteristics of the parent sample to those of the 2018 Hong Kong census population (Supplementary Table S3), the proportion of age was comparable, while those of females and secondary but not tertiary education attainment were over-sampled. There is no census data on non-income-earning people aged > 65 so we could not compare our subsample to their counterparts’ census information, but it is likely that sex was also over-represented in our subsample. If such is true, it implies that the prevalence of depression in this study might have been overestimated, as females tended to report higher levels of depression than males [57]. Besides, selection bias may occur, as participants might differ from refusers in some relevant characteristics. While the studied associations and interactions were statistically significant, some of the correlations were mild to moderate in magnitude. It should be understood that there are many determinants of depression; social distancing is only one of the potentially important perspectives and would not be able to explain a large part of the variance. A number of associations found in this study carried p value between 0.05 and 0.10 and were considered non-significant in hypothesis testing. As the sample size of this study was not large, the non-significance of such associations may have been influenced by limited statistical power; future studies may confirm the non-significance of these associations. Another limitation is that there might be multiple comparison effects when all the interaction analyses were tested simultaneously; the Type I error may have been inflated.
In conclusion, intensive WFHS and two types of negative experiences (social distancing and perceived huge inconvenience) and two types of positive experiences (improved family relationship and relaxation feeling in daily life) due to social distancing may have potential risk or protective effects on depressive symptoms. Some positive experiences also buffered the potential harms of the negative experiences on mental distress. We should pay attention to the potential positive consequences of social distancing and promote positive reframing coping strategy to social distancing. Furthermore, intensive WFHS (≥ 8 days) but not moderate WFHS interacted with social isolation, relaxation feeling in daily life, and improved family relationship due to social distancing. Thus, intensive WHFS and other positive/negative consequences of social distances might inter-play with each other to determine mental distress; modification of one factor might change other factors’ risk/protective effects on depression. Future studies are warranted to confirm these findings and explore-related interventions during the COVID-19 pandemic. The study shed some lights on a new direction of research on working from home and social distancing due to COVID-19, and extend our preparedness for a new ‘normal’ state of lifestyle in response to the COVID-19 pandemic.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all the participants for their contributions
Author contribution
Conceptualization: JTFL and YY; Methodology: YY and JTFL; Investigation: MMCL; Software: YY; Formal analysis: YY; Data curation: YY; Validation: JTFL; Resources: JTFL; Writing—original draft: YY and JTFL; Writing—review and editing: YY and JTFL; Supervision: JTFL; Funding acquisition: JTFL.
Funding
The study was supported by internal research funding of the Center for Health Behaviours Research, the Chinese University of Hong Kong.
Availability of data and materials
No other data available.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declared no conflicts of interest.
Ethical statement
The study was approved by the Survey and Behavioral Research Ethics Committee of the Chinese University of Hong Kong (No. SBRE-19-661).
References
- 1.WHO . World Health Organization, Coronavirus disease (COVID-19) weekly epidemiological update and weekly operational update. Geneva: WHO; 2020. [Google Scholar]
- 2.Hu Z, et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020;395:514. doi: 10.1007/s11427-020-1661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Tawfiq JA. Asymptomatic coronavirus infection: MERS-CoV and SARS-CoV-2 (COVID-19) Travel Med Infect Dis. 2020;35:101608. doi: 10.1016/j.tmaid.2020.101608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fong MW, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-social distancing measures. Emerg Infect Dis. 2020;26(5):976–984. doi: 10.3201/eid2605.190995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothstein MA. From SARS to Ebola: legal and ethical considerations for modern quarantine. Ind Health Law Rev. 2015;12:227. doi: 10.18060/18963. [DOI] [Google Scholar]
- 6.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2):020. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. 2020;20(6):631–633. doi: 10.1016/S1473-3099(20)30190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flaxman S, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584:257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 9.Lau H, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020;27:taaa037. doi: 10.1093/jtm/taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leung K, et al. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. 2020;395(10233):1382–1393. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stawicki SP, et al. The 2019–2020 novel coronavirus (severe acute respiratory syndrome coronavirus 2) pandemic: a joint american college of academic international medicine-world academic council of emergency medicine multidisciplinary COVID-19 working group consensus paper. J Glob Infect Dis. 2020;12(2):47. doi: 10.4103/jgid.jgid_86_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Armbruster S, Klotzbücher V (2020) Lost in lockdown? COVID-19, social distancing, and mental health in Germany. No. 2020-04; Albert-Ludwigs-Universität Freiburg, Wilfried-Guth-Stiftungsprofessur für Ordnungs- und Wettbewerbspolitik: Freiburg im Breisgau, Germany, 2020. https://www.econstor.eu/bitstream/10419/218885/1/1698957106.pdf. Accessed 1 Nov 2021
- 13.Bryan C, Bryan AO, Baker JC. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among US adults during the early COVID-19 pandemic. Suicide Life Threat Behav. 2020;50(6):1223–1229. doi: 10.1111/sltb.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abel T, McQueen D. The COVID-19 pandemic calls for spatial distancing and social closeness: not for social distancing. Int J Public Health. 2020;65:231. doi: 10.1007/s00038-020-01366-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The U.S. Centers for Disease Control and Prevention, Coping with stress (2020). Available at: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html. Accessed 26 June 26 2020
- 16.Williams SN, et al. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: a UK-based focus group study. medRxiv. 2020;18:77. doi: 10.1136/bmjopen-2020-039334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swami V, et al. General health mediates the relationship between loneliness, life satisfaction and depression. Soc Psychiatry Psychiatr Epidemiol. 2007;42(2):161–166. doi: 10.1007/s00127-006-0140-5. [DOI] [PubMed] [Google Scholar]
- 18.Cumsille PE, Epstein N. Family cohesion, family adaptability, social support, and adolescent depressive symptoms in outpatient clinic families. J Fam Psychol. 1994;8(2):202–214. doi: 10.1037/0893-3200.8.2.202. [DOI] [Google Scholar]
- 19.Herman-Stahl M, Petersen AC. Depressive symptoms during adolescence: direct and stress-buffering effects of coping, control beliefs, and family relationships. J Appl Dev Psychol. 1999;20(1):45–62. doi: 10.1016/S0193-3973(99)80003-3. [DOI] [Google Scholar]
- 20.Huws U et al (2019) The platformisation of work in Europe: Results from research in 13 European countries. https://uhra.herts.ac.uk/handle/2299/21600. Accessed 1 Nov 2021
- 21.Spreitzer GM, Cameron L, Garrett L. Alternative work arrangements: Two images of the new world of work. Annu Rev Organ Psychol Organ Behav. 2017;4:473–499. doi: 10.1146/annurev-orgpsych-032516-113332. [DOI] [Google Scholar]
- 22.Spurk D, Straub C. Flexible employment relationships and careers in times of the COVID-19 pandemic. Amsterdam: Elsevier; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Government of the U.K., Working Safely During Coronavirus (COVID-19) (2020). https://www.gov.uk/guidance/working-safely-during-coronavirus-covid-19. Accessed 29 June 2020
- 24.Bird and Bird, COVID-19: Guidance for Employers in Germany (2020). https://www.twobirds.com/en/news/articles/2020/global/multinational-employer-series-tackling-coronavirus-in-germany. Accessed 2 July 2020
- 25.Forbes, is Working from Home the Future of Work? (2020) https://www.forbes.com/sites/nextavenue/2020/04/10/is-working-from-home-the-future-of-work/#b8b864846b1f. Accessed 28 June 2020
- 26.Zhang SX, et al. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288:112958. doi: 10.1016/j.psychres.2020.112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forbes, are Home Offices Fueling a Mental Healh Crisis? (2020) https://www.forbes.com/sites/laurelfarrer/2019/04/12/are-home-offices-fueling-a-mental-health-crisis/#222f0d3a3ea3. Accessed 26 June 2020
- 28.Grant CA, Wallace LM, Spurgeon PC. An exploration of the psychological factors affecting remote e-worker's job effectiveness, well-being and work-life balance. Employ Relat. 2013;35:527. doi: 10.1108/ER-08-2012-0059. [DOI] [Google Scholar]
- 29.Mann S, Holdsworth L. The psychological impact of teleworking: stress, emotions and health. New Technol Work Employ. 2003;18(3):196–211. doi: 10.1111/1468-005X.00121. [DOI] [Google Scholar]
- 30.Healthline, Working from Home and Depression (2020). https://www.healthline.com/health/working-from-home-depression#5-to-dos. Accessed 26 June 2020
- 31.Wu AM, et al. Potential impact of Internet addiction and protective psychosocial factors onto depression among Hong Kong Chinese adolescents–Direct, mediation and moderation effects. Compr Psychiatry. 2016;70:41–52. doi: 10.1016/j.comppsych.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 32.Raffaelli M, et al. Stress, social support, and depression: a test of the stress-buffering hypothesis in a Mexican sample. J Res Adolesc. 2013;23(2):283–289. doi: 10.1111/jora.12006. [DOI] [Google Scholar]
- 33.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- 34.Muñoz-Navarro R, et al. Worry about COVID-19 contagion and general anxiety: Moderation and mediation effects of cognitive emotion regulation. J Psychiatr Res. 2021;137:311–318. doi: 10.1016/j.jpsychires.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.The Government of the Hong Kong S.A.R, Key Communications Statistics (2020). https://www.ofca.gov.hk/en/data_statistics/data_statistics/key_stat/index.html. Accessed 30 Nov 2020
- 36.Yu Y, Lau JTF, Lau MMC. Competing or interactive effect between perceived response efficacy of governmental social distancing behaviors and personal freedom on social distancing behaviors in the chinese adult general population in Hong Kong. Int J Health Policy Manag. 2020 doi: 10.34172/ijhpm.2020.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang YL, et al. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. 2013;5(4):268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 38.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Earlbaum Associates Publisher; 1988. pp. 8–16. [Google Scholar]
- 39.Hayes AF. Introduction to mediation, moderation, and conditional process analysis second edition: a regression-based approach. New York: The Guilford Press; 2018. [Google Scholar]
- 40.Yu X, et al. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry. 2012;53(1):95–102. doi: 10.1016/j.comppsych.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 41.Ni MY, et al. Depression and post-traumatic stress during major social unrest in Hong Kong: a 10-year prospective cohort study. Lancet. 2020;395(10220):273–284. doi: 10.1016/S0140-6736(19)33160-5. [DOI] [PubMed] [Google Scholar]
- 42.Gupta AK, et al. Psychological impact of ‘Lockdown’due to COVID-19 pandemic in Nepal: an online survey. Asian J Psychiatry. 2020;54:102243. doi: 10.1016/j.ajp.2020.102243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fisher JR, et al. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med J Aust. 2020;213:458. doi: 10.5694/mja2.50831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maroufizadeh S et al (2020) Prevalence of anxiety and depression in general population of Iran during the COVID-19 Pandemic: a web-based cross-sectional study. Research square (preprint). https://assets.researchsquare.com/files/rs-39082/v1/4fcaef8d-146f-4f37-9a8e-b4ce47333d8f.pdf?c=1631844925. Accessed 1 Nov 2021
- 45.Pieh C, Budimir S, Probst T (2020) Mental health during COVID-19 lockdown: a comparison of Austria and the UK. SSRN 3592372 (preprint)
- 46.Mirowsky J, Reynolds JR. Age, depression, and attrition in the National Survey of Families and Households. Sociol Methods Res. 2000;28(4):476–504. doi: 10.1177/0049124100028004004. [DOI] [Google Scholar]
- 47.Hou WK, et al. Threat to democracy: physical and mental health impact of democracy movement in Hong Kong. J Affect Disord. 2015;186:74–82. doi: 10.1016/j.jad.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hobfoll SE. The ecology of stress. New Jersey: Taylor and Francis; 1988. [Google Scholar]
- 49.Hall BJ, et al. Loss of social resources predicts incident posttraumatic stress disorder during ongoing political violence within the Palestinian Authority. Soc Psychiatry Psychiatr Epidemiol. 2015;50(4):561–568. doi: 10.1007/s00127-014-0984-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Topa G, et al. Resource loss and gain, life satisfaction, and health among retirees in Spain: mediation of social support. J Aging Health. 2017;29(3):415–436. doi: 10.1177/0898264316635589. [DOI] [PubMed] [Google Scholar]
- 51.Malhotra R, Visaria A (2020) Social isolation in the COVID-19 pandemic–is maintaining social connections online a viable option for all older persons: insights from Singapore. SSRN 3609081 (preprint)
- 52.Pew Research Center, Social Media Fact Sheet (2019). https://www.pewresearch.org/internet/fact-sheet/social-media/. Accessed 26 July 2020
- 53.Moretta T, Buodo G. Problematic internet use and loneliness: How complex is the relationship? A short literature review. Curr Addict Rep. 2020;7(2):125–136. doi: 10.1007/s40429-020-00305-z. [DOI] [Google Scholar]
- 54.Weiss RS. Loneliness: The experience of emotional and social isolation. Cambridge: MIT Press; 1973. [Google Scholar]
- 55.Lau J, et al. Monitoring community responses to the SARS epidemic in Hong Kong: from day 10 to day 62. J Epidemiol Community Health. 2003;57(11):864–870. doi: 10.1136/jech.57.11.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim JH, et al. Prevalence and the factors associated with binge drinking, alcohol abuse, and alcohol dependence: a population-based study of Chinese adults in Hong Kong. Alcohol Alcohol. 2008;43(3):360–370. doi: 10.1093/alcalc/agm181. [DOI] [PubMed] [Google Scholar]
- 57.Eid RS, Gobinath AR, Galea LA. Sex differences in depression: Insights from clinical and preclinical studies. Prog Neurobiol. 2019;176:86–102. doi: 10.1016/j.pneurobio.2019.01.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No other data available.
Not applicable.