Abstract
Objectives. To describe excess mortality during the COVID-19 pandemic in Guatemala during 2020 by week, age, sex, and place of death.
Methods. We used mortality data from 2015 to 2020, gathered through the vital registration system of Guatemala. We calculated weekly mortality rates, overall and stratified by age, sex, and place of death. We fitted a generalized additive model to calculate excess deaths, adjusting for seasonality and secular trends and compared excess deaths to the official COVID-19 mortality count.
Results. We found an initial decline of 26% in mortality rates during the first weeks of the pandemic in 2020, compared with 2015 to 2019. These declines were sustained through October 2020 for the population younger than 20 years and for deaths in public spaces and returned to normal from July onward in the population aged 20 to 39 years. We found a peak of 73% excess mortality in mid-July, especially in the population aged 40 years or older. We estimated a total of 8036 excess deaths (95% confidence interval = 7935, 8137) in 2020, 46% higher than the official COVID-19 mortality count.
Conclusions. The extent of this health crisis is underestimated when COVID-19 confirmed death counts are used. (Am J Public Health. 2021;111(10): 1839–1846. https://doi.org/10.2105/AJPH.2021.306452)
The COVID-19 pandemic directly caused at least 2 million confirmed deaths worldwide during 2020. During the first months of the pandemic, the strongest mortality impacts occurred in England and Spain, with excess mortality of 37% and 38%, respectively, between mid-February and May 2020.1 However, the Latin American region has been considerably affected during the rest of the pandemic, despite having a much younger population compared with Europe.2 Fragmented health systems, wide social inequalities, and a high prevalence of chronic conditions may have contributed to the high COVID-19 toll in Latin America.3 Guatemala, one of the poorest countries in Latin America, reported its first COVID-19 case on March 13, 2020. In response, the Guatemalan government implemented several control measures such as mobility restrictions, stay-at-home orders, prohibition of alcohol consumption, and national lockdowns. These policies were subsequently revised in periods of 15 days and were tightened or loosened depending on the number of COVID-19 cases in the country.
Studying the impact of the COVID-19 pandemic by looking only at confirmed COVID-19 deaths provides an incomplete picture of the burden of the pandemic. First, confirmed death counts usually require laboratory confirmation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection,4 which has been limited in Guatemala.5 Second, COVID-19 may exacerbate other health conditions causing deaths that may not be classified as directly caused by COVID-19.6 Third, the disruptions to the provision of health services because of COVID-19 may cause a delay in the care of other conditions leading to an increase in mortality attributable to other causes.7 Fourth, measures to control COVID-19 (including lockdowns and other physical distancing measures) may aggravate conditions, especially those related to mental health8 and intimate partner violence.9 Last, there may also have been a decrease in other causes of death because of a decrease in other respiratory infections,10 mobility,11 homicides,12 and pollution.13
Excess mortality, which we define as the relative difference between observed mortality rates and a baseline mortality rate calculated from previous years, is a general measure of the impact of mortality crises like seasonal influenza or hurricanes.14 Excess mortality provides a better way to estimate the overall impact of the pandemic than confirmed COVID-19 deaths alone, which may be underascertained because of the presence of limited testing, indirect mortality effects, and changes in other environmental factors. To advance further preparedness, we aimed to describe excess mortality patterns in Guatemala during the COVID-19 pandemic in the period of March 13 to December 31, 2020.
METHODS
Guatemala is part of the Central American region, with a population of 16.9 million inhabitants. It ranks among the poorest countries in Latin America. To mitigate the COVID-19 pandemic, the Guatemalan government announced a number of public health measures on March 14, 2020, including the suspension of schools and sport activities and travel restrictions. These measures were further strengthened on March 16, including complete air travel bans and curfews, followed shortly after by restrictions to internal mobility and stricter lockdowns. These policies were loosened during early June, and the lockdowns and travel restrictions were lifted in September 2020, based on a local system of alerts using the number of COVID-19 cases and the test positivity ratio for each municipality.
Data Sources
We analyzed de-identified individual-level mortality data from the National Registry of Persons (RENAP, for Registro Nacional de Personas), the national vital registration system of Guatemala, from January 1, 2015, to December 31, 2020. RENAP is a centralized institution with national coverage that collects information about civil registration (births, deaths, marriages, divorces. and naturalization processes). RENAP provided data on date of death and registration, sex, age, nonstandardized causes of death, region (departamentos) of occurrence, and place of death (e.g., home, public spaces, hospital). These data did not include the deaths of infants younger than 1 year.
There is a known delay in death registration, as deaths are not registered immediately. To account for this, we estimated the delay in registration by comparing date of registration and date of occurrence. We found that 50% of deaths were registered within 1 week and 90% of them within 4 weeks after occurrence. See Appendix, Figures A‒D (available as supplements to the online version of this article at http://www.ajph.org) for more details on the analysis of delays in reporting. Based on this analysis, we used data on deaths reported up until February 28, 2021. This ensured that almost all deaths that occurred up to December 31, 2020, were included, even if registration was delayed, providing for a nearly complete picture of deaths in 2020. We conducted all of the analyses using the date of occurrence, categorized in epidemiological weeks.
We used population counts as denominators from the population projections calculated by the National Institute of Statistics.15 We also obtained the official number of confirmed COVID-19 deaths by week from the Ministry of Health of Guatemala (https://tablerocovid.mspas.gob.gt), defined as deaths of people who had a confirmed COVID-19 laboratory test.
Statistical Analysis
The main objective of this analysis was to describe excess mortality during the first calendar year of the COVID-19 pandemic in Guatemala and to explore temporal trends and patterns by age, sex, and place of death. We calculated weekly mortality counts by using standardized epidemiological weeks as defined by the Centers for Disease Control and Prevention. We also estimated crude weekly mortality rates, using population projections as denominators.
We defined excess mortality as the absolute difference in weekly crude mortality rate in 2020 compared with the average weekly mortality rate in 2015 to 2019 (mortality rate in 2020‒average mortality rate in 2015 to 2019). We also calculated the weekly mortality rate ratio (mortality rate in 2020/average mortality rate in 2015 to 2019) expressed as a percentage. We further stratified all the analyses by sex (male or female), place of death (home, hospital, public spaces, health centers, and other), and age groups (1–4, 5–19, 20–39, 40–59, 60–74, and ≥ 75 years).
We estimated years of life lost as a measure of the overall impact of the COVID-19 pandemic in Guatemala. For this, we summed over all residual life expectancies at each age of death. We obtained these from sex-specific abridged life tables for Guatemala for the 2015–2020 period produced by the 2019 Revision of the United Nations World Population Prospects. We then converted these to single-age life tables using penalized composite link model graduation,16 as implemented in the DemoTools R package (https://github.com/timriffe/DemoTools). For example, every death of a male aged 15 years meant losing 58.5 years of life, as this was the life expectancy for males aged 15 years in Guatemala for the 2015–2020 period.
To estimate the total number of excess deaths during 2020, we computed a smoothed estimate of expected death counts for each week of 2020 by fitting a negative binomial generalized additive model, as detailed in Basellini et al.17 This model takes into consideration variations in mortality within the year, by using week-specific coefficients, and secular trends, by using a smoothed time component that captures long-term mortality trends.17 We fitted this model using data from 2015 to 2019, and then predicted the expected number of deaths in each week of 2020, which we compared with the actual observed number of deaths. We then summed over the weekly excess deaths for the whole year to obtain an estimate (and 95% confidence interval [CI]) for the total excess mortality in 2020. As a sensitivity analysis, we fitted the initial baseline model using data for 2015 to 2017 and repeated the calculation of excess mortality in 2020. We also show more parsimonious estimates of excess mortality, where we calculated the expected number of deaths in 2020 by fitting a generalized linear model of the negative binomial family to the 2015–2019 yearly data with a linear coefficient for year.
All the analyses were performed in R version 4.0.3 using the tidyverse and mcgv packages (R Foundation, Vienna, Austria).
RESULTS
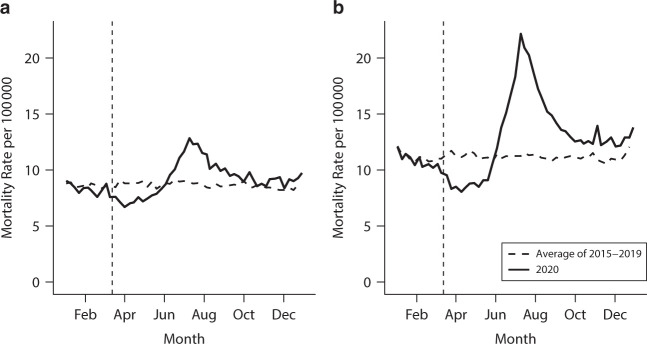
Starting at week 11 of 2020, when the first COVID-19 case was detected and the initial public health measures were implemented in Guatemala, there was a drop in all-cause mortality (Figure 1, Table 1, and Appendix, Figure E). The lowest mortality was in mid-April (week 15), with around 7.53 deaths per week per 100 000 inhabitants, as compared with an average of 9.96 deaths per week per 100 000 inhabitants in previous years. Starting in early May (week 19), mortality started increasing, reaching previous years’ levels in early June (week 22), and peaking in July (week 28), with a weekly mortality rate of 17.42 per 100 000, as compared with an average of 10.05 per 100 000 in previous years, a 73% relative mortality increase. From thereon, mortality decreased progressively, reaching an average of 10.87 deaths per 100 000 in October and December compared with 9.77 deaths per 100 000 in previous years, making for an 11% relative increase in mortality from October to December 2020. Overall, we found that there were 4 099 700 years of life lost in 2020, compared with an average of 3 731 446 in 2015 to 2019, resulting in an increase of 368 255 years of life lost, or a 9.9% relative increase.
FIGURE 1—
Weekly Crude Mortality Rate: Guatemala, January 2015‒ December 2020
Note. Vertical dashed line represents week 11, when the first case was detected in Guatemala. Line for 2015–2019 represents the average weekly mortality rate for that period.
TABLE 1—
Average Monthly Deaths, Overall, and by Sex, Age, and Place of Death: Guatemala, January 2015‒December 2020
| Year | Monthly Deaths, Thousands | Population, Millions | ||||||||||||
| Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov | Dec | |||
| Overall | 2015–2019 | 7.09 | 6.33 | 7.06 | 6.99 | 7.02 | 6.90 | 7.19 | 7.01 | 6.77 | 7.04 | 7.09 | 6.33 | 16.1 |
| 2020 | 7.29 | 6.51 | 6.37 | 5.65 | 6.34 | 8.97 | 12.15 | 9.87 | 8.28 | 8.02 | 7.29 | 6.51 | 16.9 | |
| Sex | ||||||||||||||
| Male | 2015–2019 | 3.97 | 3.51 | 3.93 | 3.88 | 3.88 | 3.80 | 3.97 | 3.90 | 3.76 | 3.91 | 3.97 | 3.51 | 7.93 |
| 2020 | 4.10 | 3.63 | 3.46 | 3.03 | 3.41 | 5.28 | 7.48 | 5.90 | 4.74 | 4.59 | 4.10 | 3.63 | 8.30 | |
| Female | 2015–2019 | 3.12 | 2.82 | 3.13 | 3.10 | 3.13 | 3.10 | 3.21 | 3.10 | 3.00 | 3.13 | 3.12 | 2.82 | 8.16 |
| 2020 | 3.19 | 2.88 | 2.91 | 2.63 | 2.93 | 3.69 | 4.67 | 3.96 | 3.54 | 3.43 | 3.19 | 2.88 | 8.56 | |
| Age, y | ||||||||||||||
| 1–4 | 2015–2019 | 0.15 | 0.16 | 0.21 | 0.23 | 0.25 | 0.24 | 0.24 | 0.22 | 0.19 | 0.18 | 0.15 | 0.16 | 1.50 |
| 2020 | 0.13 | 0.13 | 0.12 | 0.11 | 0.11 | 0.14 | 0.14 | 0.13 | 0.11 | 0.11 | 0.13 | 0.13 | 1.51 | |
| 5–19 | 2015–19 | 0.31 | 0.28 | 0.34 | 0.32 | 0.34 | 0.32 | 0.34 | 0.32 | 0.32 | 0.33 | 0.31 | 0.28 | 5.41 |
| 2020 | 0.31 | 0.25 | 0.23 | 0.21 | 0.24 | 0.23 | 0.25 | 0.28 | 0.25 | 0.25 | 0.31 | 0.25 | 5.41 | |
| 20–39 | 2015–2019 | 0.98 | 0.86 | 0.96 | 0.93 | 0.97 | 0.93 | 1.01 | 0.96 | 0.94 | 0.95 | 0.98 | 0.86 | 5.24 |
| 2020 | 0.89 | 0.85 | 0.73 | 0.65 | 0.78 | 0.92 | 1.10 | 0.98 | 0.92 | 0.95 | 0.89 | 0.85 | 5.61 | |
| 40–59 | 2015–2019 | 1.28 | 1.13 | 1.27 | 1.25 | 1.25 | 1.24 | 1.25 | 1.24 | 1.18 | 1.26 | 1.28 | 1.13 | 2.42 |
| 2020 | 1.32 | 1.15 | 1.18 | 1.05 | 1.31 | 2.04 | 2.70 | 2.06 | 1.64 | 1.57 | 1.32 | 1.15 | 2.67 | |
| 60–74 | 2015–2019 | 1.50 | 1.34 | 1.49 | 1.46 | 1.45 | 1.45 | 1.48 | 1.46 | 1.42 | 1.45 | 1.50 | 1.34 | 0.82 |
| 2020 | 1.64 | 1.51 | 1.54 | 1.36 | 1.61 | 2.49 | 3.67 | 2.74 | 2.27 | 2.07 | 1.64 | 1.51 | 0.91 | |
| ≥ 75 | 2015–2019 | 2.24 | 2.00 | 2.13 | 2.11 | 2.05 | 2.03 | 2.13 | 2.09 | 2.02 | 2.17 | 2.24 | 2.00 | 0.32 |
| 2020 | 2.44 | 2.05 | 2.09 | 1.90 | 1.92 | 2.74 | 3.87 | 3.26 | 2.71 | 2.69 | 2.44 | 2.05 | 0.36 | |
| Place of death | ||||||||||||||
| Home | 2015–2019 | 4.45 | 3.98 | 4.37 | 4.28 | 4.27 | 4.24 | 4.34 | 4.27 | 4.17 | 4.33 | 4.45 | 3.98 | NA |
| 2020 | 4.58 | 3.96 | 4.02 | 3.72 | 4.14 | 5.73 | 7.88 | 6.51 | 5.59 | 5.33 | 4.58 | 3.96 | NA | |
| Hospital | 2015–2019 | 2.01 | 1.83 | 2.08 | 2.12 | 2.15 | 2.05 | 2.21 | 2.15 | 2.02 | 2.07 | 2.01 | 1.83 | NA |
| 2020 | 2.18 | 2.05 | 1.96 | 1.63 | 1.84 | 2.81 | 3.80 | 2.86 | 2.25 | 2.22 | 2.18 | 2.05 | NA | |
| Health center | 2015–2019 | 0.03 | 0.03 | 0.03 | 0.03 | 0.04 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | NA |
| 2020 | 0.03 | 0.03 | 0.02 | 0.02 | 0.02 | 0.03 | 0.03 | 0.03 | 0.02 | 0.02 | 0.03 | 0.03 | NA | |
| Public spaces | 2015–2019 | 0.46 | 0.39 | 0.45 | 0.44 | 0.43 | 0.43 | 0.47 | 0.43 | 0.43 | 0.46 | 0.46 | 0.39 | NA |
| 2020 | 0.37 | 0.33 | 0.27 | 0.19 | 0.22 | 0.28 | 0.29 | 0.33 | 0.29 | 0.34 | 0.37 | 0.33 | NA | |
| Other | 2015–2019 | 0.13 | 0.11 | 0.14 | 0.12 | 0.14 | 0.14 | 0.14 | 0.13 | 0.13 | 0.15 | 0.13 | 0.11 | NA |
| 2020 | 0.13 | 0.13 | 0.11 | 0.10 | 0.12 | 0.13 | 0.14 | 0.14 | 0.13 | 0.11 | 0.13 | 0.13 | NA | |
Note. NA = not applicable. 2015–2019 refers to the average monthly death count or yearly population from 2015 to 2019.
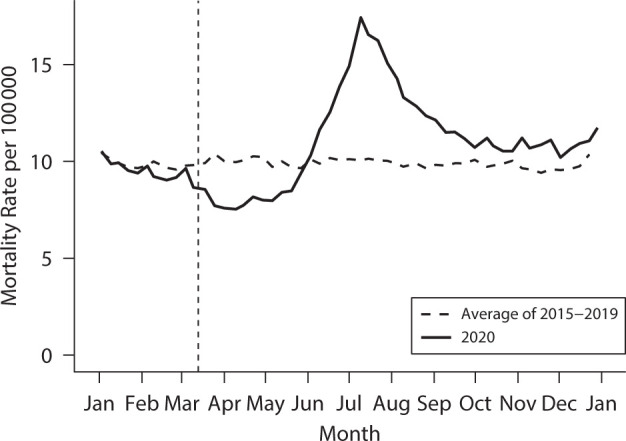
We also observed a similar shape of weekly mortality rates for females and males, with some differences (Figure 2, Table 1, and Appendix, Figure F). First, mortality rates have been higher in males, with a weekly mortality rate of 11.17 per 100 000 inhabitants in the 2015–2019 period, as compared with 8.65 per 100 000 in females. Second, the decrease in mortality during weeks 11 through 21 was stronger in males, with mortality rates dropping to 8.80 per 100 000 inhabitants, compared with 11.29 per 100 000 inhabitants in previous years, a sharper drop than for females (7.36 per 100 000 inhabitants, compared with 8.75 in previous years). Third, the increase in mortality rates was much steeper for men than for women. During week 28, the weekly mortality rate was 22.16 per 100 000 inhabitants in males and 12.84 per 100 000 inhabitants in females, compared with 11.25 and 8.89 in previous years, representing a relative increase of 96.9% and 44.4%, respectively.
FIGURE 2—
Weekly Mortality Rate Among (a) Women and (b) Men: Guatemala, January 2015‒December 2020
Note. Vertical dashed line represents week 11, when the first case was detected in Guatemala. Line for 2015–2019 represents the average weekly mortality rate for that period.
We observed distinct weekly mortality patterns by age group (Table 1 and Appendix, Figures G and H). First, among age groups 1 to 4 years and 5 to 19 years, we observed a consistent drop in mortality from week 11 onward, and this drop has continued through the end of the study period. Specifically, during 2020, we observed an average weekly mortality rate of 1.88 and 1.05 per 100 000 inhabitants in people aged 1 to 4 and 5 to 19 years, respectively, compared with an average of 3.03 and 1.35 per 100 000 inhabitants in 2015 to 2019 (38% and 22% relative drop in mortality). Mortality patterns among people aged 20 to 39 years followed an initial decline in mortality from week 11 to week 22, and a return to previous years’ average from thereon. Lastly, age groups 40 to 59, 60 to 74, and 75 years or older saw an initial decline in mortality from week 11 to week 21, followed by a large increase. Specifically, we observed a 49.4%, 66.9%, and 36.4% increase in relative mortality from week 21 onward for those age groups, respectively.
We observed distinct patterns by place of death in the mortality rates during 2020 (Table 1 and Appendix, Figures I and J). First, deaths in public spaces, such as streets or parks, declined at week 11 and persisted at lower levels than previous years. Second, deaths at home and in hospitals saw an initial decline from week 11 to week 21, with a 13.8% and 22.3% drop in mortality during that period, compared with previous years. Third, there was a large increase in deaths at home and in hospitals from weeks 22 to 52, with an excess mortality rate ratio of 34.4% and 20.5% for deaths at home and in hospitals, respectively. The higher mortality rates were found typically at home, followed by deaths in hospitals, public spaces, and health centers.
Figure 3 and Appendix, Figure K, show the results of the generalized additive model to estimate the number of excess deaths after considering seasonality and secular trends. Specifically, we found an initial mortality decline of 26% in late March, followed by a peak increase of 73% in mid-July. Compared with official confirmed COVID-19 deaths, we found a higher initial count of confirmed deaths (given that overall mortality was declining at this point), followed by a large increase in all-cause excess mortality that was higher than the confirmed death count. Compared with mortality between 2015 and 2019, we found that Guatemala had experienced a total of 8036 excess deaths (95% CI = 7935, 8137) in 2020, which is higher than the 5487 confirmed COVID-19 deaths officially reported. This means that excess mortality in Guatemala during the COVID-19 pandemic was 46.4% higher (95% CI = 44.6%, 48.3%) than the official death count. Alternative model specifications rendered similar estimates (Appendix, Table A), and the model fitted using 2015–2017 data showed a good fit to 2018–2019 data (Appendix, Figure L).
FIGURE 3—
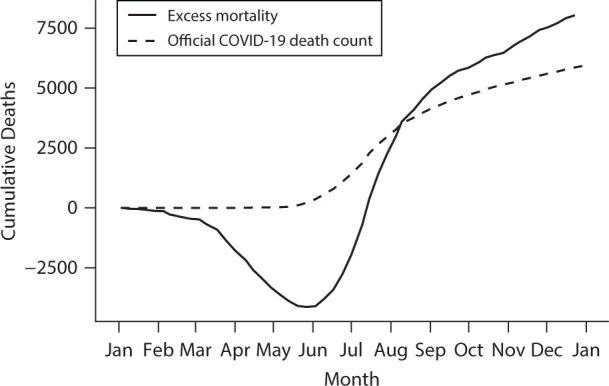
Cumulative Excess Mortality Versus Official COVID-19 Mortality Count: Guatemala, 2020
Note. Vertical dashed line represents week 11, when the first case was detected in Guatemala. Line for 2015–2019 represents the average weekly mortality rate for that period.
DISCUSSION
In this study examining mortality patterns in Guatemala during the COVID-19 pandemic, we found that by December 31, 2020, Guatemala had experienced a total of approximately 8000 excess deaths, 46% higher than the official confirmed COVID-19 death count of 5487. However, this overall number obscures 4 distinct patterns. First, we observed an initial decline in mortality from the date that the first public health measures were implemented until early June 2020. This was followed by a sharp increase in mortality, reaching 73% higher mortality compared with previous years. Second, while excess mortality affected both sexes, both the decline and the subsequent increase in mortality were steeper among men. Third, we observed a consistent lower mortality among Guatemalans younger than 20 years that lasted through the entire study period, while people aged 40 years or older saw a mortality peak during July. Lastly, we found that consistent with previous years, most deaths occurred at home, followed by hospitals, and these locations saw the highest increases in mortality, both relative and absolute. Deaths in public spaces declined and stayed low during the entire period.
These results are consistent with preliminary reports on excess mortality in Guatemala.18 Other studies have reported similar trends in other countries in Latin America19,20 and elsewhere,21,22 including large differences in COVID-19 mortality by age.23 Mortality differences by sex, with higher mortality among males, have been reported in other settings24 but are not universal.25 A deeper understanding of the sex differentials in COVID-19 mortality, including differences in sex biology or gendered behaviors, or differences in access to care or underlying diseases by either sex or gender, should be explored in future studies.
The length of the period of decreased mortality, spanning 3 months, is a unique finding of our study. This decline is unlikely to be caused by delays in registration, as we utilized mortality data registered up until February 28, 2021, allowing for a several month period of delay in registration. Although we did not have information on cause of death, it seems plausible that initial declines in mortality may be related to reductions in risk factors that account for main drivers of death in Guatemala. This reduction could be caused by many of the public health recommendations or measures introduced to mitigate the COVID-19 pandemic. For example, both reductions in air pollution26 and increases in social distancing10 may have an impact on other respiratory diseases, the second cause of death among children younger than 5 years in Guatemala.27 In the case of adolescents and young adults, and given the overall high levels of mortality from homicides and other injuries in Guatemala in previous years,28 a decline in these causes may be driving these patterns. Other Latin American countries have reported a reduction in homicides, traffic injuries, and other external causes of death during the pandemic.29 Changes in mobility could explain the same reduction in mortality in Guatemala, as there was a sharp decline in traffic (see Appendix, Figure M, for trends in mobility to transit stations and residences in Guatemala, as obtained from Google Mobility Reports). In summary, given the low case fatality of COVID-19 among children and youths,30 the potential reduction in factors driving respiratory deaths (i.e., air pollution and social distancing measures), and the potential reductions in external causes of death (the main cause of death among children and adolescents31), these reductions in mortality are not surprising.
By mid-May, the decrease in mortality was reverted, overlapping with the time when the official number of COVID-19 deaths started to increase. The highest mortality occurred at home compared with hospitals, even before the current pandemic. This phenomenon brings to the attention potential barriers such as access to health care and limited hospital capacity.32 This could be exacerbated because of restricted mobility policies including prohibition of public transportation and limited number of ambulances. Restrictions to mobility, along with lockdowns, may have affected mortality in public spaces, which stayed low during the entire study period. We also found that individuals aged 40 to 59 years were the youngest group with a strong excess mortality, a relatively younger population compared with other settings.21,33 This difference may have arisen because of a higher prevalence of chronic diseases and limited access to health services that might interrupt the access to chronic disease treatment.
Limitations
Our study had some limitations. First, RENAP has a delay in registration, which we accounted for by including 2 extra full months of death registration data (January and February 2021), to capture deaths that occurred in 2020 but were registered with a delay. However, we cannot rule out longer delayed times toward the end of the study period, or differential delays by age, sex, or place of death. Appendix Figures A through D show registration delays over time, and by age, sex, and place of death, suggesting differences at the beginning of the pandemic.
Second, while the coverage of death counts in Guatemala is generally high,34 we cannot rule out an increase in undercounting35 during the pandemic. However, if undercounting was to have increased during the pandemic, our results would be representing a conservative estimate of excess mortality.
Third, RENAP does not include data for deaths among infants younger than 1 year. Given the high infant mortality of Guatemala36 compared with other Latin American countries, this precludes us from showing the complete mortality picture during the pandemic. While mortality among children stayed low during the entire period, we cannot rule out increases in mortality among infants, especially neonatal deaths, which are highly affected by quality of health care and early access to health care, which could have been delayed because of mobility restrictions.
Fourth, we could not analyze data by cause of death, because RENAP does not codify causes of death, and this is a resource-intensive process that limits timely analyses during the pandemic. The process of coding causes of death is done by the National Institute of Statistics, which usually releases these data a year later.
Fifth, toward the end of 2020, hurricanes Iota and Eta impacted Guatemala, causing at least 60 confirmed deaths. This could cause an overestimation of the excess mortality from the COVID-19 pandemic during the few last months of 2020.
Lastly, the usual caveats about the calculation of years of life lost, including decisions about discounting of years of life lost depending on age and the choice of a reference life table, apply here.37
Conclusions
In summary, we found that the COVID-19 pandemic has created a mortality crisis in Guatemala, similar to other countries in the world. The extent of this crisis is underestimated when confirmed COVID-19 death counts are used, as we found that excess mortality was 46% higher than confirmed counts. We also identified specific age-, sex-, and place-specific patterns of death, highlighting the vulnerability of middle-aged adults (40‒59 years). As mitigation measures are lifted, and vaccine roll-out continues, consideration must be paid to this group, which is also highly exposed from their economic participation. Lastly, gaining a better understanding of deaths at home, including addressing potential barriers to accessing health care, may provide clues to mitigation strategies.
Public Health Implications
In Guatemala, high vulnerability was found not only in the elderly but also in middle-aged adults (40‒59 years), who are also highly exposed to COVID-19 because of their active participation in the economy and high prevalence of noncommunicable chronic diseases. Key stakeholders need to consider middle-aged adults with noncommunicable chronic diseases as priority for vaccination purposes and to plan a national chronic disease survey to quantify the prevalence of noncommunicable chronic diseases in this population.
ACKNOWLEDGMENTS
U. Bilal and K. Martinez-Folgar were supported by the Office of the Director of the National Institutes of Health under award DP5OD26429.
This work was presented at the Society for Epidemiologic Research Virtual Conference in the fall 2020 edition, November 3, 2020.
The authors thank Carlos Mendoza from DIALOGOS, a Guatemalan think tank, and Bernardo Arevalo, party leader in Congress of Movimiento Semilla in Guatemala, for their help in obtaining the data from the National Registry of Persons.
Note. The funding source had no role in the analysis, writing, or decision to submit the article.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This research was deemed exempt from institutional board review under 45 CF 46.104(d)(4)(ii).
Footnotes
See also Aburto, p. 1721.
REFERENCES
- 1. Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. . 2020;92(6):548–551. doi: 10.1002/jmv.25722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nepomuceno MR, Acosta E, Alburez-Gutierrez D, et al. Besides population age structure, health and other demographic factors can contribute to understanding the COVID-19 burden. Proc Natl Acad Sci U S A. . 2020;117(25):13881–13883. doi: 10.1073/pnas.2008760117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Glassman A, Gaziano TA, Buendia CPB, de Aguiar FCG. Confronting the chronic disease burden in Latin America and the Caribbean. Health Aff (Millwood). . 2010;29(12):2142–2148. doi: 10.1377/hlthaff.2010.1038. [DOI] [PubMed] [Google Scholar]
- 4. Tang Y, Schmitz JE, Persing DH, Stratton CW. Laboratory diagnosis of COVID-19: current issues and challenges. J Clin Microbiol. . 2020;58(6):e00512–e00520. doi: 10.1128/JCM.00512-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prensa Libre. Coronavirus: as cases go up there is still little evidence [in Spanish]. Available at: https://www.prensalibre.com/guatemala/comunitario/coronavirus-mientras-casos-suben-aun-hay-pocas-pruebas
- 6. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. . 2020;180(7):934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rosenbaum L. The untold toll—the pandemic’s effects on patients without COVID-19. N Engl J Med. . 2020;382(24):2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 8.Brennan GK. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(7):e41. doi: 10.1016/S2215-0366(20)30226-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calderon-Anyosa RJC, Bilal U, Kaufman JS.Variation in non-external and external causes of death in Peru in relation to the COVID-19 lockdown Yale J Biol Med. 202194123–40.. [PMC free article] [PubMed] [Google Scholar]
- 10. Liu J, Zhang L, Yan Y, et al. Excess mortality in Wuhan city and other parts of China during the three months of the COVID-19 outbreak: findings from nationwide mortality registries. BMJ. . 2021;372:n415. doi: 10.1136/bmj.n415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Badr HS, Du H, Marshall M, Dong E, Squire MM, Gardner LM. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect Dis. . 2020;20(11):1247–1254. doi: 10.1016/S1473-3099(20)30553-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Calderon-Anyosa RJC, Kaufman JS. Impact of COVID-19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. Prev Med. . 2021;143:106331. doi: 10.1016/j.ypmed.2020.106331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kephart JL, Avila-Palencia I, Bilal U, Gouveia N, Caiaffa WT, Diez Roux AV. COVID-19, ambient air pollution, and environmental health inequities in Latin American cities. J Urban Health. . 2021;98(3):428–432. doi: 10.1007/s11524-020-00509-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Spagat M, van Weezel S. Excess deaths and Hurricane María. Popul Environ. . 2020;42(1):79–94. doi: 10.1007/s11111-020-00341-x. [DOI] [Google Scholar]
- 15.Instituto Nacional de Estadistica. 2020. https://www.ine.gob.gt/ine/proyecciones/?fbclid=IwAR3o2odcXRFqV_TujkxaS4uBYseLk_2swvX6df82bbwpPx-_hqV2ppbbOwE
- 16. Rizzi S, Gampe J, Eilers PHC. Efficient estimation of smooth distributions from coarsely grouped data. Am J Epidemiol. . 2015;182(2):138–147. doi: 10.1093/aje/kwv020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Basellini U, Alburez-Gutierrez D, Del Fava E, et al. Linking excess mortality to mobility data during the first wave of COVID-19 in England and Wales. SSM Popul Health. . 2021;14:100799. doi: 10.1016/j.ssmph.2021.100799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chavez O, Barrera A, Slowing K. Excess mortality during the first wave of COVID-19 in Guatemala. La Revista Análisis de la Realidad Nacional. . 2020;9(193):59–80. http://ipn.usac.edu.gt/wp-content/uploads/2020/10/IPN-RD-193.pdf [Google Scholar]
- 19.Matus A, Matus M, Cabello F, Sierra E.2020. arXiv. https://arxiv.org/abs/2006.06447
- 20. Cevallos-Valdiviezo H, Vergara-Montesdeoca A, Zambrano-Zambrano G. Measuring the impact of the COVID-19 outbreak in Ecuador using preliminary estimates of excess mortality, March 17–October 22, 2020. Int J Infect Dis. . 2021;104:297–299. doi: 10.1016/j.ijid.2020.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vestergaard LS, Nielsen J, Richter L, et al. Excess all-cause mortality during the COVID-19 pandemic in Europe—preliminary pooled estimates from the EuroMOMO network, March to April 2020. Euro Surveill. . 2020;25(26):2001214. doi: 10.2807/1560-7917.ES.2020.25.26.2001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Trias-Llimós S, Riffe T, Bilal U. Monitoring life expectancy levels during the COVID-19 pandemic: example of the unequal impact of the first wave on Spanish regions. PLoS One. . 2020;15(11):e0241952. doi: 10.1371/journal.pone.0241952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dowd JB, Andriano L, Brazel DM, et al. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc Natl Acad Sci U S A. . 2020;117(18):9696–9698. doi: 10.1073/pnas.2004911117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bhopal SS, Bhopal R. Sex differential in COVID-19 mortality varies markedly by age. Lancet. . 2020;396(10250):532–533. doi: 10.1016/S0140-6736(20)31748-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dehingia N, Raj A. Sex differences in COVID-19 case fatality: do we know enough? Lancet Glob Health. . 2021;9(1):e14–e15. doi: 10.1016/S2214-109X(20)30464-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. To T, Viegi G, Cruz A, et al. A global respiratory perspective on the COVID-19 pandemic: commentary and action proposals. Eur Respir J. . 2020;56(1):2001704. doi: 10.1183/13993003.01704-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Castro F, Benavides Lara A, Garcés A, et al. Under-5 mortality in Central America: 1990–2016. Pediatrics. . 2021;147(1):e2020003442. doi: 10.1542/peds.2020-003442. [DOI] [PubMed] [Google Scholar]
- 28. Sanford V. From genocide to feminicide: impunity and human rights in twenty-first century Guatemala. J Hum Rights. . 2008;7(2):104–122. doi: 10.1080/14754830802070192. [DOI] [Google Scholar]
- 29.Calderon-Anyosa RJC, Kaufman JS.2020. medRxiv. 10.1101/2020.07.11.20150193 [DOI]
- 30. Zhou M-Y, Xie X-L, Peng Y-G, et al. From SARS to COVID-19: what we have learned about children infected with COVID-19. Int J Infect Dis. . 2020;96:710–714. doi: 10.1016/j.ijid.2020.04.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Adeloye D, Bowman K, Chan KY, Patel S, Campbell H, Rudan I. Global and regional child deaths due to injuries: an assessment of the evidence. J Glob Health. . 2018;8(2):021104. doi: 10.7189/jogh.08.021104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Garcia-Subirats I, Vargas I, Mogollón-Pérez AS, et al. Barriers in access to healthcare in countries with different health systems. A cross-sectional study in municipalities of central Colombia and north-eastern Brazil. Soc Sci Med. . 2014;106:204–213. doi: 10.1016/j.socscimed.2014.01.054. [DOI] [PubMed] [Google Scholar]
- 33. Stang A, Standl F, Kowall B, et al. Excess mortality due to COVID-19 in Germany. J Infect. . 2020;81(5):797–801. doi: 10.1016/j.jinf.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization. 2018. https://www.who.int/healthinfo/statistics/LT_method.pdf?ua=1&ua=1
- 35. Peralta A, Benach J, Borrell C, et al. Evaluation of the mortality registry in Ecuador (2001‒2013)—social and geographical inequalities in completeness and quality. Popul Health Metr. . 2019;17(1):3. doi: 10.1186/s12963-019-0183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Restrepo-Méndez MC, Barros AJD, Requejo J, et al. Progress in reducing inequalities in reproductive, maternal, newborn, and child health in Latin America and the Caribbean: an unfinished agenda Rev Panam Salud Publica. 20153819–16.. [PubMed] [Google Scholar]
- 37. Bonneux L. How to measure the burden of mortality? J Epidemiol Community Health. . 2002;56(2):128–131. doi: 10.1136/jech.56.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]