Abstract
Background
The symptoms of coronavirus disease 2019, caused by the novel severe acute respiratory syndrome coronavirus 2, were originally assumed to be mainly respiratory. With increasing knowledge, however, it turned out that the spectrum of complaints varies broadly with age and concomitant diseases. While many neurological symptoms were reported in the context of the disease, ranging from permanent fatigue to recurrent headaches and concentration disturbance, treatment approaches are still in development. This case discusses a possible treatment approach with immunoglobulin therapy and its outcomes.
Case presentation
We present the case of a 56-year-old Caucasian female patient who, following coronavirus disease 2019, developed peripheral sensory and autonomic disturbances that fell within subacute demyelinating neuropathy. Because a significant improvement in symptoms as well as in the results of clinical and electrophysiological examination was reported after immunoglobulin therapy, long-term therapy does not appear to be necessary.
Conclusion
Given the significant subjective and objective improvement reported, this case provides additional evidence that immunoglobulin therapy can be considered in post-coronavirus disease 2019 syndrome.
Keywords: COVID-19, Neuropathy, Post-COVID-19 syndrome, Case report
Background
The disease caused by the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is known as coronavirus disease 2019 (COVID-19). The symptoms were originally assumed to be mainly respiratory. With increasing knowledge, however, it turned out that the spectrum of complaints varies broadly with age and concomitant diseases. Mild courses, similar to a cold, up to severe disease with fatal outcomes are possible. While many nonrespiratory symptoms were mentioned in the context of the disease [1], neurological symptoms reported range from permanent fatigue, recurrent headaches, and concentration disturbance to polyneuropathy-related complaints [2]. This case reports various neurological symptoms in the postinfectious phase that are mostly attributed to an autoimmune mechanism [3] and discusses the use of immunoglobulin therapy as a treatment approach.
Case presentation
A 56-year-old Caucasian female patient presented with polyneuropathy-related complaints that manifested directly after a quarantine for a COVID-19 infection. At the time of admission, about a month after contracting the disease, the patient showed a mild viral load that was attributed to dead viral remnants. Although the previously reported respiratory symptoms of the disease had regressed, the patient reported painful abnormal sensations on the hands and feet with symmetrical acral distribution, which she described as the sensation of cold water and “1000 pinpricks.” In the course of a few days, a changed sense of touch that affected the patient’s gait was noticed distally on the legs. She felt insecure climbing stairs, with no definite paresis but rather a general weakness. No metabolic diseases were reported other than substituted hypothyroidism.
On clinical examination, the patient was alert and fully oriented with normal cranial nerves. No signs of ataxia or paresis were found other than a positive Phalen test. Muscle reflexes of the upper extremities as well as the patellar reflex were exaggerated, while the Achilles reflex was weak on both sides with no pyramidal signs. Distally symmetrical hypoesthesia on the hands and feet as well as pallhypesthesia on the metatarsophalangeal joint and the malleolus medialis on both sides was reported.
Investigations
Electrophysiological examination of peripheral nerves revealed demyelinating changes consistent with acute/chronic inflammatory demyelinating polyneuropathy given the course of time (less than 8 weeks at the time). Nerve ultrasound showed thickened nerve roots and corroborated the suspicion of immune-mediated genesis of the polyneuropathy. Involvement of the autonomic nervous system was also detected using autonomic testing.
For further investigation, a lumbar puncture was carried out and showed a discrete albuminocytological dissociation that supported the suspected diagnosis. This was followed by magnetic resonance imaging of the cervical spine to clarify the broadened reflexes. However, no spinal cord affection was found.
Treatment
With a normal level of IgA, a therapeutic attempt was carried out with a dose of 0.4 g/kg body weight of immunoglobulin on five consecutive days with thrombosis prophylaxis using 40 mg enoxaparin sodium and rheological therapy. Apart from a slight headache, no side effects were reported. Already during the therapy, the patient noticed a slight improvement in the symptoms at rest. However, the symptoms flared up again with exertion.
Outcome and follow-up
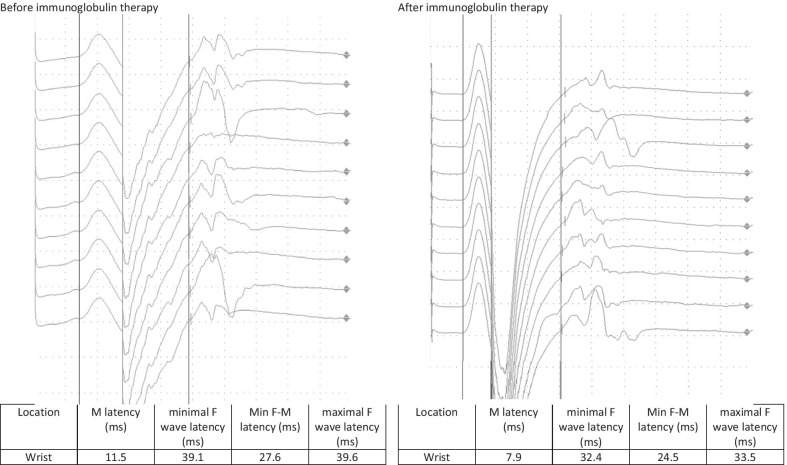
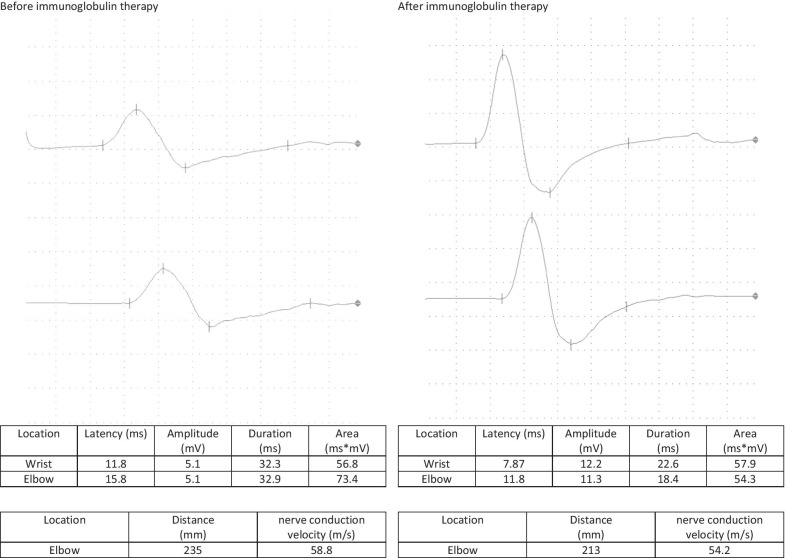
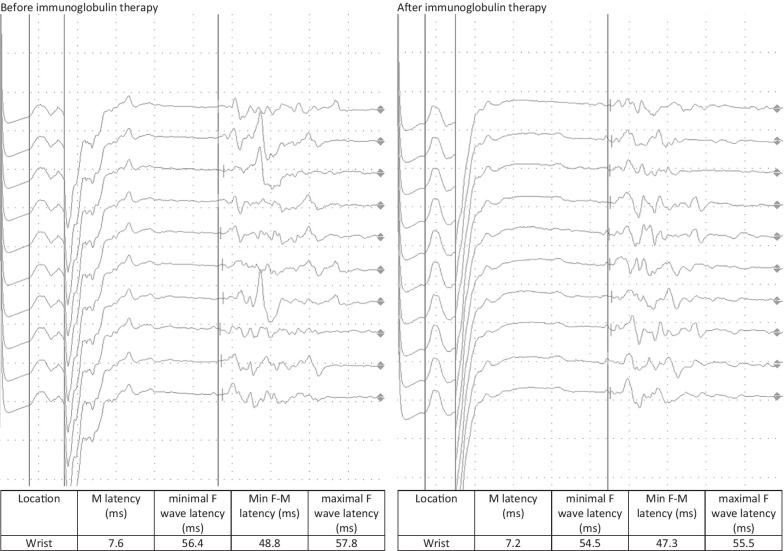
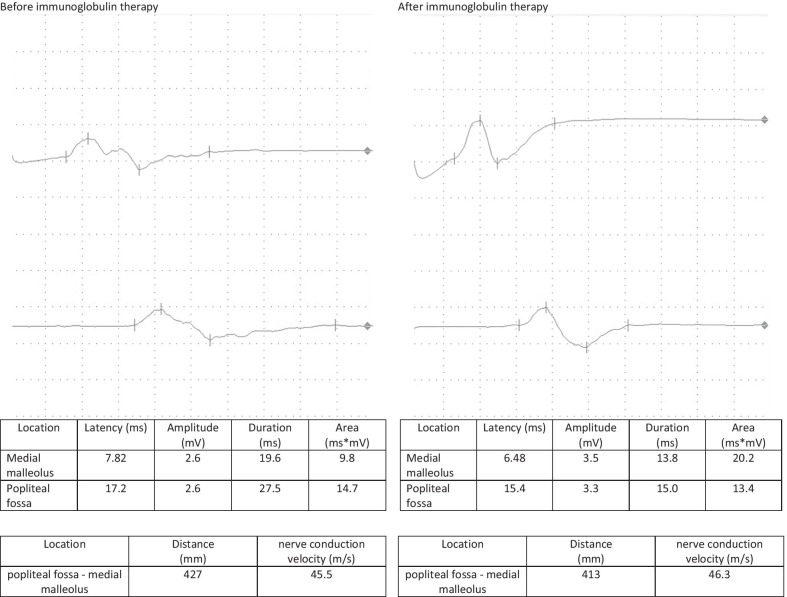
A follow-up appointment for clinical and electrophysiological follow-up was carried out after 4 weeks. The patient reported a headache for 5 days after the administration of the immunoglobulin therapy followed by a significant improvement in the complaints, especially with regard to the hypoesthesia and gait, while only minimal residual hypoesthesia at the tips of fingers, toes, and the nose persisted. The sensorimotor demyelinating polyneuropathy continued to improve on electrophysiological examination, with the electrophysiological criteria of chronic inflammatory demyelinating polyneuropathy no longer being fulfilled. A second dose of 90 g of immunoglobulin was administered without any complications (Figs. 1, 2, 3, 4).
Fig. 1.
F-wave of the right median nerve before and after immunoglobulin therapy
Fig. 2.
Nerve conduction velocity of the right median nerve before and after immunoglobulin therapy
Fig. 3.
F-wave of the right tibial nerve before and after immunoglobulin therapy
Fig. 4.
Nerve conduction velocity of the right tibial nerve before and after immunoglobulin therapy
Discussion
This report presents a case of a peripheral sensory and autonomic disturbance with demyelinating changes following COVID-19 disease. The symptoms as well as the electrophysiological changes were attributed to a postinfectious immune-mediated process [4], which was recently reported in COVID-19 patients with varying symptoms [1]. However, the exact mechanism of this autoimmune reaction as a trigger of this phenomenon [3] as well as the mechanism of the sensory disturbances themselves, in terms of being a neurofibrillary disorder or an acute/chronic inflammatory myeloid disorder, requires more research [4, 5].
Although the symptoms showed significant regression after the immunoglobulin therapy, it was not possible in the absence of clear guidelines to decide whether to continue the immunoglobulin therapy. This was left to be decided in light of the clinical findings in the course of the disease. At the time, long-term immunoglobulin therapy did not appear to be necessary.
Conclusion
This case provides additional evidence that immunoglobulin therapy can to be considered in post-COVID-19 syndrome given the significant subjective and objective improvement reported. In this regard, a good prognosis is to be expected.
Learning points/take-home messages
Chronic neurological symptoms are being frequently reported in the context of post-COVID-19 syndrome.
Sensory polyneuropathy can occur in the postinfectious phase and is attributed to an immune-mediated processes. Immunoglobulin therapy can be considered as a treatment option with an expected good prognosis.
Patient’s perspective
The COVID-19-disease and the quarantine were for me, on the personal as well as on the family level, a bitter experience. It was however more shocking when the neurological symptoms occurred after a while and I was told of their relationship to the disease, so that it seemed possible at that time that the symptoms would persist and I would always have something to remind me of this experience. Everything was new for me as well as for the physicians treating me. Every question, especially regarding the long-term treatment, needed time and further reading.
The first round of the immunotherapy went slow, while I barely noticed anything other than a headache. I though at the beginning while laying down in my hospital bed that me symptoms were getting better. However, they proved my wrong with the slightest effort I did.
The same continued after discharge. However, five days later I started noticing something. The painful numbness on my hands and toes as well as on my nose started to take a turn one day after the other. I could also walk better. Today, a month later I only have minimal numbness on the tip of my nose, which I hope it would go also away with time.
Acknowledgments
None.
Authors’ contributions
AS: acquisition of data, interpretation of data, drafting the manuscript, corresponding author. RJ: interpretation of data, drafting the manuscript. ST: analysis of data. FH: revision. MS: final revision. All authors read and approved the final manuscript.
Funding
No funding was required.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The patient gave consent after a detailed discussion and explanation of the purpose and value of the case report. No ethical approval was required.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lai CC, Ko WC, Lee PI, Jean SS, Hsueh PR. Extra-respiratory manifestations of COVID-19. Int J Antimicrob Agents. 2020;56(2):106024. doi: 10.1016/j.ijantimicag.2020.106024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Correia AO, Feitosa PWG, Moreira JLS, Nogueira SÁR, Fonseca RB, Nobre MEP. Neurological manifestations of COVID-19 and other coronaviruses: a systematic review. Neurol Psychiatry Brain Res. 2020;37:27–32. doi: 10.1016/j.npbr.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cañas CA. The triggering of post-COVID-19 autoimmunity phenomena could be associated with both transient immunosuppression and an inappropriate form of immune reconstitution in susceptible individuals. Med Hypotheses. 2020;145:110345. doi: 10.1016/j.mehy.2020.110345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoser B, Baum P, Boentert M, et al. SARS-CoV-2/COVID-19 und neuromuskuläre Erkrankungen: Bestandsaufnahme der DGN (Deutsche Gesellschaft für Neurologie) Kommission Motoneuron- und neuromuskuläre Erkrankungen [SARS-CoV-2/COVID-19 and neuromuscular disorders] DGNeurologie. 2020 doi: 10.1007/s42451-020-00198-2. [DOI] [Google Scholar]
- 5.Novak P. Post COVID-19 syndrome associated with orthostatic cerebral hypoperfusion syndrome, small fiber neuropathy and benefit of immunotherapy: a case report. eNeurologicalSci. 2020;21:100276. doi: 10.1016/j.ensci.2020.100276. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.