Abstract
Background:
Social support, which is partly emotional support, is associated with adherence to colorectal cancer (CRC) treatment, quality of life, and survival. We hypothesized that the needs, sources, and availability of emotional support would vary by race and income among CRC patients and sought to quantify the emotional support and the perceived adequacy of support reported by patients.
Methods:
We surveyed CRC patients from Detroit and Georgia Surveillance, Epidemiology and End Results registries about the quantity and quality of emotional support received from different sources. We tested differences using the chi-square test, t-tests, and logistic regression.
Results:
There were 1909 patients who met inclusion criteria and 1301 (68%) completed surveys. Among respondents, 68% were white, 25% black, and 7% other. Black patients were more likely to be female and younger and reported lower annual income and education. Patients reported high support from several sources. Among those with a spouse/partner (58%), 95% reported high levels of support; however, older, black, female, or lower income patients were less likely to have spouses/partners (P < .001). Patients also endorsed high support from family (88.6%), important others (82.9%), and clinicians (71.3%). Black patients were less likely than white patients to report support that was “just right” (P < .001).
Discussion:
Most patients reported high emotional support from at least 1 source. Black patients were most at risk for low support or unmet support needs. Spouse/partner support was important but only available to 58% of respondents. Patients at risk for unmet emotional support needs may benefit from additional support resources.
Keywords: social support, emotional support, colorectal cancer
Introduction
Social support for patients is associated with important health benefits, including improved cancer outcomes. Relative to those with reduced social support, patients who have a spouse/partner, family members, or friends who provide psychological and physical support tend to be in better health.1 Among cancer patients, social support has been associated with improved quality of life, adherence to treatment, and even improved survival.2–5 Although the mechanisms are not well established, the 4 traditional domains of social support—emotional, instrumental, informational, and appraisal—have all been associated with improved mental health among cancer patients.4 Emotional support, in particular, may contribute to the mitigation of stress associated with significant illness and has been causally associated with improved long-term health-related quality of life among colorectal cancer (CRC) patients.6
Social support may be especially relevant among CRC patients at higher than average risk for poor outcomes of treatment. Racial/ethnic disparities in CRC outcomes have been well documented, particularly among black patients relative to non-Hispanic whites.7,8 Although social support and social networks are known to have an impact on health-related quality of life outcomes for CRC care specifically,6,9,10 its influence on disparities in CRC care and outcomes is poorly understood and even less is known of the specific needs, sources, and availability of social support among CRC patients of varying sociodemographic backgrounds. Such data are critical to target and measure the results of interventions to reduce disparities and improve CRC care.
We sought to better understand existing sources of emotional support, the extent to which they meet patient needs, and how they differ by race and other sociodemographic attributes. We focused on stage III CRC patients because they tend to require multidisciplinary, multimodal long-term cancer care. To this end, we conducted a population-based survey of stage III CRC patients to describe patients’ perspectives on both extent of emotional support and how well emotional support needs were met.
Methods
Study Population
All patients who underwent surgery for stage III colon or rectal cancer between August 1, 2011 and December 31, 2013 from the Metropolitan Detroit and State of Georgia population-based Surveillance, Epidemiology and End Results (SEER) cancer registries were identified. These populations were specifically chosen to obtain racial diversity in the study group. Patients were considered eligible if they were 21–99 years of age at the time of diagnosis and underwent surgical resection within 4–12 months previously. Exclusion criteria included advanced metastatic cancer (stage IV) at diagnosis, change in diagnosis based on final histology, death prior to survey deployment, or residence outside the catchment area. This study was part of a larger project to examine racial variation in CRC care.
Data Collection
Physicians were notified of our intent to contact study subjects and permitted an opt-out period. Patients were then invited to participate using a modified multimodal Dillman approach, beginning with an information sheet, mailed survey, and a $20 gift, followed by up to 9 contact attempts using mail and telephone.11 Upon survey return, we performed extensive data checks for logic, errors, and omissions. Patients were recontacted by telephone as necessary to seek missing information. The survey data were supplemented with clinical data from the SEER registry and Census tract-level socioeconomic status data through a 2010 census linkage.
The consent forms included in the survey packets were informational and did not require the participants to sign or return them. The return of a completed survey was considered implied consent to participate in the study. The study protocol was approved by the institutional review boards of the University of Michigan, Wayne State University, Emory University, the State of Michigan, and the State of Georgia Department of Public Health (IRB HUM00032257).
Measures
The primary outcome of this analysis was the quantity of emotional support received from spouses/partners, family members, important others (friends, religious community members, coworkers), and health care providers. Emotional support was assessed using a modification of the social support subscale from the Functional Assessment of Cancer Therapy-Colon questionnaire, a quality of life survey previously validated with a sample of CRC patients.12,13 The response options consisted of a 5-point scale where “none”, “a little”, and “some” were categorized as low support, and “quite a bit” and “a lot” were categorized as high support. In order to determine the quality of emotional support, we queried whether the emotional support received aligned with what was desired. To understand whether emotional needs were met, respondents were asked to rate the quality of the emotional support they received from each source as “too little”, “just right”, or “too much”. These responses were self-defined based on previously conducted qualitative patient interviews during survey development.
The primary independent variable was self-reported race (white, black or other, that is, nonwhite, nonblack). Additional covariates included patient-reported demographics (age at diagnosis, gender, marital status), level of educational attainment, and annual household income. There were few missing values (<2%) for all variables except annual household income, for which 19% of patients did not respond or reported they did not know. Multiple imputation techniques were used to account for missing income data.
Statistical Analysis
Descriptive statistics were used to analyze the data, and univariate differences were detected using the chi-square test and t-tests as appropriate. To examine the relative impact of sociodemographic factors, we used multivariate logistic regression. All statistical tests were 2-sided. A P-value <0.05 was considered significant. Analyses were conducted using SAS 9.4 software (Cary, NC USA).
Results
We identified 2168 patients with stage III CRC who were reported to the registries of Georgia and Detroit using Rapid Case Ascertainment. Among these, 259 (12%) were determined to be ineligible (metastatic disease, noncolorectal primary, prior cancer diagnosis, or residing outside the registry area). Among the 1909 eligible patients included in the final sample, 608 could not be located or did not return the survey, resulting in 1301 completed surveys (68% response rate). Just over half of the respondents were male (53%). Among eligible respondents, 68% were white, 25% were black, and 7% were “other”, that is, nonwhite and nonblack. Black patients tended to be younger, had lower income, and were less educated than white patients (Table 1).
Table 1.
Characteristics of Respondents.
| Characteristics | All,a n (%) (N = 1301) | Black, n (%) (N = 335) | White, n (%) (N = 917) | P value |
|---|---|---|---|---|
| Sex | .1164 | |||
| Male | 685 (53) | 159 (50) | 483 (55) | |
| Female | 601 (47) | 162 (50) | 401 (45) | |
| Age (years) | <.0001 | |||
| <50 | 219 (17) | 75 (23) | 122 (14) | |
| 50–64 | 469 (36) | 128 (39) | 307 (35) | |
| 65–74 | 302 (23) | 70 (21) | 219 (25) | |
| ≥75 | 311 (24) | 54 (17) | 241 (27) | |
| Annual income ($) | <.0001 | |||
| <20 000 | 232 (18) | 96 (29) | 115 (13) | |
| 20 000–49 000 | 334 (26) | 86 (26) | 230 (26) | |
| 50 000–89 000 | 274 (21) | 52 (16) | 206 (23) | |
| >90 000 | 190 (15) | 14 (4) | 170 (19) | |
| Unknown | 271 (21) | 79 (24) | 168 (19) | |
| Highest level of education | <.0001 | |||
| <High school | 207 (16) | 80 (25) | 115 (13) | |
| High school | 318 (25) | 85 (27) | 218 (25) | |
| Some college | 413 (32) | 101 (32) | 292 (33) | |
| College or graduate degree | 335 (26) | 49 (16) | 257 (29) |
All” includes 7% nonblack and nonwhite patients.
Most respondents reported receiving high support from all sources (Figure 1). In terms of overall support received, the family was the source most commonly reported as high (89%), followed by important others (83%), and health care providers (71%). Among all sources of support, spouses/partners were most likely to be perceived as providing high support (95%); however, only 58% of patients had a spouse or partner. When we examined the presence of a spouse/partner by other demographic categories, we identified statistically significant differences among all subgroups (Table 2). Specifically, women, black patients, older patients, patients who did not complete high school, and those with <$20 000 annual income were less likely to have a spouse/partner (P < .001). When we further stratified patients by whether they had a spouse/partner, we found that patients who did not have a spouse/partner were less likely to have high support from important others (P < .001). This group did not differ from those with a spouse/partner in the level of support received from family or health care providers (Figure 2). Most patients reported high support from at least 1 source; however, black patients were more likely to report low support in all categories as compared with white patients (4% vs 8%, P < .011; data not shown).
Figure 1.
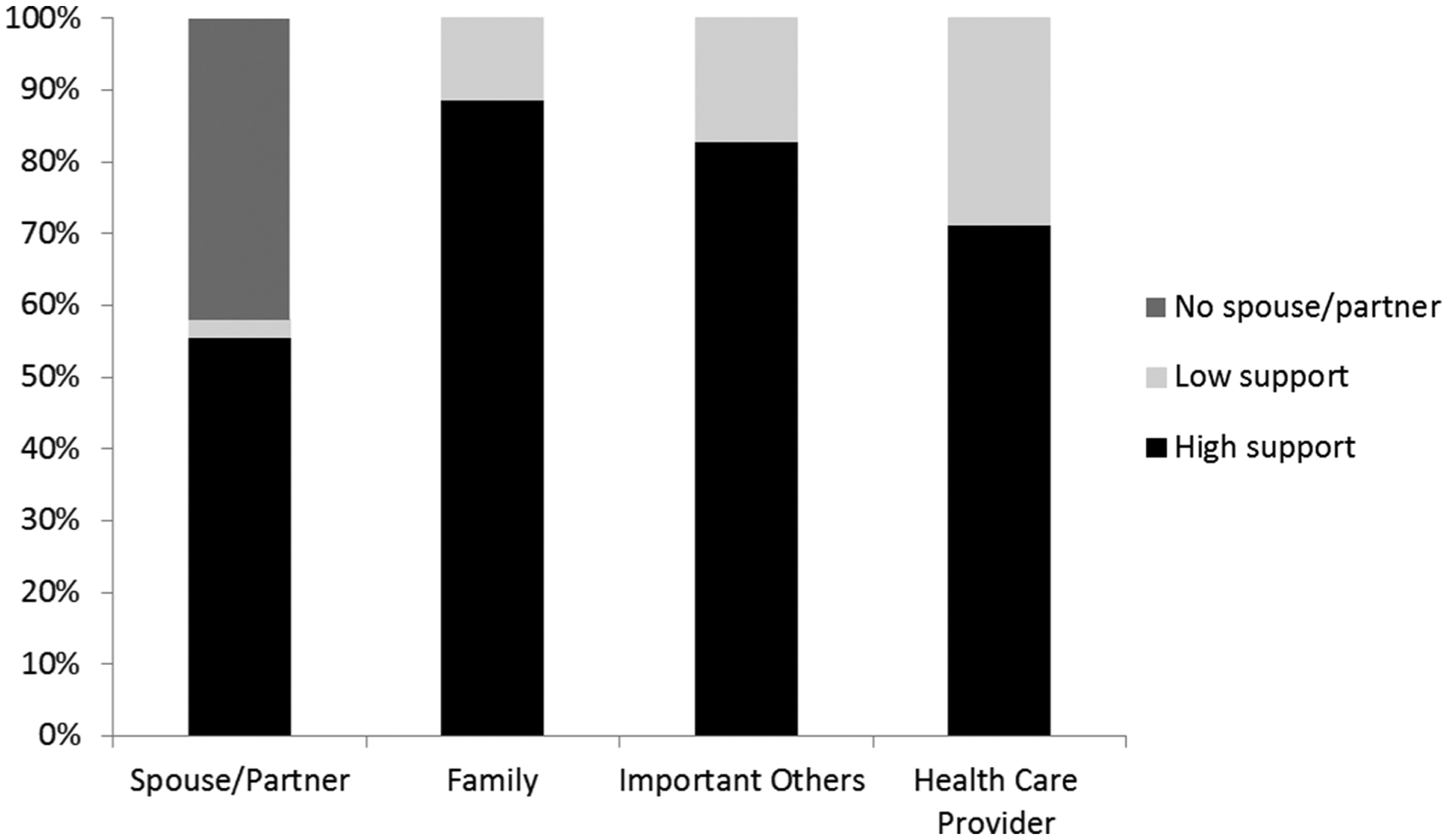
Level of emotional support by source for all patients. Important others include friends, religious community members and coworkers.
Table 2.
Presence and Level of Spouse/partner Support by Sociodemographic Characteristics.
| Characteristics | High support from spouse/partner, n (%) | Low support from spouse/partner, n (%) | No spouse/partner, n (%) | P value |
|---|---|---|---|---|
| Race | ||||
| White | 566 (61) | 19 (2) | 334 (36) | <.001 |
| Black | 131 (39) | 7 (2) | 198 (59) | |
| Other | 15 (62) | 1 (4) | 8 (34) | |
| Sex | ||||
| Male | 453 (67) | 14 (2) | 210 (31) | <.001 |
| Female | 263 (44) | 12 (2) | 322 (54) | |
| Age (years) | ||||
| <50 | 129 (59) | 7 (3) | 83 (38) | <.001 |
| 50–64 | 276 (59) | 9 (2) | 178 (38) | |
| 65–74 | 175 (59) | 6 (2) | 116 (39) | |
| ≥75 | 134 (44) | 9 (3) | 162 (53) | |
| Annual income, USD | ||||
| <20 000 | 57 (25) | 5 (2) | 166 (73) | <.001 |
| 20 000–49 000 | 176 (53) | 7 (2) | 150 (45) | |
| 50 000–89 000 | 195 (72) | 3 (1) | 70 (26) | |
| >90 000 | 159 (84) | 9 (5) | 21 (11) | |
| Highest level of education | ||||
| <High school | 88 (43) | 2 (1) | 115 (56) | <.001 |
| High school | 176 (56) | 3 (1) | 135 (43) | |
| Some college | 231 (56) | 12 (3) | 169 (41) | |
| College or graduate degree | 218 (66) | 10 (3) | 102 (31) |
Figure 2.
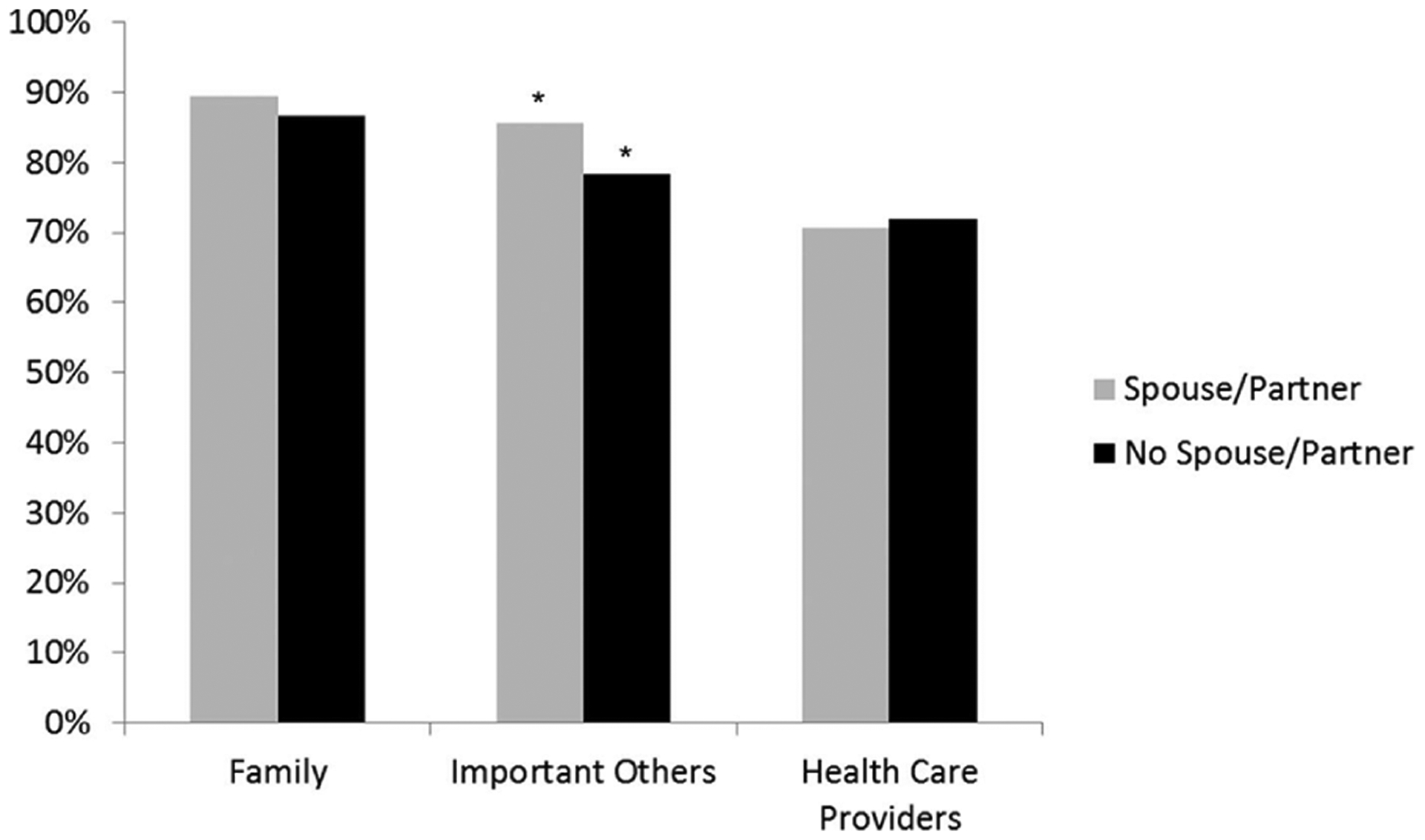
Patients reporting high levels of emotional support with and without a spouse/partner. *P < .001
The majority of patients reported that the quality of support they received was “just right” across sources of social support: spousal/partner support from patients with spouses/partners (87%), family members (88%), important others (85%), and health care providers (87%). Among patients who reported that they did not receive the desired level of support, important others and health care providers were reported more frequently to provide “too little” support as opposed to “too much”. However, this pattern was reversed for the support received from one’s spouse/partner or other family members, for which patients more frequently reported receiving “too much” support rather than “too little” (Table 3). Across all sources of support (Figure 3), black patients were significantly less likely than whites to report receipt of the desired level support in univariate analyses (P < .001 for each source). In the multivariate model adjusting for age, sex, and income, black patients consistently reported unmet emotional support needs from spouses/partners, family, and important others more often than whites.
Table 3.
Quality of Emotional Support Reported by Patients.
| Source of support | Race | Too little, n (%) | Just right, n (%) | Too much, n (%) | N/A | P value |
|---|---|---|---|---|---|---|
| Spouse/partner | Black | 7 (2) | 158 (47) | 30 (9) | 141 (42) | <.001 |
| White | 19 (2) | 733 (79) | 46 (5) | 130 (14) | ||
| Family | Black | 19 (6) | 254 (81) | 44 (14) | <.001 | |
| White | 45 (5) | 834 (92) | 27 (3) | |||
| Important others | Black | 33 (10) | 284 (87) | 10 (3) | <.001 | |
| White | 28 (3) | 883 (96) | 9 (1) | |||
| Health care providers | Black | 34 (11) | 268 (86) | 12 (4) | <.001 | |
| White | 94 (11) | 753 (88) | 9 (1) |
Figure 3.
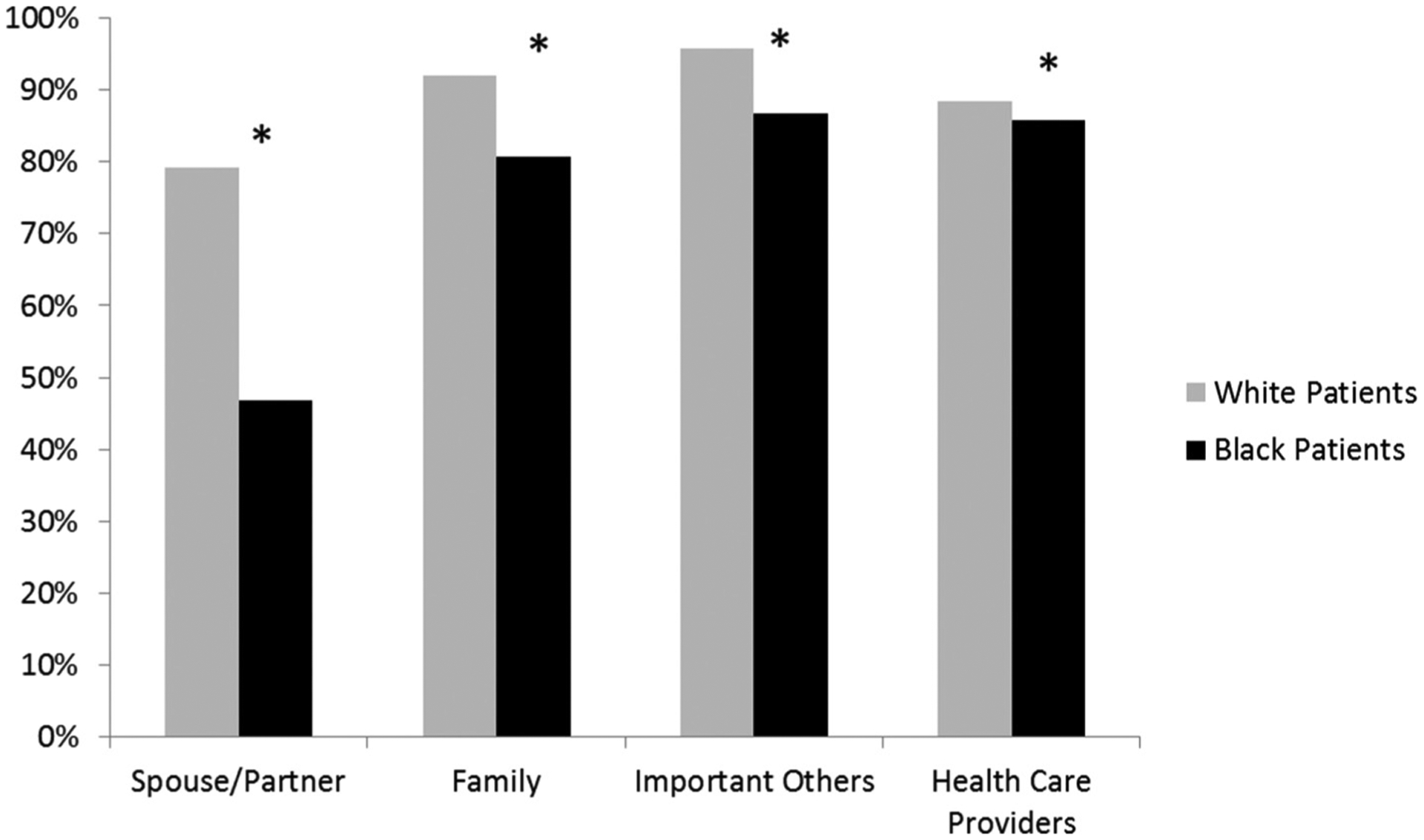
Receipt of desired level of emotional support by source for black and white patients. *P < .001 for every source of black versus white patients’ emotional support in the univariate analysis. Multivariate analysis demonstrated persistent differences between black and white patients for support from spouses/partners, family and important others (P = .002), but not health care providers. Many patients did not have a spouse/partner available.
Discussion
CRC patients in our study generally reported high emotional support from family, important others, and health care providers. Among those with spouses/partners, 95% reported high support. However, patients who were older, black, female, and those with <$20 000 annual income were less likely to have spouses or partners; thus, this source of support was less available. Furthermore, these patients receive less support from important others than patients with spousal/partner support. Concordance between the level of social support received and desired was generally high, although statistically significantly less so for black patients compared with white patients. When desired support was not met, patients more often received “too much” from spouses/partners and family members, while patients more often received “too little” from important others and health care providers.
Not surprisingly, spouses/partners were a particularly important source of emotional support in that, when present, nearly all respondents endorsed high support. Underscoring the importance of spouse/partner support, a study of partnered and unpartnered women with breast cancer found that women with partners had a higher mental and physical health-related quality of life scores after diagnosis.14 Furthermore, a recent study surveying CRC patients regarding social support found that 30% of patients did not have a partner and that poorer health-related quality of life scores were associated with lower social support.5 Health care providers should be aware that patients without a spouse/partner are a potential disadvantage and thus may require more resources from the health care system, especially given that these patients have less support available from important others. It may also be important for providers to assess for social support and to explicitly discuss the need for garnering social support in other forms such as from family and important others. There are distress screening tools available that help identify the lack of emotional support for patients and are recommended for use by the National Comprehensive Cancer Network guidelines.15 Additionally, social support has been shown to diminish over time for a significant number of patients and therefore should be periodically reassessed.5
Black patients in our cohort were especially vulnerable with respect to specific sources of support. Not only were they more likely to lack a spouse/partner but they also were more likely to report emotional support that did not meet their needs. These findings imply that black patients may be more likely to find support from sources other than spouses/partners that should be noted and included by clinicians when appropriate. Previous studies have shown that black and other minority patients, more than white patients, have active social networks including the creation of fictive kin, in which individuals are unrelated by either birth or marriage but have an emotionally significant relationship characteristic of a family relationship.16–18 These sources of support may include friends, religious community members, coworkers, and/or the medical community.
While social support among CRC patients has been associated with clinical benefits and improved health-related quality of life,5,6,9,10 the mechanism underlying this relationship is unclear. Patients with established social networks may be more inclined to follow through with taking care of themselves, not only for their own sake but for the sake of people in their lives. Additionally, they may have resources through their social networks in the form of education, access to care, and external motivation from family and friends to pursue appropriate and timely cancer care. Finally, social support may help to mitigate the deleterious associated effects of cancer treatment.
While assessing for social support is an important first step, identification alone of CRC patients with limited support is not enough to improve cancer-related outcomes. Patient navigation programs have been proposed as one potential solution toward mitigating disparities within cancer care. These programs help to identify individual barriers to cancer care and aim to reduce delays in diagnosis and treatment by overcoming barriers to health systems, providing health information about cancer care, overcoming patient barriers, and providing psychosocial support.19 Navigation programs have been used most often in the management of breast cancer; however, their use has demonstrated improved CRC screening rates among patients of low socioeconomic status.19,20 In a larger study by the multicenter Patient Navigation Research Program,21 patients were divided into those who received patient navigation and those who did not. Within the control arm, unemployed patients and unpartnered patients experienced delayed diagnostic resolution, whereas, in the patient navigation arm, there were no disparities in diagnostic resolution. While these studies boast advantages of patient navigation, funding and implementation challenges of such programs are rampant. Additionally, improvement in overall treatment outcomes with navigation for patients with CRC has not yet been demonstrated.
Our study was subject to several limitations that must be noted. First, although social support encompasses 4 recognized domains (emotional, instrumental, informational, and appraisal), we measured only emotional support. Our findings, however, are strengthened by the addition of a query regarding whether the level of emotional support received aligned with the support desired. Second, our data set relied on patient-reported assessments rather than “objectively” measured indices. We believe that patients themselves should be considered expert on the level of support that they receive and desire. However, our future work will involve further data collection to correlate patient-reported assessments with clinical outcomes. Third, this was a cross-sectional (one time) study, and we acknowledge that emotional support may fluctuate over time. Finally, support from any particular source can be complicated as is the nature of relationships, and the notion of appropriate emotional support may be variable depending on the needs of the patient. Such nuances may not be captured by quantitative survey data.
In conclusion, our work highlights important demographic differences in sources of support and in the alignment between the received and desired level of support among CRC patients. For vulnerable patients lacking sources of social support or receiving inadequate levels of support, additional resources from our health care systems may be required in order to provide appropriate and equitable cancer care. Devising and implementing screening for inadequate social support would likely benefit not only patients but also the health care team with regard to effective treatment planning. These at-risk patients may benefit from patient navigation programs or other targeted interventions at reducing disparities in emotional support.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: A.M.M and the study were supported by the American Cancer Society, Atlanta, GA (Research Scholar Grant # 11-097-01-CPHPS). C.M.V is supported by grant K07CA196752-01 from the National Institutes of Health/National Cancer Institute. The views expressed herein do not necessarily represent the views of the American Cancer Society or the National Institutes of Health/National Cancer Institute.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. doi: 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- 2.Eom C-S, Shin DW, Kim SY, et al. Impact of perceived social support on the mental health and health-related quality of life in cancer patients: results from a nationwide, multicenter survey in South Korea. Psychooncology. 2013;22(6):1283–1290. doi: 10.1002/pon.3133 [DOI] [PubMed] [Google Scholar]
- 3.Ikeda A, Kawachi I, Iso H, Iwasaki M, Inoue M, Tsugane S. Social support and cancer incidence and mortality: the JPHC study cohort II. Cancer Causes Control. 2013;24(5):847–860. doi: 10.1007/s10552-013-0147-7 [DOI] [PubMed] [Google Scholar]
- 4.Pinquart M, Duberstein PR. Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol. 2010;75(2):122–137. doi: 10.1016/j.critrevonc.2009.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haviland J, Sodergren S, Calman L, et al. Social support following diagnosis and treatment for colorectal cancer and associations with health-related quality of life: results from the UK colorectal wellbeing (crew) cohort study. Psychooncology. 2017;26(12):2276–2284. doi: 10.1002/pon.4556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gonzalez-Saenz de Tejada M, Bilbao A, Baré M, et al. Association of social support, functional status, and psychological variables with changes in health-related quality of life outcomes in patients with colorectal cancer. Psychooncology. 2016;25(8):891–897. doi: 10.1002/pon.4022 [DOI] [PubMed] [Google Scholar]
- 7.Alexander DD, Waterbor J, Hughes T, Funkhouser E, Grizzle W, Manne U. African-American and Caucasian disparities in colorectal cancer mortality and survival by data source: an epidemiologic review. Cancer Biomark. 2007;3(6):301–313. doi: 10.3233/CBM-2007-3604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morris AM, Rhoads KF, Stain SC, Birkmeyer JD. Understanding racial disparities in cancer treatment and outcomes. J Am Coll Surg. 2010;211(1):105–113. doi: 10.1016/j.jamcollsurg.2010.02.051 [DOI] [PubMed] [Google Scholar]
- 9.Trentham-Dietz A, Remington PL, Moinpour CM, Hampton JM, Sapp AL, Newcomb PA. Health-related quality of life in female long-term colorectal cancer survivors. Oncologist. 2003;8(4):342–349. doi: 10.1634/theoncologist.8-4-342 [DOI] [PubMed] [Google Scholar]
- 10.Sapp AL, Trentham-Dietz A, Newcomb PA, Hampton JM, Moinpour CM, Remington PL. Social networks and quality of life among female long-term colorectal cancer survivors. Cancer. 2003;98(8):1749–1758. doi: 10.1002/cncr.11717 [DOI] [PubMed] [Google Scholar]
- 11.Dillman D, Smyth J, Internet CL. Christian L. Internet, mail, and mixed- mode surveys : the tailored design method. 3rd ed. Wiley & Sons; 2009. [Google Scholar]
- 12.Ganesh V, Agarwal A, Popovic M, et al. Comparison of the FACT-C, EORTC QLQ-CR38, and QLQ-CR29 quality of life questionnaires for patients with colorectal cancer: a literature review. Support Care Cancer. 2016;24(8):3661–3668. doi: 10.1007/s00520-016-3270-7 [DOI] [PubMed] [Google Scholar]
- 13.Guidry JJ, Aday LA, Zhang D, Winn RJ. The role of informal and formal social support networks for patients with cancer. Cancer Pract. 1997;5(4):241–246. [PubMed] [Google Scholar]
- 14.Leung J, Smith MD, McLaughlin D. Inequalities in long term health-related quality of life between partnered and not partnered breast cancer survivors through the mediation effect of social support. Psychooncology. 2016;25(10):1222–1228. doi: 10.1002/pon.4131 [DOI] [PubMed] [Google Scholar]
- 15.Allen JO, Zebrack B, Wittman D, Hammelef K, Morris AM. Expanding the NCCN guidelines for distress management: a model of barriers to the use of coping resources. J Community Support Oncol. 2014;12(8):271–277. doi: 10.12788/jcso.0064 [DOI] [PubMed] [Google Scholar]
- 16.Johnson CL, Barer BM. Families and networks among older inner-city blacks. Gerontologist. 1990;30(6):726–733. doi: 10.1093/geront/30.6.726 [DOI] [PubMed] [Google Scholar]
- 17.Johnson CL. Fictive kin among oldest old African Americans in the San Francisco Bay area. J Gerontol B Psychol Sci Soc Sci. 1999;54(6):S368–S375. doi: 10.1093/geronb/54B.6.S368 [DOI] [PubMed] [Google Scholar]
- 18.Mead EL, Doorenbos AZ, Javid SH, et al. Shared decision-making for cancer care among racial and ethnic minorities: a systematic review. Am J Public Health. 2013;103(12):e15–e29. doi: 10.2105/AJPH.2013.301631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Honeycutt S, Green R, Ballard D, et al. Evaluation of a patient navigation program to promote colorectal cancer screening in rural Georgia, USA. Cancer. 2013;119(16):3059–3066. doi: 10.1002/cncr.28033 [DOI] [PubMed] [Google Scholar]
- 20.Jandorf L, Gutierrez Y, Lopez J, Christie J, Itzkowitz SH. Use of a patient navigator to increase colorectal cancer screening in an urban neighborhood health clinic. J Urban Health. 2005;82(2):216–224. doi: 10.1093/jurban/jti046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodday AM, Parsons SK, Snyder F, et al. Impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 2015;121(22):4025–4034. doi: 10.1002/cncr.29612 [DOI] [PMC free article] [PubMed] [Google Scholar]


