The COVID-19 pandemic has pushed healthcare systems to a limit worldwide [1]. Disrupted healthcare systems, social distancing and the need for reduced exposure risk related to travel and public transport seem to open a window of opportunity for a broader use of information and telecommunication means [2]. Consequently, telehealth solutions have gained attention [2]. A search on the PubMed (May 2021) retrieved 2101 studies about telehealth published in 2020 representing an increase of 280% compared to 2019. Of all studies published in 2020, only 51 (2%) studies included low- and middle-income countries in their title or abstract, evidencing that publication bias extends to the realm of telehealth, but also that the specific relevance of telehealth for those contexts is not being globally discussed. Furthermore, this marked difference in the number of published studies can also reflect the challenge to implement telehealth as a public health policy in low- and middle-income countries. As the evidence on the effectiveness, as well as cost-effectiveness of telehealth modalities is mounting, some questions should be considered: Is there an indication that telehealth is bridging the gap in health disparities or exposing health disparities in low- and middle-income countries? We considered the Brazilian context during the pandemic outbreak to explore this concern given Brazil has the third-highest number of confirmed cases and second-highest death toll from COVID-19 in the world. Strategies to guarantee access to health services (e.g., physiotherapy and other nonpharmacological, medical or complementary therapies) are of utmost priority and should be expected in these circumstances.
The Brazilian Unified Health System (better known by the acronym SUS) is underpinned by the principles of universality, equity and equality in healthcare access [3] and covers about 70% of Brazil's population [4]. The changes in policy for regulating the use of telehealth [2] due to the COVID-19 restrictions and an attempt to adjust telehealth within regular practices were expected to ensure access to health particularly among ethnic minorities and people with lower socioeconomic status. However, the 2020′s pandemic reinforced obstacles to health access already know by a portion of the Brazilian population, such as lack of specialized care, bringing the precarization of services to light.
Differently from some high-income countries where telehealth has been implemented over the years and was structured to support the communication between patients and health professionals [5], the Brazilian Telehealth Program focused on the qualification of health professionals from the primary health through telediagnosis and formative second opinion, not allowing teleconsultations [6]. The pandemic prompted an accelerated regulation of remote health care services, but guidance for the correct implementation was insufficiently provided to the professionals. Regulation also failed to consider populations’ readiness, needs and the access capacity to technology. In the absence of an organized national implementation plan, telehealth is likely to favor and expose existing health disparities.
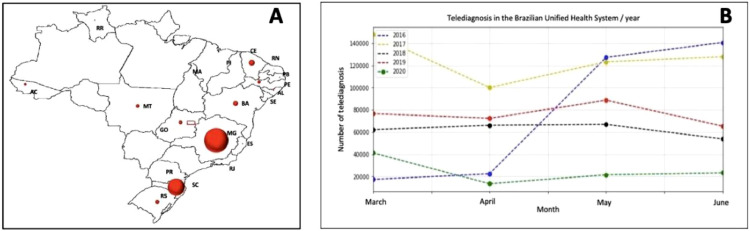
We analyzed the available data from the Digital Health Department of Brazilian Ministry of Health about telediagnosis in the period of 2016 to July 2020 and found a total of 4010,087 telediagnosis with an irregular distribution across the country. From 26 Brazilian states, only four were responsible to this result being 59.5% (2386,773) in Minas Gerais, 29.4% (1177,904) in Santa Catarina, 3.3% (131,0583) in Ceara, and 2.2 (86,547) in Bahia (Fig. 1 A). Rather than a robust support to population in need, a comparison to the same month of 2019 shows the first pandemic wave in Brazil was accompanied by a significant reduction in the number of telediagnosis: March (−53.7%), April (−18.6%), May (−24.3%), and June (−35.6%) (Fig. 1B). Our analysis suggests that, during pandemic, Brazil missed an opportunity of performing a major telehealth implementation program.
Fig. 1.
Brazilian telediagnosis registries. (A) Unequal distribution of telediagnosis within the country. (B) Number of telediagnosis registries in the Brazilian Unified Health System in the period 2016–2020.
Telehealth policies should consider that socioeconomic abysses among regions and specific population groups restrict access to adequate devices and technology. In addition, patterns of technology usage are also influenced by culture and user location, beyond socioeconomic factors [7]. According to the Brazilian ICT Panel from 2020 to 2021, internet users from privileged socioeconomic groups were more likely to engage with education and distance learning activities than those from unprivileged socioeconomic groups. In Brazil, unemployment rates reached 14.1 million people in the third trimester of 2020 (13.1%), and 5.9 million people is currently classified as displaced workers. Illiteracy rates have been dropping continuously to a margin of 6.6% in 2019, however it still implies 11 million people lack the basic skills to read or write. Considering the link between formal literacy and digital literacy, it is reasonable to assume that poor digital literacy is also present, thus a cumbersome barrier to telehealth pervasiveness. Moreover, in terms of internet usage, despite Brazil is the largest country in Latin America comprising 152 million of users (81% of the population older than 10 years), internet access is often rudimentary, supported by a prepaid smartphone with 3 G or 4 G technologies (i.e., focused on social media, limited download). Because cultural assumptions and community norms are also part of the challenge of implementing telehealth initiatives, the use of less resourceful technologies such as text messaging might not be adequate despite its greater feasibility to remote areas.
As a result of a rapid and disorganized implementation, telehealth may expose health disparities apart from not become a viable option for a large portion of the population living in Brazil or in other low- and middle-income countries. The integration of telehealth into routine practice requires substantial alterations to established workflows and infrastructures [8]. Moreover, specific challenges (e.g., patients’ and professionals’ readiness) and barriers (e.g., level of education, infrastructure, computer literacy) commonly stablished in low- and middle-income countries, remain overlooked. The lack of proper health care services may have important consequences to vulnerable groups such as Brazilian maroons, indigenous, immigrants, elderly, people with non-communicable diseases and multimorbidity, and those with multiple or more severe conditions requiring regular symptom monitoring and adjustment of complex drug regimens [9,10]. We believe that telehealth can only be employed when population have guaranteed access to the technology supporting its implementation (from telephone calls to websites and videoconference). In conclusion, authors emphasising the effectiveness and efficiency of telehealth modalities need to bear in mind that the primary goal of telehealth is to reduce disparities in health access. To fulfill this goal, attention to challenges, barriers and implementation processes is mandatory and should consider diversity of countries and economies across the world.
Funding
None.
Ethical approval
Not required.
Patient consent
Not required.
Declaration of Competing Interest
None to declare.
Acknowledgements
None to declare. PTS 7829: Validation error; following contents are missing 1. Author statement, 2. Funding, 3. Competing interests, 4. Ethical approval. Please check with copyeditors for more on HLPT Journals.
References
- 1.World Health Organization . World Health Organization; 2020. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 august 2020. [Google Scholar]
- 2.Lieneck C., Garvey J., Collins C., Graham D., Loving C., Pearson R. Healthcare. Multidisciplinary Digital Publishing Institute; 2020. Rapid telehealth implementation during the covid-19 global pandemic: a rapid review; p. 517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castro M.C., Massuda A., Almeida G., Menezes-Filho N.A., Andrade M.V., de Souza Noronha K.V.M., et al. Brazil's unified health system: the first 30 years and prospects for the future. Lancet. 2019;394(10195):345–356. doi: 10.1016/S0140-6736(19)31243-7. [DOI] [PubMed] [Google Scholar]
- 4.Jurberg C. Flawed but fair: brazil's health system reaches out to the poor. Bull World Health Organ. 2008;86(4):248–249. doi: 10.2471/BLT.08.030408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaffe D.H., Lee L., Huynh S., Haskell T.P. Health Inequalities in the Use of Telehealth in the United States in the Lens of COVID-19. Popul Health Manag. 2020;23(5):368–377. doi: 10.1089/pop.2020.0186. [DOI] [PubMed] [Google Scholar]
- 6.Scott Kruse C., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palmer K., Monaco A., Kivipelto M., Onder G., Maggi S., Michel J.-.P., et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res. 2020;32:1189–1194. doi: 10.1007/s40520-020-01601-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azarpazhooh M.R., Morovatdar N., Avan A., Phan T.G., Divani A.A., Yassi N., et al. COVID-19 pandemic and burden of non-communicable diseases: an ecological study on data of 185 countries. J Stroke Cerebrovasc Dis. 2020;29(9) doi: 10.1016/j.jstrokecerebrovasdis.2020.105089. [DOI] [PMC free article] [PubMed] [Google Scholar]