Abstract
Objectives
To evaluate the feasibility, efficiency, and safety of the transradial approach (TRA) for cerebral angiography versus the transfemoral approach (TFA) in patients.
Methods
In this trial, 2314 patients underwent cerebral angiography, with 1085 patients undergoing the procedure via radial access and 1229 via transfemoral access. The arterial puncture time, operation success rate, oppression time on puncture points, local vascular complication incidence (including bleeding, hematoma, and pseudoaneurysm), deep venous thrombosis of lower limbs (DVT), and bradycardia/hypotension were observed and compared between the two groups.
Results
Of the patients who underwent cerebral angiography via radial access, the procedure was successful in 1070 patients; compared with 1219 patients with transfemoral access, there was no significant difference (P > 0.05) in the success rate or the arterial puncture time. Radial access patients were less likely to present with oppression time on puncture points, local vascular complications, DVT, and bradycardia/hypotension compared with femoral access patients.
Conclusions
For patients undergoing cerebral angiography, radial and femoral approaches are both safe and effective. However, the lower rate of local vascular complications may be a reason to use the radial approach.
Keywords: Cerebral angiography, Transradial approach, Transfemoral approach, Intervention
1. Introduction
Cerebral angiography is the most valuable means of diagnosing and investigating intracranial vessel lesions. The transfemoral arterial approach (TFA) has been the conventional approach to cerebral angiography. However, in recent years, the transradial arterial approach (TRA) has become a feasible alternative access site for cerebral angiography. This is largely due to data demonstrating a reduction in access site complications; other benefits, such as decreased length of stay, reduced hospital costs, and improved patient satisfaction, have also been shown,1, 2, 3, 4 but there were some problems that needed to be resolved. In this paper, we review the perioperative complications and the successful recanalization rate to evaluate the safety and technical feasibility of this approach. To the best of our knowledge, this is the largest study on the use of the transradial approach for cerebral angiography to date.
2. Materials and methods
2.1. Patients
A total of 2314 cerebral angiograms were performed: 1085 were performed using a transradial arterial approach, and 1229 were performed using a transfemoral arterial approach. The patients ranged in age from 35 to 71 years (mean age, 49 years). Inclusion criteria were as follows: age <90 years; review of the patient in the hospital after surgery; good physical state; no liver or kidney function abnormalities; no history of severe allergy to drugs.
2.2. Instruments and techniques
Patients were brought to the angiographic suite. All procedures were performed for diagnostic purposes. We performed all the transradial approaches via the right side. If the right side was not available, we did not proceed with the transradial approach because performing this procedure via the left radial artery was very inconvenient. In these cases, we performed a right transfemoral approach. All patients underwent a modified Allen's test of the right wrist to evaluate satisfactory collateral perfusion prior to the procedure. If the test was abnormal, we did not proceed with radial artery access. After ulnar artery patency was proven via a modified Allen's test, patients were prepared and draped with right radial artery site exposure at the wrist and the right arm abducted at a 70° angle. The right inguinal area was draped as well for conversion of the access route from the wrist to the groin if necessary. A small amount of 2% lidocaine was infiltrated into the subcutaneous tissue on the radial artery around the styloid process of the radius, and the artery was punctured at the point of maximum pulsation using a 20-gauge needle with a modified Seldinger technique. A 5 French introducer sheath (Terumo Radifocus, Tokyo, Japan) was then placed within the artery. To prevent vasospasm of the artery, a diluted solution of nitroglycerine (200 μg/mL; 0.25 mL), verapamil (2.0 mg), and heparin (3000 IU/mL) was injected intra-arterially through the side port of the introducer, which was then continuously flushed with pressurized (300 mm Hg), heparinized saline during the procedure. A 5 French Simmons type 2 catheter (Terumo Radifocus, Tokyo, Japan) was inserted, and forearm angiography was performed through the catheter to confirm there was satisfactory collateral perfusion. Under fluoroscopy monitoring, a 5 French Simmons 2 catheter was advanced over a 0.035-inch hydrophilic guidewire (Terumo Radifocus, Tokyo, Japan) through the radial artery to the brachial artery and then through the axillary artery into the subclavian artery in all cases. Guidewire was subsequently advanced to the ascending aorta and turned back at the aortic valve for the reconstitution of the natural Simmons configuration of the catheter. After the catheter was reconstituted, the catheter tip was controlled to select the orifice of the target artery [the innominate artery, left common carotid artery (CCA), or left subclavian artery] and then advanced to the distal selection [the internal carotid artery (ICA) or vertebral artery]. After the procedure, the catheter and sheath were removed, and a superficial pressure dressing with a radial artery hemostatic device (Hangzhou Alicon Pharm Co., Ltd., Zhejiang, China) was applied to the radial artery puncture site. Patients were observed for 3 h before discharge. During this observation period, their activity was not limited to bed rest.
3. Results
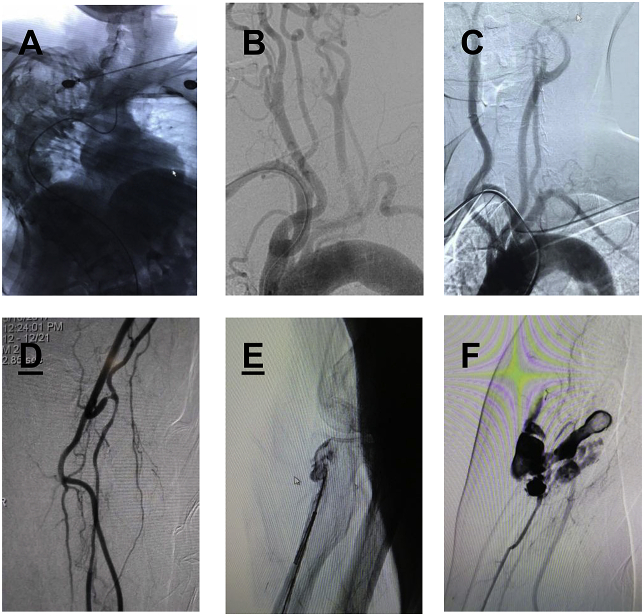
1070 patients were successed in 1085 patients via radial access, compared with 1219 patients via transfemoral access and there was no significant difference (P > 0.05), also in the arterial puncture time.Radial access patients were less likely to present with the oppress time on puncture points (Table 1).Transfemoral approach was performed in the fourteen patients with failed radial artery access.This was attributed to failure of the radial puncture, loop formation or tortuosity at the proximal end of the radial artery in two patients, and severe vasospasm of the radial artery following multiple puncture trials in two patients (Fig. 1C and D). Transradial approach was performed in the ten patients with failed femoral artery access.This was attributed to congenital scoliosis and DeBakey Ⅲ aortic arch (Fig. 1A and B). All supraaortic vessels were successfully catheterized. Patients were excluded when it was deemed impossible or dangerous to catheterize the ICA because of severe stenosis or atheromatous plaques. We did not attempt to select the vertebral artery routinely, If there was not found the legions at previous CT angiography or MR angiography. Two procedures using the same radial artery were performed in two patients. Among these patients, radial artery occlusion or stenosis (5%) was demonstrated on follow-up cerebral angiography (Table 2). In all patients in whom the transradial angiography was successful, the diagnostic adequacy and quality of images were satisfactory.
Table 1.
Procedural data compare between radial and femoral approach.
| Variables | TRA group (1085) | TFA group (1229) | P Value |
|---|---|---|---|
| Fluoroscopy time (min) | 5.46 ± 4.21 | 4.84 ± 4.01 | <0.05 |
| Operation time (min) | 25.72 ± 13.17 | 20.36 ± 10.42 | <0.05 |
| Manual pressing course (min) | No need | 15.6 ± 5.2 | <0.01 |
| Length of hospital stay (d) | 2.16 ± 1.42 | 3.97 ± 2.07 | <0.01 |
*Data are expressed as number of patients.
Fig. 1.
A:Congenital scoliosis. B:DeBakey Ⅲ aortic arch. C:Subclavian artery formations. D:Loop formation of the radial artery. E:Microcatheter twisted. F: Radial artery rupture.
Table 2.
Complication of the two groups.
| Variables | TRA group (1085) | TFA group (1229) | P Value |
|---|---|---|---|
| Radial artery occlusion | 55 | 0 | >0.01 |
| Symptomatic stroke | 1 | 15 | >0.05 |
| Puncture site hematoma | 16 | 121 | >0.05 |
| Pulmonary embolism | 0 | 5 | >0.01 |
| Pseudoaneurysm | 0 | 23 | >0.01 |
| Arteriovenous fistula | 0 | 2 | >0.05 |
*Data are expressed as number of patients.
Pain in the forearm or arm developed in three patients during the procedures, but it was usually mild and transient. Spasms were effectively resolved with the combined solution of nitroglycerin, verapamil, and heparin. Procedure related vascular complications, such as puncture site hematoma, hand ischemia, pseudoaneurysm, arteriovenous fistula and arterial dissection, were seen in our series (Table 2). However, there were two complications, one is microcatheter twisted and the other radial artery rupture (Fig. 1E and F). No patients had functional disability of the hand, and no complaints of discomfort were reported.
4. Discussion
The transradial approach was first introduced in 1998 in coronary angiography.2 It was found to reduce puncture site complications and the discomfort of the patients. The transradial approach has become popular among interventional cardiologists as a diagnostic and therapeutic tool in a number of centers worldwide because of its low puncture site complication rate, compared with the transfemoral approach, for patients undergoing anticoagulation therapy.8, 9, 10, 11 The transradial approach to cerebral angiography and neurointervention was introduced in 2000.14 Some authors expected that this new approach would become a gold standard for cerebral angiography16; however, the transfemoral approach is usually favored because of familiarity and convenience.
The femoral artery is the most common puncture site used for cerebral angiography because most angiographers and neurointerventionalists are comfortable using this access point for the entire cerebral vascular system. However, there are some limitations to this approach. The transfemoral approach cannot be used when patients have extensive atherosclerotic disease in their aortic arch, atypical anatomy of their aortic or brachiocephalic vessels, dissection of the thoracic artery, iliofemoral occlusive disease, or groin infection.1,3,7 Additionally, this procedure can lead to several complications, such as retroperitoneal hematoma, pseudoaneurysm formation, arteriovenous fistula formation, femoral nerve injury, lower limb ischemia, and pulmonary embolism.7,12,13,15,17 One of the major limitations of the transfemoral approach is the requirement of 4–6 h of leg immobilization and bed rest to prevent bleeding complications at the femoral access site.13 In some cases, the duration of the leg immobilization can be greatly reduced by the application of percutaneous closure devices. However, these devices are expensive.
The most important advantage of the transradial approach is easy hemostasis. The transfemoral approach may cause more suffering for the patients, particularly those with advanced age, degenerative spine or spinal lesions, or benign prostate hypertrophy, because these conditions require complete bed rest for at least several hours following femoral artery puncture.18 Furthermore, after the transfemoral approach, patients are usually kept in the hospital overnight for observation. In contrast, the transradial approach does not require bed rest and allows the patient to be ambulatory immediately without the restriction of arm movement after the procedure. In our institution, after the transfemoral approach, we perform manual compression for 15 min without the use of additional percutaneous groin closure devices in the angiographic suite. However, the transradial approach does not require extra time for compression. It is not necessary to compress the puncture site manually, as a simple compression device is sufficient to achieve hemostasis without special precautions. We generally observe patients for 6 h with leg immobilization after transfemoral angiography. This is quite uncomfortable for patients and may lead to anxiety toward future angiographic trials. However, transradial angiography does not require prolonged observation. It requires 3 h for observing patients and allows cerebral angiography to be easily performed on outpatient basis, which is useful for the image follow-up of patients after neurointerventional procedures.
The transradial approach is especially useful for patients with obesity or severe atherosclerotic change of the bilateral femoral arteries, as the radial artery is an easier and safer access route.15 In these cases, femoral artery puncture often fails due to the artery's deep location and weak pulsation. However, the radial artery is superficially located on the underlying firm tendon, relatively fixed, easily compressible, and, most important, not an end artery. Since no major nerves or veins run in the vicinity of the radial artery over the radial styloid, neuropathies or arteriovenous fistulas are less likely to occur.15
Transradial cerebral angiography has some advantages after the administration of anticoagulants or with effective antiplatelet therapy.13,15,16 In the elderly, as the rate of atherosclerotic cerebrovascular and coronary diseases increases, anticoagulation or antiplatelet therapies are more common. These conditions are a contraindication for the femoral approach, secondary to the potential for neurologic compromise caused by a large hematoma.16 It is usually necessary to discontinue the anticoagulant or antithrombotic agents before the procedure to reduce the risk of serious hemorrhagic complications. Additionally, it may be difficult and time-consuming to restart and readjust the level of anticoagulation after angiography if this has been stopped for the angiogram. However, the transradial approach does not require these agents to be discontinued. A total of 965 of the patients in our study received anticoagulant and/or antiplatelet therapy perioperatively and did not experience any major hemorrhagic complications, such as significant puncture site hematoma, pseudoaneurysm, or arteriovenous fistula formation. Therefore, it is reasonable to expect that anticoagulant and antiplatelet therapies need not be discontinued for cerebral angiography via the transradial approach. In addition, the continuation or addition of these agents may actually reduce the intraprocedural thromboembolic complications. We also recommend the use of pressurized, heparinized saline for the continuous flushing of the introduced sheath in order to prevent thrombosis.
With advancing patient age, vascular tortuosity and atheromatous changes increase. The transradial approach is very useful in patients with significant tortuosity or ectatic changes of the aortic arch and patients with acute right vertebral artery course from the subclavian artery.12 In some patients with very tortuous supra-aortic branches or bovine-type left CCA, it is necessary to exchange Simmons or other specialized catheters for transfemoral access. However, the transradial approach allows easy catheterization without exchanging the catheter. Additionally, it is more suitable in the right vertebral and right carotid systems. At times, the right vertebral artery is extremely difficult to catheterize with a transfemoral approach. In this condition, the right vertebral artery is easily catheterized with the transradial approach. The stability of guiding catheters in the right vertebral and carotid systems is outstanding with a transradial approach.16 The catheter stability is excellent because the catheter system is confined to vessels with relatively small diameters, whereas guiding-catheter instability often occurs with a transfemoral approach because of transverse ectatic and large-diameter aortic arches.16
Transradial cerebral angiography has some limitations. The success rate of selective catheterization is relatively low, especially for the left vertebral and internal carotid artery.12 However, this is not a severe problem in vascular evaluation because in most cases the target vessels are successfully visualized with the left common carotid artery injection and the left subclavian artery and/or right vertebral artery injection. In our institution, to avoid vessel wall damage in the vertebral artery, we place the catheter tip just at the orifice or the proximal portion of the vertebral artery. Otherwise, we prefer the transfemoral approach if it is absolutely necessary to evaluate the left vertebral artery.
As a transradial approach is technically somewhat difficult and more challenging than a transfemoral approach, it has a steep and significant learning curve to increase the success rate. It is difficult to negotiate the wire into the aortic arch because the vessels originating from the arch become tortuous with advancing age. Additionally, potential trauma to the radial artery is more likely to occur in elderly patients, in whom the radial artery may be quite tortuous.13 The success rate of transradial cerebral angiography is reported to be 92.7–99%.6,10,13,15,18 Hildick-Smith et al.5 reported that the success rate of a transradial approach ranged from 88% for beginners to 94% for experienced specialists. In our study, the success rate was 92.2% in elderly patients (>60 years old). Some authors, such as Simmons,12 have expressed concern about procedure-related thromboembolism with a reverse-angle catheter. They suggest that the whirling motion of the bulky catheter within a tortuous atheromatous aorta is dangerous. We had one patient who experienced intraprocedural thrombosis. However, this complication rate is comparable with that of transfemoral access.4,12 It is important to be gentle with catheter manipulation in the aortic arch to reduce the chances of disturbing atheromatous plaques.
5. Conclusion
Transradial cerebral angiography is a useful routine or alternative method for patients in whom transfemoral cerebral angiography is less favorable. With advancing patient age, transradial angiography is helpful for overcoming vessel tortuosity and patient discomfort.
References
- 1.Bendok B.R., Przybylo J.H., Parkinson R., Hu Y., Awad I.A., Batjer H.H. Neuroendovascular interventions for intracranial posterior circulation disease via the transradial approach : technical case report. Neurosurgery. 2005;56:E626. doi: 10.1227/01.NEU.0000154820.28342.38. discussion E626. [DOI] [PubMed] [Google Scholar]
- 2.Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16:3–7. doi: 10.1002/ccd.1810160103. [DOI] [PubMed] [Google Scholar]
- 3.Fessler R.D., Wakhloo A.K., Lanzino G., Guterman L.R., Hopkins L.N. Transradial approach for vertebral artery stenting : technical case report. Neurosurgery. 2000;46:1524–1527. doi: 10.1097/00006123-200006000-00044. ; discussion 1527-1528. [DOI] [PubMed] [Google Scholar]
- 4.Heiserman J.E., Dean B.L., Hodak J.A. Neurologic complications of cerebral angiography. AJNR Am J Neuroradiol. 1994;15:1401–1407. ; discussion 1408-1411. [PMC free article] [PubMed] [Google Scholar]
- 5.Hildick-Smith D.J., Walsh J.T., Lowe M.D., Shapiro L.M., Petch M.C. Transradial coronary angiography in patients with contraindications to the femoral approach : an analysis of 500 cases. Cathet Cardiovasc Interv. 2004;61:60–66. doi: 10.1002/ccd.10708. [DOI] [PubMed] [Google Scholar]
- 6.Iwasaki S., Yokoyama K., Takayama K. The transradial approach for selective carotid and vertebral angiography. Acta Radiol. 2002;43:549–555. doi: 10.1080/j.1600-0455.2002.430601.x. [DOI] [PubMed] [Google Scholar]
- 7.Jo K.W., Park S.M., Kim S.D., Kim S.R., Baik M.W., Kim Y.W. Is transradial cerebral angiography feasible and safe? A single center's experience. J Korean Neurosurg Soc. 2010;47:332–337. doi: 10.3340/jkns.2010.47.5.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kiemeneij F., Laarman G.J. Transradial artery Palmaz-Schatz coronary stent implantation : results of a single-center feasibility study. Am Heart J. 1995;130:14–21. doi: 10.1016/0002-8703(95)90229-5. [DOI] [PubMed] [Google Scholar]
- 9.Kiemeneij F., Laarman G.J., Odekerken D., Slagboom T., van der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches : the access study. J Am Coll Cardiol. 1997;29:1269–1275. doi: 10.1016/s0735-1097(97)00064-8. [DOI] [PubMed] [Google Scholar]
- 10.Kim J.H., Park Y.S., Chung C.G., Park K.S., Chung D.J., Kim H.J. Feasibility and utility of transradial cerebral angiography : experience during the learning period. Korean J Radiol. 2006;7:7–13. doi: 10.3348/kjr.2006.7.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laarman G., Muthusamy T.S., Swart H. Direct coronary stent implantation : safety, feasibility, and predictors of success of the strategy of direct coronary stent implantation. Cathet Cardiovasc Interv. 2001;52:443–448. doi: 10.1002/ccd.1099. [DOI] [PubMed] [Google Scholar]
- 12.Lee D.H., Ahn J.H., Jeong S.S., Eo K.S., Park M.S. Routine transradial access for conventional cerebral angiography : a single operator's experience of its feasibility and safety. Br J Radiol. 2004;77:831–838. doi: 10.1259/bjr/89933527. [DOI] [PubMed] [Google Scholar]
- 13.Levy E.I., Boulos A.S., Fessler R.D. Transradial cerebral angiography : an alternative route. Neurosurgery. 2002;51:335–340. ; discussion 340-342. [PubMed] [Google Scholar]
- 14.Matsumoto Y., Hokama M., Nagashima H. Transradial approach for selective cerebral angiography : technical note. Neurol Res. 2000;22:605–608. doi: 10.1080/01616412.2000.11740727. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto Y., Hongo K., Toriyama T., Nagashima H., Kobayashi S. Transradial approach for diagnostic selective cerebral angiography : results of a consecutive series of 166 cases. AJNR Am J Neuroradiol. 2001;22:704–708. [PMC free article] [PubMed] [Google Scholar]
- 16.Nohara A.M., Kallmes D.F. Transradial cerebral angiography : technique and outcomes. AJNR Am J Neuroradiol. 2003;24:1247–1250. [PMC free article] [PubMed] [Google Scholar]
- 17.Park S.H., Park J.C., Hwang J.H., Hwang S.K., Hamm I.S. Role of three-dimensional computed tomography angiography in the follow-up of patients with aneurysm clips. J Korean Neurosurg Soc. 2006;39:427–431. [Google Scholar]
- 18.Wu C.J., Hung W.C., Chen S.M. Feasibility and safety of transradial artery approach for selective cerebral angiography. Cathet Cardiovasc Interv. 2005;66:21–26. doi: 10.1002/ccd.20396. [DOI] [PubMed] [Google Scholar]