Abstract
Objective
To investigate the value of application of low-dose and optimized length CT scan on puncture results, complications and patients’ radiation dosage during CT-guided percutaneous biopsy of pulmonary nodules (PTNB).
Methods
A total of 231 patients with PTNB under CT guidance were collected. Low dose scanning utilized tube current of 20 mA as compared with 40 mA in conventional dosage. Optimized length in CT is defined as intentionally narrowing the range of CT scanning just to cover 25 mm (5 layers) around the target layer during needle adjustment. According to whether low-dose scans and optimized length scans techniques were utilized, patients were divided into three groups: conventional group (conventional sequence + no optimization), optimized length group (conventional sequence + optimized length), and low-dose optimized length group (low dose sequence + optimized length). The ED (effective dose), the DLP (dose length product), the average CTDIvol (Volume CT dose index), total milliampere second between subgroups were compared.
Results
Compared with the conventional group, ED, intraoperative guidance DLP, total milliseconds and operation time in the optimized length group were reduced by 18.2% (P=0.01), 37% (P=0.003), 17.5% (P=0.013) and 13.3% (P=0.021) respectively. Compared with the optimized length group, the ED was reduced by 87%, preoperative positioning, intraoperative guidance and postoperative review DLP were also reduced by 88%, total milliampere second was reduced by 79%, with an average CTDIvol was reduced by 86%, in the low-dose optimized length group (P<0.001 for all).
Conclusion
Optimizing the length during CT scanning can effectively reduce the intraoperative radiation dose and reduce the operation time compared with conventional plan; low-dose and optimized length CT scan can further reduce the total radiation dose compared with optimized length group with no differences on intraoperative complications, biopsy results and operation time.
Keywords: Lung biopsy, CT guided, Low dose, Radiation dose, Optimized scan
1. Introduction
With the clinical demand for pathological results of lung tumors and the application of genetic testing, the demand for lung tumor tissue specimens is increasing.1, 2, 3, 4 Among them, CT-guided percutaneous transthoracic needle biopsy (PTNB) of pulmonary nodules has the advantages of safety, effectiveness, and convenience and is widely used in clinical practice.4, 5, 6 Reportedly, 97.5% of PTNB procedures are guided by CT.5 In the PTNB guidelines proposed by a consensus of Chinese experts, CT has become the primary choice and the most common guidance modality.7 Though the Chinese Expert Consensus Guidelines do not mention the maximum allowable radiation dose for patients undergoing PTNB under CT guidance, the consensus statement and recommendations of the Korean Thoracic Radiology Society point out that the radiation dose of CT-guided PTNB should not exceed 2.7 mSv.8 The typical chest scanning scheme used in an imaging examination would not comply with the recommendation of the Korean expert consensus. Therefore, reducing the radiation dose during CT in PTNB to optimize radiation protection has become an important field of research.
2. Materials and methods
2.1. General information
A total of 231 patients who underwent PTNB between June 2019 and July 2020 in the CT1 Department of the Department of Minimally Invasive Intervention, Cancer Center, Sun Yat-sen University were retrospectively reviewed. Sun Yat-sen University Cancer Center Hospital Ethics Committee approved this study. This was a retrospective analysis of routine data and therefore we requested and were granted a waiver of individual informed consent from the ethics committee. According to different scan parameters and the length of optimization of the scan, the cohort was divided into three subgroups: conventional group (conventional sequence + no optimization; n = 74 cases), optimized-length group (conventional sequence + optimized-length; n = 72 cases), and low-dose optimized-length group (low-dose sequence + optimized-length; n = 85 cases). The baseline information for each patient was recorded. The CT-guided PTNB procedure was divided into the following three stages from the time of needle insertion to the time of needle retraction: preoperative localization, intraoperative guidance, and postoperative review.
2.2. Definition of scanning techniques
All PTNBs of the three groups of patients were performed using the Siemens SOMATOM Definition AS CT scanner. Written informed consent was obtained from all patients. The scanning pitch for all three groups was 1.2, the scanning layer thickness and layer spacing were 5 mm, and automatic tube current modulation (CARE Dose 4D) and automatic tube voltage selection (CARE kV) were adopted for all groups.
Conventional CT scanning is performed using a reference tube voltage of 120 kV, a reference tube current of 140 mA, and standard image reconstruction. In contrast, a low-dose optimized CT scan refers to CT scanning performed using a reference tube voltage of 120 kV and a reference tube current of 20 mA, with low-contrast image reconstruction.
The conventional length of CT scanning refers to scanning covering more than 30 mm (6 layers) around the layer of the designated puncture route during the procedure. Length optimization is defined as narrowing the range of CT scanning to cover 25 mm (five layers) around the target layer. In both the optimized-length group and low-dose optimized-length group, the optimal length plan was used for intraoperative guidance.
2.3. Radiation dose parameters and definitions
Volume CT dose index (CTDIvol): The CT dose index represents the dosage output of a single layer of radiation along the z-axis. Usually, a CT scan consists of many layers. Owing to the diffusivity of X-rays, the actual dose area covered in a single-slice scan will have a “tail area” at the edge of the layer in the z-axis. As the multi-layer scan has a dose superposition in the “tail area,” scientists put forward the concept of CTDIvol (measurement unit for both indices: mGy).
Dose-length product (DLP): DLP, measured in mGy∗cm, is a measure of CT tube radiation output/exposure. It is related to CTDIvol, but CTDIvol represents the dose through a slice of an appropriate phantom, whereas DLP accounts for the length of the radiation output along the z-axis (the long axis of the patient). DLP = (CTDIvol) × (scan length in cm) [units: mGy × cm].
Effective dose (ED): The effective dose represents the average radiation dose received by the whole body, as it considers the non-uniformity of the radiation dose received by different parts of the body. It is obtained based on the weighting factor (K) for different parts of the body. According to the European CT quality standard guidelines, K of the chest has an average value of 0.014 mSv/mGy × cm. ED = DLP × K [units: mSv].
Milliampere-second (mAs): The mAs represents the number of X-rays. An increase in mAs indicates an increase in the number of X-ray photons reaching the detector.
2.4. Baseline information and intraoperative parameters
The baseline information collected for each patient included sex, age, weight, height, body mass index (BMI), and intraoperative position. An interventional doctor and a CT technician jointly analyzed and recorded the intraoperative parameters, including the location and size of the puncture lesion, puncture depth, distance across the lung, number of adjustments, number of scans, bleeding, pneumothorax, and puncture results.
2.5. Statistical analysis
Statistical analyses were performed using SPSS Statistics 23.0. The clinicopathological characteristics of the three groups were compared using the Mann–Whitney U test (continuous variables) or chi-square test (categorical variables). The CT parameters of the three groups were compared using an independent-samples t-test. Univariate and multivariate analyses were performed using logistic regression analyses. All variables with p < 0.05 in the univariate analysis were subsequently included in the multivariable logistic regression model. Statistical significance was set at p < 0.05.
3. Results
3.1. General assessment
A total of 231 patients were enrolled: 141 men and 90 women, aged 18–85 years, with a median age of 59 years. The sex, age, weight, height, and BMI characteristics of the three groups of patients were added up separately for each group. There were no significant differences between the three groups (p > 0.05) (Table 1).
Table 1.
Comparison of basic information of the three groups of patients.
| basic information | Conventional group | optimized length group | Low-dose optimized length group | Con/Opti |
Opti/Low |
|---|---|---|---|---|---|
| P | P | ||||
| Gender(M/F) | 49/25 | 42/30 | 50/35 | 0.326 | 0.950 |
| Age(year) | 58.54 ± 12.24 | 59.18 ± 10.97 | 57.31 ± 11.67 | 0.609 | 0.245 |
| Weight(kg) | 61.77 ± 9.88 | 60.91 ± 10.09 | 59.08 ± 10.20 | 0.507 | 0.159 |
| Height (cm) | 165.31 ± 7.48 | 163.40 ± 7.93 | 162.88 ± 8.12 | 0.154 | 0.592 |
| BMI (kg/m2) | 22.56 ± 3.05 | 22.77 ± 3.08 | 22.21 ± 3.07 | 0.823 | 0.172 |
3.2. Comparison of intraoperative parameters between groups
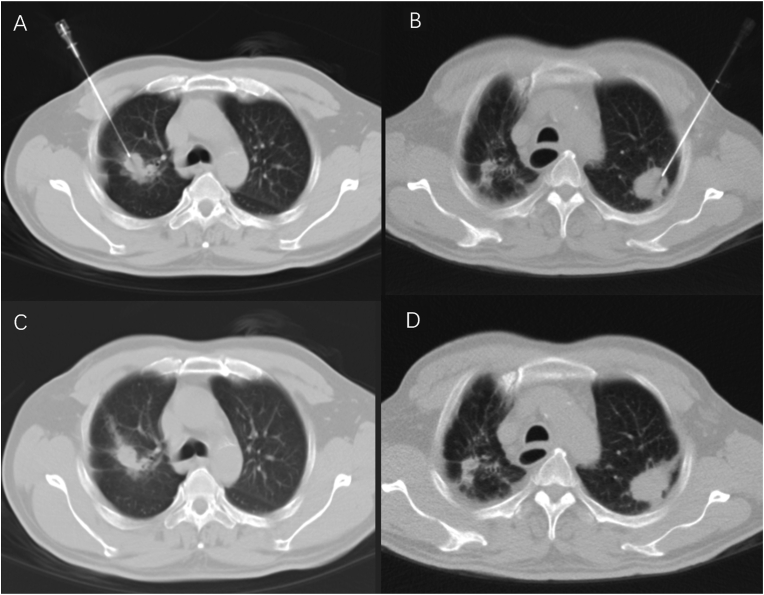
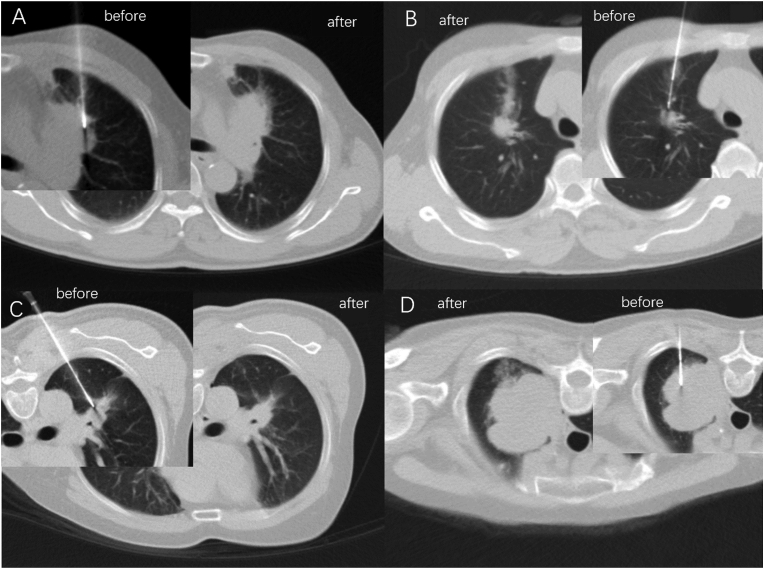
The intraoperative parameters of the three groups included the patient's position, location of lesion and its diameter, puncture depth, distance across lung, number of needle adjustments, number of scans, bleeding, pneumothorax, and puncture results. There were no significant differences between the three groups (p > 0.05) (Table 2). The quality of CT images of the three groups met the need for puncture operations (Fig. 1, Fig. 2).
Table 2.
Comparison of the information of the three groups of patients during puncture.
| Intraoperative condition | Conventional group | optimized length group | Low-dose optimized length group | Con/ Opti |
Opti/Low |
|---|---|---|---|---|---|
| P | P | ||||
| Biopsy needle (BARD/BD/ARGON) | 34/32/8 | 35/27/10 | 35/26/24 | 0.729 | 0.093 |
| Position (supine/prone) | 34/40 | 38/34 | 52/33 | 0.409 | 0.289 |
| Lesion location (right upper/middle/lower/left upper/lower) | 19/8/22/10/15 | 21/7/13/13/18 | 24/5/14/27/15 | 0.538 | 0.320 |
| Lesion size(cm) | 3.81 ± 2.38 | 3.19 ± 1.41 | 3.73 ± 1.87 | 0.229 | 0.094 |
| Puncture depth (cm) | 6.20 ± 1.94 | 6.27 ± 1.78 | 6.04 ± 1.75 | 0.474 | 0.363 |
| Distance across lung (cm) | 2.05 ± 1.98 | 2.23 ± 1.48 | 1.86 ± 1.54 | 0.196 | 0.122 |
| Number of adjustments | 2.89 ± 1.79 | 2.72 ± 1.53 | 2.59 ± 1.54 | 0.800 | 0.467 |
| Number of scans | 6.18 ± 2.48 | 5.78 ± 1.87 | 5.53 ± 1.74 | 0.684 | 0.345 |
| Bleeding (present vs absent) | 67/7 | 62/10 | 71/14 | 0.404 | 0.429 |
| Pneumothorax (present vs absent) | 64/10 | 57/15 | 73/12 | 0.240 | 0.404 |
| Puncture results (positive/suspicious/negative) | 59/6/9 | 58/3/11 | 75/1/9 | 0.554 | 0.315 |
Note: A positive in the puncture result indicates a confirmed malignant tumor, a suspected malignant tumor is not excluded, and a negative result indicates a non-malignant tumor.
Fig. 1.
A and C are pictures during CT guidance before and after puncture in the optimized length group, B and D are during CT guidance before and after puncture in the low-dose optimization length group. Both groups of pictures can clearly show the puncture needle and the lesion. The relationship of normal lung structure can also be clearly shown for postoperative review for identification of potential complications, such as needle bleeding.
Fig. 2.
A-D showed that the quality of CT pictures in low-dose optimization length group meet the demand of biopsy for lung lesions in different lobes and patients in different position.
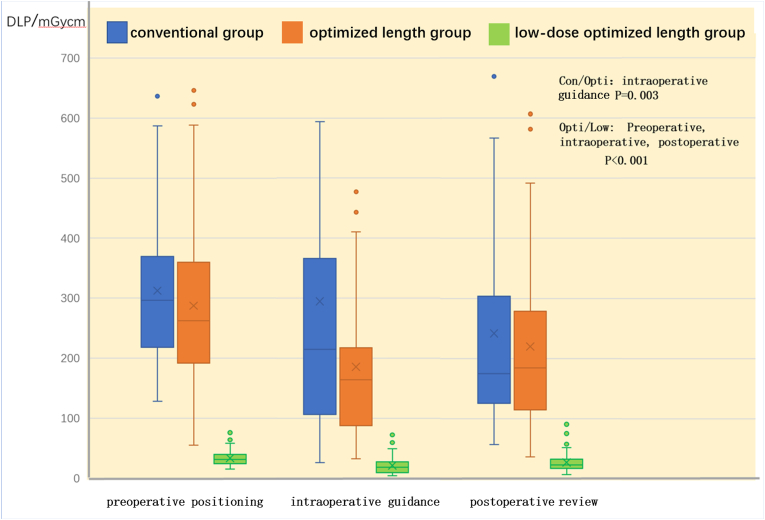
3.3. Radiation dose
The DLP distributions of the three groups during preoperative positioning, intraoperative guidance, and postoperative review are shown in Fig. 3. On comparison of the optimized-length group with the conventional group, we found that the intraoperative guidance DLP of the optimized-length group was reduced by 37% (p = 0.003); the ED and total mAs of the optimized-length group were reduced by 18.2% (p = 0.01) and 17.5% (p = 0.013), respectively; and the operation time was reduced by 13.3% (p = 0.021). The differences between the other items were not significant (p > 0.05).
Fig. 3.
Comparison of the distribution of DLP among the three groups in terms of preoperative positioning, intraoperative guidance and postoperative review.
On comparison of the low-dose optimized-length group with the optimized-length group, we found no significant difference in the operation time (p > 0.05); however, in the low-dose optimized-length group, the patient's total mAs was reduced by 79%; CTDIvol by 86% on average; ED by 87%; and preoperative positioning, intraoperative guidance, and postoperative review DLPs by 88% (p < 0.001) (Table 3).
Table 3.
Comparison of radiation dose and operation time among the three groups.
| Dose parameters | Conventional group | optimized length group | Low-dose optimized length group | Con/ Opti |
Opti/Low |
|---|---|---|---|---|---|
| P | P | ||||
| positioning DLP(mGy·cm) | 312.4 ± 143.9 | 287.5 ± 130.1 | 33.87 ± 11.99 | 0.274 | <0.001 |
| guided DLP(mGy·cm) | 294.3 ± 259.4 | 185.3 ± 157.4 | 21.34 ± 15.10 | 0.003 | <0.001 |
| review DLP(mGy·cm) | 241.7 ± 197.2 | 220.2 ± 141.3 | 27.10 ± 14.55 | 0.451 | <0.001 |
| Total mAs | 6211 ± 3043 | 5122 ± 2111 | 1070.6 ± 306.7 | 0.013 | <0.001 |
| Average CTDIvol(mGy) | 9.79 ± 3.75 | 9.44 ± 3.04 | 1.33 ± 0.38 | 0.531 | <0.001 |
| ED(mSv) | 11.95 ± 5.86 | 9.77 ± 4.07 | 1.23 ± 0.41 | 0.010 | <0.001 |
| Operation duration(min) | 25.85 ± 8.95 | 22.40 ± 7.45 | 21.42 ± 7.91 | 0.021 | 0.214 |
3.4. Factors affecting radiation dose
The ED results of 85 patients in the low-dose optimized-length group were divided into high and low groups based on the average value. Their baseline information and intraoperative parameters were analyzed using single factor analysis. The single factor analysis results for significant factors—weight, BMI, puncture depth, number of needle adjustments, pneumothorax, and total scan length—were subjected to a multivariate binary logistic regression analysis. Multivariate analysis showed that BMI and total scan length were independent factors affecting the radiation dose (Table 4).
Table 4.
binary logistic regression analysis of influencing factors of radiation dose in low dose optimized length group.
| Variable parameter | Standard error | Wald | P | Exp(B) | 95% CI of EXP(B) |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Univariate analysis | ||||||
| Weight(kg) | 0.029 | 11.451 | 0.001 | 1.103 | 1.042 | 1.167 |
| BMI (kg/m2) | 0.093 | 11.076 | 0.001 | 1.365 | 1.136 | 1.639 |
| Puncture depth (cm) | 0.154 | 10.507 | 0.001 | 1.647 | 1.218 | 2.226 |
| Number of needle adjustment | 0.179 | 10.769 | 0.001 | 1.802 | 1.268 | 2.561 |
| Pneumothorax (present vs absent) | 0.812 | 7.346 | 0.007 | 9.038 | 1.840 | 44.41 |
| Total scan length(cm) | 0.023 | 18.023 | <0.001 | 1.104 | 1.054 | 1.155 |
| multi-factor analysis | ||||||
| BMI (kg/m2) | 0.184 | 13.647 | <0.001 | 1.973 | 1.376 | 2.829 |
| Total scan length(cm) | 0.045 | 16.346 | <0.001 | 1.199 | 1.098 | 1.309 |
To analyze the factors that affect the scan range of patients in the low-dose optimized-length group, we divided the overall scan lengths during single procedure sessions of all patients in the low-dose optimized-length group into two groups based on the mean value. The single factor analysis results for significant factors, including lesion diameter, puncture depth, distance across lung, bleeding, and pneumothorax, were subjected to a multivariate binary logistic regression analysis. Multivariate analysis showed that distance across the lung, bleeding, and pneumothorax were independent factors affecting overall scan lengths during a single procedure session (Table 5).
Table 5.
Single factor binary logistic regression analysis of the total scan length of the low-dose optimization group.
| Variable parameter | Standard error | Wald | P | Exp(B) | 95% CI of EXP(B) |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Univariate analysis | ||||||
| Lesion diameter (cm) | 0.164 | 9.961 | 0.002 | 0.596 | 0.433 | 0.822 |
| Puncture depth (cm) | 0.150 | 9.260 | 0.002 | 1.578 | 1.176 | 2.116 |
| Distance across lung (cm) | 0.216 | 14.241 | <0.001 | 2.255 | 1.478 | 3.441 |
| Bleeding (present vs absent) | 0.698 | 7.977 | 0.005 | 7.181 | 1.828 | 28.202 |
| Pneumothorax (present vs absent) | 1.074 | 8.398 | 0.004 | 22.458 | 2.738 | 184.235 |
| multi-factor analysis | ||||||
| Distance across lung (cm) | 0.228 | 7.282 | 0.007 | 1.852 | 1.184 | 2.899 |
| Bleeding (present vs absent) | 0.765 | 8.086 | 0.004 | 8.810 | 1.966 | 39.475 |
| Pneumothorax (present vs absent) | 1.116 | 9.155 | 0.002 | 29.250 | 3.284 | 260.513 |
4. Discussion
Low-dose scanning is widely used during chest imaging examinations. Though the overall image quality is poor owing to the high natural contrast of the lungs, low-dose scanning does not affect the display of lung lesions and surrounding vicinity structures.9, 10, 11, 12 As most patients who undergo PTNB also have preoperative imaging data, this information is commonly sufficient for doctors to perform PTNB. Many researchers, who studied the use of the low-dose scanning scheme in PTNB, found that the most common method followed in clinical practice was to change the electrical parameters of the CT, such as reducing the tube current from 60 to 10 mAs or reducing the tube voltage from 120 to 100 kV.13, 14, 15 This study not only investigated the impact of low-dose scans on the radiation dose received by patients undergoing PTNB but also evaluated the impact of optimizing the scan length on the radiation dose received. The radiation dose received by PTNB patients was optimized by combining these two techniques to optimize patient radiation protection.
Apart from the impact related to the settings of the electrical parameters applied during CT, the length of the CT scan also has an impact on the radiation dose received by the patient.15, 16, 17 The results of the optimized-length group, whose scan length was optimized during the intraoperatively guided needle insertion stage, demonstrated a reduced effective radiation dose (p < 0.05). Not only was the scan length optimized in the low-dose optimized-length group but ultra-low tube current (reference value 20 mA) was also applied combined with automatic tube current and tube voltage technology to ensure image quality, thereby significantly reducing the effective radiation dose when compared with the other two groups.
Several factors affect the radiation dose received by the patient during CT-guided PTNB. It has been pointed out in a previously published report18 that the patient's body weight and the size of the lesion have an impact on the radiation dose in CT-guided percutaneous liver biopsy. The influence of body weight on radiation dose is mainly manifested in the automatic adjustment of CT scanning parameters. At present, the techniques of automatic tube current and tube voltage in CT scanning are very mature19 and can automatically adjust corresponding parameters based on the size and density of the scanned body. The results of the independent factors affecting the total radiation dose in our study were in line with those of previous studies.
In summary, the optimized-length scan can effectively reduce the DLP produced during PTNB and thereby reduce the effective radiation dose received by the patient. When combined with low-dose scanning, the effective radiation dose received by the patient can be further reduced, with no increase in intraoperative complications and no changes in puncture results. Therefore, the low-dose scanning scheme combined with the optimized-length scanning scheme is worthy of promotion in CT-guided PTNB.
Declaration of competing interest
The authors declare no conflict of interest. Acknowledgements This work was supported by grants from National Natural Science Foundation of China (No. 81801804).
References
- 1.Fabrizio F.P., Sparaneo A., Centra F. Methylation density pattern of KEAP1 gene in lung cancer cell lines detected by quantitative methylation specific PCR and pyrosequencing. Int J Mol Sci. 2019;20:2697. doi: 10.3390/ijms20112697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jamshidi N., Huang D., Abtin F.G. Genomic adequacy from solid tumor core needle biopsies of ex vivo tissue and in vivo lung masses: prospective study. Radiology. 2017;282:903–912. doi: 10.1148/radiol.2016132230. [DOI] [PubMed] [Google Scholar]
- 3.Mendoza D.P., Dagogo-Jack I., Chen T. Imaging characteristics of BRAF-mutant non-small cell lung cancer by functional class. Lung Canc. 2019;129:80–84. doi: 10.1016/j.lungcan.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Lee C., Guichet P.L., Abtin F. Percutaneous lung biopsy in the molecular profiling era: a survey of current practices. J Thorac Imag. 2017;32:63–67. doi: 10.1097/RTI.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 5.Tavare A.N., Hare S.S., Miller F.N.A. A survey of UK percutaneous lung biopsy practice: current practices in the era of early detection, oncogenetic profiling, and targeted treatments. Clin Radiol. 2018;73:800–809. doi: 10.1016/j.crad.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Capalbo E., Peli M., Lovisatti M. Trans-thoracic biopsy of lung lesions: FNAB or CNB? Our experience and review of the literature. Radiol Med. 2014;119:572–594. doi: 10.1007/s11547-013-0360-1. [DOI] [PubMed] [Google Scholar]
- 7.Guo Z., Shi H., Li W. Chinese multidisciplinary expert consensus: guidelines on percutaneous transthoracic needle biopsy. Thorac Cancer. 2018;9:1530–1543. doi: 10.1111/1759-7714.12849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoon S.H., Lee S.M., Park C.H. Clinical practice guideline for percutaneous transthoracic needle biopsy of pulmonary lesions: a consensus statement and recommendations of the Korean society of thoracic Radiology. Korean J Radiol. 2021. 2020;22:263–280. doi: 10.3348/kjr.2020.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hu-Wang E., Schuzer J.L., Rollison S. Chest CT scan at radiation dose of a posteroanterior and lateral chest radiograph series: a proof of principle in lymphangioleiomyomatosis. Chest. 2019;155:528–533. doi: 10.1016/j.chest.2018.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Svahn T.M., Sjöberg T., Ast J.C. Dose estimation of ultra-low-dose chest CT to different sized adult patients. Eur Radiol. 2019;29:4315–4323. doi: 10.1007/s00330-018-5849-5. [DOI] [PubMed] [Google Scholar]
- 11.Shieh Y., Bohnenkamp M. Low-dose CT scan for lung cancer screening: clinical and coding considerations. Chest. 2017;152:204–209. doi: 10.1016/j.chest.2017.03.019. [DOI] [PubMed] [Google Scholar]
- 12.Tang H., Liu Z., Hu Z. Clinical value of a new generation adaptive statistical iterative reconstruction (ASIR-V) in the diagnosis of pulmonary nodule in low-dose chest CT. Br J Radiol. 2019;92 doi: 10.1259/bjr.20180909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee H.N., Lee S.M., Choe J. Diagnostic performance of CT-guided percutaneous transthoracic core needle biopsy using low tube voltage (100 kVp): comparison with conventional tube voltage (120 kVp) Acta Radiol. 2018;59:425–433. doi: 10.1177/0284185117719589. [DOI] [PubMed] [Google Scholar]
- 14.Fu Y.F., Li G.C., Xu Q.S. Computed tomography-guided lung biopsy: a randomized controlled trial of low-dose versus standard-dose protocol. Eur Radiol. 2020;30:1584–1592. doi: 10.1007/s00330-019-06464-6. [DOI] [PubMed] [Google Scholar]
- 15.Kallianos K.G., Elicker B.M., Henry T.S. Instituting a low-dose CT-guided lung biopsy protocol. Acad Radiol. 2016;23:1130–1136. doi: 10.1016/j.acra.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huo D., Kiehn M., Scherzinger A. Investigation of low-dose CT lung cancer screening scan "Over-Range" issue using machine learning methods. J Digit Imag. 2019;32:931–938. doi: 10.1007/s10278-019-00233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chintapalli K.N., Montgomery R.S., Hatab M. Radiation dose management: part 1, minimizing radiation dose in CT-guided procedures. AJR Am J Roentgenol. 2012;198:W347–W351. doi: 10.2214/AJR.11.7958. [DOI] [PubMed] [Google Scholar]
- 18.Li J., Udayasankar U.K., Carew J. CT-guided liver biopsy: correlation of procedure time and radiation dose with patient size, weight, and lesion volume and depth. Clin Imag. 2010;34:263–268. doi: 10.1016/j.clinimag.2009.06.029. [DOI] [PubMed] [Google Scholar]
- 19.MacDougall R.D., Kleinman P.L., Callahan M.J. Size-based protocol optimization using automatic tube current modulation and automatic kV selection in computed tomography. J Appl Clin Med Phys. 2016;17:328–341. doi: 10.1120/jacmp.v17i1.5756. [DOI] [PMC free article] [PubMed] [Google Scholar]