Abstract
Background and Aims
In the United States, respiratory infections due to respiratory syncytial virus (RSV) cause an estimated 57 000 hospitalizations annually among children aged <5 years and 177 000 hospitalizations among adults aged ≥65 years. RSV‐associated deaths are less well described. It will be important to establish a baseline of RSV‐coded deaths prior to the introduction of vaccines, immunoprophylaxis products, and anti‐viral therapies currently in development.
Methods
US death certificate data for all ages from 2005 through 2016 were compiled through the National Center for Health Statistics. Deaths with International Classification of Diseases codes of J12.1 (RSV‐pneumonia), J20.5 (RSV‐bronchitis), or J21.0 (RSV‐bronchiolitis) assigned as either the underlying cause of death or a contributing cause of death were considered “RSV‐associated” for this analysis.
Results
Among 30.5 million deaths, 1001 (.003%) were assigned an RSV‐associated cause of death as follows: 697 (69.6%) RSV‐pneumonia, 277 (27.7%) RSV‐bronchiolitis, 17 (1.7%) RSV‐bronchitis, and 10 (1.0%) with multiple RSV‐associated causes. Most deaths were among children <5 (47.8%) and adults ≥50 (40.4%) years of age. Almost half (46.8%) had an RSV‐associated cause as the primary underlying cause of death. The average annual number of RSV‐associated deaths did not significantly change among those aged <5 and 5 to 49 years. However, RSV‐pneumonia deaths among adults aged ≥50 years increased from 17.6 in 2005 to 2012 to 57.3 in 2013 to 2016 (P value <.0001).
Conclusions
From 2005 to 2016, the number of recorded RSV‐associated deaths increased, primarily due to greater RSV‐associated pneumonia deaths among older adults since 2013. The reasons for this increase are not clear but likely reflect increased testing for RSV among adults. The number of RSV‐associated deaths according to death certificates compared with estimates derived from active, laboratory‐confirmed surveillance and models using hospital administrative data suggests that counts from death certificates are a large underestimation, particularly among adults.
Keywords: death certificates, mortality, human, respiratory syncytial virus, United States
1. BACKGROUND
Respiratory syncytial virus (RSV) is a leading cause of morbidity in the United States, particularly at the extremes of age, causing an estimated 57 000 hospitalizations annually among children aged <5 years and 177 000 hospitalizations among adults aged ≥65 years. 1 , 2 With new vaccines, immunoprophylaxis products, and anti‐viral therapies in development to reduce RSV‐associated morbidity and mortality, better documentation of the incidence of RSV‐associated mortality is needed to help interpret changes that may be observed over time. This report describes deaths among all ages from 2005 through 2016 using death certificate data from the National Center for Health Statistics.
2. METHODS
Multiple‐cause US mortality data from 2005 through 2016 were obtained from the National Center for Health Statistics of the Centers for Disease Control and Prevention. 3 Each record included in these datasets includes one coded underlying cause of death (CoD), defined by the World Health Organization as “the disease or injury which initiated the train of events leading directly to death….”. Records also include up to 20 additional contributing CoD codes. Deaths considered “RSV‐associated” had one of the following International Classification of Diseases 10th revision (ICD‐10) codes assigned as either the primary underlying cause of death or a contributing CoD: J12.1 (RSV‐pneumonia), J20.5 (RSV‐bronchitis), or J21.0 (RSV‐bronchiolitis). ICD‐10 codes have been used for CoD classification since 1999, and the three RSV‐specific codes described here were consistently used throughout the 12‐year period for this report. The billable ICD‐10 code for “Respiratory syncytial virus as the cause of diseases classified elsewhere” (B97.4) is not used by the National Center for Health Statistics for CoD classifications.
RSV‐associated deaths were stratified by age, sex, and race/ethnicity, and were also analyzed by primary underlying or contributing CoD. For deaths with an RSV‐associated CoD, the specific primary underlying causes were grouped into broader medical categories for comparisons across age groups. Chi‐square statistics were calculated to compare unadjusted frequencies, and P values <.05 were considered statistically significant.
This work was considered public health surveillance by the Centers for Disease Control and Prevention (CDC), and no formal Institutional Review Board oversight was required.
3. RESULTS
From 2005 to 2016, among 30.5 million US deaths, 1001 (.003%) were assigned a primary underlying or contributing RSV‐associated CoD: 697 (69.6%) were assigned an RSV‐pneumonia code, 277 (27.7%) an RSV‐bronchiolitis code, 17 (1.7%) an RSV‐bronchitis code, and 10 (1%) were assigned more than one RSV‐associated cause (Table 1). Among the 1001 with an RSV‐associated CoD, 468 (46.8%) had an RSV‐associated code listed as the primary underlying CoD, and the distribution of the three causes in this subset was similar to that observed among the broader group (62.6%, 35.0%, and 2.4%, respectively). Most of the RSV‐associated deaths (88.9%) occurred during the months of November through April.
TABLE 1.
Characteristics (n, column %) of RSV‐associated deaths by age groups, 2005 to 2016
| <1 year (n = 315) | 1‐4 years (n = 163) | 5‐19 years (n = 67) | 20‐49 years (n = 51) | ≥50 years (n = 405) | All ages (N = 1001) | |
|---|---|---|---|---|---|---|
| Male | 169 (53.7) | 69 (42.3) | 34 (50.1) | 27 (52.9) | 182 (44.9) | 481 (48.1) |
| Race/ethnicity a : | ||||||
| Non‐Hispanic White | 135 (42.9) | 76 (46.6) | 39 (58.2) | 36 (70.6) | 332 (82.0) | 618 (61.7) |
| Non‐Hispanic Black | 80 (25.4) | 26 (16.0) | 10 (14.9) | 6 (11.8) | 27 (6.7) | 149 (14.9) |
| Non‐Hispanic Other | 19 (6.0) | 8 (4.9) | 5 (7.5) | 1 (2.0) | 20 (4.9) | 53 (5.3) |
| Hispanic (any race/country of origin) | 79 (25.1) | 53 (32.5) | 13 (19.4) | 8 (15.7) | 26 (6.4) | 179 (17.9) |
| Primary underlying OR contributing CoD b : | ||||||
| RSV‐pneumonia (ICD‐10 code = J12.1) | 148 (47.0) | 74 (45.4) | 56 (83.6) | 49 (96.1) | 370 (91.4) | 697 (69.6) |
| RSV‐bronchitis (ICD‐10 code = J20.5) | 5 (1.6) | 3 (1.8) | 0 (0.0) | 0 (0.0) | 9 (2.2) | 17 (1.7) |
| RSV‐bronchiolitis (ICD‐10 code = J21.0) | 158 (50.2) | 84 (51.5) | 9 (13.4) | 2 (3.9) | 24 (5.9) | 277 (27.7) |
| RSV listed as the primary underlying CoD | 203 (64.4) | 77 (47.2) | 26 (38.8) | 14 (27.5) | 148 (36.5) | 468 (46.8) |
Abbreviations: CoD, cause of death; ICD‐10, International Classification of Diseases 10th revision; RSV, respiratory syncytial virus.
Race/ethnicity data were missing for two individuals.
Excludes 10 deaths with more than 1 RSV‐associated contributing CoD.
Among the 1001 reported deaths, 31.4% were aged <1 year, 16.3% were 1 to 4 years, and 40.5% were ≥50 years (Table 1). Among those aged <1 year, the number of deaths was highest among those <6 months and peaked at 1 month. Among those aged ≥50 years, the greatest number of deaths was reported in those aged 80 to 89 years (Figure 1). Almost half of all persons (48.1%) were male, 61.7% were non‐Hispanic white, 17.9% were Hispanic (any race), and 14.9% were non‐Hispanic Black. Race and ethnicity distributions differed by age groups. With increasing age, the race/ethnicity distribution shifted toward a greater proportion of non‐Hispanic Whites and fewer Hispanics and non‐Hispanic Blacks (both P values were <.0001).
FIGURE 1.
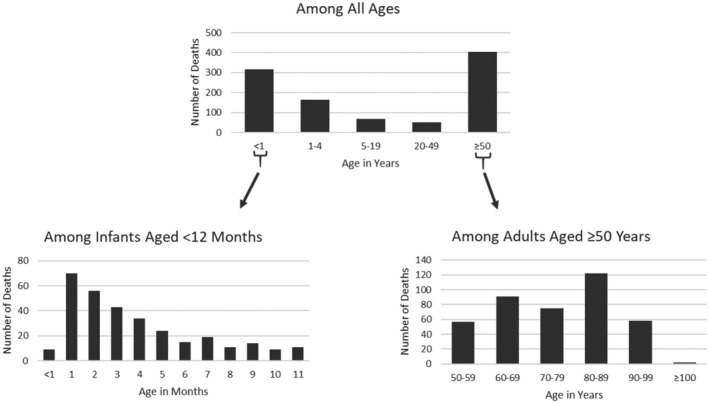
Number of RSV‐associated deaths according to US death certificates, by age groups (2005‐2016)
The specific RSV‐associated CoD on the death certificates also differed by age. Among children aged <5 years, the CoDs were nearly evenly divided between RSV‐bronchiolitis (50.6%) and RSV‐pneumonia (46.4%), whereas the code for RSV‐pneumonia was assigned for almost all (90.8%) of the RSV‐associated deaths among those aged ≥5 years. RSV‐bronchitis as a CoD was rarely documented in any age group (Table 1).
Among those with an RSV‐associated CoD, the specific primary underlying CoD listed on death certificates varied by age. Having RSV listed as the primary underlying CoD was more likely for children aged <1 (64.4%) or 1 to 4 years (47.2%) than for children aged 5 to 19 years (38.8%), adults aged 20 to 49 years (27.5%) or adults aged ≥50 years (36.5%) (Table 1). Among children aged <5 years with an RSV‐associated CoD, the most common primary underlying CoD was RSV (58.6%) followed by a variety of mainly chronic, genetic, and congenital conditions; no other single category of illness contributed more than 6% of the total. Among those aged 5 to 49 and adults aged ≥50 years with an RSV‐associated CoD, RSV accounted for just over a third of the reported primary underlying causes of death (33.9% and 36.5% respectively), followed by blood and solid organ cancers for roughly a quarter of the deaths in each age group (26.3% and 24.7% respectively). The next largest category was neurologic/neuromuscular conditions (11.0%) among those aged 5 to 49 years and cardiovascular disease (9.6%) among those aged ≥50 years. (Figure 2).
FIGURE 2.
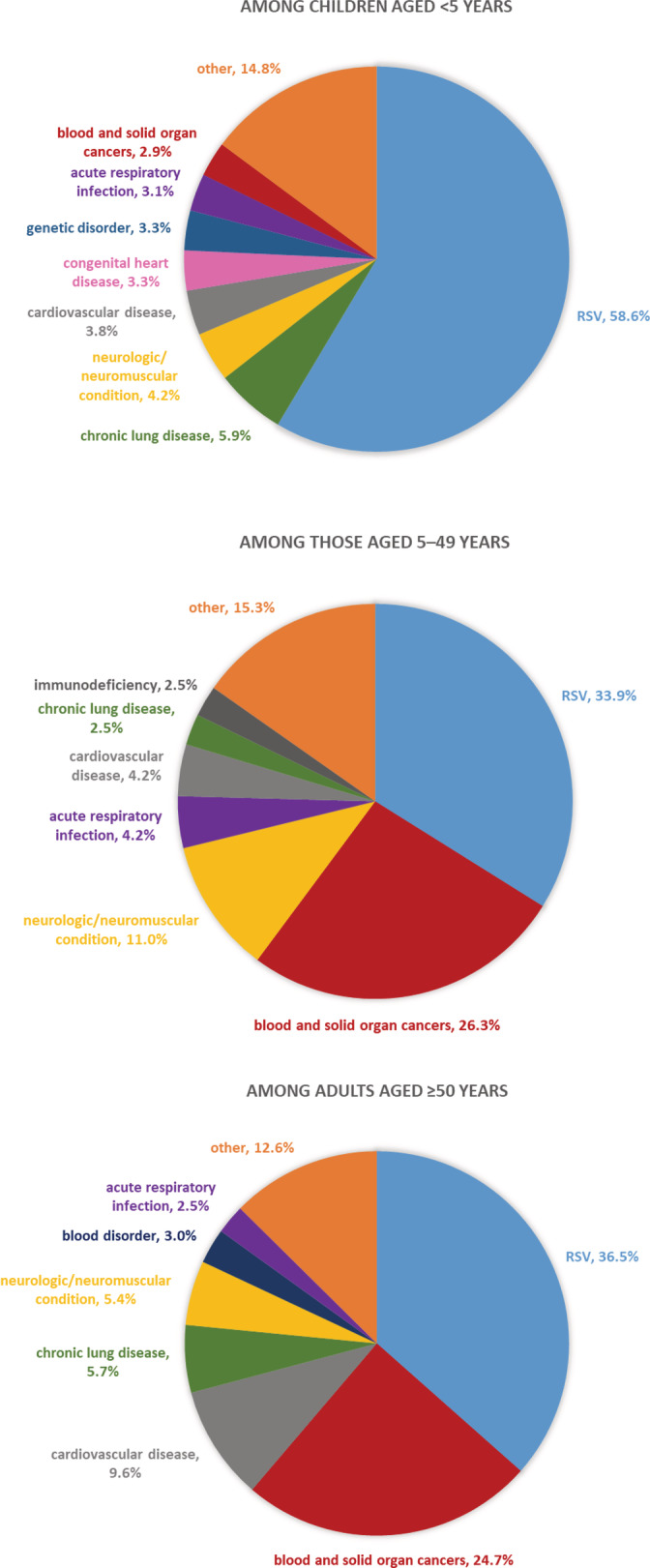
Primary underlying cause of death (%) among those with an RSV‐associated cause according to US death certificates, by age groups (2005‐2016)
Over the 12 years of observation, the number of RSV‐associated deaths did not significantly change among those aged <1, 1 to 4, and 5 to 49 years (Figure 3). There was an overall increase in the number of RSV‐associated deaths among adults aged ≥50 years, particularly for deaths assigned the ICD‐10 code for RSV‐pneumonia. The average annual number of RSV‐pneumonia deaths among adults aged ≥50 years increased from 17.6 in 2005 to 2012 to 57.3 in 2013 to 2016 (P value <.0001).
FIGURE 3.
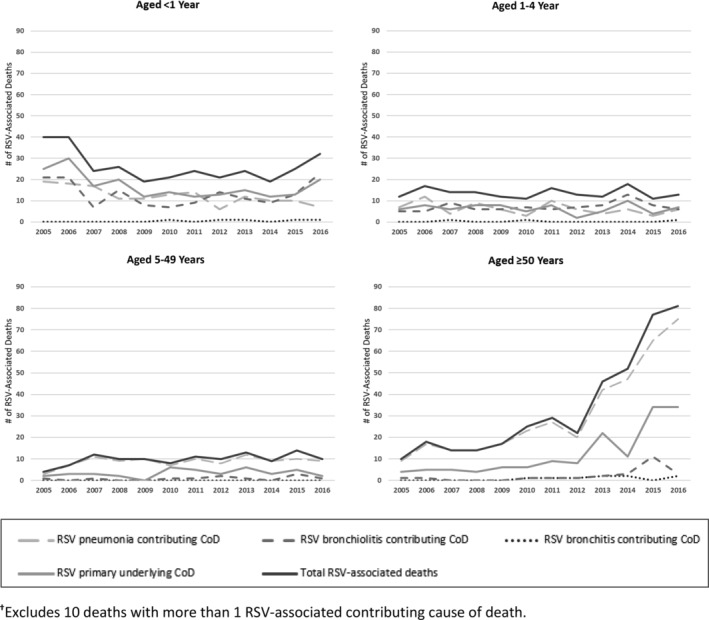
RSV‐associated deaths by contributing cause† (RSV‐pneumonia, RSV‐bronchiolitis, RSV‐bronchitis, RSV primary underlying, and total RSV‐associated deaths), four age groups (<1, 1‐4, 5‐49, and ≥50 years), and year of death (2005‐2016)
4. DISCUSSION
Reports of RSV‐coded deaths increased from 2005 to 2016 and coincided with the typical annual seasonality of RSV circulation in the United States. 4 The rise in deaths was mostly due to increases in coded RSV‐associated pneumonia deaths among older adults in recent years, which may reflect increased diagnostic testing among adults rather than a true increase in fatal RSV‐associated illnesses. Consistent with RSV hospitalization rates, most deaths occurred at the extremes of age, with nearly half of deaths occurring among those aged <5 years and 40% among those aged ≥50 years. 1 , 2 , 5 Similarly, deaths among those aged <5 years were especially concentrated among those aged <6 months.
Death certificate data provide one valuable way of tracking trends in RSV mortality and the potential impact of interventions, but likely underestimate RSV‐associated mortality. Active surveillance for acute respiratory infections that included laboratory confirmation of RSV estimated about 10 000 to 14 000 RSV‐associated deaths annually among adults aged >65 years. 2 Models using hospital administrative data estimate 100 to 500 deaths annually among children aged <5 years. 6 When compared with the total number of RSV‐associated deaths according to death certificates over the 12 years in this report (348 for adults aged >60 years and 478 for children aged <5 years), the underestimate based on death certificates appears especially pronounced among adults. People of all ages with severe RSV‐associated illness who are not treated in a hospital before dying are unlikely to be tested for RSV and are therefore less likely to be assigned an RSV‐associated CoD. Among those who are hospitalized, the underestimate may be more pronounced among adults than children because of a lack of recognition that RSV can cause severe disease in adults. 7 Also, since adults have a higher prevalence of co‐morbidities, clinicians may focus more on complications due to concurrent or underlying health conditions. In one study, even when hospitalized adults tested positive for RSV, only about half had an RSV‐specific code listed in their discharge diagnosis. 5 There is no recommendation to conduct diagnostic testing for RSV because it generally does not impact clinical care, but the use in recent years of multiplex molecular respiratory panels that include RSV has likely led to an increase in testing. 5 In addition, it should be noted that several RSV vaccines for adults have entered clinical trials in recent years. The resulting increase in clinician awareness regarding RSV as a potential cause of serious illness combined with the increase in availability of RSV testing is likely the reason for the observed increase in RSV‐coded deaths among adults and overall. While increased testing is beneficial for infection control in hospitals and congregate living settings, strengthens respiratory virus surveillance in general, and improves the accuracy of disease burden and mortality estimates in particular, changes in testing practices add to the challenge of interpreting changing trends in death certificate data.
The use of death certificate data to measure RSV‐associated mortality has several additional limitations. While ICD‐10 codes were consistently used throughout the study period, the CoDs recorded may not reflect the true primary underlying or contributing CoD. For instance, clinicians may not correctly diagnose a condition or may not accurately record the primary underlying or contributing causes. In addition, while the information included in death certificate data may help identify populations to target for interventions by contributing to a better understanding of factors such as age, race, and access to care that could impact a person's risk for RSV‐associated deaths, death certificates do not provide enough detailed clinical information to fully assess underlying medical conditions associated with risk of death.
RSV‐associated death is not a nationally notifiable condition and RSV is not a reportable condition in most jurisdictions. Therefore, carrying out systematic surveillance efforts at the national level is challenging. However, in 2018, the Council of State and Territorial Epidemiologists (CSTE) approved a position statement that established a standardized case definition for use by jurisdictions that choose to carry out investigations of potential RSV‐associated deaths. 8 The main clinical criteria for case classification stipulate that the death must result from a clinically compatible illness that was confirmed to be RSV by an appropriate laboratory or rapid diagnostic test and that there should be no period of complete recovery between the illness and the death. Additional guidance is provided regarding appropriate confirmatory laboratory evidence and case ascertainment approaches. CDC can also now receive electronic notifications of RSV‐associated deaths from state and local health departments via the National Notifiable Diseases Surveillance System.
5. CONCLUSION
More accurate assessment of RSV‐associated deaths and establishing an incidence baseline before the licensure of new products for children and adults will aid in more fully understanding the impact of new interventions. RSV‐coded deaths will likely be more useful for ascertaining the impact of interventions in young children than among adults since a larger percentage of applicable deaths are being captured for children in these mortality data and these reports have remained relatively stable over time. In adults, however, the percentage of deaths captured by RSV‐associated CoD codes on death certificate is substantially lower and the diagnostic testing practices are changing over time. Therefore, it will be more challenging to interpret trends and the impact of interventions among adults using these data alone. Surveillance for RSV‐associated deaths requires a multifaceted approach including (a) continued monitoring of death certificate data, (b) measuring deaths through active respiratory surveillance systems with laboratory confirmation of cases, and (c) case notifications from state health departments to CDC using the CSTE case definition for an RSV‐associated death. Despite the challenges of interpreting death certificate data, efforts should be made to improve the completeness and accuracy of this one piece of the larger picture. The ability to compare any changes in the trends of RSV‐associated deaths reported through various data sources will support a better understanding of the key factors leading to these deaths within the context of new interventions and treatments in coming years.
FUNDING
This work was supported by the Centers for Disease Control and Prevention.
AUTHOR CONTRIBUTIONS
Conceptualization: Mila Prill, Gayle Langley, Amber Winn, Susan Gerber.
Formal Analysis: Mila Prill, Gayle Langley.
Supervision: Gayle Langley, Susan Gerber.
Writing—Reviewing and Editing: Mila Prill, Gayle Langley, Amber Winn, Susan Gerber.
Writing—Original Draft Preparation: Mila Prill.
All authors have read and approved the final version of the manuscript.
The lead author, Mila Prill, had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
TRANSPARENCY STATEMENT
Mila Prill also affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Prill MM, Langley GE, Winn A, Gerber SI. Respiratory syncytial virus‐associated deaths in the United States according to death certificate data, 2005 to 2016. Health Sci Rep. 2021;4:e428. doi: 10.1002/hsr2.428
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding information Centers for Disease Control and Prevention
DATA AVAILABILITY STATEMENT
The data that support the overarching findings of this report are available in the CDC Wonder Online Database (Multiple Cause of Death 1999‐2019) at http://wonder.cdc.gov/mcd-icd10.html. Some of the detailed data used for this report are not publicly available due to privacy or ethical restrictions. These additional data are provided in restricted‐use files upon special request and approval from the National Center for Health Statistics Division of Vital Statistics. Restrictions apply to the availability of these additional data, which were used under the terms of a data use agreement for this project.
REFERENCES
- 1. Hall CB, Weinberg GA, Iwane MK, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009;360(6):588‐598. doi: 10.1056/NEJMoa0804877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high‐risk adults. N Engl J Med. 2005;352(17):1749‐1759. doi: 10.1056/NEJMoa043951 [DOI] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention . National Center for Health Statistics. Public Use Multiple‐Cause Mortality File (2005‐2016) SAS Database, released 2018.
- 4. Rose EB, Wheatley A, Langley G, Gerber S, Haynes A. Respiratory syncytial virus seasonality—United States, 2014–2017. MMWR Morb Mortal Wkly Rep. 2018;67(2):71‐76. doi: 10.15585/mmwr.mm6702a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Datta S, Walsh EE, Peterson DR, Falsey AR. Can analysis of routine viral testing provide accurate estimates of respiratory syncytial virus disease burden in adults? J Infect Dis. 2017;215(11):1706‐1710. doi: 10.1093/infdis/jix196 [DOI] [PubMed] [Google Scholar]
- 6. Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179‐186. doi: 10.1001/jama.289.2.179 [DOI] [PubMed] [Google Scholar]
- 7. Allen KE, Chommanard C, Haynes AK, Erdman DD, Gerber SI, Kim L. Respiratory syncytial virus testing capabilities and practices among National Respiratory and enteric virus surveillance system laboratories, United States, 2016. J Clin Virol. 2018;107:48‐51. doi: 10.1016/j.jcv.2018.08.009 [DOI] [PubMed] [Google Scholar]
- 8. CSTE Standardized Case Definition for Surveillance of RSV‐Associated Mortality . 2018 Position Statement 18‐ID‐01. https://cdn.ymaws.com/www.cste.org/resource/resmgr/2018_position_statements/18-ID-01.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the overarching findings of this report are available in the CDC Wonder Online Database (Multiple Cause of Death 1999‐2019) at http://wonder.cdc.gov/mcd-icd10.html. Some of the detailed data used for this report are not publicly available due to privacy or ethical restrictions. These additional data are provided in restricted‐use files upon special request and approval from the National Center for Health Statistics Division of Vital Statistics. Restrictions apply to the availability of these additional data, which were used under the terms of a data use agreement for this project.


