Abstract
Background and Aims:
Inadequately managed pain due to multiple rib fractures (MRFs) can lead to atelectasis, pneumonia, prolonged ICU stay thereby leads to significant morbidity, morbidity and cost of treatment. Opioids, non-steroidal anti-inflammatory drugs and regional anaesthesia techniques like thoracic epidural or paravertebral blocks, intercostal nerve blocks are used to manage pain. Serratus anterior plane block (SAPB) is an ultrasound (US) guided interfascial plane block which has been used in managing pain due to MRFs. In this retrospective study, we compared analgesic efficacy and 24 hr fentanyl consumption in patients with MRFs who were managed with continuous SAPB versus patients who were managed with fentanyl infusion alone.
Material and Methods:
After Institutional Ethics Committee approval, we retrospectively collected data of 72 patients (38 in SAPB group and 34 in fentanyl group). Demographic data, VAS scores and 24 hrs fentanyl consumption was analysed in both groups.
Results:
There were statistically significant lower pain scores in patients of SAPB group when compared to that of fentanyl group (p=0.001) and in 24 hrs fentanyl consumption in patients who received continuous SAPB versus that in fentanyl group(p=0.001). No complications were observed in patients who received US guided SAPB.
Conclusion:
US guided SAPB is an opioid sparing, effective interfascial plane block which is safe and should be considered early in all patients who sustain MRFs. Continuous SAPB by placing a catheter can provide pain relief for longer duration, facilitate early mobilization, physiotherapy and early ICU discharge.
Keywords: Fentanyl, fracture, nerve block, pain relief, ribs, serratus anterior, ultrasound
Introduction
Multiple rib fractures (MRFs) lead to excruciating pain and splinting of multiple ribs, unable to breathe adequately and cough leading to significant morbidity and mortality of trauma patients, particularly in patients with poor respiratory reserve.[1,2,3,4,5] Untreated pain leads to basal atelectasis, pneumonia, and a reduction in functional residual capacity. These factors contribute towards a decreased lung compliance, ventilation-perfusion mismatch, hypoxemia, and respiratory distress. Therefore, effective pain relief remains the cornerstone of management to prevent serious respiratory complications. Patients can have concomitant head, internal thoracic, intra-abdominal, and limb injuries resulting in poor clinical outcomes.[6,7,8] The number of rib fractures >3, rib fracture locations, bilateral rib fractures, intraparenchymal pulmonary injuries, flail chest, and a first rib fracture influence the mortality rates.[9,10,11,12]
The involvement of acute pain services in MRFs is based on “Rib Fracture score”.[13] Rib fracture score = (breaks × sides) + age factor. “Breaks” is the total number of fractures to the rib. Score of 1 is for unilateral fractures and 2 for bilateral fractures. Age is factored into the equation due to an increased risk of complications (age factor = 0 if <50 years; 1 if 51–60 years; 2 if 61–70 years; 3 if 71–80 years; 4 if above 80 years). A score >7, requires the involvement of acute pain team.
Serratus anterior plane block (SAPB) is an ultrasound (US) guided interfascial plane block that has been used successfully in managing acute pain due to MRFs.[14]
We hypothesized that a continuous SAPB would be more effective in managing pain dueto MRFs. The primary outcome was to compare pain scores in patients who received SAPB versus those who were managed with fentanyl infusion.The secondary objectives were to compare 24 hrs fentanyl infusion and complications if any.
The purpose of this study was to address and establish the role of continuous SAPB (CSAPB) in managing pain due to lateral rib fractures.
Material and Methods
We performed a retrospective cohort study in patients who sustained MRFs and were managed with either SAPB or fentanyl infusion. We retrospectively analyzed data of patients who sustained lateral rib fractures from 2016-2019 after Institutional Ethics Committee approval. All patients had a Rib fracture score of more than 7. Computerized tomography (CT) scan was done for all patients. We retrieved data of 38 patients who received a SAPB (henceforth referred to as group S) and 34 patients were treated with intravenous (IV) infusion of fentanyl (henceforth referred to as group F) after a bolus dose. Patients who along with MRFs sustained other injuries like intra-abdominal, limb injuries but were not serious or considered for an immediate surgical intervention were included in the analysis. Patients with multiple injuries (intra-thoracic, intra-abdominal, lower, or upper limb) and who underwent surgeries for the same were not analyzed. Patients with head injuries were excluded from data collection. Patients in both groups had associated injuries like intrathoracic, intra-abdominal, upper, and lower limb injuries which were for observation and not for any intervention [Tables 1 and 2]. Patients who sustained posterior rib fractures were managed with US-guided erector spinae plane block (ESPB) and were not included in analysis.
Table 1.
Showing demographic data (age, gender) and comparison of associated injuries along with fracture ribs
| Group F (n=34) | Group S (n=38) | |
|---|---|---|
| Age (years) | 28-65 (42.38) | 32-74 (50.23) |
| Gender | M=22, F=12 | M=21, n=17 |
| Intra-thoracic injuries | 4 | 5 |
| Intra-abdominal injuries | 0 | 1 |
| Upper limb injuries | 7 | 13 |
| Lower limb injuries | 12 | 5 |
| Head injuries | 0 | 0 |
Table 2.
Showing comparison of rib fractures in either groups
| No of Rib Fractures | Group F (n=34) | Group S (n=38) |
|---|---|---|
| Left | n=25 | n=22 |
| Right | n=9 | n=16 |
| Bilateral | nil | nil |
| First Rib | n=1 | n=3 |
Group S
Patients in group S received US-guided SAP block within 4–6 h of admission in the ICU after an informed consent. With patient in supine position, linear US probe (5–12 mHz Sonosite, M-Turbo; Sonosite Inc.) was placed longitudinally in the midaxillary line at the level of 4–5 ribs. The ribs were measured from supraclavicular fossa (rib 1), infraclavicular fossa (rib 2), and then gradually downwards and laterally towards the midaxillary line. An 18 G Tuohy needle was inserted in plane, in the midaxillary line. The needle was coursed through latissimus dorsi, the outer sheath of serratus anterior muscle (SAM), the SAM and the inner sheath of SAM [Figure 1].
Figure 1.
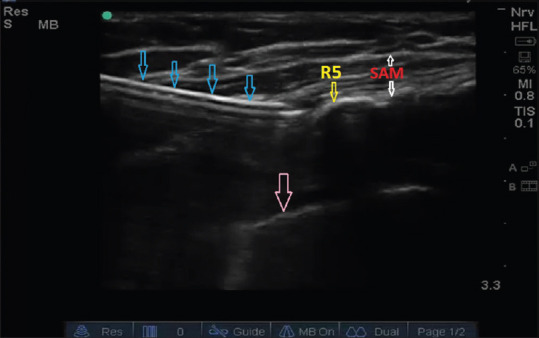
Showing USG guided serratus anterior plane block. (Blue arrows- needle, SAM- serratus anterior muscle, R5- fifth rib, pink arrow- pleura)
Three ml of 0.9% normal saline was injected to identify the correct plane between the SAM and the intercostal muscles (ICMs). Once the needle tip was confirmed in the SAP, 25 ml 0.2% ropivacaine and 50 μg of clonidine was injected in SAP. The spread was observed in the SAP for a distance of 4-5 intercostal spaces in the posterior plane. Influenced by gravity in the supine position, the spread was more in the posterior plane. 20 G catheter was introduced to a distance of 5-6 cm in the SAP. All patients in group S received a continuous infusion of 0.1% ropivacaine at 8 ml/hr for 24 hrs. IV fentanyl at a dose of 0.5 μg/kg was ordered as rescue analgesia i.e., if pain on Visual Analogue Score (VAS) was more than 4 in group S.
Group F
Patients in group F received a bolus of IV fentanyl (1.5 μg/kg, a maximum of 100 μg) if VAS was more than 4 followed by an infusion of 0.5 μg/hr. A bolus of 0.5 μg/kg was ordered for breakthrough pain i.e., if pain on VAS was more than 4. VAS was assessed every hourly. All patients in both the groups S and F were administered1 gmIV paracetamol 8th hourly. This was a retrospective study. Therefore, a sample size calculation was not done. Patients admitted from January 2016 to December 2019 were included.
Statistical Package for the Social Sciences (SPSS) version 21 was used for statistical analysis. P < than 0.05 was considered as statistically significant. Appropriate statistical tests were used for the analysis of collected data (Chi-Square test for age, unpaired t test for 24 h fentanyl consumption and age, ANOVA was analyzing VAS in two groups).
We retrieved data of 72 patients out of which 38 patients had received US-guided SAPB and 34 patients were managed with IV fentanyl infusion and fentanyl bolus for breakthrough pain. The demographic data (age, gender) is shown in Table 1. On analysis, gender of patients in both groups was not statistically significant (P = 0.41, Chi-square test). There was a statistically significant difference pertaining to age based on t test (P = 0.001).
In group F, patients received 0.5 μg/kg/h fentanyl infusion continuously. These patients received boluses of 0.5 μg/kg on several occasions when VAS was more than 4 in the first 24 h. Patients in group S were on CSAPB with 0.1% ropivacaine infusion and received boluses of 0.5 μg/kg when VAS was more than 4 in the first 24 h. There was a statistically significant difference between VAS score of two groups measured at 6 hourly intervals (repeated measured ANOVA test) [Figure 2]. Mean fentanyl consumption patients from group S was 95.26 ± 17.16 μg compared to 717.06 ± 83.10 in μg. There was statistically significant difference in fentanyl consumption in both the groups (P = 0.001, t-test) Table 3. In group F, in 15 patients IV fentanyl infusion was slowly weaned off once the VAS settled to 2-3 in the next 24 h. In the same group F US-guided SAPB was performed in remaining 19 patients at the end of 24 hrs since the VAS did not improve. In the group S, all patients had a VAS of 2–3 and a bolus of IV fentanyl 0.5 μg/kg was administered when VAS was more than 4 which was noticed after chest physiotherapy.
Figure 2.
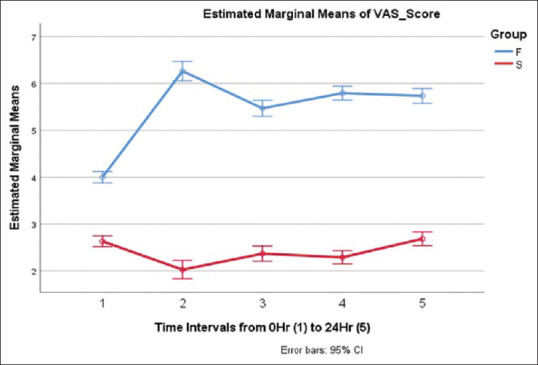
Shows comparison of VAS score for 1st 24 hrs in both groups. The figure is of a comparative line graph of means + 95% confidence interval in every 6 hrs
Table 3.
Showing comparison of 24 hrs fentanyl consumption in both groups
| Group | n | Mean | Sth. Deviation | Sth. Error Mean | |
|---|---|---|---|---|---|
| 24 hrs fentanyl consumption (µg) | F | 34 | 717.06 | 83.104 | 14.252 |
| S | 38 | 95.26 | 17.162 | 2.784 |
There is statistically significant difference in fentanyl consumption in both the groups (P=0.001) based on t-test
Discussion
An effective analgesia promptly prevents hypoventilation, enables deep breathing, adequate coughing with clearance of pulmonary secretions, and compliance with chest physiotherapy in patients who sustain MRFs. Overall, this reduced secondary pulmonary complications, including atelectasis, pneumonia, respiratory failure, and the need for respiratory support.[15,16] Opioids are commonly used in managing pain due to MRFs. But use of opioids comes at the cost of significant side-effects like respiratory depression, depressed cough reflex, constipation, and delirium.[17,18,19]
May et al. proposed an algorithm for pain management in MRF patients which also uses Rib fracture score.[19] The algorithm describes 4 steps. Step 1 involves use of paracetamol, codeine and/or non-steroidal anti-inflammatory drugs (NSAIDs) and/or oral morphine. In step 2 (pain score is 2–3), IV morphine needs to be titrated to response with anti-emetics. In step 3 (pain is uncontrolled), IV morphine patient-controlled analgesia, gabapentin and anti-emetics should be used. In step 4 (pain is still uncontrolled) with above measures: regional nerve block, TEA (thoracic epidural analgesia), SAPB, paravertebral block with catheter with rib fixation is suggested.
TEA is contraindicated in the following conditions: spinal cord injury, epidural or spinal cord hematoma, thoracic vertebral body fracture, spinal injury awaiting assessment, and coagulopathy (platelets <50 × 109 litre −1, INR >1.5). Patients on oral anticoagulants or antiplatelets further limit the use of TEA.[20,21] Injections of local anesthetic (LA) into the wedge-shaped paravertebral space, that is, the thoracic paravertebral block––which blocks the motor, sensory and sympathetic fibres produce effective analgesia across 4-5 dermatomes. Evidence suggests that paravertebral blocks are as effective as TEA without many of the contraindications, complications, and side-effects observed with epidurals.[22,23] Further a TEA for lateral rib fractures would be an overkill, which could be easily managed with multiple intercostal blocks (MICBs). However, MICBs involves multiple injections with multiples of complications like pneumothorax and intravascular injections.[24,25]
A variation and advancement of MICBs is the SAPB described initially by Blanco et al.[26] The lateral thoracic wall is innervated by the lateral cutaneous nerves that arise from the intercostal nerves. The lateral nerves travel in a potential space between the two planes of superficial and deep SAM. Injection of LA and catheter insertion with infusion provides analgesia to the anterolateral part of the thorax, with paraesthesia from T2 to T9.[27] Till date, there are only case reports which have described the efficacy of SAPB for managing pain due to fracture ribs.[28,29,30] Although retrospective, our study compares opioid-sparing analgesic efficacy of SAPB versus opioid alone.
In this retrospective comparative study, we observed opioid sparing, good quality pain relief (VAS of 2-3/10) in patients who were managed with CSAPB in group S with 0.1% ropivacaine at 8 ml/hour and IV paracetamol 1 g 8 hourly. All patients were mobilized on day 3. As against this, patients in group F required frequent intermittent IV fentanyl boluses leading to significant opioid consumption. 15 patients out of 34 required CSAPB as a rescue intervention after 24 hrs.
With the current retrospective comparative study, we feel CSAPB should be instituted earlier in the course of rib fracture pain pathway management to improve outcome, early ambulation, and discharge from ICU. The proposed algorithm by May et al. recommends the interventional technique i.e., regional anesthesia techniques like TEA, paravertebral block, and SAPB as a step 4, which appears too late. An earlier intervention with SAPB for lateral rib fractures greatly improves outcomes. Further, the SAPBs are performed in supine position and alleviates pain immediately. This study recommends the use of CSAPBs for lateral rib fractures extending from posterior angle of rib to 4–5 cm beyond the midaxillary line till anterior aspect, 3-4 cm anterior to the mid-axillary line.
There are limitations to this study. Being a retrospective study, there could be issues like bias which can be addressed only with randomization of patients into either group. In the presence of an underlying pneumothorax with subcutaneous emphysema, visualization of the SAP will be poor. In patients with dyspnoea, needle tracking will be difficult in the SAP and an echogenic needle may be required. Moreover, the two groups received different drugs thus were not matched well enough.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tulay CM, Yaldiz S, Bilge A. Do we really know the duration of pain after rib fracture.? Kardiochir Torakochirurgia Pol. 2018;15:147–50. doi: 10.5114/kitp.2018.78437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Witt CE, Bulger EM. Comprehensive approach to the management of the patient with multiple rib fractures: A review and introduction of a bundled rib fracture management protocol. Trauma Surg Acute Care Open. 2017;2:e000064. doi: 10.1136/tsaco-2016-000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin TJ, Eltorai AS, Dunn R, Varone A, Joyce MF, Kheirbek T, et al. Clinical management of rib fractures and methods for prevention of pulmonary complications: A review. Injury. 2019;50:1159–65. doi: 10.1016/j.injury.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 4.Marasco S, Lee G, Summerhayes R, Fitzgerald M, Bailey M. Quality of life after major trauma with multiple rib fractures. Injury. 2015;46:61–5. doi: 10.1016/j.injury.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 5.Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: A systematic review and meta-analysis. Injury. 2012;43:8–17. doi: 10.1016/j.injury.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Karadayi S, Nadir A, Sahin E, Celik B, Arslan S, Kaptanoglu M. An analysis of 214 cases of rib fractures. Clinics (Sao Paulo) 2011;66:449–51. doi: 10.1590/S1807-59322011000300015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talbot BS, Gange CP, Jr, Chaturvedi A, Klionsky N, Hobbs SK, Chaturvedi A. Traumatic rib injury: Patterns, imaging pitfalls, complications, and treatment. Radiographics. 2017;37:628–51. doi: 10.1148/rg.2017160100. [DOI] [PubMed] [Google Scholar]
- 8.Dehghan N, de Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: A review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76:462–8. doi: 10.1097/TA.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 9.Kieninger AN, Bair HA, Bendick PJ, Howells GA. Epidural versus intravenous pain control in elderly patients with rib fractures. Am J Surg. 2005;189:327–30. doi: 10.1016/j.amjsurg.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 10.Van Vledder MG, Kwakernaak V, Hagenaars T, Van Lieshout EM, Verhofstad MHJ South West Netherlands Trauma Region Study Group. Patterns of injury and outcomes in the elderly patient with rib fractures: A multicenter observational study. Eur J Trauma Emerg Surg. 2019;45:575–83. doi: 10.1007/s00068-018-0969-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin FC, Li RY, Tung YW, Jeng KC, Tsai SC. Morbidity, mortality, associated injuries, and management of traumatic rib fractures. J Chin Med Assoc. 2016;79:329–34. doi: 10.1016/j.jcma.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Peek J, Beks RB, Kingma BF, Marsman M, Ruurda JP, Houwert RM, et al. Epidural analgesia for severe chest trauma: An analysis of current practice on the efficacy and safety. Crit Care Res Pract. 2019;2019:4837591. doi: 10.1155/2019/4837591. doi: 10.1155/2019/4837591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holcomb J, McMullin N, Kozar R, Lygas M, Moore F. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196:549–55. doi: 10.1016/S1072-7515(02)01894-X. [DOI] [PubMed] [Google Scholar]
- 14.Southgate SJ, Herbst MK. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2019. [Last accessed on 2019 Aug 04]. Ultrasound guided serratus anterior blocks. [Updated 2019 Mar 19] Available from: https://www.ncbi.nlm.nih.gov/books/NBK538476/ [PubMed] [Google Scholar]
- 15.Karmakar M, Ho A. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54:615–25. doi: 10.1097/01.TA.0000053197.40145.62. [DOI] [PubMed] [Google Scholar]
- 16.Malchow RJ, Black IH. The evolution of pain management in the critically ill trauma patient: Emerging concepts from the global war on terrorism. Crit Care Med. 2008;36(Suppl):S346–57. doi: 10.1097/CCM.0b013e31817e2fc9. [DOI] [PubMed] [Google Scholar]
- 17.Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid complications and side effects. Pain Physician. 2008;11(Suppl):S105–20. [PubMed] [Google Scholar]
- 18.Porreca F, Ossipov MH. Nausea and vomiting side effects with opioid analgesics during treatment of chronic pain: Mechanisms, implications, and management options. Pain Med. 2009;10:654–62. doi: 10.1111/j.1526-4637.2009.00583.x. [DOI] [PubMed] [Google Scholar]
- 19.Thiruvenkatarajan V, Cruz Eng H, Adhikary SD. An update on regional analgesia for rib fractures. Curr Opin Anaesthesiol. 2018;31:601–7. doi: 10.1097/ACO.0000000000000637. [DOI] [PubMed] [Google Scholar]
- 20.May L, Hillermann C, Patil S. Rib fracture management. BJA Educ. 2016;16:26–32. [Google Scholar]
- 21.Agamohammdi D, Montazer M, Hoseini M, Haghdoost M, Farzin H. A comparison of continuous thoracic epidural analgesia with bupivacaine versus bupivacaine and dexmedetomidine for pain control in patients with multiple rib fractures. Anesth Pain Med. 2018;8:e60805. doi: 10.5812/aapm.60805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hashemzadeh S, Hashemzadeh K, Hosseinzadeh H, Aligholipour Maleki R, Golzari SE. Comparison thoracic epidural and intercostal block to improve ventilation parameters and reduce pain in patients with multiple rib fractures. J Cardiovasc Thorac Res. 2011;3:87–91. doi: 10.5681/jcvtr.2011.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Malekpour M, Hashmi A, Dove J, Torres D, Wild J. Analgesic choice in management of rib fractures: Paravertebral block or epidural analgesia? Anesth Analg. 2017;124:1906–11. doi: 10.1213/ANE.0000000000002113. [DOI] [PubMed] [Google Scholar]
- 24.Yeying G, Liyong Y, Yuebo C, Yu Z, Guangao Y, Weihu M, et al. Thoracic paravertebral block versus intravenous patient-controlled analgesia for pain treatment in patients with multiple rib fractures. J Int Med Res. 2017;45:2085–91. doi: 10.1177/0300060517710068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Truitt MS, Murry J, Amos J, Lorenzo M, Mangram A, Dunn E, et al. Continuous intercostal nerve blockade for rib fractures: Ready for primetime. Trauma. 2011;71:1548–52. doi: 10.1097/TA.0b013e31823c96e0. [DOI] [PubMed] [Google Scholar]
- 26.Hwang EG, Lee Y. Effectiveness of intercostal nerve block for management of pain in rib fracture patients. J Exerc Rehabil. 2014;10:241–4. doi: 10.12965/jer.140137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: A novel ultrasound- guided thoracic wall nerve block. Anaesthesia. 2013;68:1107–13. doi: 10.1111/anae.12344. [DOI] [PubMed] [Google Scholar]
- 28.Biswas A, Castanov V, Li Z, Perlas A, Kruisselbrink R, Agur A, et al. Serratus plane block: A cadaveric study to evaluate optimal injectate spread. Reg Anesth Pain Med. 2018;43:854–8. doi: 10.1097/AAP.0000000000000848. [DOI] [PubMed] [Google Scholar]
- 29.Kunhabdulla NP, Agarwal A, Gaur A, Gautam SK, Gupta R, Agarwal A. Serratus anterior plane block for multiple rib fractures. Pain Physician. 2014;17:E553–5. [PubMed] [Google Scholar]
- 30.Durant E, Dixon B, Luftig J, Mantuani D, Herring A. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med. 2017;35:197.e3-e6. doi: 10.1016/j.ajem.2016.07.021. [DOI] [PubMed] [Google Scholar]


