Abstract
Background and Aims:
Tracheostomy is a commonly performed procedure in critically ill patients because patients requiring chronic mechanical ventilation (MV) are rising by as much as 5.5% per year. The controversy on likely benefits of early versus late tracheostomy is ongoing. We aimed to study the impact of early versus late tracheostomy on patient outcomes.
Material and Methods:
A retrospective observational study was performed in intensive care unit (ICU) patients who underwent tracheostomy in a 31-bedded multispeciality ICU of a 350-bedded tertiary care hospital, over a period of 1 year. Data collected included the age, sex, APACHE II score, indication for tracheostomy, timing of procedure, whether surgical or percutaneous, any complication, MV days, ICU stay, and patient outcome. Patients were divided into two groups for statistical comparison: early ≤7 days and late >7 days of MV.
Results:
A total of 102 patients underwent tracheostomy over the study period, of which 19 were excluded because of inadequate data and exclusion criteria. Of the 83 study patients, 60 had percutaneous, while 23 had surgical tracheostomy. About 51 (61.45%) had early, while 32 (38.55%) had late tracheostomy. On statistical analysis, there was a significant difference in MV days (5 vs 12.5 days, P = 0.002), ICU stay (10 vs 16 days, P = 0.004), mortality (21.6% vs 43.8%, P = 0.032), and decannulation rate (29.41% vs 6.25%, P = 0.009). No difference was observed in hospital stay or complication rates.
Conclusion:
Early tracheostomy is associated with both morbidity and mortality benefits. Patients requiring MV should be given an option of early tracheostomy.
Keywords: Critically ill, mechanical ventilation, percutaneous, tracheostomy
Introduction
Tracheostomy is a common procedure in the critically ill patients requiring prolonged ventilation and it is being increasingly performed in intensive care units (ICUs) with the introduction of less invasive percutaneous techniques. The reported benefits of tracheostomy over prolonged translaryngeal endotracheal intubation include reduced need for sedation, greater patient comfort, improved clearance of pulmonary secretions, faster weaning, and shorter hospital stay. However, tracheostomy is also associated with adverse effects including procedure-related and late complications.[1]
Despite decades of experience and number of studies in literature, there is conflicting evidence on the ideal time for tracheostomy. Many studies have reported beneficial effects of early tracheostomy, whereas a recent multicenter randomized controlled trial (RCT) was unable to demonstrate improvement in mortality or other patient-related secondary outcomes.[2,3,4] Recently, a systematic review of RCTs has suggested that early tracheostomy leads to more ventilator-free days, less sedation, and reduced mortality compared with late tracheostomy. There is also no clear agreement regarding what constitutes early tracheostomy, as the time used to define early tracheostomy in clinical studies ranges from 48 hours to as late as 10 days following ICU admission.[5] However, there is still a considerable variation in opinion among physicians and institutions regarding optimum timing of tracheostomy. There are a very limited data available from the developing world regarding the timing of tracheostomy and its implications on patient outcomes.
Developing countries like Indian healthcare have limited availability of well-equipped critical care units, with ICU bed strength typically less than 5% of total hospital beds in a majority of advanced centers. It becomes difficult to obtain an ICU bed for many of the deserving critically ill patients.[6] Hence, there is a considerable interest in interventions including early tracheostomy which can shorten the duration of mechanical ventilation (MV) and ICU stay, potentially leading to better utilization of scarce resources.
In this study, we retrospectively evaluated the benefits of early versus late tracheostomy in terms of its ability to reduce MV duration, length of ICU stay, and mortality rates in ICU patients in a tertiary care institution in an Indian setting.
Material and Methods
The study was conducted in a 31-bed multi-disciplinary ICU of a tertiary care hospital after approval by the hospital board of ethics. The 350-bed hospital has 24 medical/surgical and 7 neurology/neurosurgical ICU beds which are staffed by full-time intensivists 24 h a day with an average nurse-to-patient ratio of 1:2. We retrospectively analyzed the medical records of ICU patients who underwent tracheostomy over a period of 1 year from November 2015 to October 2016. The decision to proceed with tracheostomy was made by the attending physician. There was no formal criteria to proceed with tracheostomy and the decision was based on clinical criteria including neurological reasons [low Glasgow Coma Scale (GCS)], difficult weaning from MV, neuromuscular weakness, or acute respiratory failure. Patients with previous tracheostomy, emergency tracheostomy, or age younger than 18 years were excluded from the study. Tracheostomy was performed either as bedside percutaneous technique using Griggs method or as standard surgical procedure in the operation theater. Medical records were analyzed for age, sex, admitting diagnosis, APACHE II score, indication for tracheostomy, timing of procedure, whether surgical or percutaneous, any complication, and number of MV days, ICU stay, hospital stay, and patient outcome. The study patients were divided into two groups based on the timing of tracheostomy: early tracheostomy (ET) group (tracheostomy performed ≤7 days after intubation); and the late tracheostomy (LT) group (tracheostomy performed 8 or more days after intubation). In our hospital, the intensivist-led tracheostomy review team follows up the patients who are discharged from the ICU on tracheostomy to the wards. The patients are looked after by tracheostomy nurses in the wards. The study patients who underwent decannulation during hospital stay were noted. The primary outcomes of interest were the in-hospital mortality, ICU length of stay (LOS), and total duration on MV. The secondary outcomes were the length of hospital stay, decannulation rate, and the complications associated with tracheostomy.
Statistical analysis
All statistical calculations were done using SPSS (Statistical Package for the Social Science), version 17 statistical program for Microsoft Windows. Data were as described in terms of range, mean ± standard deviation, median, frequencies (number of cases), and relative frequencies (percentages) as appropriate. Comparison of the quantitative variables between the study groups was done using Student's t-test and Mann–Whitney U-test for independent samples for parametric and nonparametric data, respectively. For comparing categorical data, Chi-square (χ2) test was performed and exact test was used when the expected frequency is less than 5. Logistic regression and receiver operating characteristic (ROC) curve analysis were done. A probability value (P-value) less than 0.05 was considered statistically significant.
Results
During the study period, a total of 102 patients underwent tracheostomy. Of these, 19 patients were excluded from the study because of inadequate data and exclusion criteria. Of the 83 study patients, there were 59 males (71.1%) and 24 females (28.9%). The median age of patients was 61 years with a range from 18 to 92 years. The majority of tracheostomies were done using percutaneous (72%) technique. The indications for tracheostomy were neurological (low GCS) and respiratory (acute respiratory failure, difficult weaning, neuromuscular weakness).
Among the 83 study patients, 51 (61.45%) underwent early tracheostomy and 32 (38.55%) late tracheostomy [Figure 1]. The median time for early and late tracheostomy after endotracheal intubation was 3 (2–5) and 12 (10–16) days, respectively. The majority of study patients were tracheostomized by day 15 [Figure 2]. The two groups presented similar characteristics in terms of demographic data (age, gender) and APACHE II score. The percutaneous approach of tracheostomy was predominantly used in both the ET and LT groups (66.7% vs 81.3%, P = 0.149). The proportion of neurological reasons as the indication for tracheostomy was significantly higher in the ET group (74.5% vs 53.1%, P = 0.045) [Table 1].
Figure 1.
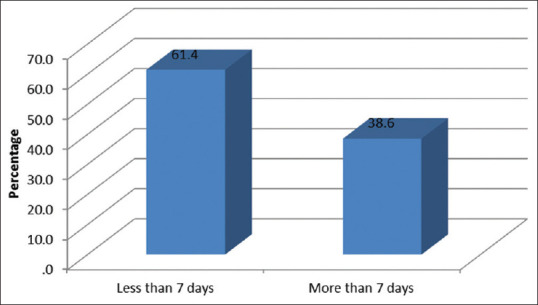
Number of patients (early versus late tracheostomy)
Figure 2.
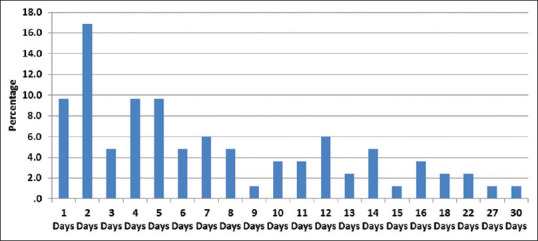
Day-wise distribution of tracheostomy
Table 1.
Patient characteristics and indications of tracheostomy
| ET group n=51 | LT group n=32 | P | |
|---|---|---|---|
| Age (years) a | 57.16±18.11 | 63.53±17.77 | 0.120 |
| Genderb | |||
| Male | 40 (78.4%) | 19 (59.4%) | 0.062 |
| Female | 11 (21.6%) | 13 (40.6%) | |
| APACHE II scorea | 21.25±5.62 | 21.84±7.22 | 0.679 |
| Percutaneous techniqueb | 34 (66.7%) | 26 (81.3%) | 0.149 |
| Reason for tracheostomy | |||
| Respiratoryb,# | 13 (25.5%) | 15 (46.9%) | 0.045 |
| Neurologicalb,$ | 38 (74.5%) | 17 (53.1%) |
ET=early tracheostomy, LT=late tracheostomy, SD=standard deviation, GCS=Glasgow Coma Scale.aMean±SD. bNumber. #Acute respiratory failure, neuromuscular weakness. $Low GCS
The median (interquartile range) duration of MV was significantly shorter in the ET group than the LT group patients at 5 (3–8) days versus 12.5 (5.25–20.25) days; P = 0.002. There was statistically significant reduction in ICU LOS by 6 days in the ET group. The duration of ICU stay in the ET and LT groups was 10 (6–16) and 16 (13–25) days, respectively; P = 0.004. The median (interquartile range) duration of hospital stay was 17 (12–27) days in the ET group and 22 (16–31) days in the LT group which was statistically nonsignificant; P = 0.461. The overall hospital mortality among tracheostomized patients was 30.1% (25/83). There was statistically significant lower mortality [n = 11 (21.6%)] in the ET than the LT group [n = 14 (43.8%)] (P = 0.032). Of the total 83 tracheostomized patients, 17 (20.48%) could be decannulated during the study period. The decannulation rate during hospital stay was significantly higher in the ET group (29.41% vs 6.25%, P = 0.009). No major complication was noted in tracheostomized patients. Only one patient had accidental decannulation which was handled by tracheostomy nurse. There was no statistically significant difference in the number of ventilator-associated pneumonia between the ET and LT groups (5.8% vs 6.2%, P = 0.94) [Table 2].
Table 2.
Comparison of outcomes in two groups
| ET group n=51 | LT group n=32 | P | |
|---|---|---|---|
| Mechanical ventilation daysa | 5 (3-8) | 12.5 (5.25-20.25) | 0.002 |
| No. of ICU daysa | 10 (6-16) | 16 (13.25-25) | 0.004 |
| Hospital stay (days) a | 17 (12-27) | 22 (16-31) | 0.461 |
| Mortalityb | 11 (21.6%) | 14 (43.8%) | 0.032 |
| Decannulation rateb | 15 (29.41%) | 2 (6.25%) | 0.009 |
| Ventilator-associated pneumoniab | 3 (5.8%) | 2 (6.2%) | 0.94 |
ET=early tracheostomy, LT=late tracheostomy, ICU=intensive care unit. aResults are presented as median (interquartile range), bNumber
Using univariate analysis of the data, late tracheostomy (P = 0.032), the number of ICU days (P = 0.009), and APACHE II score (P = 0.00002) were found to be associated with increased hospital mortality [Table 3]. No. of ICU days and late tracheostomy were however not independent predictors of mortality on multivariate analysis. The parameter which independently predicted mortality on multivariate analysis was APACHE II score [P = 0.001] [Table 4]. ROC curve analysis also showed APACHE II score to be the most important mortality predictor, followed by ICU LOS for tracheostomized patients [Figure 3].
Table 3.
Univariate analysis of mortality
| Discharge | Expired | P | |
|---|---|---|---|
| Age (years)a | 57.91±18.82 | 63.56±16.13 | 0.195 |
| Genderb | |||
| Male | 42 (72.4%) | 17 (68%) | 0.684 |
| Female | 16 (27.6%) | 8 (32%) | |
| No. of ICU daysc | 11.50 (6-16) | 17.00 (9.50-26.50) | 0.009 |
| Hospital stay (days)c | 18.50 (12-27) | 18.00 (14.50-29) | 0.757 |
| Mechanical ventilation daysc | 5.00 (2-5) | 8.00 (5-21.50) | 0.059 |
| APACHE II scorea | 19.66±4.76 | 25.72±7.28 | 0.00002 |
| Timing of Tracheostomyb | |||
| Early tracheostomy (≤7 days) | 40 (69%) | 11 (44%) | 0.032 |
| Late tracheostomy (>7 days) | 18 (31.0%) | 14 (56.0%) | |
| Indication of tracheostomyb | |||
| Neurological | 40 (69%) | 15 (60%) | 0.428 |
| Respiratory | 18 (31%) | 10 (40%) |
ICU=Intensive Care Unit, aMean±Standard Deviation, bNumber, cResults are presented as Median (Interquartile Range)
Table 4.
Multivariate analysis of mortality
| P | Odds ratio | 95% Confidence interval for odds ratio | ||
|---|---|---|---|---|
|
| ||||
| Lower | Upper | |||
| No. of ICU days | 0.698 | 1.012 | 0.952 | 1.076 |
| APACHE II score | 0.001 | 1.219 | 1.084 | 1.371 |
| Late tracheostomy (>7 days) | 0.066 | 2.998 | 0.928 | 9.687 |
ICU=Intensive Care Unit
Figure 3.
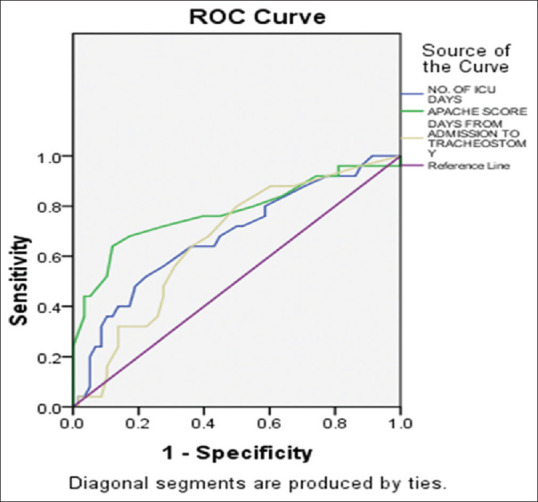
ROC analysis
Discussion
Our study showed that early tracheostomy in multispeciality ICU patients is associated with significant reduction in hospital mortality, duration of MV, and ICU LOS, but had no effect on the duration of hospital stay. However, on multivariate analysis, APACHE II score was the only independent predictor of hospital mortality and not the late tracheostomy.
Our finding of better patient outcomes with early tracheostomy is consistent with the results of previous studies.[2,7,8] Rumbak et al. prospectively randomized 120 medical ICU patients requiring long-term ventilation to either early tracheostomy (within 48 h) or delayed tracheostomy (at days 14–16) and noted that early tracheostomy group was associated with significant reduction in mortality (31.7% vs 61.7%), ICU LOS and duration of MV.[2] A recent Cochrane systematic review of eight RCTs evaluated the effectiveness of early (≤10 days after tracheal intubation) versus late tracheostomy (≥10 days after intubation). Patients in early tracheostomy group had lower risk of mortality (risk ratio 0.83, 95% CI 0.70–0.98; P = 0.03).[9]
Some studies in literature point toward cost savings and improved patient outcomes with early tracheostomy, but with no mortality benefit.[3,10] Arabi et al. in an observational study analyzed trauma ICU patients requiring tracheostomy and reported that ET (performed by day 7 of MV) is associated with shorter duration of MV and ICU LOS without affecting hospital mortality. The authors also reported that there was no significant difference in the median hospital LOS between ET (68 days) and LT (83 days) group, as was found in our study. This may be due to the severity of admitting diagnosis and the associated comorbidities of study patients requiring prolonged hospital stay.[10] Moreover, unlike developed countries, in our healthcare setup, there are limited rehabilitation facilities available outside the hospital setting and patient stay gets extended as they undergo rehabilitation while in hospital itself.
The beneficial effects of early tracheostomy observed in our study were not evident in some of the previous studies.[4,11] Blot et al. conducted the first large multicenter RCT comparing patients with early tracheostomy (within 4 day of MV) versus those in whom intubation was maintained for at least 14 days. A total of 123 patients across 25 centers were included in the study and the authors concluded that there was no difference between two groups in any of primary or secondary outcomes except for greater patient comfort reported by patients in the ET group. However, this trial was underpowered and only a small proportion of patients fulfilling inclusion criteria could be actually included.[11]
The results of various studies on tracheostomy are difficult to interpret due to the differences in patient characteristics, admitting diagnosis, indications, technique (percutaneous or surgical), and timing of early versus late tracheostomy. Even though we noted substantially lower hospital mortality in the ET group (21.6% vs 43.8%, P = 0.032), this difference can be due to small sample size, heterogeneity of studied patients, and different indications for tracheostomy in the two groups. For patients who are critically ill with high APACHE II score, as in our study, the impact of any specific therapeutic measure alone including early tracheostomy would be limited.[12]
We noted that low GCS was the predominant indication of tracheostomy in the ET group. Patients with low neurologic status require immediate airway protection to minimize the risk of aspiration which may lead to worsened gas exchange and secondary brain insult. Early tracheostomy in such patients can lead to less use of sedation, early liberation from MV, and shorter LOS in critical care.[13] Percutaneous technique is now the preferred method of performing tracheostomy in ICUs, as noted in our study. There is no mortality difference between percutaneous and surgical technique of tracheostomy. However, percutaneous approach is associated with less stoma infection, less unfavorable scarring, and lower cost.[14] In our study, we did not come across any major complication in study patients.
We observed significantly higher decannulation rates before hospital discharge in patients who underwent early tracheostomy. In our hospital, the intensivist-led tracheostomy team oversees the care of patients discharged on tracheostomy from the ICU to the wards. We had previously reported that a tracheostomy care nurse program across the hospital wards can result in improvement in patient care, decannulation rates, and significant decrease in long-term complications associated with tracheostomy.[15] In a single-center prospective cohort study, the authors found positive impact of an intensivist-led multidisciplinary team on the decannulation rates in wards. They also reported that the decannulation rates depend on tracheostomy indication, with hazard ratio for decannulation of 0.5 (95% CI 0.33–0.7, P < 0.01) among patients with coma as the indication of tracheostomy.[16] The more recent meta-analysis by Chorath et al has indicated beneficial effect of early tracheostomy in lowering duration of mechanical ventilation and ICU stay with no significant effect on all-cause mortality.[17] Previously one retrospective study in Indian care setting has compared the impact of early tracheostomy in neuro trauma patients.[18] However there is limited data available on benefits of early tracheostomy in this part of world and well-conducted multicenter adequately powered randomized trials with relevant subgroups are needed to address the issue.
Our study has several limitations. It was a retrospective study conducted in a single center and involved a small number of patients. The decision to perform tracheostomy was arbitrary, based on the clinical judgment of treating physician. Long-term follow-up of patients after hospital discharge was not conducted, and therefore could not be included in the analysis. Also, we did not do any cost analysis in our patients.
In conclusion, our study indicates the possible benefits of early tracheostomy in reduction of MV duration and ICU LOS. Although no cost analysis was performed, early tracheostomy may result in better cost savings and resource utilizations by reducing ICU LOS. We conclude that early tracheostomy is associated with both morbidity and mortality benefits, and patients requiring MV should be given an option of early tracheostomy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rana S, Pendem S, Pogodzinski MS, Hubmayr RD, Gajic O. Tracheostomy in critically ill patients. Mayo Clin Proc. 2005;80:1632–8. doi: 10.4065/80.12.1632. [DOI] [PubMed] [Google Scholar]
- 2.Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med. 2004;32:1689–94. doi: 10.1097/01.ccm.0000134835.05161.b6. [DOI] [PubMed] [Google Scholar]
- 3.Koch T, Hecker B, Hecker A, Brenck F, Preub M, Schmelzer T, et al. Early tracheostomy decreases ventilation time but has no impact on mortality of intensive care patients: A randomized study. Langenbecks Arch Surg. 2012;397:1001–8. doi: 10.1007/s00423-011-0873-9. [DOI] [PubMed] [Google Scholar]
- 4.Young D, Harrison DA, Cuthbertson BH, Rowan K TracMan Collaborators. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: The TracMan randomized trial. JAMA. 2013;309:2121–9. doi: 10.1001/jama.2013.5154. [DOI] [PubMed] [Google Scholar]
- 5.Hosokawa K, Nishimura M, Egi M, Vincent JL. Timing of tracheostomy in ICU patients: A systematic review of randomized controlled trials. Crit Care. 2015;19:424. doi: 10.1186/s13054-015-1138-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeolekar ME, Mehta S. ICU care in India – status and challenges. JAPI. 2008;56:221–2. [PubMed] [Google Scholar]
- 7.Flaaten H, Gjerde S, Heimdal H, Aardal S. The effect of tracheostomy on outcome in intensive care unit patients. Acta Anaesthesiol Scand. 2006;50:92–8. doi: 10.1111/j.1399-6576.2005.00898.x. [DOI] [PubMed] [Google Scholar]
- 8.Kollef MH, Ahrens TS, Shannon W. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 1999;27:1714–20. doi: 10.1097/00003246-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Andriolo BN, Andriolo RB, Saconato H, Atallah AN, Valente O. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst Rev. 2015;1:CD007271. doi: 10.1002/14651858.CD007271.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arabi Y, Haddad S, Shirawi N, Al Shimmemeri A. Early tracheostomy in intensive care trauma patients improves resource utilization: A cohort study and literature review. Crit Care. 2004;8:R347–52. doi: 10.1186/cc2924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blot F, Similowski T, Trouillet JL, Chardon P, Korach JM, Costa MA. Early tracheostomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive Care Med. 2008;34:1779–87. doi: 10.1007/s00134-008-1195-4. [DOI] [PubMed] [Google Scholar]
- 12.Scales DC, Kahn JM. Tracheostomy timing, enrolment and power in ICU clinical trials. Intensive Care Med. 2008;34:1743–5. doi: 10.1007/s00134-008-1194-5. [DOI] [PubMed] [Google Scholar]
- 13.Pinheiro Bdo V, Tostes Rde O, Brum CI, Carvalho EV, Pinto SP, Oliveira JC. Early versus late tracheostomy in patients with acute severe brain injury. J Bras Pneumol. 2010;36:84–91. doi: 10.1590/s1806-37132010000100014. [DOI] [PubMed] [Google Scholar]
- 14.Longworth A, Veitch D, Gudibande S, Whitehouse T, Snelson C, Veenith T. Tracheostomy in special groups of critically ill patients: Who, When, and Where? Indian J Crit Care Med. 2016;20:280–4. doi: 10.4103/0972-5229.182202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sodhi K, Shrivastava A, Singla MK. Implications of dedicated tracheostomy care nurse program on outcomes. J Anesth. 2014;28:374–80. doi: 10.1007/s00540-013-1718-1. [DOI] [PubMed] [Google Scholar]
- 16.Tobin AE, Santamaria JD. An intensivist-led tracheostomy review team is associated with shorter decannulation time and length of stay: A prospective cohort study. Crit Care. 2008;12:R48. doi: 10.1186/cc6864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chorath K, Hoang A, Rajasekaran K, Moreira A. Association of early vs late tracheostomy placement with pneumonia and ventilator days in critically ill patients: A meta-analysis. JAMA Otolaryngol Head Neck Surg. 2021;147(5):450–459. doi: 10.1001/jamaoto.2021.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zirpe KG, Tambe DV, Deshmukh AM, Gurav SK. The impact of early tracheostomy in neurotrauma patients: a retrospective study. Indian J Crit Care Med. 2017;21(1):6–10. doi: 10.4103/0972-5229.198309. [DOI] [PMC free article] [PubMed] [Google Scholar]


