Abstract
Background and Aims:
Caudal epidural and ultrasound-guided ilioinguinal, iliohypogastric nerve (IL/IH) blocks are commonly used regional anesthesia techniques for postoperative analgesia in pediatric inguinal surgeries. Dexmedetomidine as an adjuvant has been proven to prolong the duration of both neuraxial and peripheral nerve blocks. We compared the duration of analgesia provided by local anesthetic (LA) and dexmedetomidine for caudal and IL/IH block for pediatric inguinal surgeries.
Material and Methods:
Forty-six children undergoing inguinal hernia repair were selected for this randomized double-blind study. After general anesthesia, children received either 0.75 mL.kg−1 of 0.25% bupivacaine with 1 mcg.kg−1 of dexmedetomidine in caudal epidural or 0.25 mL.kg−1 of 0.25% bupivacaine with 1 mcg.kg−1 of dexmedetomidine in IL/IH block. The pain was assessed up to 24 h postoperatively using face, legs, activity, cry, consolability (FLACC) score. For FLACC ≥4, rescue analgesia was provided using 1 μg/kg of intravenous fentanyl, up to 2 h postoperatively and 10 mg/kg of oral ibuprofen between 2 and 24 postoperative hours. The time for first rescue analgesia was taken as the duration of analgesia.
Results:
There were no significant differences in the pain scores or analgesic utilization between the groups. The duration of analgesia of caudal and IL/IH blocks was similar (720.3 ± 430.1 min and 808.4 ± 453.1 min, respectively). The time taken for the performance of block was significantly higher for caudal compared to IL/IH (547 ± 93 vs. 317 ± 179 s; P < 0.001).
Conclusion:
Both caudal epidural and USG-IL/IH block with dexmedetomidine as additive provide the comparable duration of postoperative analgesia with no significant side effects.
Keywords: Acute pain, child, hernia surgery, regional pain, regional ultrasound
Introduction
A pediatric caudal epidural block is a simple, safe procedure with a high success rate. Hence, it is the preferred mode of analgesia for pediatric inguinal surgeries. Its main disadvantage is that the duration of analgesia is very short when used as a single-shot injection. Many additives have been used along with local anesthetics in the single-shot caudal epidural to prolong the duration of analgesia.[1] Ilioinguinal and iliohypogastric nerve block (IL/IH) is another regional anesthesia technique that is equally effective for inguinal hernia surgeries in children.[2] But, the main drawback of the IL/IH block is a high failure rate when performed blindly. Ultrasound-guided (USG) IL/IH has been described with a significantly higher success rate.[3,4,5] USG-IL/IH has been shown to be as effective as a caudal block for postoperative analgesia in children undergoing unilateral groin surgery.[6]
Many additives have been successfully used as an adjunct to local anesthetic in pediatric regional anesthesia.[7] Dexmedetomidine is a highly selective α2 agonist and has shown to prolong the duration of caudal analgesia when used in pediatric surgeries.[8] Animal trials demonstrated that perineural dexmedetomidine in combination with bupivacaine enhanced sensory and motor block, without neurotoxicity in experimental studies.[9] Dexmedetomidine has been shown to prolong the duration of peripheral nerve blocks in children.[10,11] Even though there are separate studies showing the efficacy of dexmedetomidine as an adjuvant for central neuraxial block and in peripheral nerve blocks, there are no direct studies comparing the efficacy of dexmedetomidine as adjuvant in central neuraxial block to its effect in the peripheral block for similar surgeries. The primary aim of this study was to compare the duration of postoperative analgesia following caudal epidural and USG-IL/IH block using a combination of bupivacaine and dexmedetomidine. Pain scores after the surgery, rescue analgesic requirement and side effects were the secondary outcome measures studied.
Material and Methods
This prospective randomized double-blind study was conducted after approval from the institute's ethical committee. This study was registered in the clinical trial registry of India reference: CTRI/2018/01/011327. Informed written consent was obtained from the parents of children, after explaining to them about the postoperative pain assessment and its treatment.
Forty-six children of ASA class I and II, aged between 1 and 10 years scheduled to undergo unilateral herniotomy were included in the study. Children with active respiratory tract infection, bleeding disorders, neuromuscular abnormalities, deformities of the caudal space, and those allergic to nonsteroidal anti-inflammatory drugs or any of the study drugs were excluded from the study.
All children received 0.5 mg/kg of syrup midazolam orally as premedication about 30 min prior to the start of anesthesia. Standard monitoring consisted of the electrocardiogram, noninvasive blood pressure, pulse oximetry, and capnograph. Inhalation induction of anesthesia was conducted using sevoflurane in oxygen and nitrous oxide and intravenous access were secured. Anesthesia was maintained with 2% sevoflurane in 66% nitrous oxide. The airway was secured by face mask or classic laryngeal mask airway and spontaneous ventilation was maintained.
The children were randomized using a computer-generated randomization table as either USG-IL/IH block group (group B) or caudal epidural group (group C). Double blinding was ensured by not allowing the parents of the child and the person who assessed the postoperative pain in the operation theater while giving the block.
For children in group C, the caudal block was performed by identifying the landmarks and after loss of resistance to the needle. They received 0.75 mL/kg body weight of 0.25% bupivacaine and 1 μg/kg of dexmedetomidine as an additive. In group B, the children received USG-IL/IH block with 0.25 mL/kg body weight of 0.25% bupivacaine with 1 μg/kg of dexmedetomidine. 50 μg of dexmedetomidine was diluted in 1 mL syringe (0.5 mL of dexmedetomidine and 0.5 mL normal saline, resulting in 5 μg/0.1 mL). The dose of dexmedetomidine was rounded off to the nearest multiple of 5 μg (e.g., for a 12 kg child 10 μg and for a 13 kg child 15 μg of dexmedetomidine was used).
For USG-IL/IH block, the ultrasound machine (Samsung sonoACE-R7) with a linear transducer (5–12 MHz) was used. Two anesthesiologists, who had performed at least 20 caudal epidurals and USG-IL/IH before, performed all the blocks for the study. The skin was disinfected and the transducer was placed medial to the anterior superior iliac spine (ASIS), oriented on a line joining the ASIS with the umbilicus. The three muscle layers were identified as internal oblique muscle (IOM), external oblique muscle (EOM), and transversus abdominis muscle (TAM). The IL/IH nerves appear as hypoechoic ovals between the IOM and TAMs. The needle was inserted in-plane in a medial to lateral orientation, through the subcutaneous tissue, EOM, and IOM, and was advanced toward the nerves. The local anesthetic was injected under the guidance of ultrasound. Time to perform the block was defined as the time needed for positioning (lateral for caudal block), aseptic precautions (probe preparation for ILIH), block performance, and the patient being ready for surgery (return positioning to supine in case of the caudal block).
20% increase in the heart rate or respiratory rate above the baseline, or patient movement at skin incision or during the intraoperative period was considered as a failed block. In this case, fentanyl 1 μg.kg−1 was given intravenously. Heart rate, blood pressure, and respiratory rate were recorded every 5 min for 30 min after the block. After surgery, patients were transferred to the recovery room and were monitored every 15 min during the first 2 h in a post-anesthesia care unit (PACU) and every 1 h for the next 2 h and every 6th hourly for up to 24 h postoperative period in the ward. Emergence delirium was assessed using pediatric anesthesia emergence delirium (PAED) score. Postoperative pain was assessed with the FLACC score.[12] Patients having pain scores equal to or more than 4 in the first 2 h after the surgery were given intravenous fentanyl 1 μg/kg as a rescue analgesic. Between 2 and 24 h of the postoperative period, 10 mg/kg of oral ibuprofen syrup was used as the rescue analgesic. If the pain did not subside within half an hour of giving syrup, they were given 15 mg/kg of paracetamol syrup orally. Time for first rescue analgesia was recorded. Pain score, number of rescue analgesics in 24 h period, time for ambulation, time for voiding urine after the surgery, postoperative nausea and vomiting (PONV) were noted. The parent's satisfaction for analgesia was noted in percentages. Heart rates less than 60/min were considered as bradycardia and was treated with intravenous atropine. Other side effects such as PONV were noted.
Statistical analysis
A previous study using 1 μg/kg dexmedetomidine in the caudal block noted the mean duration of analgesia of 809 ± 156 (95% CI: 625–965) min.[13] Based on this, the sample size needed to show a 20% change in the duration of analgesia with 80% power and an α-error of 0.05 was 18 patients in each group. Considering some dropouts we decided to include 23 patients in each group.
Statistical analyses were performed using SPSS ver. 20.0 (SPSS Inc., Chicago, IL). Categorical variables were compared using the Chi-square test or Fisher's exact test. Continuous variables were compared using independent t-test. Data are presented as mean ± standard deviation or as the number of patients and percentages. Time to first analgesic administration was analyzed by Kaplan-Meier survival analysis and log-rank test. P value of less than 0.05 was considered statistically significant.
Results
A total of 46 patients were randomized into two groups of 23 patients each [Figure 1]. Two patients in the caudal block group had failed block for which intraoperative fentanyl was given. Age, sex, weight of the children, and indication for surgery are shown in Table 1. There was no difference in intraoperative heart rate or respiratory rate between the groups. There was no significant difference in the FLACC scores throughout the postoperative duration of 24 h [Figure 2]. The mean duration of analgesia for the caudal group was 720.3 ± 430.1 min and for USG-IL/IH group was 808.3 ± 453.1 min, which was not significantly different [Table 2]. The Kaplan–Meier survival curves [Figure 3] for the two groups show that the time to first analgesic request was comparable between caudal group (range 548.3–892.2 min) and IL/IH group (range 627.2–989.5) (P-value 0.64 by log-rank test for equality in survivor function). Three children in the caudal group and none in USG-IL/IH had pain in the first 2 postoperative hours. Four children in the caudal epidural group and six children in USG- IL/IH group did not require any analgesic up to 24 h postoperatively. An average number of oral analgesics used was not different between the groups. Time to perform block was significantly higher for caudal compared to USG-IL/IH (547 ± 93 vs. 317 ± 179 s). There was no significant difference in parent's satisfaction for postoperative analgesia between the groups.
Figure 1.
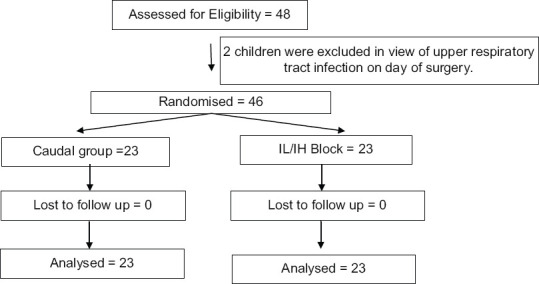
CONSORT Flow chart on randomization and allocation of patients
Table 1.
Demographic parameters
| Parameters | Caudal block | IL/IH block |
|---|---|---|
| Age (years) | 4.5±2.9 | 3.7±2.3 |
| Weight (kg) | 14.3±4.7 | 13.1±3.8 |
| Gender (Male: Female) | 21:2 | 21:2 |
| Indication for surgery (Hydrocele: Hernia) | 15:8 | 10:3 |
Values given are mean±SD or the number of patients
Figure 2.
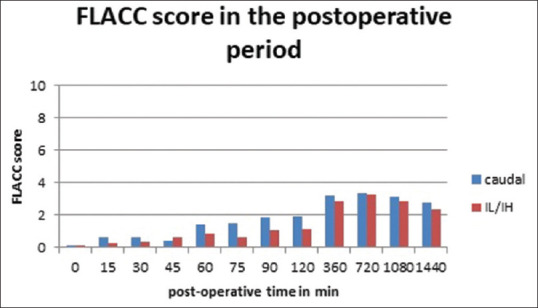
Postoperative face, legs, activity, cry, consolability pain score
Table 2.
Effectiveness of block in two groups
| Parameters | Caudal block | USG-IL/IH block | P |
|---|---|---|---|
| Block failures | 2 | 0 | 0.48 |
| Duration of postoperative analgesia (minutes) | 720.3±430.1 | 808.3±453.1 | 0.50 |
| Number of patients needing fentanyl in first 2 postoperative h | 3 | 0 | 0.23 |
| Number of doses of oral analgesics needed | 1.43+0.99 | 1.30+0.92 | 0.64 |
| Time taken for administration of block (seconds) | 547.3±93.7 | 317.4±179.8 | <0.001 |
| Parent satisfaction (%) | 73.6±13.9 | 72.1±14.2 | 0.717 |
Values given are number of patient or mean±SD
Figure 3.
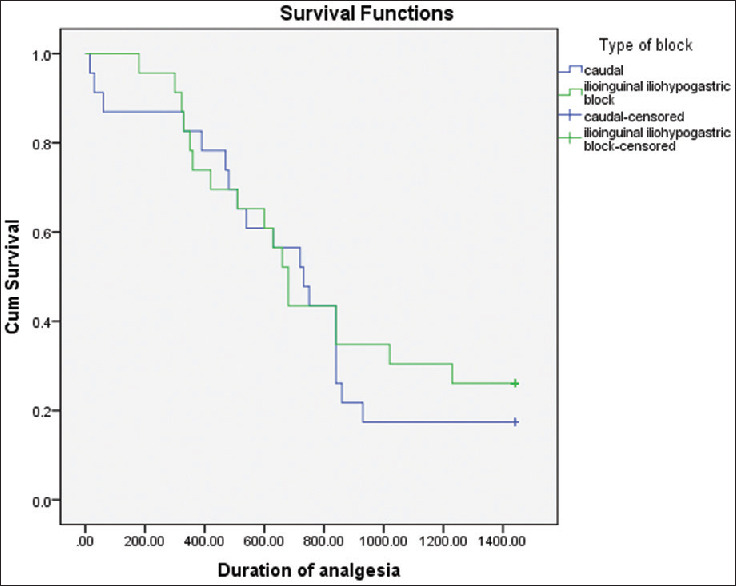
Kaplan–Meier survival plot for the duration of analgesia
One child in each group had bradycardia in the immediate postoperative period, which was treated with intravenous atropine. There was no difference in the postoperative heart rate between the groups. There was no difference between the groups for incidence of emergence delirium, PONV, time for ambulation, or voiding urine [Table 3]. Two children in USG-IL/IH group developed fever postoperatively, which could not be ascertained in the immediate postoperative period, although both the children developed upper respiratory tract infections on postoperative days 2 and 3.
Table 3.
Side effects and complication in two groups
| Parameters | Caudal block | IL/IH block | P |
|---|---|---|---|
| Emergence delirium | 2 | 1 | 0.500 |
| Bradycardia | 1 | 1 | 0.833 |
| PONV | 2 | 2 | 1.000 |
| Fever | 0 | 2 | 0.449 |
| Time for first voluntary voiding of urine (minutes) | 178.2±118.4 | 230.5±151.6 | 0.199 |
| Time taken for ambulation (minutes) | 388.3±148.6 | 357.3±169.7 | 0.510 |
PONV: postoperative nausea and vomiting. Values given are number of patient or mean±SD
Discussion
We found that the duration of postoperative analgesia provided by caudal epidural and ILIH with dexmedetomidine as an additive were comparable. Analgesia provided in both groups lasted for about 12–14 h, making both a good choice for postoperative analgesia for hernia surgery.
A previous study compared analgesia provided by caudal epidural to USG-IL/IH block using 0.25% bupivacaine and found that the mean duration of analgesia for the caudal group was 4.8 h and USG guided IL/IH block was 5.0 h, which was not statistically significant.[14] These results are similar to our study, although the duration of analgesia is significantly longer in both the groups in our study. Abualhassan et al. found that the duration of analgesia was significantly higher with USG-IL/IH block than blind caudal analgesia.[6] The average time for first rescue analgesia was longer in the USG- IL/IH block with 253 ± 102.6 min as compared to 219.6 ± 48.4 min in the caudal group, although this difference was not statistically significant. In our study, we found both techniques to be equally efficacious and provide analgesia for about 730–808 min. This prolonged duration in the present study is attributed to the addition of dexmedetomidine in both the groups as compared to only plain local anesthetics used in earlier studies.
We found two failures in the caudal analgesia group and no failures in USG-IL/IH technique; however, this difference was statistically not significant. Higher success in USG-IL/IH can be attributed to the accuracy provided by ultrasound guidance in the identification of anatomical structures as compared to its blind counterpart.
The advantage of the caudal epidural was that several additives could be added to local anesthetic to prolong the duration of analgesia. Many studies have been conducted using dexmedetomidine as the adjunct in caudal showing a prolongation in the duration of analgesia.[15,16,17]
Saadawy et al. compared the analgesic efficacy of caudal dexmedetomidine with bupivacaine as compared to bupivacaine alone and found a significant prolongation of the duration of analgesia by dexmedetomidine (18.5 ± 2.8 h vs. 6.2 ± 2.8 h).[18] In order to find the effective dose of dexmedetomidine, a study was conducted comparing caudal bupivacaine alone with bupivacaine and 1 and 2 μg/kg of dexmedetomidine for postoperative analgesia in pediatric patients undergoing infraumbilical surgeries.[13] The study found that the mean duration of analgesia provided by bupivacaine with 1 μg/kg dexmedetomidine was 809 min (652–965 min), bupivacaine with 2 μg/kg of dexmedetomidine was 880 min (733–1026 min), and plain bupivacaine was 396 min (343–448 min). The authors found more side effects in the 2 μg/kg dexmedetomidine group as compared to the 1 μg/kg group. Thus, dexmedetomidine in the dose of 1 μg/kg had comparable prolongation of postoperative analgesia to 2 μg/kg of dexmedetomidine with significantly lesser side effects. Therefore, we chose 1 μg/kg of dexmedetomidine for our study.
Several adjuncts now are being used in peripheral blocks as well. There are few studies comparing the efficacy of dexmedetomidine as an additive to local anesthetics for peripheral nerve blocks to prolong the duration of analgesia.[11,19,20] A meta-analysis of the studies on the use of alpha 2 adreno-receptor agonists showed that the addition of dexmedetomidine prolongs the duration of analgesia of the peripheral nerve blocks.[21] Lundblad et al. used dexmedetomidine as an adjunct to IL/IH nerve blocks for pediatric inguinal hernia repair and concluded that the time for first postoperative supplementation of analgesia was prolonged by 88% in dexmedetomidine group as compared to plain ropivacaine.[11] The mean duration of analgesia with the dexmedetomidine group was 7.6 h. In our study, too, we found a similar analgesic profile with the addition of dexmedetomidine.
The studies so far, including meta-analysis, have demonstrated that dexmedetomidine prolongs the duration of the central neuraxial block as well as peripheral nerve blocks.[22] There are many studies testing whether prolongation of the duration of perineural dexmedetomidine is caused by a peripheral mechanism of action or by central effects due to absorption and systemic redistribution of the perineurally administered dexmedetomidine.[23,24,25] But, to the best of our knowledge, there are no studies directly comparing the analgesic efficacy of dexmedetomidine in neuraxial block vs. peripheral nerve block. Comparing the results of our study results with previous studies, we can extrapolate that dexmedetomidine as an additive to local anesthetics prolonged the duration of analgesia in both caudal and USG-IL/IH block effectively. Hence, dexmedetomidine is a useful additive to local anesthetics in both caudal and USG-IL/IH block.
In the present study, the average time taken for performing caudal analgesia was significantly more than the USG-IL/IH block. The additional time is taken to position the patient laterally for a caudal epidural and turning them back to supine after the block was approximately 5 min, which was more in the caudal group than USG-IL/IH block. As USG-IL/IH block was performed in the supine position itself, it could be performed much faster. We found that IL/IH block could be performed much more easily, with less dependence on additional assistance (to look after the patient in lateral position for caudal). Previous studies also have shown that caudal epidural takes almost 10–15 min for the onset of analgesia, which is longer compared to peripheral nerve blocks. In a busy operating schedule, with many short procedures, the time and manpower needed for the performance of the block can become important. We could not find any previous studies comparing the ease of performance and time taken for the performance of blocks.
The main limitation of the study is, even though we noted that dexmedetomidine works equally effective in the central neuraxial block as well as peripheral block, we did not confirm it with either receptor distribution or blood concentration of dexmedetomidine in this study. We used the same dose of dexmedetomidine in USG-IL/IH and caudal epidural (1 μg/kg), but different doses of local anesthetic, 0.25 mL/kg for USG-IL/IH and 0.75 mL/kg for the caudal group, as per usual clinically effective dose recommendations. Whether the action of dexmedetomidine varies with dose at the different sites needs to be tested with further studies.
Conclusion
Both caudal epidural and USG-IL/IH block with dexmedetomidine as additive provide the comparable duration of postoperative analgesia with no significant side effects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lloyd-Thomas AR. Pain management in paediatric patients. Br J Anaesth. 1990;64:85–104. doi: 10.1093/bja/64.1.85. [DOI] [PubMed] [Google Scholar]
- 2.Markham SJ, Tomlinson J, Hain WR. Ilioinguinal nerve block in children. A comparison with caudal block for intra and postoperative analgesia. Anaesthesia. 1986;41:1098–103. doi: 10.1111/j.1365-2044.1986.tb12956.x. [DOI] [PubMed] [Google Scholar]
- 3.Willschke H, Marhofer P, Bösenberg A, Johnston S, Wanzel O, Cox SG, et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005;95:226–30. doi: 10.1093/bja/aei157. [DOI] [PubMed] [Google Scholar]
- 4.Grosse B, Eberbach S, Pinnschmidt HO, Vincent D, Schmidt-Niemann M, Reinshagen K. Ultrasound-guided ilioinguinal-iliohypogastric block (ILIHB) or perifocal wound infiltration (PWI) in children: a prospective randomized comparison of analgesia quality, a pilot study. BMC Anesthesiol. 2020;20:256. doi: 10.1186/s12871-020-01170-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Y, Wu T, Terry MJ, et al. Improved perioperative analgesia with ultrasound-guided ilioinguinal/iliohypogastric nerve or transversus abdominis plane block for open inguinal surgery: a systematic review and meta-analysis of randomized controlled trials. J Phys Ther Sci. 2016;28:1055–1060. doi: 10.1589/jpts.28.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdellatif AA. Ultrasound-guided ilioinguinal/iliohypogastric nerve blocks versus caudal block for postoperative analgesia in children undergoing unilateral groin surgery. Saudi J Anaesth. 2012;6:367–72. doi: 10.4103/1658-354X.105868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krishna Prasad GV, Khanna S, Jaishree SV. Review of adjuvants to local anesthetics in peripheral nerve blocks: Current and future trends. Saudi J Anaesth. 2020;14:77–84. doi: 10.4103/sja.SJA_423_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meenakshi Karuppiah NP, Shetty SR, Patla KP. Comparison between two doses of dexmedetomidine added to bupivacaine for caudal analgesia in paediatric infraumbilical surgeries. Indian J Anaesth. 2016;60:409–14. doi: 10.4103/0019-5049.183394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brummett CM, Norat MA, Palmisano JM, Lydic R. Perineural administration of dexmedetomidine in combination with bupivacaine enhances sensory and motor blockade in sciatic nerve block without inducing neurotoxicity in rat. Anesthesiology. 2008;109:502–11. doi: 10.1097/ALN.0b013e318182c26b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karan D, Swaro S, Mahapatra PR, Banerjee A. Effect of Dexmedetomidine as an Adjuvant to Ropivacaine in Ilioinguinal-Iliohypogastric Nerve Blocks for Inguinal Hernia Repair in Pediatric Patients: A Randomized, Double-Blind, Control Trial. Anesth Essays Res. 2018;12:924–929. doi: 10.4103/aer.AER_169_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lundblad M, Marhofer D, Eksborg S, Lönnqvist PA. Dexmedetomidine as adjunct to ilioinguinal/iliohypogastric nerve blocks for paediatric inguinal hernia repair: An exploratory randomised controlled trial. Paediatr Anaesth. 2015;25:897–905. doi: 10.1111/pan.12704. [DOI] [PubMed] [Google Scholar]
- 12.Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatric Nursing. 1997;23:293–7. [PubMed] [Google Scholar]
- 13.Al Zaben KR, Udaisat I, Abu Halaweh SA, Al Ghanem SM, Al Mustafa MM, Aljabari AN, et al. Comparison of caudal bupivacaine alone with bupivacaine plus two doses of dexmedetomidine for postoperative analgesia in paediatric patients undergoing infra-umbilical surgery: A randomised controlled double-blinded study. Paediatr Anaesth. 2015;25:883–90. doi: 10.1111/pan.12686. [DOI] [PubMed] [Google Scholar]
- 14.Ravi T, Kumar ND, Kumar BS. Ultrasound guided nerve block versus caudal block for post-operative analgesia in children undergoing unilateral groin surgery. Int Arch Integr Med. 2016;3:115–25. [Google Scholar]
- 15.El-Hennawy AM, Abd-Elwahab AM, Abd-Elmaksoud AM, El-Ozairy HS, Boulis SR. Addition of clonidine or dexmedetomidine to bupivacaine prolongs caudal analgesia in children. Br J Anaesth. 2009;103:268–74. doi: 10.1093/bja/aep159. [DOI] [PubMed] [Google Scholar]
- 16.Goyal V, Kubre J, Radhakrishnan K. Dexmedetomidine as an adjuvant to bupivacaine in caudal analgesia in children. Anesth Essays Res. 2016;10:227–232. doi: 10.4103/0259-1162.174468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anand VG, Kannan M, Thavamani A, Briget MJ. Effects of dexmedetomidine added to caudal ropivacaine in paediatric lower abdominal surgeries. Indian J Anaesth. 2011;55:340–6. doi: 10.4103/0019-5049.84835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saadawy I, Boker A, Elshahawy MA, Almazrooa A, Melibary S, Abdellatif AA, et al. Effect of dexmedetomidine on the characteristics of bupivacaine in a caudal block in pediatrics. Acta Anaesthesiol Scand. 2009;53:251–6. doi: 10.1111/j.1399-6576.2008.01818.x. [DOI] [PubMed] [Google Scholar]
- 19.El-Rahmawy GF, Hayes SM. Efficacy of dexmedetomidine addition to bupivacaine on the quality of blind fascia iliaca compartment block in children undergoing femur fracture surgery. Egypt J Anaesth. 2013;29:137–42. [Google Scholar]
- 20.Gihan MO, Refaie A, Aboushanab O, Neamat I, Mossad A. Addition of dexmedetomidine to bupivacaine for greater palatine nerve block prolongs postoperative analgesia after cleft palate repair. European J Anaeth. 2010;27:280–4. doi: 10.1097/EJA.0b013e3283347c15. [DOI] [PubMed] [Google Scholar]
- 21.Lundblad M, Trifa M, Kaabachi O, Ben Khalifa S, Fekih Hassen A, Engelhardt T, et al. Alpha- 2 adreno receptor agonists as adjuncts to peripheral nerve blocks in children: A meta-analysis. Paediatr Anaesth. 2016;26:232–8. doi: 10.1111/pan.12825. [DOI] [PubMed] [Google Scholar]
- 22.Abdallah FW, Brull R. Facilitatory effects of perineural dexmedetomidine on neuraxial and peripheral nerve block: A systematic review and meta-analysis. Br J Anaesth. 2013;110:915–25. doi: 10.1093/bja/aet066. [DOI] [PubMed] [Google Scholar]
- 23.Marhofer D, Kettner SC, Marhofer P, Pils S, Weber M, Zeitlinger M. Dexmedetomidine as an adjuvant to ropivacaine prolongs peripheral nerve block: A volunteer study. Br J Anaesth. 2013;110:438–42. doi: 10.1093/bja/aes400. [DOI] [PubMed] [Google Scholar]
- 24.Andersen JH, Grevstad U, Siegel H, Dahl JB, Mathiesen O, Jæger P. Does dexmedetomidine have a perineural mechanism of action when used as an adjuvant to ropivacaine?: A paired, blinded, randomized trial in healthy volunteers. Anesthesiology. 2017;126:66–73. doi: 10.1097/ALN.0000000000001429. [DOI] [PubMed] [Google Scholar]
- 25.Abdallah FW, Chan DT, Niazi VW, Ogilvie-Harris AU, Oldfield DJ, Patel S, et al. IV and perineural dexmedetomidine similarly prolong the duration of analgesia after interscalene brachial plexus block: A randomized, three-arm, triple-masked, placebo-controlled trial. Anesthesiology. 2016;124:683–95. doi: 10.1097/ALN.0000000000000983. [DOI] [PubMed] [Google Scholar]


