Abstract
We report a case of a 54-year-old immunocompetent male who had lung abscess secondary to Streptococcus intermedius that led to discitis by contiguous spread of infection. He initially presented with constant chest pain for 6 weeks that radiated to lower back, with no fever, chills or weight loss. He denied smoking cigarettes, alcohol use or any illicit drug. On investigation, a mass was identified on the posterior medial aspect of the right lower lobe with direct infiltration into right side of the T5–T6 vertebral bodies. Histopathology identified organising pneumonia with abscess. Tissue cultures showed S. intermedius, and were negative for other microorganisms. This case highlights a rare presentation of S. intermedius discitis by contiguous spread of infection from posterior right lower lobe lung abscess. S. intermedius usually occurs in older patients with pulmonary infections complicated with pleural effusion or lung abscess, but can present in young patients with no clear symptoms of lung infection, like our patient.
Keywords: pneumonia (infectious disease), respiratory system, infections
Background
Streptococcus anginosus group (SAG) is a gram-positive coccus that is a normal flora of the oral cavity, gastrointestinal tract and respiratory tract. Three different species have been classified into the SAG: S. intermedius, S. constellatus and S. anginosus. S. intermedius is an important cause of pneumonia, pulmonary abscesses and empyema.1
This report presents a case of lung abscess in a young immunocompetent male with no clear symptoms of lung infection, he had a clear chest X-ray on presentation, but on further investigations, a large mass identified on the posterior medial aspect of the right lower lobe with direct infiltration into the right side of the T5 and T6 vertebral bodies.
This represents a diagnostic dilemma and emphasises on a thorough history and physical examination. On literature review, few cases have shown empyema and lung abscesses caused by S. intermedius, none with contiguous spread to vertebra/disc.
Case presentation
A 54-year-old man with a history of hypertension and diabetes presented with right-sided chest pain. The pain was started 6 weeks ago, it was 5/10 to 10/10 in severity, sharp in nature, constant, radiated to lower back and right shoulder, it was associated with cough, nausea and vomiting and was aggravated by coughing and deep breathing. The patient denied fever, chills or weight loss, but on review of systems he mentioned that he has been having a problem with his left tooth, which had cracked recently, and has been painful for him. He denied smoking cigarettes, alcohol use or any illicit drug. On physical examination, vital signs on admissions were blood pressure 181/90 mm Hg, heart rate (86 beats/min), respiratory rate (20 breaths/min), temperature 37.1°C and oxygen saturation 98% on room air. Cardiovascular examination revealed normal heart rate with a regular rhythm, normal S1 and S2, with no murmurs. On respiratory examination, normal breathing bilaterally, no wheeze or crackles, but the patient had tenderness along the right ribs. He had poor dental hygiene with tooth caries. The rest of the physical examination was unremarkable.
Investigations
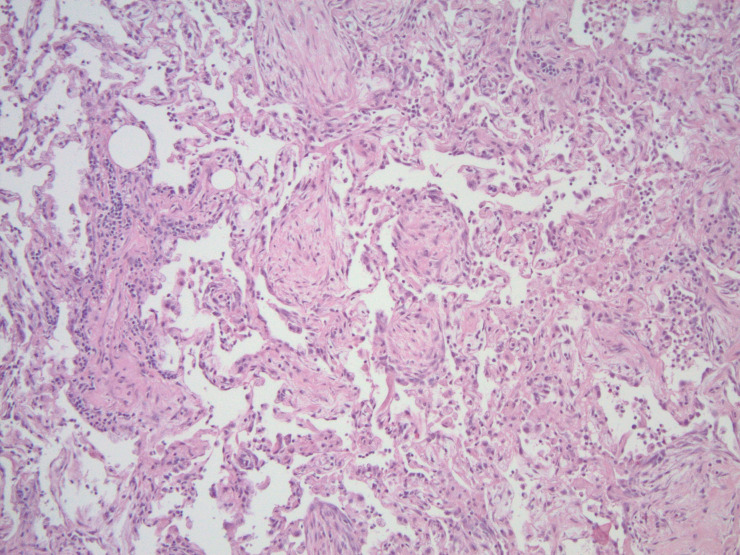
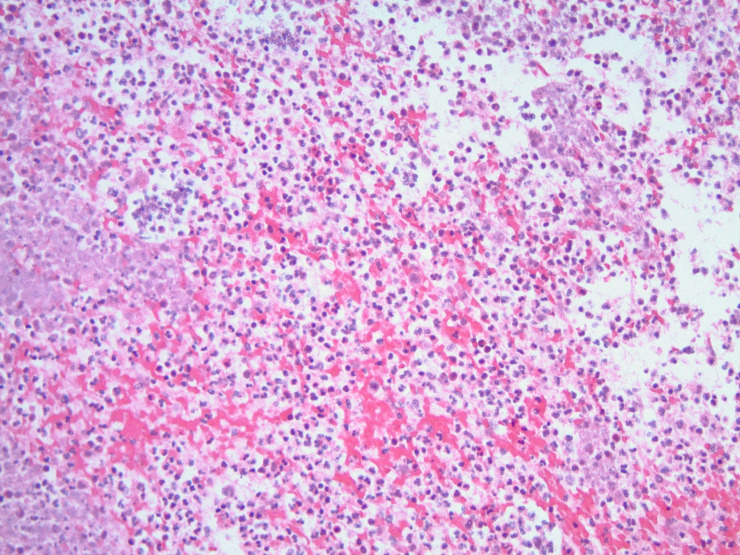
Complete blood count and basic metabolic panel were within normal range. D-dimer was elevated to 0.72 mcg/mL (normal is less than 0.5 mcg/mL). ECG showed normal sinus rhythm with no ischaemic changes, chest X-ray showed no evidence of acute cardiopulmonary processes. Due to concern of pulmonary embolism (PE), CT for pulmonary embolism was ordered and was negative for PE, but it showed 4.5 cm soft tissue mass in the right posterior mediastinum involving the superior azygo-oesophageal recess, which was not seen on prior imaging (figure 1). MRI of the chest confirmed the mass in the posterior medial aspect of the right lower lobe with direct infiltration into right side of the T5 and T6 vertebral bodies with lymphadenopathy (figure 2).
Figure 1.
Irregular radiolucent 4.5 cm soft tissue mass in the right posterior mediastinum involving the superior azygo-oesophageal recess.
Figure 2.
MRI of the chest confirmed the mass in the posterior medial aspect of the right lower lobe with direct infiltration into the right side of the T5 and T6 vertebral bodies with lymphadenopathy.
Due to concern for cancer of unknown primary origin, CT scan of the abdomen and pelvis with contrast was done but was inconclusive. CT-guided biopsy of the paraspinal mass was performed and showed fibroconnective tissue with acute and chronic inflammation, dense collagen deposition, no evidence of malignancy, lymphoma or soft tissue tumour.
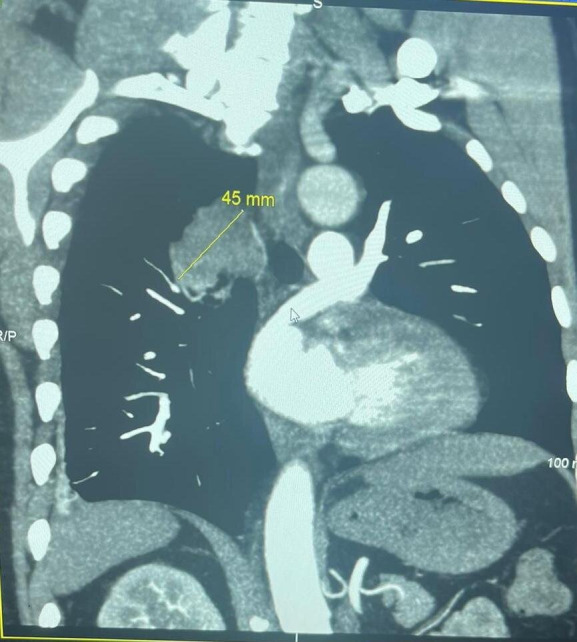
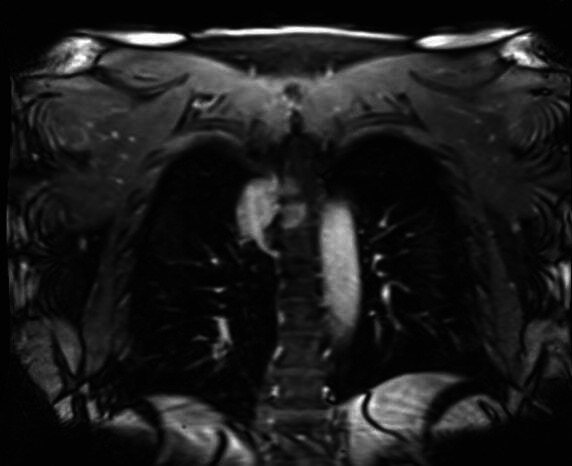
Right posterior lateral thoracotomy with pulmonary decortication along with excision of the posterior mediastinal mass was performed by a cardiothoracic surgeon. Histopathology identified organising pneumonia with abscess and pleuritis (figures 3 and 4). Tissue cultures showed S. intermedius and were negative for anaerobes, mycobacteria and fungi, and no evidence of malignancy was seen. Serial blood cultures were negative. HIV testing was negative.
Figure 3.
Histopathology identified organising pneumonia.
Figure 4.
Histopathology showing lung abscess.
Differential diagnosis
The differential diagnosis includes mainly malignancy, but the rapid progression of a mass that developed within 6 weeks was less likely to be a primary tumour, so the concern of metastasis with unknown primary tumour was high, although extensive work-up as described before was negative for malignancy. Another possible differential diagnosis is a paraspinal abscess which may develop after chronic infection especially as this patient had poor dental hygiene.
Treatment
Intravenous metronidazole and ceftriaxone were started empirically while the patient was in the hospital for 3 days. S. intermedius susceptibility came back pansensitive.
Outcome and follow-up
The patient improved clinically and was discharged on high dose co-amoxiclav for 3 weeks based on sensitivity. Follow-up CT scan of the chest after 1 month showed no acute changes besides postsurgical changes from wedge resection of the right lower lobe. The patient continued to be asymptomatic.
Discussion
Lung abscess is a type of liquefactive necrosis of the lung parenchyma. Most lung abscesses arise as a complication of aspiration. They are typically polymicrobial and indolent in onset but less frequently can complicate acute monomicrobial infections with pyogenic bacteria like SAG. SAG-based infections account for 13%–50% of all cases of pulmonary abscess.2
A retrospective, observational, cohort study, between the years 2009 and 2015 done by Kobo et al, which examined the association between SAG species and the presence of pyogenic infection,3 concluded that S. intermedius was associated with pyogenic non-bacteraemic infections, while S. anginosus and S. constellatus were associated with bacteraemia with no abscess or empyema formation. A retrospective review of 25 cases of pulmonary infection caused by SAG revealed significant mortality (24%) and was characterised by a strong male predominance and non-specific symptoms.4
S. intermedius infections were mainly identified in older patients with pulmonary infections complicated with pleural effusion and/or lung abscess. Predisposing conditions noted with infection by SAG include previous surgery, trauma, diabetes, immunodeficiency and malignancy, but may also be related to hygiene or the patient’s overall general health condition.5
Our case is unique, as our patient is relatively young and immunocompetent and he did not report fever, chills or any other symptoms that may indicate lung infection. Possible risk factors are diabetes and poor dental hygiene. A possible mechanism for abscess formation is aspiration, although he had no difficulty swallowing or any residual weakness on physical examination, this presented a dilemma when we found that the patient had such presentation.
In our patient S. intermedius caused lung abscess located in posterior right lower lobe with direct extension to vertebrae causing discitis, we did not find similar presentation on the literature review.
Patient’s perspective.
The patient stated that “I was scared when the doctors described the finding of MRI of the chest and told me about the possibility of cancer. Luckily enough, it was an abscess and I was so happy that it got removed and I was discharged from the hospital. On the follow-up, I was still having some pain but improved overtime”.
Learning points.
Streptococcus anginosus is an important cause of rapidly progressive purulent infection at different body sites including lung parenchyma.
This case highlights a rare and unusual presentation of S. intermedius discitis by contiguous spread of infection from posterior lung abscess.
S. intermedius infections were mainly identified in older patients with pulmonary infections complicated with pleural effusion and lung abscess but still can occur in young patients with no clear symptoms of lung infection, like our case.
Footnotes
Contributors: NM was involved in taking care of the patient from the day of admission until discharge, planned to write the case with the help of coauthors, did an extensive literature review, wrote a detailed case presentation and part of the discussion and learning points. SNR helped also in the literature review, reviewing the patient’s chart and wrote part of the discussion. AAS did analysis and interpretation of data, also reviewed the design of the case. WH did help also in the literature review and analysis and interpretation of data and did review the case for finalising it for publication.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Noguchi S, Yatera K, Kawanami T, et al. Pneumonia and empyema caused by Streptococcus intermedius that shows the diagnostic importance of evaluating the microbiota in the lower respiratory tract. Intern Med 2014;53:47–50. 10.2169/internalmedicine.53.0971 [DOI] [PubMed] [Google Scholar]
- 2.Shinzato T, Saito A. The Streptococcus milleri group as a cause of pulmonary infections. Clin Infect Dis 1995;21 Suppl 3:S238–43. 10.1093/clind/21.Supplement_3.S238 [DOI] [PubMed] [Google Scholar]
- 3.Kobo O, Nikola S, Geffen Y, et al. The pyogenic potential of the different Streptococcus anginosus group bacterial species: retrospective cohort study. Epidemiol Infect 2017;145:3065–9. 10.1017/S0950268817001807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong CA, Donald F, Macfarlane JT. Streptococcus milleri pulmonary disease: a review and clinical description of 25 patients. Thorax 1995;50:1093–6. 10.1136/thx.50.10.1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.. Available: https://hardydiagnostics.com/wpcontent/uploads/2016/05/Streptococcus-anginosis-group-by-Kerry-Pierce.pdf