Abstract
BACKGROUND AND PURPOSE:
There is a paucity of evidence regarding the safety of endovascular treatment for patients with acute ischemic stroke due to primary medium-vessel occlusion. The aim of this study was to examine the willingness among stroke physicians to perform endovascular treatment in patients with mild-yet-disabling deficits due to medium-vessel occlusion.
MATERIALS AND METHODS:
In an international cross-sectional survey consisting of 7 primary medium-vessel occlusion case scenarios, participants were asked whether the presence of personally disabling deficits would influence their decision-making for endovascular treatment despite the patients having low NIHSS scores (<6). Decision rates were calculated on the basis of physician characteristics. Univariable logistic regression clustered by respondent and scenario identity was performed.
RESULTS:
Three hundred sixty-six participants from 44 countries provided 2562 answers to the 7 medium-vessel occlusion scenarios included in this study. In scenarios in which the deficit was relevant to the patient's profession, 56.9% of respondents opted to perform immediate endovascular treatment compared with 41.0% when no information regarding the patient's profession was provided (risk ratio = 1.39, P < .001). The largest effect sizes were seen for female participants (risk ratio = 1.68; 95% CI, 1.35–2.09), participants older than 60 years of age (risk ratio = 1.61; 95% CI, 1.23–2.10), those with more experience in neurointervention (risk ratio = 1.60; 95% CI, 1.24–2.06), and those who personally performed >100 endovascular treatments per year (risk ratio = 1.63; 95% CI, 1.22–2.17).
CONCLUSIONS:
The presence of a patient-relevant deficit in low-NIHSS acute ischemic stroke due to medium-vessel occlusion is an important factor for endovascular treatment decision-making. This may have relevance for the conduct and interpretation of low-NIHSS endovascular treatment in randomized trials.
In 2015, five randomized controlled trials demonstrated the safety and efficacy of endovascular therapy (EVT) for acute ischemic stroke (AIS) due to large-vessel occlusion.1 The observed superiority over best medical management, however, partially resulted from strict inclusion criteria, including restriction of randomization to patients with more severe strokes, as determined by the NIHSS score. As a result, there is no consensus on whether EVT should be offered to patients with mild stroke symptoms (NIHSS score <6). While clinical outcomes of conservatively treated patients with low-NIHSS AIS are more favorable compared with those with larger deficits, approximately 27%–35% of these patients are either functionally dependent at discharge or deceased,2-4 partly due to the risk of early neurologic deterioration (12%–15%)5,6 without EVT. Furthermore, not all low-NIHSS strokes are necessarily mild from the patient's perspective; for example, an NIHSS score of 2 due to complete hemianopia would be devastating to a truck driver. The current literature presents conflicting results regarding the safety and efficacy of EVT in patients with low NIHSS scores with large-vessel occlusion, and multiple randomized trials are presently underway (Endovascular Therapy for Low NIHSS Ischemic Strokes [ENDOLOW], ClinicalTrials.gov identifier: NCT04167527; InExtremis/Minor Stroke Therapy Evaluation [MOSTE], ClinicalTrials.gov identifier: NCT03796468), which will hopefully provide a clearer picture of the optimal treatment strategy.7,8
At the same time, EVT for other underrepresented trial subgroups such as those with medium-vessel occlusions (MeVOs) is being discussed. MeVOs, defined as occlusions of the M2, M3, A2, A3, P2, or P3 segment with disabling deficits,9,10 account for approximately 25%–40% of all AIS.11 Current recanalization rates with intravenous alteplase range from 21% to 43%, with only approximately half of these patients achieving excellent outcome.12 This result underscores the need for a more effective treatment strategy, with EVT being the most obvious choice.
In an effort to understand current clinician perspectives concerning the management of MeVO stroke, a case-based survey (MeVO–Finding Rationales and Objectifying New Targets for IntervEntional Revascularization in Stroke [MeVO-FRONTIERS]) was conducted. We sought to determine how the interplay of patient profession, physician and patient characteristics, and the specific nature of “minor” deficits influences physicians' EVT decision-making in MeVO stroke.
MATERIALS AND METHODS
Survey Design
An international online, cross-sectional, anonymous survey (MeVO FRONTIERS) using Qualtrics (www.qualtrics.com) was conducted among stroke physicians to understand their current treatment practice and endovascular decision-making in AIS caused by MeVO. The survey consisted of 7 cases with clinical descriptions and illustrative images. The cases were subdivided into 3–6 consecutive scenarios in which 1 key feature was changed. Respondents were asked whether and how they would treat the described patient. The survey took approximately 30 minutes to complete, and participants were required to answer each question before moving on (“forced response”). Response data were obtained from November 12, 2020 to December 31, 2020. Approval by the local research ethics board (The Conjoint Health Research Ethics Board [CHREB] of the University of Calgary) was obtained. Data used in the current study are available from the author on reasonable request.
Survey Participants
Approximately 1400 stroke physicians (neurologists, interventional neurologists and neuroradiologists, neurosurgeons, and other physicians directly involved in acute stroke care) from 44 countries were invited to participate in this Web-based survey. There were no restrictions with regard to case volume, experience, or academic-versus-nonacademic centers. Before accessing the case scenarios, physicians were asked to provide the following personal data: age, sex, years of stroke-treatment experience, annual personal and center stroke treatment volumes, geographic region, subspecialty, and hospital setting.
Clinical Case Scenarios
Overall, the survey comprised of 7 MeVO narrative cases (4 primary MeVOs and 3 secondary MeVOs) with 3–6 clinical case vignettes each. Noncontrast head CT and/or digital subtraction angiography images were provided for each case. The accompanying clinical case vignettes provided patient age, profession, medical history, stroke severity and imaging details (ASPECTS), location of the occlusion, and, if relevant, CT perfusion–based core and penumbral volumes. For each combination of images and clinical factors, participants were asked to state whether they would treat the patient with EVT. One key piece of information was then changed in each subsequent case vignette (eg, age, stroke severity, ischemic core volume), to assess changes in decision-making based on these items. The current study was restricted to cases in which the patients in question had low NIHSS scores (<6). For detailed descriptions of all case-scenarios that were included in this study see the Online Supplemental Data.
Statistical Analysis
Case scenarios were subdivided into cases in which a profession was listed (ie, in which a person-relevant deficit that would substantially impair the patient in his or her profession was present) and those without any information of this nature. Treatment decisions were binarized into immediate EVT yes/no, the latter including the options “no EVT” and “EVT only if the patient worsens.” Participant baseline characteristics and response data were analyzed using descriptive statistics, and group differences in the willingness to endovascularly treat patients with mild MeVO strokes were assessed using the χ2 test. Univariable regression of the effect of a person-relevant deficit on EVT decision-making was performed, stratified by participant baseline characteristics (respondent's age and sex, years of experience, personal and center stroke-treatment volume per year, and hospital setting and specialty) and clustered for participant and scenario identity. To control for multiple testing, we performed subgroup interaction analyses for profession and each of the respondent-variable subgroups. Risk ratios (RRs) derived from binary logistic regression are reported. P values <.05 were considered statistically significant. Only completed surveys were included in the analysis. Data analysis was performed in STATA 16.1 (StataCorp), and figures were created with Power BI Desktop 2016 and the Mapbox Visual plugin (Microsoft).
RESULTS
Respondent Demographics
A total of 366 physicians (84.2% male) from 44 countries completed the survey. Most (170, 46.5%) were interventional neuroradiologists, followed by neurologists (97, 26.5%), neurosurgeons (39, 10.7%), interventional neurologists (36, 9.8%), interventional radiologists (18, 4.9%), and other physicians involved in acute stroke care (6, 1.6%). A total of 2562 responses were obtained for the primary MeVO cases with low NIHSS scores. Detailed participant characteristics are listed in the Online Supplemental Data.
EVT in Low-NIHSS MeVO
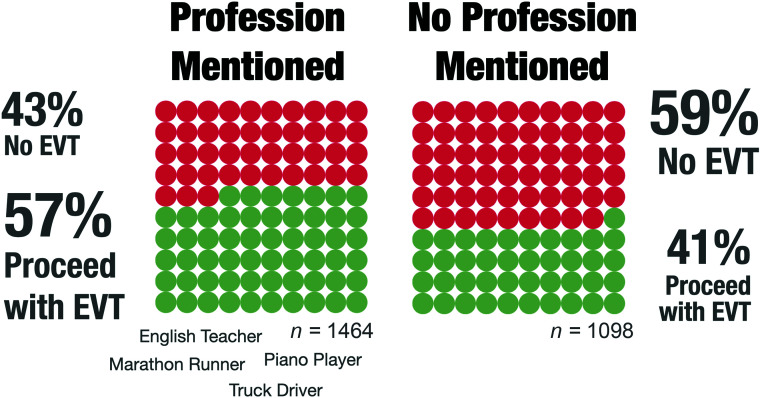
Figure 1 shows the main results of the study. In scenarios in which the occlusion-related deficit was relevant to the patient's profession, respondents were more likely to perform immediate EVT (56.9% in favor of EVT, 833/1464) compared with those case vignettes in which no information regarding the patient's profession was provided (41.0% in favor of EVT, 450/1098; RR = 1.39, P < .001.
FIG 1.
Willingness to perform immediate EVT in patients with NIHSS < 6, stratified by patients with mild-yet-disabling deficits with respect to their professions versus patients with mild deficits without a described profession.
Physician Factors Influencing EVT Decisions in Low-NIHSS MeVO
Subgroup analyses of each variable revealed no significant interactions between profession and each of the respondent-variable subgroups on EVT decision-making (Online Supplemental Data); the presented results are, therefore, exploratory in nature. In almost every subgroup of physician characteristics, the presence of a deficit relevant to the individual's livelihood led to a significantly increased chance of proceeding with immediate EVT (Online Supplemental Data). The most prominently influencing factors appeared to be sex, age, experience, and personal EVT treatment volume per year. Female participants were more likely to choose immediate EVT (RR = 1.68; 95% CI, 1.35–2.09; P < .001), as were those older than 60 years of age (RR = 1.61; 95% CI, 1.23–2.10; P < .001). Physicians at either end of the spectrum with respect to years of experience were the most likely to select immediate EVT for patients with a described profession (0–5 years of experience: RR = 1.49; 95% CI, 1.19–1.86; P < .001; >20 years of experience: RR = 1.60; 95% CI, 1.24–2.06; P < .001). Annual stroke-treatment volume also played a role, particularly for participants performing >100 procedures per year (RR = 1.63; 95% CI, 1.22–2.17; P < .001).
Within the no EVT responses, most physicians chose no EVT rather than performing EVT only if the patient worsens, irrespective of the presence of a patient-relevant deficit (54.6% versus 45.4%, P = .57).
Regional Factors Influencing EVT Decisions in Low-NIHSS MeVO
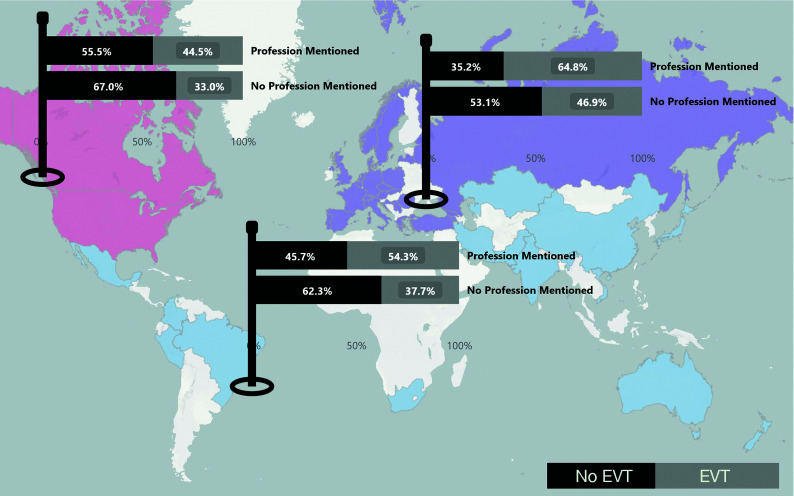
EVT decision rates differed significantly by the respondents' geographic location (Fig 2). In general, participants from Europe and the rest of the world (comprising Africa, Asia and the Pacific, the Middle East, and South and Latin America) were more willing to treat patients with low NIHSS scores, regardless of the patient's profession (716/1253, 57.1%, and 304/644, 47.2%, respectively), compared with physicians working in North America (263/665, 39.6%). Indeed, the North American group was the only one still less likely to perform EVT in the presence of a patient-relevant deficit, with 44.5% (169/380) for EVT.
FIG 2.
Geographic differences in the decision to proceed with immediate EVT, stratified by patients with mild-yet-disabling deficits with respect to their professions versus patients with mild deficits without a described profession. In North America, physicians would have treated patients with low NIHSS scores and personally disabling deficits in 44.5% (169/380) of cases, in contrast to 33% (94/285) of cases for which information regarding a profession was not provided. In Europe and the rest of the world (comprising Africa, Asia and the Pacific, the Middle East, and South and Latin America), the practitioners were in favor of immediate EVT in 64.8% (464/716) and 54.3% (200/368) in patients with a personally relevant deficit, respectively, compared with 46.9% (252/537) and 37.7% (104/276), respectively, of scenarios in which a personally disabling deficit was not mentioned.
DISCUSSION
In this survey-based study, we found that physicians were approximately 50% more willing to treat mild-deficit MeVO strokes with EVT if the deficits were personally disabling with respect to a patient's profession (56.9 versus 41.0%). Our results demonstrate the importance of individual patient factors for EVT decision-making in AIS. The largest effect sizes were seen for female participants, as well as those who were older than 60 years of age, more experienced in neurointervention (>20 years), and having a higher annual personal EVT case volume (>100). The latter findings are in some ways consistent: Physicians who are older, more experienced, and regularly perform EVT are more familiar with novel devices and techniques and are more likely to have encountered cases with low-NIHSS MeVO in their clinical practice. As a result, they may be more confident in their skills with respect to such cases. The fact that women were more likely to opt for EVT in this particular population could be due to a number of reasons: Female respondents comprised only 15% of the participant population, possibly inflating the results, and most (72%) were from high-volume centers (>100 EVTs/year). Thus, the female participants may have also had more experience with such scenarios.
The results of this survey highlight the interplay of factors currently relevant to stroke-treatment decision-making. While a previous study demonstrated the willingness of physicians to pursue EVT in patients with low-NIHSS strokes due to large-vessel occlusion,13 the consensus becomes more vague for MeVOs. Providing clarity for this patient subgroup is important for several reasons: AIS due to primary MeVO is commonly assumed to be milder than cases due to large-vessel occlusion.12 Furthermore, MeVOs tend to result in a more heterogeneous clinical presentation.14 At the same time, the current rates of excellent outcome after best medical management in AIS due to M2 and M3 occlusions are moderate, ranging from 21% to 55%.15-17
Finally, not all low NIHSS scores are equal, with varying outcomes observed for such AIS patient groups.4 A study that looked at differences in outcome between 2 syndromic low-NIHSS patient collectives (level of consciousness and language versus right motor function) found that those in the latter category had lower morbidity and mortality rates, suggesting that identical NIHSS scores at presentation may still translate to very different patient prognoses.18 These findings are important from a trial perspective because the inclusion of patients with low NIHSS scores has the potential for biased interpretation or “cherry-picking” of results.
Taken together, the results of the current survey and the above studies point toward a need for a case-by-case risk-benefit analysis for low-NIHSS MeVO cases.
Limitations
A major limitation of this study comes from the construction of the case scenarios. Their design to best reflect the real-world situation introduces some inherent confounding factors. For example, we could not examine the effects of patient-specific factors, such as age, on the decision to treat because all the patients with low NIHSS scores were younger (younger than 65 years of age). Furthermore, the occlusion sites were specifically selected to have an impact on the patient profession. Although the effect of scenario characteristics on EVT decision-making was not analyzed in this study, participants may have been more willing to perform EVT for occlusions of the M2 segment as opposed to those of the A3 segment, for example. We were also unable to perform a direct comparison of scenarios with and without information regarding profession because other features of the vignette were simultaneously changed. Because there is no international registry of stroke physicians or interventionalists, participant enrollment was based on institutional networks and co-operations. The participant sample may therefore not be representative of the entire stroke community. In addition, while survey responses reflect participants' attitudes, they are not necessarily equivalent to the decision-making processes of routine clinical practice. Finally, participants were provided with radiologic images for each case, with anatomic details that are not generalizable to all occlusions of a particular vessel segment. Despite these limitations, we believe that this study provides important insight into physician decision-making for EVT in MeVO strokes with mild neurologic deficits.
CONCLUSIONS
In this survey, the presence of a patient-relevant deficit in low-NIHSS AIS due to MeVO had a significant impact on physicians' decision-making in favor of immediate EVT, highlighting the importance of not only guideline recommendations but also patient-specific factors for the current stroke community.
ACKNOWLEDGMENTS
The authors acknowledge the survey participants for their invested time and effort.
ABBREVIATIONS:
- AIS
acute ischemic stroke
- EVT
endovascular therapy
- RR
risk ratio
- MeVO
medium-vessel occlusion
Footnotes
Disclosures: Nobuyuki Sakai—UNRELATED: Grants/Grants Pending: Daiichi Sankyo, NeuroVasc Technologies, Medtronic, Terumo, Comments: modest*; Payment for Lectures Including Service on Speakers Bureaus: Asahi-Intec, Johnson and Johnson, Medtronic, Stryker, Terumo, Comments: modest. Jens Fiehler—UNRELATED: Consultancy: Acandis, Codman, Cerenovus, Medtronic, MicroVention, Penumbra, phenox, Stryker; Grants/Grants Pending: Acandis, Medtronic, MicroVention, Stryker*; Stock/Stock Options: Tegus; OTHER RELATIONSHIPS: CEO of eppdata. Michael Chen—RELATED: Consulting Fee or Honorarium: Penumbra, Genentech, Medtronic, Stryker, MicroVention, Imperative Health. Mayank Goyal—UNRELATED: Consultancy: Medtronic, Stryker, Microvention, Mentice; Grants/Grants Pending: Medtronic, Cerenovus*; Royalties: GE Healthcare, MicroVention. *Money paid to the institution.
References
- 1. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 2. Barber PA, Zhang J, Demchuk AM, et al. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology 2001;56:1015–20 10.1212/WNL.56.8.1015 [DOI] [PubMed] [Google Scholar]
- 3. Goldhoorn RB, Mulder MJ, Jansen IG, et al. MR CLEAN Registry investigators. Safety and outcome of endovascular treatment for minor ischemic stroke: results from the Multicenter Clinical Registry of Endovascular Treatment of Acute Ischemic Stroke in the Netherlands. J Stroke Cerebrovasc Dis 2019;28:542–49 10.1016/j.jstrokecerebrovasdis.2018.10.029 [DOI] [PubMed] [Google Scholar]
- 4. Kenmuir CL, Hammer M, Jovin T, et al. Predictors of outcome in patients presenting with acute ischemic stroke and mild stroke scale scores. J Stroke Cerebrovasc Dis 2015;24:1685–89 10.1016/j.jstrokecerebrovasdis.2015.03.042 [DOI] [PubMed] [Google Scholar]
- 5. Seners P, Ben Hassen W, Lapergue B, et al. MINOR-STROKE Collaborators. Prediction of early neurological deterioration in individuals with minor stroke and large-vessel occlusion intended for intravenous thrombolysis alone. JAMA Neurol 2021;78:321–28 10.1001/jamaneurol.2020.4557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim JT, Park MS, Chang J, et al. Proximal arterial occlusion in acute ischemic stroke with low NIHSS scores should not be considered as mild stroke. PLoS One 2013;8:e70996 10.1371/journal.pone.0070996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Turc G, Bhogal P, Fischer U, et al. European Stroke Organisation (ESO): European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy in Acute Ischaemic Stroke Endorsed by Stroke Alliance for Europe (SAFE). Eur Stroke J 2019;4:6–12 10.1177/2396987319832140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ospel JM, Kashani N, Turjman F, et al. Discrepancies between current and ideal endovascular stroke treatment practice in Europe and North America: results from UNMASK EVT—a multidisciplinary survey. Interv Neuroradiol 2020;26:420–24 10.1177/1591019920908131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saver JL, Chapot R, Agid R, et al. Distal Thrombectomy Summit Group. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke 2020;51:2872–84 10.1161/STROKEAHA.120.028956 [DOI] [PubMed] [Google Scholar]
- 10. Goyal M, Ospel JM, Menon BK, et al. MeVO: the next frontier? J Neurointerv Surg 2020;12:545–47 10.1136/neurintsurg-2020-015807 [DOI] [PubMed] [Google Scholar]
- 11. Goyal M, Kappelhof M, McDonough R, et al. Secondary medium vessel occlusions: when clots move north. Stroke 2021;52:1147–53 10.1161/STROKEAHA.120.032799 [DOI] [PubMed] [Google Scholar]
- 12. Ospel JM, Menon BK, Demchuk AM, et al. Clinical course of acute ischemic stroke due to medium vessel occlusion with and without intravenous alteplase treatment. Stroke 2020;51:3232–40 10.1161/STROKEAHA.120.030227 [DOI] [PubMed] [Google Scholar]
- 13. Ospel JM, Kim B, Heo JH, et al. Endovascular treatment decision-making in acute ischemic stroke patients with large vessel occlusion and low National Institutes of Health Stroke Scale: insights from UNMASK EVT, an international multidisciplinary survey. Neuroradiology 2020;62:715–21 10.1007/s00234-020-02371-6 [DOI] [PubMed] [Google Scholar]
- 14. Kunz WG, Almekhlafi MA, Goyal M. Distal vessel occlusions: when to consider endovascular thrombectomy. Stroke 2018;49:1581–83 10.1161/STROKEAHA.118.021887 [DOI] [PubMed] [Google Scholar]
- 15. Lima FO, Furie KL, Silva GS, et al. Prognosis of untreated strokes due to anterior circulation proximal intracranial arterial occlusions detected by use of computed tomography angiography. JAMA Neurol 2014;71:151–57 10.1001/jamaneurol.2013.5007 [DOI] [PubMed] [Google Scholar]
- 16. Menon BK, Hill MD, Davalos A, et al. Efficacy of endovascular thrombectomy in patients with M2 segment middle cerebral artery occlusions: meta-analysis of data from the HERMES Collaboration. J Neurointerv Surg 2019;11:1065–69 10.1136/neurintsurg-2018-014678 [DOI] [PubMed] [Google Scholar]
- 17. Tian H, Parsons MW, Levi CR, et al. Influence of occlusion site and baseline ischemic core on outcome in patients with ischemic stroke. Neurology 2019;92:e2626–43 10.1212/WNL.0000000000007553 [DOI] [PubMed] [Google Scholar]
- 18. Sucharew H, Khoury J, Moomaw CJ, et al. Profiles of the National Institutes of Health Stroke Scale items as a predictor of patient outcome. Stroke 2013;44:2182–87 10.1161/STROKEAHA.113.001255 [DOI] [PMC free article] [PubMed] [Google Scholar]