Objective:
We examined associations of negative employment changes during the COVID-19 pandemic with mental health in a national sample of U.S. workers, and whether the associations differed by race.
Methods:
Data were from the Health, Ethnicity, and Pandemic Study, a cross-sectional survey. The effects of negative employment changes on psychological distress in 1510 workers were examined via linear regression, and stratified analyses were conducted across racial subgroups.
Results:
After adjustment for covariates, compared to workers with no change in employment, those who experienced permanent job loss had the highest psychological distress (β and 95% CI = 3.27 [1.89, 4.65]). Permanent job loss had the greatest effect on psychological distress in Blacks and Asians.
Conclusion:
Negative employment changes related to the pandemic may have deleterious impacts on workers’ mental health, with disproportionate effects on racial minorities.
Keywords: COVID-19, ethnic groups, mental health, occupational health, unemployment
Learning Objectives
Discuss previous findings on associations between employment loss and psychological distress.
Summarize the new findings on acute increases in negative employment changes during the COVID-19 pandemic and levels of psychological distress.
Discuss the findings on the modifying effects of race on the mental health effects of employment loss.
The COVID-19 pandemic has brought about immense changes to American society, with vast implications for workers. As the risk of infection and subsequent adverse health outcomes have prompted a prolonged shutdown of the United States economy, financial losses have mounted rapidly. Work and school closures have swept the nation, provoking a range of emotional and psychological reactions, including psychological distress and psychiatric conditions.1 Recent data have indicated that the prevalence of depressive symptoms during the COVID-19 pandemic has increased more than threefold compared to the time before, with the most remarkable effects seen in vulnerable populations such as low-income groups.2 The mental health effects of COVID-19 and its associated employment changes may lead to severe consequences throughout the world; for instance, globally, increasing unemployment rates are projected to increase rates of attempted and completed suicide.3,4
Furthermore, there are stark racial and ethnic disparities in COVID-19 hospitalization and mortality, with disadvantaged minority groups suffering a disproportionate burden of the health risks associated with COVID-19.5 While psychological distress has increased broadly throughout the U.S. population, elevated depressive symptomatology has been observed in socially vulnerable groups.6 These disparities are also present in the economic fallout of the pandemic and are evidenced by differential employment outcomes and occupational characteristics.7 For example, Hispanics and Blacks experienced notable increases in unemployment in 2020.8 At the same time, data from the Current Population Survey showed a significant increase in the white–nonwhite gap in employment and disadvantages in the likelihood of being laid off for nonwhite racial groups.9 While financial insecurity is a well-known risk factor for mental illness, preliminary evidence from 2020 indicates more severe psychological distress among low-income groups compared to high-income groups, and among Hispanics and Blacks compared to Whites.10
This study presents a unique opportunity to capture acute increases in employment loss and assess their associations with psychological distress. Although a substantial body of research has demonstrated associations of unemployment and job insecurity with depressive symptoms,11 in the past, severe employment loss usually occurred gradually. For example, unemployment rates from the global financial crisis in 2008 did not peak until 2010, 2 years after the precipitating events.12 In contrast, the COVID-19 pandemic resulted in acute and rapid employment loss, with unemployment rates spiking from around 4% to above 14% in March 2020.13 Therefore, the objective of our study is to investigate the associations of COVID-19 related negative employment changes with mental health in a nationally representative, population-based sample of U.S. workers, with a special focus on potential effect modification by race. To our knowledge, no such study has been conducted before. We hypothesize that negative employment changes such as pay cuts and temporary or permanent job loss are associated with increased psychological distress, with differentiated effect by race. We further hypothesize that these associations of negative employment changes with psychological distress will be stronger than seen in prior studies of negative employment changes, which reported an associated 20% to 30% increased risk of depressive symptoms.11
METHODS
Study Sample
Data from the 2020 Health, Ethnicity, and Pandemic Study were used. The study was conducted by the National Opinion Research Center (NORC) at the University of Chicago on behalf of the University of Nebraska Medical Center in October 2020, and the study sample was drawn from NORC's AmeriSpeak Panel, with additional Asian-American respondents from global online market research firm Dynata's nonprobability online opt-in panel. Participants were selected from the AmeriSpeak panel using 48 sampling strata, including age, race, education, and gender. A total of 2709 web-based surveys were conducted, representing a weighted sample from the AAPOR. NORC implemented weighting procedures to bring the distributions of the sample in line with the broader population distribution of the U.S., thus better approximating a nationally representative sample. Written informed consent was obtained from each participant.
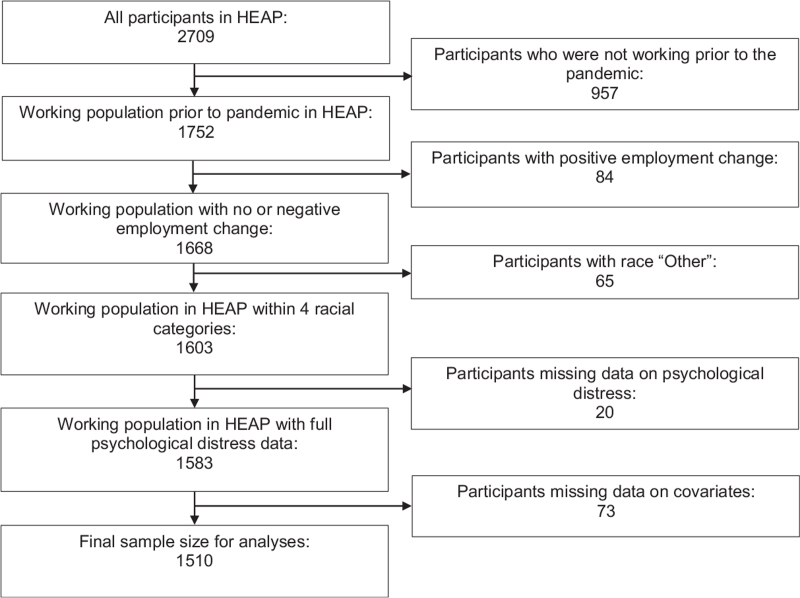
We used data from participants who were employed before the COVID-19 pandemic and had complete data on psychological distress and other relevant covariates. We excluded from our analysis participants who experienced a positive change in employment (e.g., pay raise, opened new business,…) and who had a race other than White, Hispanic, Black, or Asian due to small numbers. Furthermore, we also excluded subjects with missing values. The procedure followed for sample size selection is shown in Figure 1.
FIGURE 1.
Flow chart of study sample selection.
Measures
Employment change was assessed via a single question, “How has your employment status changed during the pandemic?” The response categories included no change (reference group), positive change, a pay cut, temporary unemployment, or permanent job loss (example items include “I lost my job or closed my business permanently” and “I experienced a pay cut or reduction of business income”).
Psychological distress in the past 30 days was assessed with the Kessler Psychological Distress Scale (K6), a validated and widely used self-report measure of moderate psychological distress.14,15 The K6 measures psychological distress with six questions (e.g., “How often did you feel nervous? “How often did you feel worthless?”) scored on a five-point Likert scale ranging from none of the time to all of the time. K6 ranged from 0 to 24, with a high value indicating a high level of psychological distress. As a rule of thumb in psychiatric research, serious mental illness is indicated when the value of K6 is above 12.14,15
Data regarding sociodemographic factors and health behaviors were also collected, including sex, age (18 to 29, 30 to 44, 45 to 59, and 60+); race (non-Hispanic White, single race; Hispanic or Latino; non-Hispanic Black, single race; non-Hispanic Asian, single race); marital status (married/living with a partner, never married, divorced/widowed/separated); educational attainment (high school or less, some college, university or more); annual household income (<$40,000, $40,000 to 99,999, >$99,999); current physical exercise (less than 30 min/day, 30 to 60 min/day, more than 60 min/day); smoking (no and yes); alcohol consumption (no drinking, moderate drinking—up to two drinks per day for men and one drink per day for women, heavy drinking—more than moderate drinking).16
Statistical Analysis
First, weighted descriptive statistics for the study participants were generated. Next, associations of negative employment changes with psychological distress were estimated using weighted multivariable linear regression, and the results were expressed as point estimates (β) with 95% confidence intervals (CIs). Two-sided hypothesis testing was conducted at the significance level α = 0.05. Multivariable models were calculated in three steps: Model I adjusted for age and sex; Model II included further adjustment for race, marital status, educational attainment, and household income; and Model III additionally adjusted for physical exercise, smoking, and alcohol consumption. Moreover, we tested interactions between race and negative employment changes to justify race-specific analyses, and stratified analyses by race were conducted accordingly. Sensitivity analyses were conducted with weighted logistic regression when using dichotomized K6 (serious mental illness, no vs yes) as an outcome, to test the robustness of associations. All analyses were performed using the SAS 9.4 software package, Survey Analysis Procedures.
RESULTS
The characteristics of the study sample are shown in Table 1. The sample of 1510 participants was predominantly middle-aged, with around 30% of participants falling into the age category of 30 to 44 and an age range of 18 to 60+. Males and females were roughly equally distributed, and most participants were married or living with a partner. The majority of participants had at least some college education. Most participants were non-smokers (82%) and exercised less than 30 min/day (52%). The sample was primarily White (60%), and included Hispanic (19%), Black (13%), and Asian (7%) racial groups. Whites and Asians had relatively higher household income, with 30% and nearly 40% earning above $99,999 a year, respectively. Most participants did not experience any change in employment status (57%). The prevalence of negative employment changes was 43%, including 19.13% with pay cuts, 10.53% temporarily unemployed, and 13.69% with permanent job loss. Hispanic and Black people experienced the highest rate of permanent job loss. The mean level of K6 was 6.90, and Hispanic and Asian people had the highest levels of K6, at 7.20 and 7.45, respectively. In addition, compared to participants with complete data, those with missing data were found to be younger, less educated, more of them Hispanic and Black people, and more distressed. Importantly, however, there were no systematic differences with regard to sex, marital status, household income, smoking, alcohol drinking, exercise, and the prevalence of negative employment changes (see online supplemental Table S1).
TABLE 1.
Characteristics of the Study Sample (N = 1510), the Health, Ethnicity, and Pandemic (HEAP) Study, 2020, Weighted
| Variables (%) | Non-Hispanic White, single race (unweighted N = 273, weighted N = 885, 61.24%) | Hispanic or Latino (unweighted N = 332, weighted N = 276, 19.09%) | Non-Hispanic Black, single race (unweighted N = 356, weighted N = 190, 13.15%) | Non-Hispanic Asian, single race (unweighted N = 549, weighted N = 94, 6.52%) | Total (N = 1510) |
| Sex | |||||
| Male | 47.05% | 53.79% | 48.95% | 53.36% | 49.06% |
| Female | 52.95% | 46.21% | 51.05% | 45.64% | 50.94% |
| Age (yrs) | |||||
| 18–29 | 20.36% | 25.16% | 24.90% | 19.01% | 21.79% |
| 30–44 | 31.20% | 34.72% | 37.43% | 43.66% | 33.50% |
| 45–59 | 30.34% | 27.62% | 24.96% | 27.73% | 28.94% |
| 60+ | 18.10% | 12.50% | 12.71% | 9.60% | 15.77% |
| Marital status | |||||
| Married/living with partner | 61.94% | 56.11% | 37.93% | 57.70% | 57.39% |
| Never married | 21.71% | 26.03% | 44.82% | 33.65% | 26.36% |
| Divorced/widowed/separated | 16.35% | 17.86% | 17.25% | 8.65% | 16.25% |
| Educational attainment | |||||
| University or more | 42.31% | 22.83% | 29.19% | 67.72% | 38.52% |
| Some college | 29.92% | 23.59% | 27.74% | 15.40% | 27.48% |
| High school or less | 27.77% | 53.58% | 43.07% | 16.88% | 34.00% |
| Household income (annual U.S. dollars) | |||||
| >99,999 | 31.19% | 13.90% | 11.92% | 38.41% | 25.82% |
| 40,000–99,999 | 48.06% | 41.83% | 41.00% | 39.40% | 45.38% |
| <40,000 | 20.75% | 44.27% | 47.08% | 22.19% | 28.80% |
| Exercise | |||||
| More than 60 min/day | 19.75% | 19.09% | 19.99% | 21.38% | 19.76% |
| 30–60 min/day | 31.33% | 21.09% | 21.67% | 30.29% | 28.04% |
| Less than 30 min/day | 48.92% | 59.82% | 58.34% | 48.33% | 52.20% |
| Smoking | |||||
| No | 81.77% | 84.32% | 74.02% | 87.71% | 81.62% |
| Yes | 18.23% | 15.68% | 25.98% | 12.29% | 18.38% |
| Alcohol | |||||
| No drinking | 43.12% | 46.58% | 43.78% | 60.77% | 45.02% |
| Moderate drinking | 42.27% | 46.58% | 46.51% | 35.39% | 43.20% |
| Heavy drinking | 14.61% | 6.84% | 9.71% | 3.84% | 11.78% |
| Negative employment change | |||||
| No change | 59.80% | 49.62% | 51.88% | 57.22% | 56.65% |
| Pay cut | 19.80% | 17.13% | 20.26% | 16.47% | 19.13% |
| Temporary unemployment | 9.37% | 12.48% | 10.45% | 15.83% | 10.53% |
| Permanent job loss | 11.03% | 20.77% | 17.41% | 10.48% | 13.69% |
| Psychological distress (mean) | 6.07 | 7.20 | 6.40 | 7.45 | 6.90 |
Table 2 displays the results of the linear regression analyses for the entire sample. The analyses demonstrated significant associations between negative employment change and psychological distress; compared to American workers with no job change, those who experienced permanent job loss had the highest psychological distress (fully-adjusted β and 95% CI = 3.27 [1.89, 4.65]), followed by those who had a pay cut (fully-adjusted β and 95% CI = 2.15 [1.02, 3.27]), and those who experienced temporary unemployment (fully-adjusted β and 95% CI = 1.77 [0.46, 3.09]).
TABLE 2.
Associations of Negative Employment Change with Psychological Distress (N = 1510), the Health, Ethnicity, and Pandemic (HEAP) Study, 2020
| Negative Employment Change | Unadjusted (β and 95% CI) | Model I (β and 95% CI) | Model II (β and 95% CI) | Model III (β and 95% CI) |
| No change (referent) | 0.00 | 0.00 | 0.00 | 0.00 |
| Pay cut | 2.47 (1.17, 3.78) | 2.27 (1.05, 3.49) | 2.20 (1.00, 3.40) | 2.15 (1.02, 3.27) |
| Temporary unemployment | 1.79 (0.23, 3.34) | 2.07 (0.70, 3.45) | 1.85 (0.46, 3.23) | 1.77 (0.46, 3.09) |
| Permanent job loss | 4.60 (2.97, 6.24) | 4.05 (2.49, 5.61) | 3.56 (2.05, 5.06) | 3.27 (1.89, 4.65) |
Multivariable linear regression. Model I: adjustment for age and sex; Model II: Model I + additional adjustment for race, marital status, educational attainment, and household income; Model III: Model II + additional adjustment for smoking, alcohol consumption, and physical exercise.
The interaction analysis indicated a significant interaction between race and negative employment change (P < 0.05). Stratified analyses revealed differentiated responses to negative employment change by race (see Table 3). Relative to Whites, Blacks, and Asians were more severely impacted by permanent job loss (fully-adjusted β and 95% CIs = 3.69 [1.84, 5.54] and 3.76 [1.96, 5.56], respectively). Whites and Asians also had significantly higher psychological distress associated with temporary unemployment (fully-adjusted β and 95% CIs = 2.25 [0.22, 4.29] and 2.65 [1.19, 4.11], respectively), while other races did not. Asians also experienced significantly greater psychological distress with pay cuts (fully-adjusted β and 95% CI = 2.28 [0.73, 3.82]), while other races did not. The findings of the sensitivity analyses showed a similar pattern of associations (see online supplemental Tables S2–S4).
TABLE 3.
Associations of Negative Employment Change with Psychological Distress by Race (N = 1510), the Health, Ethnicity, and Pandemic (HEAP) Study, 2020
| Race | Negative Employment Change | Unadjusted (β and 95% CI) | Model I (β and 95% CI) | Model II (β and 95% CI) | Model III (β and 95% CI) |
| Non-Hispanic White, single race | No change | 0.00 | 0.00 | 0.00 | 0.00 |
| Pay cut | 2.80 (0.90, 4.69) | 2.50 (0.74, 4.27) | 2.43 (0.66, 4.20) | 2.15 (−0.08, 4.37) | |
| Temporary unemployment | 1.70 (−0.87, 4.27) | 2.34 (0.18, 4.50) | 2.33 (0.22, 4.44) | 2.25 (0.22, 4.29) | |
| Permanent job loss | 4.24 (1.32, 7.15) | 3.75 (1.01, 6.49) | 3.55 (0.97, 6.14) | 3.10 (0.72, 5.49) | |
| Hispanic or Latino | No change | 0.00 | 0.00 | 0.00 | 0.00 |
| Pay cut | 2.31 (−0.26, 4.88) | 2.25 (−0.18, 4.68) | 2.07 (−0.28, 4.41) | 2.15 (−0.09, 4.37) | |
| Temporary unemployment | 1.06 (−1.39, 3.52) | 0.76 (−1.51, 3.03) | 0.45 (−1.82, 2.72) | 0.28 (−1.86, 2.42) | |
| Permanent job loss | 4.28 (2.25, 6.30) | 3.67 (1.68, 5.65) | 2.81 (0.97, 4.65) | 2.58 (0.83, 4.33) | |
| Non-Hispanic Black, single race | No change | 0.00 | 0.00 | 0.00 | 0.00 |
| Pay cut | 1.16 (−0.70, 3.02) | 0.87 (−0.85, 2.59) | 0.68 (−0.94, 2.30) | 0.25 (−1.17, 1.66) | |
| Temporary unemployment | 1.47 (−0.86, 3.80) | 1.68 (−0.48, 3.83) | 1.22 (−0.96, 3.39) | 0.68 (−1.45, 2.81) | |
| Permanent job loss | 5.26 (2.60, 7.92) | 4.85 (2.37, 7.32) | 4.33 (1.81, 6.85) | 3.69 (1.84, 5.54) | |
| Non-Hispanic Asian, single race | No change | 0.00 | 0.00 | 0.00 | 0.00 |
| Pay cut | 2.56 (0.96, 4.16) | 2.40 (0.80, 4.00) | 2.23 (0.74, 3.73) | 2.28 (0.73, 3.82) | |
| Temporary unemployment | 3.31 (1.63, 5.00) | 3.46 (1.84, 5.09) | 2.66 (1.06, 4.26) | 2.65 (1.19, 4.11) | |
| Permanent job loss | 5.12 (3.27, 6.98) | 4.35 (2.54, 6.17) | 3.77 (1.93, 5.62) | 3.76 (1.96, 5.56) |
Multivariable linear regression. Model I: adjustment for age and sex; Model II: Model I + additional adjustment for marital status, educational attainment, and household income; Model III: Model II + additional adjustment for smoking, alcohol consumption, and physical exercise.
DISCUSSION
In this study, we tested the hypothesis that negative employment change was associated with increased psychological distress during the COVD-19 pandemic in a nationally representative sample of working adults in the U.S. Furthermore, we examined the potential moderating effects of race and ethnicity in this relationship via stratified analyses. We observed significant associations of negative employment change with psychological distress, with the greatest increases in psychological distress observed in participants who experienced permanent job loss, followed by those who had a pay cut and then by those who experienced temporary unemployment. Stratified analyses by race indicated that Blacks and Asians experienced the greatest increases in psychological distress associated with permanent job loss. Whites and Asians had the highest increases in psychological distress associated with temporary unemployment, and only Asians had significantly increased psychological distress associated with pay cuts.
These results may be explained by the $600 per week supplement to unemployment benefits instated by the CARES Act. Whites and Asians had a relatively high income. Their unemployment benefits may have been less than their regular salary, resulting in the observed higher psychological distress in Whites and Asians with temporary unemployment. In contrast, Hispanics and Blacks had overall lower incomes, and the amount of unemployment benefit received may have been similar or even higher than original salary for some, leading them not to experience significant psychological distress with temporary unemployment.
The economic and employment-related effects of the COVID-19 pandemic have been a major focus of epidemiological and occupational health research efforts. Our findings are consistent with recent reports of adverse mental health impacts related to employment changes; a June 2020 study of 2301 U.S. workers with convenience sampling found higher symptoms of depression, anxiety, and stress, as well as lower positive mental health among those who lost their jobs,17 while a study of 4852 young U.S. adults in April 2020 reported poor mental health across multiple measures of depression and anxiety among those who experienced employment loss among any household member.18 Additionally, while psychological distress as measured by K6 was generally stable in recent years,19 K6 sharply increased in 2020 compared to 2018.20 These findings are also in line with longstanding research evidence demonstrating associations of employment loss with depressive symptoms, with lowered self-esteem and loss of personal control acting as potential driving factors.21,22 However, as expected, we found that the odds of mental illness were elevated sharply, by over 100%, due to acute COVID-19 related unemployment (see online supplemental Tables S2–S4), which is much stronger compared with evidence generated before the pandemic (i.e., by 20% to 30% only).11 Such adverse mental health effects of pandemic-related unemployment may have serious implications for the future of the American workforce, as the development of depression following job loss has been found to predict lower rates of reemployment.23 Effective mobilization and dispensation of mental health resources may be critical in the overall economic sheme of recovery from the COVID-19 pandemic.
Our results regarding racial differences in mental health and employment changes generally corroborate with recent findings. Data from the Current Population Survey illustrate a substantial white–nonwhite gap in employment, with the racial gap in employment between White and Black men increasing by 43.7% between February 2020 and May 2020, while the gap between White and Asian men increased more than twofold.9 Furthermore, the effects of COVID-19 related unemployment have been found to disproportionately affect Hispanics, Blacks, and women, especially in the short term.6,10,24 We would also like to highlight the marked increase in anti-Asian sentiment and violent crime since the advent of the pandemic; this intensified anti-Asian discrimination and stigma is an ongoing issue that has received extensive media coverage.25,26 Such experiences of anti-Asian xenophobia have been linked with worsened mental health outcomes and decreased use of mental health resources.27 While Asian Americans had the lowest mean level of K6 in 2018,20 they had the highest mean level of K6 in our sample, which was collected in October 2020, representing the greatest increase in K6 across all races during the COVID-19 pandemic. Notably, the observed increases in psychological distress associated with negative employment change only capture a portion of the pandemic's impacts. We must consider that adverse mental health outcomes may also be exacerbated by social determinants of health external to employment change.28 Furthermore, there are numerous dimensions for which pre-existing inequalities have widened sharply since the onset of the COVID-19 pandemic, including further increased household demands for families with young children.29,30
Economic policy directives such as unemployment relief and stimulus payments may also have a substantial role in shaping workers’ responses to employment changes.31 Data suggest that the CARES act stimulus payments made to approximately 160 million people as of May 31, 2020, resulted in “large and immediate” effects on spending, primarily in low-income households.32,33 Additionally, data from the National Bureau of Economic Research demonstrate that while high-wage workers displayed considerably reduced spending in mid-March 2020, these effects were transient. In contrast, low-wage workers experienced much larger employment-related losses that persisted for months.32 Furthermore, locational disparities in unemployment have been found to remain for many years due to limited migration, suggesting that low-income people living in areas with high job losses may be in greatest need of financial or employment assistance.34 Such economic implications are especially important for racial and ethnic minority groups, which have long been challenged by income inequality and limited social mobility.35,36 Indeed, income inequality has been found to increase in the wake of economic shocks such as the 2008 financial crisis, and COVID-19 may precipitate similar, even more severe changes, resulting in a downward spiral of workplace trends such as increased burnout, absenteeism, bullying, and turnover.37 Critically, psychological distress has been suggested to be a strong predictor of suicidal behaviors; in consideration of suicide prevention, it is valuable and vital to target the risk factors of suicide, such as psychological distress, before the psychiatric process advances and becomes potentially irreversible.38 Finally, adverse changes in mental health status may have implications for substance abuse and the ongoing opioid epidemic—recent evidence has demonstrated surges in opioid and other substance use during the pandemic.39–41 Such implications emphasize the need to develop and implement effective policy measures targeting mental health and financial insecurity.42
Strengths
A major strength of this study is that it uses data collected during the Fall 2020 surge surge of the COVID-19 pandemic; thus, survey responses are likely to reflect the acute impacts of the pandemic. The analyses conducted are based on timely data representing real-time employment changes and psychological distress during the pandemic. To the best of our knowledge, this is the first study in the U.S. with a nationally representative sample investigating associations between employment change and psychological stress. While we are unable to make causal inferences due to the cross-sectional nature of the data, our analyses took into account temporality consistent with our hypotheses in that the independent variable of negative employment change was assessed since the onset of the pandemic in March 2020 and the dependent variable of K6 was measured by self-reported symptoms experienced in the past 30 days.
Limitations
This study has several limitations. While the survey sample included members of racial groups other than White, Hispanic, Black, and Asian, the numbers of these individuals were too low to be included in our analysis, limiting the generalizability of our findings, especially for less well-represented minority groups or those with multiple racial identities. We were also unable to identify associations of employment status or psychological distress with individual income, as only household income was reported—in dual-earner households, the effect of reductions in an individual's income may be partially offset by other household members. Similarly, we were unable to account for personality traits relevant to mental health, which have been shown to influence psychological appraisals of the COVID-19 pandemic.43 Finally, we were not able to rule out potential selection bias given that the excluded subjects with missing data were younger, more socially disadvantaged, and psychologically distressed.
CONCLUSION
In a nationally representative sample of working adults in the U.S., negative employment change was significantly associated with psychological distress. The employment-related effects of the COVID-19 pandemic are extensive, pervasive, and continually evolving, with broad implications for working populations in the U.S. and worldwide. Adverse changes in employment status related to the pandemic, including reductions in income and temporary and permanent job loss, may severely affect workers’ mental health. Given the protracted state of the economic and employment-related effects of the pandemic, comprehensive government and employer policy interventions, as well as considerations of racial equity, may be necessary to prevent further deterioration of workers’ mental health.
Supplementary Material
Acknowledgments
We are grateful to Baojiang Chen, Lijun Chen, Keyonna King, Tzeyu Michaud, Athena Ramos, Drissa Toure, Bruce Barr, Eric Gober, and Mark Watts for their inputs in developing the survey instrument.
Footnotes
This work was supported by the Center for Reducing Health Disparities at University of Nebraska Medical Center, the Chinese Economists Society, and Calvin J. Li Memorial Foundation. In addition, TAM and JL were supported by a Start-Up Grant from the University of California, Los Angeles to JL as a new faculty member.
None of the funders was involved in the study design, the collection, the analysis, the interpretation of the data, and in the decision to submit the article for publication. Views and opinions expressed hereby are the sole responsibility of the authors and do not necessarily reflect those of the funding agencies. The JOEM editorial board and planners have no financial interest related to this research.
Li, Matthews, L. Chen, Z. Chen, Han, Shi, Y. Li, Wen, Zhang, H. Li, and Su have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
Data availability statement: Due to its proprietary nature and the protection of study participant privacy, supporting data cannot be made openly available for now. Further information about the data and conditions for access are available from Dr. Dejun Su (dejun.su@unmc.edu) at University of Nebraska Medical Center.
Ethical considerations and disclosures: The National Opinion Research Center (NORC) Institutional Review Board reviewed and approved this study (NORC IRB Protocol #20.10.43), and obtained written informed consent from each participant. The research protocol conformed to the principles embodied in the Declaration of Helsinki. This current analytic project was reviewed and approved for exemption by the University of California, Los Angeles (UCLA) Institutional Review Board (UCLA IRB Protocol #21-000363).
Author contribution: D.S., Z.C., and H.L. raised the funds. L.C., Z.C., X.H., H.L., Y.L., L.S., D.S., M.W., and D.Z. were involved in the study design and implementation. J.L., T.A.M., L.C., Z.C., H.L., D.S. actively participated in data acquisition. J.L. conceived the analytic concept. T.A.M. and J.L. contributed to the data analysis and manuscript drafting. All authors were involved in critically interpreting the results, revising the manuscript, and approved the final version.
Clinical significance: These findings demonstrate significant associations of negative employment changes with psychological distress during the COVID-19 pandemic. Racial differences in the associations suggest disproportionate mental health impacts on racial minorities. The adverse mental health impacts of employment changes during the COVID-19 pandemic are severe and require government and employer policy interventions.
Supplemental digital content is available for this article.
REFERENCES
- 1.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med 2020; 383:510–512. DOI 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 2.Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 2020; 3:e2019686.DOI 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry 2020; 7:389–390. DOI 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Devitt P. Can we expect an increased suicide rate due to Covid-19? Ir J Psychol Med 2020; 37:264–268. DOI 10.1017/ipm.2020.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA 2020; 323:2466–2467. DOI 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fitzpatrick KM, Harris C, Drawve G. Living in the midst of fear: depressive symptomatology among US adults during the COVID-19 pandemic. Depress Anxiety 2020; 37:957–964. DOI 10.1002/da.23080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Selden TM, Berdahl TA. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff (Millwood) 2020; 39:1624–1632. DOI 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- 8.Moen P, Pedtke JH, Flood S. Disparate disruptions: intersectional COVID-19 employment effects by age, gender, education, and race/ethnicity. Work Aging Retire 2020; 6:207–228. DOI 10.1093/workar/waaa013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dias FA. The racial gap in employment and layoffs during COVID-19 in the United States: a visualization. Socius 2021; 7:2378023120988397.DOI 10.1177/2378023120988397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Purtle J. COVID-19 and mental health equity in the United States. Soc Psychiatry Psychiatr Epidemiol 2020; 55:969–971. DOI 10.1007/s00127-020-01896-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim TJ, von dem Knesebeck O. Perceived job insecurity, unemployment and depressive symptoms: a systematic review and meta-analysis of prospective observational studies. Int Arch Occup Environ Health 2016; 89:561–573. DOI 10.1007/s00420-015-1107-1. [DOI] [PubMed] [Google Scholar]
- 12. Long H, Dam AV. U.S. Unemployment Rate Soars to 14.7 Percent, The Worst Since the Depression Era. Washington Post. https://www.washingtonpost.com/business/2020/05/08/april-2020-jobs-report/. Published May 8, 2020. Accessed April 8, 2021. [Google Scholar]
- 13. The Employment Situation — March 2021. U.S. Department of Labor. Bureau of Labor Statistics. Accessed April 8, 2021. https://www.bls.gov/news.release/pdf/empsit.pdf. [Google Scholar]
- 14.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry 2003; 60:184–189. DOI 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 15.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32:959–976. DOI 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Department of Agriculture and U.S. Department of Health and Human Services, U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025. 2020; Available at DietaryGuidelines.gov. [Google Scholar]
- 17.McDowell CP, Herring MP, Lansing J, Brower CS, Meyer JD. Associations between employment changes and mental health: US data from during the COVID-19 pandemic. Front Psychol 2021; 12:631510.DOI 10.3389/fpsyg.2021.631510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ganson KT, Tsai AC, Weiser SD, Benabou SE, Nagata JM. Job insecurity and symptoms of anxiety and depression among U.S. young adults during COVID-19. J Adolesc Health 2021; 68:53–56. DOI 10.1016/j.jadohealth.2020.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Tomitaka S, Kawasaki Y, Ide K, Akutagawa M, Ono Y, Furukawa TA. Distribution of psychological distress is stable in recent decades and follows an exponential pattern in the US population. Sci Rep 2019; 9:11982.DOI 10.1038/s41598-019-47322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Twenge JM, Joiner TE. Mental distress among U.S. adults during the COVID-19 pandemic. J Clin Psychol 2020; 76:2170–2182. DOI 10.1002/jclp.23064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Price RH, Choi JN, Vinokur AD. Links in the chain of adversity following job loss: how financial strain and loss of personal control lead to depression, impaired functioning, and poor health. J Occup Health Psychol 2002; 7:302–312. DOI 10.1037//1076-8998.7.4.302. [DOI] [PubMed] [Google Scholar]
- 22.Sinclair RR, Allen T, Barber L, et al. Occupational health science in the time of COVID-19: now more than ever. Occup Health Sci 2020; 4:1–22. DOI 10.1007/s41542-020-00064-3. Published online June 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stolove CA, Galatzer-Levy IR, Bonanno GA. Emergence of depression following job loss prospectively predicts lower rates of reemployment. Psychiatry Res 2017; 253:79–83. DOI 10.1016/j.psychres.2017.03.036. [DOI] [PubMed] [Google Scholar]
- 24.National Bureau of Economic Research, Bianchi F, Bianchi G, Song D. The Long-Term Impact of the COVID-19 Unemployment Shock on Life Expectancy and Mortality Rates. 2021; DOI 10.3386/w28304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tessler H, Choi M, Kao G. The anxiety of being Asian American: hate crimes and negative biases during the COVID-19 pandemic. Am J Crim Justice 2020; 45:636–646. DOI 10.1007/s12103-020-09541-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Le TK, Cha L, Han H-R, Tseng W. Anti-Asian xenophobia and Asian American COVID-19 disparities. Am J Public Health 2020; 110:1371–1373. DOI 10.2105/AJPH.2020.305846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Misra S, Le PD, Goldmann E, Yang LH. Psychological impact of anti-Asian stigma due to the COVID-19 pandemic: a call for research, practice, and policy responses. Psychol Trauma Theory Res Pract Policy 2020; 12:461–464. DOI 10.1037/tra0000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis 2021; 72:703–706. DOI 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myers KR, Tham WY, Yin Y, et al. Unequal effects of the COVID-19 pandemic on scientists. Nat Hum Behav 2020; 4:880–883. DOI 10.1038/s41562-020-0921-y. [DOI] [PubMed] [Google Scholar]
- 30.Kniffin KM, Narayanan J, Vugt M. COVID-19 is a moderating variable with its own moderating factors. Ind Organ Psychol 2021; 14:149–151. DOI 10.1017/iop.2021.38. [Google Scholar]
- 31.National Bureau of Economic Research, Casado MG, Glennon B, Lane J, McQuown D, Rich D, Weinberg BA. The Effect of Fiscal Stimulus: Evidence from COVID-19. 2020; DOI 10.3386/w27576. [Google Scholar]
- 32.National Bureau of Economic Research, Chetty R, Friedman J, Hendren N, Stepner M, Team TOI. The Economic Impacts of COVID-19: Evidence From a New Public Database Built Using Private Sector Data. 2020; w27431. DOI 10.3386/w27431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Bureau of Economic Research, Baker SR, Farrokhnia RA, Meyer S, Pagel M, Yannelis C. Income, Liquidity, and the Consumption Response to the 2020 Economic Stimulus Payments. 2020; DOI 10.3386/w27097. [Google Scholar]
- 34.Yagan D. Employment hysteresis from the great recession. J Polit Econ 2019; 127:2505–2558. [Google Scholar]
- 35.Galaskiewicz J, Anderson KF, Thompson-Dyck K. Minority-White income inequality across metropolitan areas: the role of racial/ethnic residential segregation and transportation networks. J Urban Aff 2021; 43:16–39. DOI 10.1080/07352166.2019.1660581. [Google Scholar]
- 36.Hoover GA, Yaya ME. Racial/ethnic differences in income inequality across US regions. Rev Black Polit Econ 2010; 37:79–114. DOI 10.1007/s12114-010-9057-z. [Google Scholar]
- 37.Kniffin KM, Narayanan J, Anseel F, et al. COVID-19 and the workplace: implications, issues, and insights for future research and action. Am Psychol 2021; 76:63–77. DOI 10.1037/amp0000716. [DOI] [PubMed] [Google Scholar]
- 38.Cheref S, Benoit JS, Walker RL. Refining psychological, substance use, and sociodemographic predictors of suicide ideation and attempts in a national multiethnic sample of adults. J Nerv Ment Dis 2019; 207:675–682. DOI 10.1097/NMD.0000000000001026. [DOI] [PubMed] [Google Scholar]
- 39.Volinn E, Loeser JD. Upsurges in the joblessness and opioid epidemics in the U.S. after the COVID-19 epidemic: the plight of the jobless patient in the clinic. Pain 2021; 162:1608–1611. DOI 10.1097/j.pain.0000000000002253. Published online February 26. [DOI] [PubMed] [Google Scholar]
- 40.Chiappini S, Guirguis A, John A, Corkery JM, Schifano F. COVID-19: the hidden impact on mental health and drug addiction. Front Psychiatry 2020; 11:767.DOI 10.3389/fpsyt.2020.00767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry 2021; 78:372–379. DOI 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goldman ML, Druss BG, Horvitz-Lennon M, et al. Mental health policy in the era of COVID-19. Psychiatr Serv 2020; 71:1158–1162. DOI 10.1176/appi.ps.202000219. [DOI] [PubMed] [Google Scholar]
- 43.Niemi L, Kniffin KM, Doris JM. It's not the flu: popular perceptions of the impact of COVID-19 in the U.S. Front Psychol 2021; 12:668518.DOI 10.3389/fpsyg.2021.668518. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.