Abstract
Background
Among those with injection drug use-associated infective endocarditis (IDU-IE), against medical advice (AMA) discharge is common and linked to adverse outcomes. Understanding trends, risk factors, and timing is needed to reduce IDU-IE AMA discharges.
Methods
We identified individuals ages 18–64 with International Classification of Diseases, 9thRevision, diagnosis codes for infective endocarditis (IE) in the National Inpatient Sample, a representative sample of United States hospitalizations from January 2010 to September 2015. We plotted unadjusted quarter-year trends for AMA discharges and used multivariable logistic regression to identify factors associated with AMA discharge among IE hospitalizations, comparing IDU-IE with non-IDU-IE.
Results
We identified 7259 IDU-IE and 23 633 non-IDU-IE hospitalizations. Of these hospitalizations, 14.2% of IDU-IE and 1.9% of non-IDU-IE resulted in AMA discharges. More than 30% of AMA discharges for both groups occurred before hospital day 3. In adjusted models, IDU status (adjusted odds ratio [AOR], 3.92; 95% confidence interval [CI], 3.43–4.48)] was associated with increased odds of AMA discharge. Among IDU-IE, women (AOR, 1.21; 95% CI, 1.04–1.41) and Hispanics (AOR, 1.32; 95% CI, 1.03–1.69) had increased odds of AMA discharge, which differed from non-IDU-IE. Over nearly 6 years, odds of AMA discharge increased 12% per year for IDU-IE (AOR, 1.12; 95% CI, 1.07–1.18) and 6% per year for non-IDU-IE (AOR, 1.06; 95% CI. 1.00–1.13).
Conclusions
AMA discharges have risen among individuals with IDU-IE and non-IDE-IE. Among those who inject drugs, AMA discharges were more common and increases sharper. Efforts that address the rising fraction, disparities, and timing of IDU-IE AMA discharges are needed.
Keywords: infective endocarditis, injection drug use, discharge against medical advice
In this national cohort, against medical advice (AMA) discharges grew, affecting one-fifth of injection drug use-associated infective endocarditis (IDU-IE) hospitalizations. Odds of AMA discharge were 4 times higher for IDU-IE versus non-IDU-IE; one-third occurred before hospital day 3.
Injection drug use-associated infective endocarditis (IDU-IE) is an expensive and life-threatening heart valve infection. IDU-IE hospitalizations doubled between 2000 and 2014 and deaths tripled during a similar period with more dramatic increases in some regions [1–3]. Infective endocarditis (IE) can be successfully treated with an extended course of intravenous antibiotic therapy, but sometimes valve replacement is needed. Antibiotic treatment and surgery are frequently interrupted by discharges against medical advice (AMA) among those with IDU-IE [3–5]. AMA discharges are associated with increased rehospitalization, mortality, and resource utilization compared with planned discharges [6–9].
Qualitative studies have demonstrated that individuals with opioid use disorder (OUD) frequently experience AMA discharge because of untreated or undertreated opioid withdrawal symptoms, cravings, pain, and stigma [10, 11]. Additionally, many patients with IDU-IE lack access to home- or facility-based postacute medical care, and thus remain hospitalized for the duration of intravenous antibiotic treatment (often 6 weeks) [12]. During these hospitalizations, conflict with the hospital care team over ongoing substance use, psychiatric comorbidities, prior trauma, loss of autonomy, poor communication, and restricted movement may increase the risk of AMA discharge [8, 10].
AMA discharges for mental health and substance-related diagnoses decreased 2.3% annually across all US hospitalizations between 2002 and 2011 [13]. However, AMA discharge remained more common among individuals who use substances than those who do not and more frequent when multiple substances were used [9, 13–15]. Several studies have demonstrated high rates of AMA discharge among IDU-IE and in-hospital injection drug use increased risk [4, 5, 8]. Trends, additional risk factors, and timing for these discharges are not known despite their importance for clinical care and program development. Moreover, it is not known how these trends and factors compare with individuals with non-IDU-IE. In this study, we test the following hypotheses: AMA discharge will be more common among IDU-IE than non-IDU-IE hospitalizations; IDU-IE AMA discharges will have increased over time and non-IDU-IE AMA discharges will remain constant; and IDU-IE AMA discharges will be more concentrated in the first 3 days of admission than non-IDU-IE (a window during which opioid withdrawal can be severe and, if not treated, lead to AMA discharge).
METHODS
Study Design and Data Source
We used data from the National Inpatient Sample (NIS) between January 1, 2010, and August 31, 2015, to identify all IE discharges. The NIS is a large, publicly available database comprising a sample of all inpatient hospitalizations in the United States. By using sample weights, NIS can estimate outcomes for all US hospitalizations, excluding those at Veterans Administration facilities. We assessed for changes in AMA discharge rate among IDU-IE and non-IDU-IE hospitalizations; used logistic regression to identify demographic and clinical factors associated with AMA discharge among all IE, non-IDU-IE, and IDU-IE; and described the proportion of AMA discharges by hospital length of stay (LOS). The Boston University Medical Campus institutional review board determined this study did not constitute human subjects research.
Cohort Selection
Hospitalizations among individuals aged 18 to 64 with an International Classification of Diseases, 9th Revision (ICD-9), diagnosis of native valve IE (421.0, 421.1 421.9, 424.90, 424.91, 424.99, 112.81) were included in the cohort, which was previously described [16]. We excluded quarter 4 of 2015 because of increases in OUD coding after the transition from ICD-9 to ICD-10 [16, 17]. We selected these ages to limit misclassification of older individuals with structural heart disease or younger individuals with congenital heart disease, consistent with prior IDU-IE studies [16, 18, 19].
We stratified the cohort by IDU status using ICD-9 diagnosis codes corresponding to drug use (including opioids and stimulants) or hepatitis C based on a previously validated algorithm for identifying IDU as the etiology for IE [20]. The algorithm, which used ICD-10 codes, had a 93% sensitivity, 61% specificity, and resulting positive predictive value of 83% when compared with chart review. We mapped ICD-10 codes to ICD-9 codes using the 2015 general equivalence mapping from the Centers for Medicaid and Medicare Services as previously described (Supplementary Table 1) [16, 21]. We excluded hospitalizations with missing data in the main models.
Variables of Interest
The primary outcome was AMA discharge following hospitalization for IE. Some researchers have referred to AMA discharges as “patient-directed discharges” to highlight the importance of shared discharge decision making [8]. We used the term AMA because we were unable to decipher the circumstances of discharges assigned AMA in our data. We included the following descriptive clinical covariates from NIS: age, sex, race/ethnicity (where Hispanic is exclusive of race), insurance status, income quartile of patient’s ZIP code, elective admission (eg, planned cardiac surgery), cardiac valve surgery defined by ICD-9 procedure codes previously detailed [16], LOS, and death. We then examined time to AMA discharge and LOS for live/non-AMA discharge. We calculated a modified Elixhauser score, a composite comorbidity index associated with inpatient mortality risk commonly used in administrative data to adjust for comorbidities [22]. The Elixhauser score is calculated by identifying diagnostic codes in 30 clinical categories from selected billing codes. We removed depression, psychosis, alcohol use, and drug use from the summed Elixhauser score and evaluated these factors individually because they have been previously associated with AMA discharge and IDU status [13, 15]. For drug use comorbidities, we excluded the codes used in our definition of IDU and created separate variables for cannabis (ICD-9 305.2) and sedative use (ICD-9 304.1 and 305.4) [22]. We grouped Elixhauser scores into the following categories: 0, 1–2, 3–4, and ≥5. We also included several hospital-level characteristics available in NIS (hospital region, hospital size, and teaching status of hospital). Hospitals size was classified as small, medium, or large in the NIS based on the number of acute care beds with thresholds specific to region, urban/rural classification, and teaching status [23].
Statistical Analysis
In bivariate analyses comparing IDU-IE and non-IDU-IE, we used t tests and χ 2 tests for continuous and categorical variables, respectively. We plotted quarterly unadjusted proportion of AMA discharges among IDU-IE and non-IDU-IE between quarter 1 2010 and quarter 3 2015. We used multivariable logistic regression models to test for factors associated with AMA discharge among IDU-IE, non-IDU-IE, and all IE in separate models. Other than LOS, which is associated with the AMA outcome, we included all covariates previously mentioned and a term for calendar quarter to adjust for temporal trends. Based on these findings, we plotted unadjusted proportion of AMA discharges among IDU-IE and non-IDU-IE for males and females separately. Additionally, we plotted the proportion of all AMA and non-AMA, live discharges by hospital day in which hospitalizations with missing death data were excluded. To improve visualization and address extreme outliers, we grouped hospitalizations with a LOS above the 99th percentile as having occurred at the 99th percentile. To account for NIS’s representative sampling, we used survey procedures in SAS, version 9.4, (SAS Institute Inc., Cary, NC, USA).
RESULTS
We identified 40 386 hospitalizations for IE. We excluded hospitalizations resulting in transfer to another acute care hospital to prevent double counting (4630). We also excluded those hospitalizations with missing data: discharge date (1322), race (2263), payor (109), ZIP code income quartile (832), elective status (75), teaching classification of hospital (223), and disposition (40). One hospitalization with missing death data was retained in the cohort because death was not in our main models. The resulting study sample was 30 892 hospitalizations corresponding to an estimated 153 616 national hospitalizations from January 1, 2010, to August 31, 2015. Non-IDU-IE accounted for 76.5% (117 482) and IDU-IE for 23.5% (36 133) of all IE hospitalizations. Compared with non-IDU hospitalizations, IDU hospitalizations were more common among young adults, whites, females, those uninsured or insured by Medicaid, those who live in the lowest ZIP code income quartile, as well as those who were admitted nonelectively. Additionally, IDU-IE hospitalizations had lower modified Elixhauser scores, but higher rates of alcohol, cannabis, sedative use, psychoses, and depression. Those with IDU-IE were less likely to die in the hospital or receive cardiac surgery and were hospitalized 2.6 days longer compared with non-IDU-IE (Table 1).
Table 1.
Characteristics of Infective Endocarditis Hospitalizations in the United States among Individuals Ages 18–64 Between 1 January 2010, and 31 August 2015
| Full Cohort | IDU | Non-IDU | P Valuea | |||||
|---|---|---|---|---|---|---|---|---|
| n = 30 892 | n = 7259 | n = 23 633 | ||||||
| Weighted n = 153 616 | SEb | Weighted n = 36 133 | SE | Weighted n = 117 482 | SE | |||
| Age | <.0001 | |||||||
| 18–24 | 5.3%c | 0.2 | 10.8% | 0.4 | 3.6% | 0.1 | ||
| 25–34 | 14.9% | 0.2 | 31.8% | 0.6 | 9.7% | 0.2 | ||
| 35–44 | 15.8% | 0.2 | 21.1% | 0.5 | 14.2% | 0.2 | ||
| 45–55 | 27.2% | 0.3 | 22.6% | 0.6 | 28.6% | 0.3 | ||
| 56–65 | 36.8% | 0.3 | 13.8% | 0.5 | 43.8% | 0.4 | ||
| Female | 41.6% | 0.3 | 43.3% | 0.6 | 41.1% | 0.4 | .0017 | |
| Race/ethnicity | <.0001 | |||||||
| White | 64.2% | 0.5 | 72.3% | 0.8 | 61.8% | 0.6 | ||
| Black | 21.0% | 0.4 | 14.9% | 0.6 | 22.9% | 0.5 | ||
| Hispanic | 9.5% | 0.3 | 9.1% | 0.5 | 9.6% | 0.3 | ||
| Asian | 1.8% | 0.1 | 0.6% | 0.1 | 2.1% | 0.1 | ||
| Native American | 0.7% | 0.1 | 0.8% | 0.1 | 0.7% | 0.1 | ||
| Other | 2.8% | 0.2 | 2.3% | 0.2 | 2.9% | 0.2 | ||
| Payor | <.0001 | |||||||
| Medicare | 27.5% | 0.3 | 14.4% | 0.5 | 31.6% | 0.4 | ||
| Medicaid | 27.4% | 0.4 | 45.9% | 0.7 | 21.8% | 0.4 | ||
| Commercial | 29.9% | 0.4 | 13.1% | 0.4 | 35.1% | 0.4 | ||
| Self | 10.3% | 0.3 | 19.9% | 0.6 | 7.3% | 0.2 | ||
| No charge | 1.2% | 0.1 | 2.4% | 0.2 | 0.8% | 0.1 | ||
| Other | 3.7% | 0.2 | 4.3% | 0.3 | 3.5% | 0.2 | ||
| ZIP code income quartile d | <.0001 | |||||||
| Quartile 1 | 37.6% | 0.5 | 42.2% | 0.8 | 36.2% | 0.5 | ||
| Quartile 2 | 25.2% | 0.3 | 25.6% | 0.6 | 25.0% | 0.4 | ||
| Quartile 3 | 20.8% | 0.3 | 19.1% | 0.5 | 21.4% | 0.4 | ||
| Quartile 4 | 16.4% | 0.4 | 13.1% | 0.5 | 17.5% | 0.5 | ||
| Hospital region | <.0001 | |||||||
| Northeast | 19.9% | 0.6 | 20.0% | 0.8 | 19.9% | 0.7 | ||
| Midwest | 17.3% | 0.6 | 14.2% | 0.7 | 18.3% | 0.6 | ||
| South | 42.8% | 0.7 | 42.3% | 1.0 | 43.0% | 0.7 | ||
| West | 19.9% | 0.5 | 23.5% | 0.8 | 18.8% | 0.5 | ||
| Hospital location/teaching status | .0108 | |||||||
| Rural | 7.0% | 0.3 | 6.1% | 0.4 | 7.3% | 0.3 | ||
| Urban, nonteaching | 29.1% | 0.6 | 28.4% | 0.8 | 29.3% | 0.6 | ||
| Urban, teaching | 63.9% | 0.6 | 65.5% | 0.9 | 63.4% | 0.7 | ||
| Hospital bed size | .6676 | |||||||
| Small | 11.0% | 0.2 | 11.1% | 0.5 | 10.9% | 0.3 | ||
| Medium | 24.0% | 0.5 | 24.4% | 0.8 | 23.9% | 0.5 | ||
| Large | 65.0% | 0.6 | 64.5% | 0.9 | 65.2% | 0.6 | ||
| Modified Elixhauser score e | <.0001 | |||||||
| 0 | 2.6% | 0.1 | 4.0% | 0.2 | 2.1% | 0.1 | ||
| 1–2 | 22.3% | 0.3 | 29.0% | 0.6 | 20.2% | 0.4 | ||
| 3–4 | 34.7% | 0.3 | 35.2% | 0.6 | 34.5% | 0.3 | ||
| ≥5 | 40.5% | 0.4 | 31.8% | 0.6 | 43.1% | 0.5 | ||
| Alcohol | 7.5% | 0.2 | 12.4% | 0.4 | 6.0% | 0.2 | <.0001 | |
| Cannabis | 2.3% | 0.1 | 6.1% | 0.3 | 1.1% | 0.1 | <.0001 | |
| Sedatives | 0.5% | 0.04 | 1.8% | 0.2 | 0.1% | 0.01 | <.0001 | |
| Psychoses | 7.3% | 0.2 | 12.6% | 0.4 | 5.7% | 0.2 | <.0001 | |
| Depression | 11.7% | 0.2 | 14.5% | 0.4 | 10.8% | 0.2 | <.0001 | |
| Elective admission | 11.8% | 0.3 | 7.3% | 0.4 | 13.2% | 0.3 | <.0001 | |
| CT surgery | 12.6% | 0.3 | 11.8% | 0.4 | 12.9% | 0.3 | .0244 | |
| LOS, d | 14.0 | 0.1 | 16.0 | 0.2 | 13.4 | 0.2 | <.0001 | |
| Died during hospitalization f | 9.4% | 0.2 | 7.9% | 0.3 | 9.9% | 0.2 | <.0001 |
Abbreviations: AMA, against medical advice; CT, cardiothoracic; IDU, injection drug use; SE, standard error.
aIDU vs non-IDU; all variables compared using chi-squared analysis except modified Elixhauser, which was compared using a t test.
bStandard error is calculated from weighted sample.
cPercentages reported are estimates for all US hospitalizations based on sample weights.
dOrdered from lowest income quartile to highest income quartile.
eElixhauser score contains 30 components weighted equally and is used to adjust for inpatient comorbidities. We included 26 of these components in the modified Elixhauser. We separated psychoses, depression, and alcohol and drug use because these conditions have been previously associated with AMA discharge and IDU. We excluded measures of drug use overlapping with our IDU measure, and included measures for cannabis and sedative use separately.
fDeath data were missing for 1 individual. Percentage is based on a denominator of 30 891 hospitalizations.
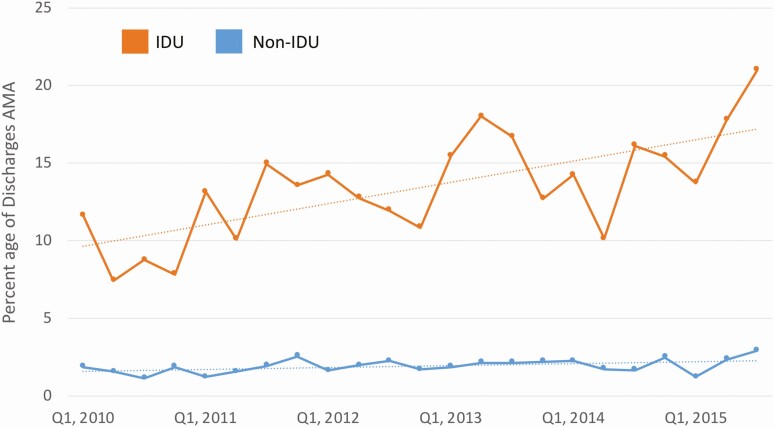
AMA Discharges
During the study period, the frequency of AMA discharges per quarter for IDU-IE increased from 11.7% to 21.0% of hospitalizations, whereas non-IDU-IE AMA discharges increased from 1.9% to 2.9% (Figure 1). In adjusted models, IDU-IE hospitalizations were associated with increased risk of AMA discharge (adjusted odds ratio [AOR], 3.92; 95% confidence interval [95% CI], 3.43–4.48). The odds of AMA discharge increased significantly for IDU-IE (AOR, 1.12; 95% CI, 1.07–1.18) each year and nearly reached significance for non-IDU-IE (AOR, 1.06; 95% CI, 1.00–1.13) (Table 2).
Figure 1.
Proportion of injection drug use and non-injection drug use-associated infective endocarditis discharges resulting in against medical advice discharge by quarter, 1 January 2010, to 31 August 2015. Abbreviations: AMA, against medical advice; IDU, injection drug use.
Table 2.
Multivariable Logistic Regression Models with Discharge Against Medical Advice as Outcome for All Infective Endocarditis and Stratified by Injection Drug Use
| Full Cohort n = 30 892 Weighted n = 153 616 | IDU n = 7259 Weighted n = 36 133 | Non-IDU n = 23 633 Weighted n = 117 482 | ||
|---|---|---|---|---|
| Adjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted OR (95% CI) | ||
| IDU | 3.92 (3.43–4.48) | N/A | N/A | |
| Time | 1.10 (1.06–1.15) | 1.12 (1.07–1.18) | 1.06 (1.00–1.13) | |
| Age, y | ||||
| 18–24 | 3.34 (2.60–4.31) | 3.02 (2.10–4.34) | 2.94 (1.85–4.67) | |
| 25–34 | 3.33 (2.71–4.10) | 2.87 (2.08–3.95) | 4.01 (2.97–5.40) | |
| 35–44 | 2.54 (2.05–3.14) | 2.31 (1.66–3.21) | 2.65 (1.98–3.54) | |
| 45–55 | 1.62 (1.32–1.99) | 1.61 (1.16–1.41) | 1.56 (1.18–2.06) | |
| 56–65 | Ref | Ref | Ref | |
| Female | 1.00 (.89–1.13) | 1.21 (1.04–1.41) | 0.71 (.58–.87) | |
| Race/ethnicity a | ||||
| White | Ref | Ref | Ref | |
| Black | 1.16 (.98–1.38) | 1.13 (.89–1.45) | 1.17 (.92–1.50) | |
| Hispanic | 1.07 (.88–1.30) | 1.32 (1.03–1.69) | 0.76 (.53–1.09) | |
| Asian | 0.39 (.17–.86) | 0.59 (.18–1.94) | 0.27 (.09–.86) | |
| Native American | 0.65 (.30–1.44) | 1.01 (.42–2.46) | <0.001 (<.001–<.001) | |
| Other | 1.09 (.72–1.66) | 0.99 (.62–1.59) | 1.21 (.69–2.14) | |
| Payor | ||||
| Medicare | 0.77 (.65–.92) | 0.75 (.58–.96) | 0.75 (.58–.98) | |
| Medicaid | Ref | Ref | Ref | |
| Commercial | 0.44 (.36–.54) | 0.57 (.44–.74) | 0.35 (.26–.47) | |
| Self | 1.39 (1.18–1.65) | 1.37 (1.13–1.66) | 1.44 (1.06–1.95) | |
| No charge | 1.31 (.90–1.92) | 1.24 (.79–1.94) | 1.61 (.81–3.19) | |
| Other | 0.73 (.52–1.02) | 0.70 (.46–1.05) | 0.79 (.47–1.33) | |
| ZIP code income quartile | ||||
| Quartile 1 | 1.57 (1.28–1.92) | 1.56 (1.21–1.99) | 1.57 (1.11–2.42) | |
| Quartile 2 | 1.25 (1.01–1.55) | 1.24 (.96–1.60) | 1.25 (.87–1.81) | |
| Quartile 3 | 1.22 (.98–1.51) | 1.16 (.89–1.52) | 1.30 (.91–1.87) | |
| Quartile 4 | Ref | Ref | Ref | |
| Hospital region | ||||
| Northeast | Ref | Ref | Ref | |
| Midwest | 0.74 (.61–.91) | 0.81 (.63–1.04) | 0.62 (.44–.87) | |
| South | 0.63 (.53–.75) | 0.60 (.48–.75) | 0.69 (.53–.89) | |
| West | 0.93 (.77–1.12) | 0.84 (.67–1.06) | 1.13 (.83–1.54) | |
| Hospital location/teaching status | ||||
| Rural | Ref | Ref | Ref | |
| Urban, nonteaching | 1.20 (.93–1.56) | 1.12 (.82–1.53) | 1.38 (.91–2.09) | |
| Urban, teaching | 0.95 (.74–1.22) | 0.91 (.67–1.24) | 1.03 (.69–1.55) | |
| Hospital bed size | ||||
| Small | Ref | Ref | Ref | |
| Medium | 0.84 (.70–1.02) | 0.96 (.76–1.22) | 0.68 (.50–.92) | |
| Large | 0.70 (.59– .83) | 0.76 (.61–.94) | 0.61 (.47–.80) | |
| Modified Elixhauser score b | ||||
| 0 | Ref | Ref | Ref | |
| 1–2 | 0.61 (.47–.78) | 0.71 (.53–.95) | 0.40 (.26–.60) | |
| 3–4 | 0.39 (.30–.51) | 0.41 (.30–.55) | 0.33 (.22–.51) | |
| ≥5 | 0.33 (.25–.42) | 0.31 (.23–.44) | 0.30 (.20–.46) | |
| Alcohol | 1.11 (.91–1.35) | 0.92 (.73–1.16) | 1.61 (1.16–2.24) | |
| Cannabis | 1.37 (1.07–1.74) | 1.26 (.96–1.65) | 2.0 (1.20–3.33) | |
| Sedative | 0.94 (.58–1.52) | 1.05 (.64–1.71) | 1.27 (.13–12.37) | |
| Psychoses | 1.28 (1.07–1.54) | 0.96 (.59–1.56) | 1.78 (1.28–2.47) | |
| Depression | 1.03 (.87–1.22) | 0.97 (.79–1.18) | 1.14 (.85–1.54) | |
| Elective | 0.59 (.46–.76) | 0.58 (.42–.80) | 0.63 (.43–.91) | |
| CT surgery | 0.20 (.14–.27) | 0.23 (.16–.33) | 0.14 (.08–.28) |
Abbreviations: AMA, against medical advice; CI, confidence interval; CT, cardiothoracic; IDU, injection drug use; N/A, not available; OR, odds ratio.
aIn the National Inpatient Sample, hospitalized individuals are categorized by Hispanic ethnic exclusive of other racial categories.
bElixhauser score contains 30 components weighted equally and is used to adjust for inpatient comorbidities. We included 26 of these components in the modified Elixhauser. We separated drug use, psychoses, depression, and alcohol use because these conditions have been previously associated with AMA discharge and IDU status.
Among both non-IDU and IDU-IE, younger age and residing in the lowest ZIP code income quartiles were associated with increased odds of AMA discharge. Having commercial or Medicare insurance, higher Elixhauser scores, being hospitalized in the South, being admitted electively, receiving cardiothoracic surgery, and receiving care in a large hospital were all significantly associated with decreased odds of AMA discharge for both groups. There were no associations with AMA discharge and hospital teaching status or differences between white and Black individuals with IDU-IE or non-IDU-IE. However, compared with white individuals, Hispanic individuals with IDU-IE were more likely (AOR, 1.32; 95% CI, 1.03–1.69) and Asians with non-IDU-IE were less likely to have an AMA discharge (AOR, 0.27; 95% CI, .09–.86). Alcohol, cannabis, and psychosis were all associated with increased odds of an AMA discharge among non-IDU-IE but not for IDU-IE (Table 2).
Female sex was associated with increased AMA discharge (AOR, 1.21; 95% CI, 1.04–1.41) among IDU-IE, but was associated with decreased AMA discharge among non-IDU-IE (AOR, 0.71; 95% CI, .58–.87). To explore this association further, we plotted the unadjusted, quarterly proportions of AMA discharges stratified by sex. During the study period, AMA IDU-IE discharges among females increased from 14.5% to 25.0% while increasing from 10.0% to 18.0% among males. Among non-IDU-IE hospitalizations, AMA discharges among females increased from 1.9% to 2.5% while increasing among males from 1.9% to 3.2% (Supplementary Figure 1).
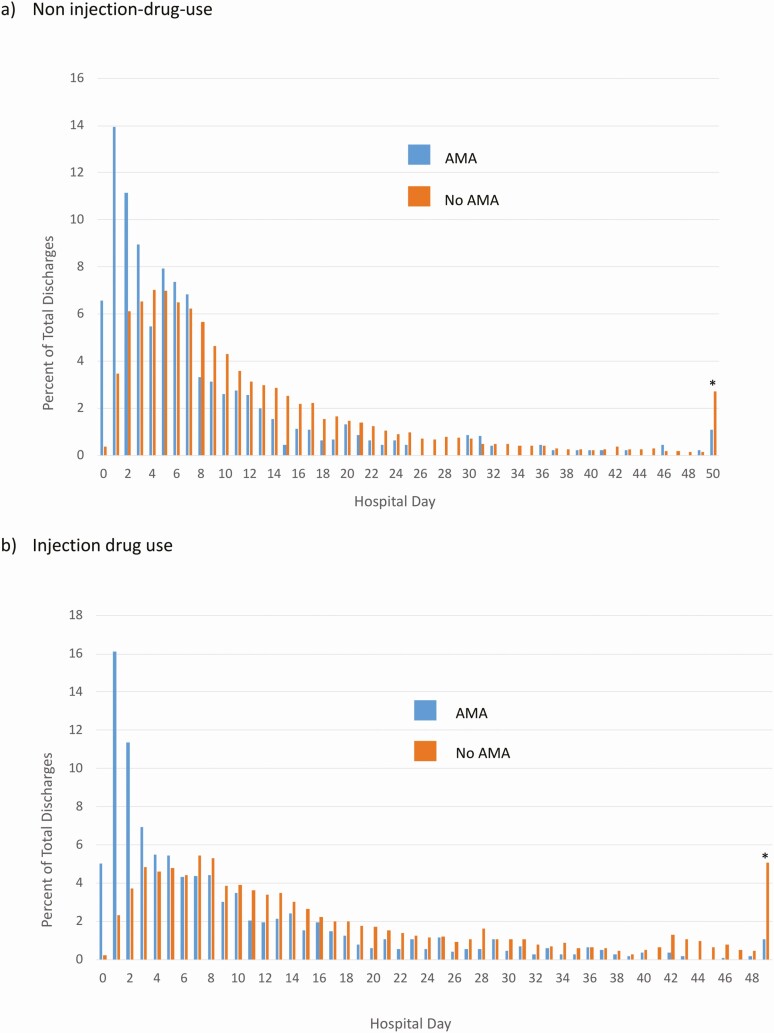
Though the mean LOS is 16.0 days for IDU-IE and 13.4 days for non-IDU, AMA discharges were concentrated early in the hospitalization for both IDU and non-IDU IE. Among IDU-IE AMA discharges, 32.5% occurred on hospital day 0–2 and 31.6% occurred during that same time period for non-IDU-IE. In comparison, non-AMA, live discharges for IDU (6.3%) and non-IDU-IE (10.0%) were uncommon before hospital day 3 (Figure 2).
Figure 2.
Proportion of injection drug use and non-injection drug use-associated infective endocarditis against medical advice discharges and non-AMA, live discharges by hospital day.a,b Abbreviations: AMA, against medical advice; IDU, injection drug use; LOS, length of stay. aHospitalizations with a LOS above the 99th percentile were grouped as having occurred at the 99th percentile, marked by an asterisk (*) at 49 days for IDU and 50 days for non-IDU.
bThis analysis excluded 2910 discharges with in-hospital death and 1 person with missing death data from the study cohort.
DISCUSSION
The proportion of hospitalizations for IE resulting in AMA discharge increased from 2010 to 2015, and during the last quarter of our study (quarter 3 2015), accounted for more than 1 in 5 of all IDU-IE discharges. AMA discharge may result in adverse risk for individuals with IE, a diagnosis that carries morbidity, mortality, and risk of rehospitalization even for those who complete treatment [9, 19]. These data predate evidence for oral antibiotic treatment for IE, suggesting individuals with AMA discharge did not complete treatment in a timely manner, though the treatment may have been completed on subsequent admissions [24]. Furthermore, oral antibiotics are often withheld for those with AMA discharges despite potential benefit [25]. Though several studies have documented rising rates and demographic shifts in individuals with IDU-IE (eg, more women and young people), there has been little examination into the rising proportion or timing of these AMA discharges, particularly in comparison to non-IDU-IE hospitalizations [16, 18].
AMA discharges were common early in the hospitalization of both IDU-IE and non-IDU-IE, but they represented a much larger percentage (21.0% vs 2.9%) and grew more rapidly among IDU-IE. Although initial hospital days can be marked by pain, uncertainty about diagnosis, hospitalization duration, or timing of necessary diagnostic tests and procedures for all individuals with IE, during this period, individuals who inject drugs, such as opioids or stimulants, may experience severe withdrawal symptoms and cravings that can drive AMA discharges [8–11, 14]. In particular, prompt and effective management of opioid withdrawal with methadone or buprenorphine can control opioid withdrawal symptoms. An additional downstream benefit is that after these medications are initiated in the hospital, they can be continued with linkage to outpatient care [26]. Among individuals with infectious complications from injection drug use, medications for opioid use disorder are not routinely offered, although they may facilitate completion of treatments, improve transitions of care, and reduce readmissions and overdose [27–29]. Appropriate withdrawal management early in the hospitalization may reduce AMA discharges for patients with IDU-IE, as demonstrated among people with human immunodeficiency virus who inject drugs [30, 31]. Further, experiences of stigma or poor health literacy may contribute to AMA discharges [11]. Additional strategies to mitigate this outcome include expanding trauma-informed care, linkages, and follow-up with culturally and linguistically competent peers, in-hospital harm reduction services, and treatment of nicotine withdrawal [10, 11, 30, 32, 33]. Hospital-based harm reduction including syringe distribution and supervised injection were acceptable to hospitalized patients who inject drugs, but it is not yet known if these approaches improve outcomes, including AMA discharge [34, 35].
Our study identified several characteristics that were associated with AMA for both IDU-IE and non-IDU-IE. Among both IDU and non-IDU-IE, those with more comorbidities or who received cardiac surgery were less likely to have AMA discharges, perhaps because they lacked the physical capacity to leave. Moreover, receipt of cardiac surgery may be a marker of disease severity and adherence with hospital and treatment team expectations. Younger age, being from low income ZIP codes, and being uninsured or insured by Medicaid were all associated with increased AMA discharges. These patients may also benefit from previously studied approaches including improved health care communication and integrated treatment teams linked to outpatient providers, especially early in the hospitalization when AMA discharges are concentrated [30].
Although the factors associated with the AMA discharge among non-IDU-IE largely parallel those of IDU-IE, gender is 1 exception. Women with non-IDU-IE have 29% lower odds of leaving AMA than men, whereas women with IDU-IE have 21% increased odds of AMA discharge. Higher rates of AMA discharge among women with IDU-IE may be related to high rates of trauma, polysubstance use, and comorbid psychiatric diseases [36]. Additionally, because those with IDU-IE are younger, they may have additional childcare, family, or other competing priorities compared with older women without IDU. Further research is needed to understand these differences and determine if targeted interventions focused on childcare or custody concerns would be beneficial.
The odds of AMA discharge increased 12% per year for IDU-IE and 6% for non-IDU-IE when adjusting for covariates. There are several possible explanations, which we were unable to fully explore with these administrative data. For those with IDU-IE, first, efforts to limit opioid analgesia in the hospital may have resulted in reluctance to treat pain or withdrawal symptoms among individuals with OUD [37]. Second, patients with IDU-IE in the later years of the study may be more likely to use multiple substances, including methamphetamine or cocaine, whose stimulating effects could contribute to AMA discharge [9, 38]. Third, fentanyl, a shorter acting and potent synthetic opioid, entered the heroin supply in certain regions in 2013 [39]. Although this may not fully explain these changes, rapid opioid withdrawal and need for more frequent opioid injections may increase risk for AMA discharge [40].
Several other factors that contributed to the rise in AMA discharges may be relevant for both those with IDU-IE and non-IDU-IE. First, it is not known if hospitals and clinicians have changed their likelihood to assign AMA discharges to patients, either by creating limits on time a patient may leave the hospital floor or less flexibility in negotiating discharge plans because inpatient providers care for a greater number and higher acuity patients in systems focused on patient throughput. Second, patients with both IDU and non-IDU-IE increasingly have lower socioeconomic status [16], and lower health literacy or engagement may have contributed to secular increases in AMA discharges.
This study contributes to improved understanding of IE hospitalization and discharge. First, this study is representative of almost all US IE hospitalizations over more than 5 years. Second, we included separate models for IDU-IE, non-IDU-IE, as well as all IE hospitalizations, allowing detailed comparisons of factors associated with AMA discharge among different groups. Based on these findings, we further explored trends by gender. Third, we included several patient and hospital covariates to adjust for potential confounding and included measurements for length of stay.
This observational study has several limitations. As has been previously described, attribution of IDU status to IE in this cohort is imperfect despite using a validated algorithm [16, 20]. Because coding for opioid use disorder increased with the implementation of ICD-10, we excluded quarter 4 2015 when ICD-9 transitioned to ICD-10 [17]. Second, though we included the Elixhauser score to control for increased comorbidities, granular clinical management for either IE or OUD were not available. Third, we are unable to account for changes in hospital policies about what constitutes an AMA discharge or the likelihood of a clinician to assign AMA status to a discharge. Fourth, because our data are only at the inpatient hospitalization level, we were unable to observe an individual’s subsequent clinical course following AMA discharge, including postdischarge death or total cost of care. Additional hospitalizations may be included in the sample, but were not linked at the individual level. Fifth, we were limited by the data in NIS. For example, information about an individual’s caregiving responsibilities or access to substance use treatment in the hospital is not included. Further, approximately 15% of IE hospitalizations eligible for study inclusion had missing data and thus were excluded from the analytic sample. Finally, these results may not be generalizable to those with prosthetic valves which are difficult to identify in NIS using diagnostic codes in administrative data.
Our results have important implications for clinicians, researchers, hospitals, and policy makers seeking to improve care for individuals with IE. Amid rising IE cases and AMA discharges, our results identify potential opportunities to improve IE care especially early in the hospitalization (eg, treatment of opioid withdrawal) and reduce disparities among women, young people, and socioeconomically disadvantaged individuals.
CONCLUSIONs
In a nationally representative sample of IE admissions, IDU status was highly associated with AMA discharge. Because AMA discharges cluster early in the hospitalization, aggressive withdrawal management, especially for opioids, may mitigate these adverse events. Further efforts are also needed to reduce socioeconomic and gender disparities in AMA discharges.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. The authors acknowledge Ellen McCarthy and Shimon Shaykevich for assistance with data manipulation.
Financial support. S. D. K. received support from the American Society of Addiction Medicine 2017 Annual Fellowship Award, National Institute on Drug Abuse (NIDA) including the Fellows Immersion Training Program (R25DA013582), Research in Addiction Medicine Scholars (RAMS) Program (R25DA033211), the National Institute of Allergy and Infectious Diseases through the Boston University Clinical HIV/AIDS Training Program (5T32AI052074), consulting fees from Abt Associates, and grants as co-principle investigator from RIZE Massachusetts, outside the submitted work. J.-H. K. was supported by the National Research Service Award for Primary Care grant T32HP12706 from the National Institutes of Health. J. H. S. was supported by the RAMS Program (R25DA033211). A. Y. W. reports support from the Clinical Addiction Research and Education Program (R25DA013582), salary support from Massachusetts Department of Public Health; multiple grants as a co-investigator from National Institutes of Health, principle investigator grants from Centers for Disease Control and Prevention, and honorarium from the American Society of Addiction Medicine and University of Kentucky, outside the submitted work. M. R. L. was supported by NIDA (K23 DA042168) and a Boston University School of Medicine Department of Medicine Career Investment Award and research funds paid to his institution from OptumLabs, outside the submitted work. All other authors report no potential conflicts.
Potential conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Deo SV, Raza S, Kalra A, et al. Admissions for infective endocarditis in intravenous drug users. J Am Coll Cardiol 2018; 71:1596–7. [DOI] [PubMed] [Google Scholar]
- 2. Njoroge LW, Al-Kindi SG, Koromia GA, ElAmm CA, Oliveira GH. Changes in the association of rising infective endocarditis with mortality in people who inject drugs. JAMA Cardiol 2018; 3:779–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schranz AJ, Fleischauer A, Chu VH, Wu LT, Rosen DL. Trends in drug use-associated infective endocarditis and heart valve surgery, 2007 to 2017: a study of statewide discharge data. Ann Intern Med 2019; 170:31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rudasill SE, Sanaiha Y, Mardock AL, et al. Clinical outcomes of infective endocarditis in injection drug users. J Am Coll Cardiol 2019; 73:559–70. [DOI] [PubMed] [Google Scholar]
- 5. Rodger L, Glockler-Lauf SD, Shojaei E, et al. Clinical characteristics and factors associated with mortality in first-episode infective endocarditis among persons who inject drugs. JAMA Netw Open 2018; 1:e185220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saitz R, Ghali WA, Moskowitz MA. The impact of leaving against medical advice on hospital resource utilization. J Gen Intern Med 2000; 15:103–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med 2012; 125:594–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eaton EF, Westfall AO, McClesky B, et al. In-hospital illicit drug use and patient-directed discharge: barriers to care for patients with injection-related infections. Open Forum Infect Dis 2020; 7. Available at: 10.1093/ofid/ofaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Merchant E, Burke D, Shaw L, et al. Hospitalization outcomes of people who use drugs: one size does not fit all. J Subst Abuse Treat 2020; 112:23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bearnot B, Mitton JA, Hayden M, Park ER. Experiences of care among individuals with opioid use disorder-associated endocarditis and their healthcare providers: results from a qualitative study. J Subst Abuse Treat 2019; 102:16–22. [DOI] [PubMed] [Google Scholar]
- 11. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: a qualitative study [manuscript published online ahead of print 22 October 2019]. Subst Abus 2019. [DOI] [PubMed] [Google Scholar]
- 12. Wakeman SE, Rich JD. Barriers to post-acute care for patients on opioid agonist therapy; an example of systematic stigmatization of addiction. J Gen Intern Med 2017; 32:17–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Spooner KK, Salemi JL, Salihu HM, Zoorob RJ. Discharge against medical advice in the United States, 2002–2011. Mayo Clin Proc 2017; 92:525–35. [DOI] [PubMed] [Google Scholar]
- 14. Ti L, Ti L. Leaving the hospital against medical advice among people who use illicit drugs: a systematic review. Am J Public Health 2015; 105:e53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Onukwugha E, Alfandre D. Against medical advice discharges are increasing for targeted conditions of the medicare hospital readmissions reduction program. J Gen Intern Med 2019; 34:515–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kimmel SD, Walley AY, Linas BP, et al. Effect of publicly reported aortic valve surgery outcomes on valve surgery in injection drug– and non–injection drug–associated endocarditis. Clin Infect Dis 2019. Available at: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciz834/5584178. Accessed 15 November 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Heslin KC, Owens PL, Karaca Z, Barrett ML, Moore BJ, Elixhauser A. Trends in opioid-related inpatient stays shifted after the US transitioned to ICD-10-CM diagnosis coding in 2015. Med Care 2017; 55:918–23. [DOI] [PubMed] [Google Scholar]
- 18. Wurcel AG, Anderson JE, Chui KKH, et al. Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis 2016; 3:ofw157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bor DH, Woolhandler S, Nardin R, Brusch J, Himmelstein DU. Infective endocarditis in the U.S., 1998–2009: a nationwide study. PLoS One 2013; 8:e60033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ball LJ, Sherazi A, Laczko D, et al. Validation of an algorithm to identify infective endocarditis in people who inject drugs. Med Care 2018; 56:e70–5. [DOI] [PubMed] [Google Scholar]
- 21. Centers for Medicare and Medicard Services General Equivalence Mapping. Available at: http://www.nber.org/data/icd9-icd-10-cm-and-pcs-crosswalk-general-equivalence-mapping.html. Accessed 18 March 2018.
- 22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998; 36:8–27. [DOI] [PubMed] [Google Scholar]
- 23. Healthcare Cost and Utilization Project. National Inpatient Sample Description of Data Elements. Available at: https://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp. Accessed 19 June 2020.
- 24. Iversen K, Ihlemann N, Gill SU, et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N Engl J Med 2019; 380:415–24. [DOI] [PubMed] [Google Scholar]
- 25. Marks LR, Liang SY, Muthulingam D, et al. Evaluation of partial oral antibiotic treatment for persons who inject drugs and are hospitalized with invasive infections. Clin Infect Dis 2020. Available at: http://www.ncbi.nlm.nih.gov/pubmed/32239136. Accessed 3 April 2020. [DOI] [PMC free article] [PubMed]
- 26. Trowbridge P, Weinstein ZM, Kerensky T, et al. Addiction consultation services—linking hospitalized patients to outpatient addiction treatment. J Subst Abuse Treat 2017; 79:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Marks LR, Munigala S, Warren DK, Liang SY, Schwarz ES, Durkin MJ. Addiction medicine consultations reduce readmission rates for patients with serious infections from opioid use disorder. Clin Infect Dis 2018. Available at: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciy924/5142876. Accessed 14 January 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Barocas JA, Morgan JR, Wang J, McLoone D, Wurcel A, Stein MD. Outcomes associated with medications for opioid use disorder among persons hospitalized for infective endocarditis. Clin Infect Dis 2020. Available at: http://www.ncbi.nlm.nih.gov/pubmed/31960025. Accessed 4 March 2020. [DOI] [PMC free article] [PubMed]
- 29. Rosenthal ES, Karchmer AW, Theisen-Toupal J, Castillo RA, Rowley CF. Suboptimal addiction interventions for patients hospitalized with injection drug use-associated infective endocarditis. Am J Med 2016; 129:481–5. [DOI] [PubMed] [Google Scholar]
- 30. Ti L, Milloy MJ, Turje RB, Montaner J, Wood E, Kerr T. The impact of an HIV/AIDS adult integrated health program on leaving hospital against medical advice among HIV-positive people who use illicit drugs. J Public Health (Oxf) 2017; 39:e33–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chan AC, Palepu A, Guh DP, et al. HIV-positive injection drug users who leave the hospital against medical advice: the mitigating role of methadone and social support. J Acquir Immune Defic Syndr 2004; 35:56–9. [DOI] [PubMed] [Google Scholar]
- 32. Sharma M, Lamba W, Cauderella A, Guimond TH, Bayoumi AM. Harm reduction in hospitals. Harm Reduct J 2017; 14:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kathuria H, Seibert RG, Cobb V, et al. Patient and physician perspectives on treating tobacco dependence in hospitalized smokers with substance use disorders: a mixed methods study. J Addict Med 2019; 13:338–45. [DOI] [PubMed] [Google Scholar]
- 34. Ti L, Buxton J, Harrison S, et al. Willingness to access an in-hospital supervised injection facility among hospitalized people who use illicit drugs. J Hosp Med 2015; 10:301–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Brooks HL, O’Brien DC, Salvalaggio G, Dong K, Hyshka E. Uptake into a bedside needle and syringe program for acute care inpatients who inject drugs. Drug Alcohol Rev 2019; 38:423–7. [DOI] [PubMed] [Google Scholar]
- 36. Liebschutz J, Savetsky JB, Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH. The relationship between sexual and physical abuse and substance abuse consequences. J Subst Abuse Treat 2002; 22:121–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Herzig SJ, Mosher HJ, Calcaterra SL, Jena AB, Nuckols TK. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med 2018; 13:263–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Winkelman TNA, Admon LK, Jennings L, Shippee ND, Richardson CR, Bart G. Evaluation of amphetamine-related hospitalizations and associated clinical outcomes and costs in the United States. JAMA Netw Open 2018; 1:e183758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. O’Donnell JK. Deaths involving fentanyl, fentanyl analogs, and U-47700—10 States, July–December 2016. MMWR Morb Mortal Wkly Rep 2017; 66:1197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lambdin BH, Bluthenthal RN, Zibbell JE, Wenger L, Simpson K, Kral AH. Associations between perceived illicit fentanyl use and infectious disease risks among people who inject drugs. Int J Drug Policy 2019; 74:299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.