Abstract
Background
The Cholera Hospital-Based Intervention for 7 Days (CHoBI7) mobile health (mHealth) program was a cluster-randomized controlled trial of diarrhea patient households conducted in Dhaka, Bangladesh.
Methods
Patients were block-randomized to 3 arms: standard message on oral rehydration solution use; health facility delivery of CHoBI7 plus mHealth (no home visits); and health facility delivery of CHoBI7 plus 2 home visits and mHealth. The primary outcome was reported diarrhea in the past 2 weeks collected monthly for 12 months. The secondary outcomes were stunting, underweight, and wasting at a 12-month follow-up. Analysis was intention-to-treat.
Results
Between 4 December 2016 and 26 April 2018, 2626 participants in 769 households were randomly allocated to 3 arms: 849 participants to the standard message arm, 886 to mHealth with no home visits arm, and 891 to the mHealth with 2 home visits. Children <5 years had significantly lower 12-month diarrhea prevalence in both the mHealth with 2 home visits arm (prevalence ratio [PR]: 0.73 [95% confidence interval {CI}, .61–.87]) and the mHealth with no home visits arm (PR: 0.82 [95% CI, .69–.97]). Children <2 years were significantly less likely to be stunted in both the mHealth with 2 home visits arm (33% vs 45%; odds ratio [OR]: 0.55 [95% CI, .31–.97]) and the mHealth with no home visits arm (32% vs 45%; OR: 0.54 [95% CI, .31–.96]) compared with children in the standard message arm.
Conclusions
The CHoBI7 mHealth program lowered pediatric diarrhea and stunting among diarrhea patient households.
Clinical Trials Registration
Keywords: diarrhea, mobile health, child growth, randomized controlled trial
In this trial, young children in diarrhea patient households receiving the CHoBI7 mobile health program had less stunting and diarrhea compared with those only receiving the standard recommendation on oral rehydration solution for dehydration.
(See the Editorial Commentary by Syed and Moore on pages e2569–70.)
Globally, diarrheal diseases are estimated to cause 1.6 million deaths annually [1]. During the time a patient with diarrhea presents at a health facility for treatment, the household members of the patients are at a much higher risk of developing diarrheal diseases (>100 times for cholera) than the general population [2, 3, 4]. This risk is highest during the 7-day period after the patient is admitted to the health facility. This is likely because of a shared contaminated water source and poor hygiene practices in the home [3, 5]. However, despite this high risk, there have been few interventions targeting this susceptible population. The time patients and their caregivers spend at a health facility for the treatment of severe diarrhea provides an opportunity to deliver water, sanitation, and hygiene (WASH) interventions when perceived severity of diarrheal diseases and perceived benefits of water treatment and handwashing with soap are likely highest [6].
In an effort to develop a standard of care to reduce diarrhea among household members of diarrhea patients, our research group developed the Cholera Hospital-Based Intervention for 7 Days (CHoBI7) [7]. Chobi means “picture” in Bangla for the pictorial modules delivered as part of the intervention. This targeted WASH intervention focuses on promoting handwashing with soap and water treatment to diarrhea patients and their household members during the 1-week period after the patient is admitted to the health facility. Delivery of the CHoBI7 program in a randomized controlled trial (RCT) of cholera patient households resulted in a significant reduction in symptomatic cholera during the 1-week high-risk period after the presentation of the index patient [7], and sustained improvements in stored drinking water quality and observed handwashing with soap practices 12 months post-intervention [8].
To build evidence to take the CHoBI7 program to scale in Bangladesh, we partnered with the Bangladesh Ministry of Health and Family Welfare to develop and evaluate scalable approaches for CHoBI7 program delivery. Mobile health (mHealth) messages present a scalable approach for which public health information can be sent to a large population at minimal cost, and has the potential to serve as cues to action to facilitate behavior change [9]. In the past 10 years, mobile phone access and ownership have increased substantially, with mobile phone subscriptions doubling globally [10]. In Bangladesh alone, >158 million phone numbers are registered [11]. This presents an ideal environment for large-scale messaging of public health information using mobile phones. However, there are no published RCTs evaluating delivery of a WASH mHealth program.
We aimed to investigate whether delivery of the CHoBI7 mHealth program through sending mobile messages and conducting in-person visits with diarrhea patient households could significantly reduce diarrhea, improve child growth, and increase handwashing with soap behaviors and stored drinking water quality over the 12 month program period.
METHODS
Study Design
The CHoBI7 mHealth study was a 3-arm cluster RCT conducted in urban Dhaka, Bangladesh, from 4 December 2016 to 26 April 2019, where a diarrhea patient’s household was a cluster including the patient and their corresponding household members. Diarrhea patients were recruited from 2 tertiary-level health facilities, Mugda Hospital (government hospital) and the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) Dhaka Hospital (private hospital). The cluster RCT compared the standard recommendation given in Bangladesh to diarrhea patients at discharge from health facility staff on oral rehydration solution use for dehydration (standard message arm) to the CHoBI7 mHealth program with either a single in-person visit for health facility delivery of the program (mHealth with no home visits arm) or health facility delivery of the program plus 2 home visits (mHealth with 2 home visits arm). The 2 home visits were delivered by study health promoters twice during the 1-week high-risk period, after the diarrhea patient was discharged from the health facility. The mHealth program included WASH-related voice and text messages weekly for 12 months. The study protocol was approved by the Ethical Review Committee at icddr,b (Protocol 15133) and the Institutional Review Board of the Johns Hopkins Bloomberg School of Public Health (Protocol 6785).
Participants
To be eligible for the trial, patients had to (1) have had ≥3 loose stools over the past 24 hours; (2) plan to reside in Dhaka for the next 12 months; (3) have no basin for running water in their home (mostly slum areas of Dhaka); (4) have a child <5 years of age in their household (including themselves) who produced a stool sample at baseline (used to determine the etiology of diarrhea); and (5) have a working mobile phone in the household. Household members of the diarrhea patient were eligible for the trial if (1) they shared the same cooking pot and resided in the same home with the patient for the last 3 days; and (2) planned to reside with the patient for the next 12 months. Study recruitment of diarrhea patients at Dhaka icddr,b and Mugda Hospital occurred Saturday–Thursday from 7:30 am to 4 pm each week during the study period from December 2016 to April 2018.
Randomization and Masking
Block randomization of diarrhea patients to study arms was performed based on the date of hospital admission, stratified by site, and the hospital ward where patients received treatment using a random number generator. A detailed description of the randomization and masking is included in Supplementary Appendix 1.
Intervention Procedures
The CHoBI7 mHealth program was developed through a theory-driven approach informed by the Integrated Behavioral Model for Water, Sanitation and Hygiene and the Risks, Attitudes, Norms, Abilities, and Self-Regulation model. A detailed description of intervention development is published elsewhere [12]. The CHoBI7 mHealth program targets 5 key behaviors: (1) preparing soapy water using water and detergent powder; (2) handwashing with soap at food- and stool-related events; (3) treating household drinking water using chlorine tablets during the 1-week high-risk period after the diarrhea patient in the household is admitted to the health facility; (4) storing safe drinking water in a water vessel with a lid and tap; and (5) heating household drinking water until it reaches a rolling boil after the 1-week high-risk period.
The CHoBI7 mHealth program is initially delivered during a health facility visit by a health promoter bedside to a diarrhea patient and their accompanying household members during the time of illness. The health promoter delivers a pictorial CHoBI7 WASH module on how diarrhea can spread, and instructions on handwashing with soap at stool- and food-related events and water treatment. A diarrhea prevention package containing the following items is also provided: a 1-month supply of chlorine tablets (Aquatabs [sodium dichloroisocyanurate]; Medentech, Wexford, Ireland, UK) for water treatment, a soapy water bottle containing water and detergent powder, a handwashing station, and a water vessel with a lid and tap to ensure safe water storage. Households are instructed to boil their drinking water once their supply of chlorine tablets is completed, and encouraged to make more soapy water after their provided bottle is finished. After health facility delivery of the program, diarrhea patient households receive weekly voice and text messages from the CHoBI7 mHealth program over a 12-month period. These mobile messages are sent using the web-based VIAMO mobile platform to all phone numbers provided by study households. Two characters deliver the CHoBI7 mHealth messages: “Dr Chobi” and “Aklima” [12]. Dr Chobi is a doctor at a hospital who calls and texts participants to share information and reminders on handwashing with soap and water treatment behaviors. Aklima is a woman who brought her child to a health facility for diarrhea treatment, and who learned proper handwashing with soap and water treatment behaviors from Dr Chobi in voice and text messages. The following is an example of a CHoBI7 mHealth program voice message:
Dr Chobi: Hello, this is Dr Chobi from the hospital. Aklima is here with me again today and wants to share her story.
Aklima: My son was very sick; he almost died. Dr Chobi told me about washing my hands with soap at 4 key times: before I prepare food, before I eat, and after I use the toilet or clean my child’s feces or anus. I have followed all these instructions all the time, and my family is now healthy and happy!
The following is an example of a CHoBI7 mHealth program text message:
Though your water may look clean, it can still have germs. Heat your water until it reaches a rolling boil then the diarrhea germs will be killed. Keep your family healthy. Share this message! -Dr. Chobi
In the mHealth with 2 home visits arm, two 30-minute home visits are conducted during the week after the index diarrhea patient is recruited at the health facility.
Evaluation Procedure
Diarrhea was defined as at least ≥3 loose stools over a 24-hour period in the preceding 2 weeks. Clinical surveillance for diarrhea was performed at baseline enrollment and monthly thereafter until the 12-month time point for all enrolled household members. For children <12 years of age, diarrhea was assessed through caregiver reports. For children <5 years, research assistants trained in standardized anthropometry measured the child’s weight once and height/length 3 times at baseline and at a 12-month follow-up. Height and weight measurements were used to calculate height-for-age z scores (HAZ), weight-for-age z scores (WAZ), and weight-for-height z scores (WHZ) according to the World Health Organization (WHO) child growth standards [13]. The z score cutoff point of < −2 standard deviations was used to define stunting (HAZ < −2), underweight (WAZ < −2), and wasting (WHZ < −2).
To assess household stored drinking water quality, unannounced spot checks were performed in a randomly selected subset of 150 households per study arm at 1 week, and 1, 3, 6, 9, and 12 months after enrollment to collect a water sample from the household’s stored drinking water to test for Escherichia coli by bacterial culture [14]. Two cutoffs were used: (1) the WHO water quality guideline of <1 colony-forming unit (CFU)/100 mL of E. coli in drinking water; and (2) the WHO classification of high risk for drinking water supplies cutoff of 100 CFU/100 mL E. coli [15]. To observe handwashing behaviors, 5-hour structured observation was conducted in a randomly selected subset of 50 households per study arm from 7:30 am to 12:30 pm at 1 week, and 1, 3, 6, 9, and 12 months after enrollment. Handwashing with soap was recorded at food- and stool-related events.
Outcomes
Primary outcomes were the prevalence of diarrhea among children <2 and <5 years, and diarrhea prevalence in all age groups over the 12-month study period based on monthly surveillance. Secondary outcomes were: (1) stunting, underweight, and wasting at 12 months for children <2 and <5 years; (2) household members handwashing with soap at food- and stool-related events (a measure of handwashing compliance) (for all individuals in the household >2 years of age); and (3) households with stored drinking water samples without detectable E. coli (<1 CFU/100 mL) and ≥100 CFU/100 mL E. coli. All diarrhea prevalence and WASH outcomes were measured over the 12-month study period.
Statistical Analysis
The sample size calculation is listed in Supplementary Appendix 1. We analyzed participants according to their randomized assignment (intention-to-treat). Log binomial regression was performed to estimate the prevalence ratio for diarrheal disease, and logistic regression was performed to calculate odds ratios (ORs) for child growth outcomes using generalized estimating equations (GEEs) to account for clustering at the individual and household level and to approximate 95% confidence intervals (CIs). Models for diarrheal disease were adjusted for follow-up time, and models for follow-up child growth were adjusted for baseline growth measurements. Logistic regression models were performed to compare indicators of intervention fidelity by study arm using GEE to account for clustering within households and approximate 95% CIs. Models for stored drinking water quality were adjusted for source water E. coli concentrations at each time point. Analyses were performed in SAS software (version 9.4). The trial is registered at ClinicalTrials.gov (identifier NCT04008134).
RESULTS
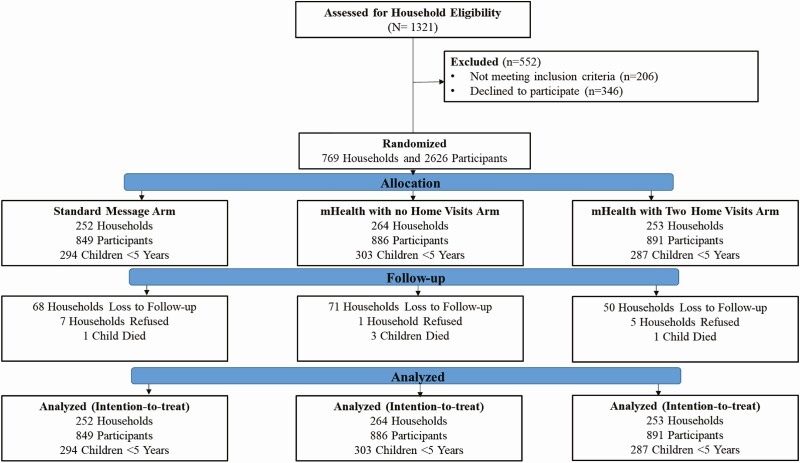
Between December 2016 and April 2018, we randomly allocated 769 diarrhea patient households (2626 participants total) to the following arms: standard message, mHealth with no home visits, or mHealth with 2 home visits (Figure 1). Twenty-five percent of households (n = 189) were lost to follow-up at the 12-month time point. Five children died during the study period. Baseline characteristics of enrolled households were similar across study arms (Table 1).
Figure 1.
Trial profile and analysis populations for primary outcomes. Abbreviation: mHealth, mobile health.
Table 1.
Baseline Population Characteristics by Study Arm
| Characteristic | Standard Message Arm | mHealth With No Home Visits Arm | mHealth With 2 Home Visits Arm |
|---|---|---|---|
| Study households, No. | 252 | 264 | 253 |
| All study participants, No. | 849 | 886 | 891 |
| Index diarrhea patients, No. | 252 | 264 | 253 |
| Household members of index diarrhea patients, No. | 597 | 622 | 638 |
| Children <5 y of age at baseline, No. | 294 | 303 | 289 |
| Baseline household member age, y | |||
| Median ± SD (Min–Max) | 19 ± 15 (0.08–75) | 20 ± 15 (0.08–80) | 20 ± 15 (0.08–75) |
| 0–5 | 34% | 34% | 32% |
| 5–17 | 13% | 11% | 12% |
| ≥18 | 53% | 55% | 56% |
| Sex | |||
| Female | 56% | 55% | 54% |
| Household roof type | |||
| Tin | 33% | 28% | 28% |
| Concrete | 66% | 71% | 72% |
| Other | 1% | <1% | 0% |
| Household wall type | |||
| Concrete | 73% | 71% | 71% |
| Mud | 4% | 3% | 4% |
| Tin | 22% | 26% | 25% |
| Other | <1% | 0% | <1% |
| Household floor type | |||
| Concrete | 96% | 97% | 96% |
| Other | 4% | 3% | 4% |
| Household electricity access | 94% | 93% | 92% |
| Household refrigerator ownership | 41% | 45% | 43% |
| Household baseline water source | |||
| <1 CFU/100 mL of Escherichia coli | 28% | 20% | 30% |
| 1–10 CFU/100 mL of E. coli | 6% | 9% | 10% |
| 10–100 CFU/100 mL of E. coli | 14% | 19% | 17% |
| >100 CFU/100 mL of E. coli | 52% | 52% | 43% |
| At least 1 household member can read and write | 92% | 95% | 93% |
| Anthropometric measurements for children <5 y of age at baseline | |||
| Stunting (HAZ < −2) | 24% | 20% | 25% |
| Underweight (WAZ < −2) | 35% | 33% | 30% |
| Wasting (WHZ < −2) | 31% | 32% | 26% |
Abbreviations: CFU, colony-forming units; HAZ, height-for-age z score; SD, standard deviation; WAZ, weight-for-age z score; WHZ, weight-for-height z score.
Compared to the standard message arm, children <5 years of age had significantly lower 12-month diarrhea prevalence in the mHealth with 2 home visits arm (prevalence ratio [PR]: 0.73 [95% CI: .61–.87]) and the mHealth with no home visits arm (PR: 0.82 [95% CI: .69–.97]) (Table 2). This impact was stronger for children <2 years of age in both the mHealth with 2 home visits arm (PR: 0.69 [95% CI: .58–.83]) and the mHealth with no home visits arm (PR: 0.78 [95% CI: .65–.93]). For all age groups combined (children and adults), the diarrhea prevalence was 29% lower in the mHealth with 2 home visits arm (PR: 0.71 [95% CI: .60–.84]), and 18% lower in the mHealth with no home visits arm (PR: 0.82 [95% CI: .69–.97]). There was no statistically significant difference between the mHealth with two home visits arm compared to the mHealth with no home visits arm on diarrhea prevalence for any age group.
Table 2.
Effects of the Cholera Hospital-based Intervention for 7 Days (CHoBI7) Mobile Health Program on 12-Month Diarrhea Prevalence
| Study Arm | No. | Mean Diarrhea Prevalence, % | Prevalence Ratio (95% CI)a |
|---|---|---|---|
| Standard message | |||
| <2 y | 195 | 25% | – |
| <5 y | 273 | 21% | – |
| All age groups | 771 | 12% | – |
| mHealth with no home visits | |||
| <2 y | 198 | 19% | 0.78 (.65–.93) |
| <5 y | 279 | 17% | 0.82 (.69–.97) |
| All age groups | 793 | 10% | 0.82 (.69–.97) |
| mHealth with 2 home visits | |||
| <2 y | 214 | 17% | 0.69 (.58–.83) |
| <5 y | 276 | 15% | 0.73 (.61–.87) |
| All age groups | 824 | 8% | 0.71 (.60–.84) |
Abbreviations: CI, confidence interval; mHealth, mobile health.
aAdjusted for follow-up timepoint.
Children <2 years were significantly less likely to be stunted in both the mHealth with 2 home visits arm (33% vs 45%; OR, 0.55 [95% CI: .31–.97]) and the mHealth with no home visits arm (32% vs 45%; OR, 0.54 [95% CI: .31–.96]) compared with the standard message arm after adjustment for baseline growth measures (Table 3). There were no other statistically significant differences in stunting, wasting, or underweight identified for either age group between study arms.
Table 3.
Effects of the Cholera Hospital-based Intervention for 7 Days (CHoBI7) Mobile Health Program on Child Growth at the 12-Month Timepoint
| 12-Month Timepoint | StandardMessage Arm | mHealth With No Home Visits Arm | mHealth With 2 Home Visits Arm | mHealth With No Home Visits Arm | mHealth With 2 Home Visits Arm | ||
|---|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | ||||||
| Unadjusted | Adjusteda | Unadjusted | Adjusteda | ||||
| Children <2 y of age, No. | 108 | 108 | 123 | ||||
| Stunting | 45% | 32% | 33% | 0.57 (.33–.99) | 0.54 (.31–.96) | 0.60 (.35–1.03) | 0.55 (.31–.97) |
| Underweight | 30% | 31% | 27% | 1.04 (.58–1.87) | 1.23 (.66–2.32) | 0.89 (.50–1.59) | 1.05 (.55–2.00) |
| Wasting | 13% | 19% | 14% | 1.53 (.73–3.20) | 1.56 (.73–3.31) | 1.08 (.50–2.30) | 1.16 (.53–2.51) |
| Children <5 y of age, No. | 188 | 187 | 203 | ||||
| Stunting | 39% | 30% | 35% | 0.66 (.43–1.02) | 0.72 (.46–1.12) | 0.81 (.54–1.23) | 0.82 (.53–1.27) |
| Underweight | 27% | 28% | 24% | 1.06 (.67–1.70) | 1.20 (.72–1.99) | 0.87 (.54–1.38) | 1.00 (.60–1.66) |
| Wasting | 13% | 16% | 12% | 1.20 (.67–2.16) | 1.19 (.65–2.16) | 0.92 (.50–1.67) | 1.00 (.54–1.85) |
Abbreviations: CI, confidence interval; mHealth, mobile health.
aAdjusted for baseline stunting, underweight, or wasting.
Handwashing with soap at food related events was significantly higher in the mHealth with no home visits arm and mHealth with 2 home visits arm compared to the standard message arm at all time points except for 6 months (Table 4). Relative to the WHO water quality guideline (<1 CFU E.coli/ 100 mL), the mHealth arms had significantly higher water quality compared to the standard message arm at the week 1 and month 1 time points (Table 5). Relative to the WHO high-risk category for water quality (≥100 CFU E.coli/100 mL), both mHealth arms had significantly fewer households in this high-risk category compared to the standard message arm at the month 12 time point.
Table 4.
Effects of the Cholera Hospital-based Intervention for 7 Days (CHoBI7) Mobile Health Program on Handwashing With Soap at Stool- and Food-related Events During 5-Hour Structured Observation (Individuals >2 Years of Age)
| Study Arm | Individuals Handwashing With Soap at a Stool- or Food-related Event | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Week (n = 297) | 1 Month (n = 276) | 3 Months (n = 233) | 6 Months (n = 349) | 9 Months (n = 352) | 12 Months (n = 382) | |||||||
| % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | |
| Standard message | 40 | – | 27 | – | 23 | – | 30 | – | 23 | – | 31 | – |
| mHealth with no home visits | 70 | 3.38 (1.67–6.84) | 50 | 2.72 (1.40–5.27) | 52 | 3.63 (1.77–7.45) | 48 | 2.19 (1.25–3.83) | 34 | 1.69 (.94–3.04) | 44 | 1.73 (1.08–2.78) |
| mHealth with 2 home visits | 71 | 3.60 (1.84–7.05) | 52 | 2.89 (1.47–5.67) | 58 | 4.67 (2.39–9.10) | 40 | 1.54 (.92–2.59) | 39 | 2.13 (1.19–3.79) | 31 | 1.02 (.61–1.69) |
| mHealth with 2 home visits vs mHealth with no home visits | – | 1.06 (.61–1.86) | – | 1.06 (.55–2.04) | – | 1.29 (.65–2.56) | – | 0.71 (.40–1.26) | – | 1.26 (.75–2.12) | – | 0.59 (.36–.97) |
| Individuals Handwashing With Soap at a Food-related Event | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Week (n = 279) | 1 Month (n = 253) | 3 Months (n = 221) | 6 Months (n = 326) | 9 Months (n = 321) | 12 Months (n = 347) | |||||||
| % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | |
| Standard message | 26 | – | 13 | – | 12 | – | 15 | – | 10 | – | 9 | – |
| mHealth with no home visits | 47 | 2.56 (1.20–5.49) | 36 | 3.89 (1.62–9.33) | 34 | 3.63 (1.64–8.05) | 26 | 1.92 (.95–3.87) | 26 | 3.16 (1.47–6.80) | 34 | 5.16 (2.38–11.19) |
| mHealth with 2 home visits | 59 | 4.07 (1.95–8.51) | 44 | 5.42 (2.34–12.55) | 38 | 4.27 (1.97–9.26) | 26 | 1.97 (.99–3.93) | 22 | 2.50 (1.17–5.33) | 25 | 3.34 (1.53–7.31) |
| mHealth with 2 home visits vs mHealth with no home visits | – | 1.59 (.87–2.90) | – | 1.39 (.67–2.91) | – | 1.17 (.58–2.36) | – | 1.03 (.51–2.08) | – | 0.79 (.40–1.58) | – | 0.65 (.35–1.18) |
| Individuals Handwashing With Soap at a Stool-related Event | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Week (n = 221) | 1 Month (n = 178) | 3 Months (n = 148) | 6 Months (n = 198) | 9 Months (n = 203) | 12 Months (n = 241) | |||||||
| % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | |
| Standard message | 36 | – | 35 | – | 31 | – | 44 | – | 30 | – | 38 | – |
| mHealth with no home visits | 71 | 4.26 (1.85–9.80) | 50 | 1.89 (.91–3.94) | 57 | 2.97 (1.32–6.70) | 57 | 1.65 (.81–3.35) | 35 | 1.22 (.59–2.54) | 37 | 0.96 (.51–1.79) |
| mHealth with 2 home visits | 67 | 3.50 (1.64–7.48) | 51 | 1.96 (.89–4.31) | 60 | 3.35 (1.58–7.13) | 45 | 1.05 (.54–2.05) | 49 | 2.23 (1.06–4.68) | 34 | 0.83 (.43–1.57) |
| mHealth with 2 home visits vs mHealth with no home visits | – | 0.82 (.44–1.53) | – | 1.03 (.52–2.07) | – | 1.13 (.51–2.52) | – | 0.64 (.30–1.34) | – | 1.82 (.93–3.58) | – | 0.86 (.44–1.68) |
Abbreviations: CI, confidence interval; mHealth, mobile health; OR, odds ratio.
Table 5.
Effects of the Cholera Hospital-based Intervention for 7 Days (CHoBI7) Mobile Health Program on Household Stored Drinking Water Quality Assessed During Unannounced Spot Checks
| Study Arm | 1 Week (n = 486) | 1 Month (n = 375) | 3 Months (n = 438) | 6 Months (n = 441) | 9 Months (n = 418) | 12 Months (n = 483) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | |
| WHO high-risk category for water quality (≥100 CFU/100 mL Escherichia coli) | ||||||||||||
| Standard message | 51 | – | 50 | – | 60 | – | 45 | – | 47 | – | 52 | – |
| mHealth with no home visits | 27 | 0.37 (.23–.58) | 40 | 0.64 (.38–1.08) | 43 | 0.52 (.33–.83) | 43 | 0.91 (.57–1.46) | 38 | 0.71 (.44–1.16) | 40 | 0.63 (.40–.99) |
| mHealth with 2 home visits | 18 | 0.22 (.14–.37) | 32 | 0.43 (.25–.72) | 41 | 0.51 (.32–.82) | 43 | 0.90 (.57–1.42) | 39 | 0.76 (.47–1.23) | 40 | 0.64 (.41–.99) |
| mHealth with 2 home visits vs mHealth with no home visits | – | 0.61 (.36–1.04) | – | 0.66 (.40–1.11) | – | 0.98 (.61–1.57) | – | 0.91 (.62–1.56) | – | 1.07 (.66–1.73) | – | 1.02 (.66–1.58) |
| WHO safe water quality guideline (<1 CFU/100 mL E. coli) | ||||||||||||
| Standard message | 8 | – | 9 | – | 12 | – | 11 | – | 12 | – | 14 | – |
| mHealth with no home visits | 51 | 11.07 (5.91–20.76) | 21 | 2.68 (1.22–5.91) | 15 | 1.23 (.63–2.40) | 9 | 0.80 (.36–1.78) | 20 | 1.67 (.85–3.26) | 17 | 1.18 (.63–2.20) |
| mHealth with 2 home visits | 68 | 22.45 (11.82–42.64) | 31 | 4.95 (2.39–10.45) | 13 | 0.95 (.47–1.94) | 13 | 1.27 (.62–2.59) | 18 | 1.51 (.77–2.96) | 15 | 1.03 (.55–1.92) |
| mHealth with 2 home visits vs mHealth with no home visits | – | 2.03 (1.29–3.19) | – | 1.85 (1.04–3.29) | – | 0.78 (.39–1.53) | – | 1.59 (.74–3.39) | – | 0.90 (.50–1.65) | – | 0.87 (.48–1.57) |
Abbreviations: CFU, colony-forming units; CI, confidence interval; mHealth, mobile health; OR, odds ratio; WHO, World Health Organization.
Discussion
Delivery of the CHoBI7 mHealth program resulted in significantly lower pediatric diarrhea and stunting, and led to sustained improvements in household stored drinking water quality and handwashing with soap behaviors over the 12-month program period. Furthermore, there was no evidence of a large difference in child growth or diarrhea outcomes when including 2 homes visits vs no home visits for intervention delivery. This result shows that WASH behavior change is possible without the need for frequent home visits by a promoter. Our findings demonstrate that the CHoBI7 mHealth program can be delivered to improve child health and facilitate sustained WASH behavior change.
The success of the CHoBI7 mHealth program is likely because of several key factors. First is the timing of intervention delivery when there was acute illness in the household. This was the time when perceived susceptibility of diarrheal diseases and the perceived benefits of practicing WASH behaviors were likely the highest [6], and therefore more amenable to change. Second, we targeted a population living mostly in slum areas of Dhaka without running water in their home that was at high risk for diarrheal disease. This allowed us to focus on a population that would likely benefit the most from the recommended WASH behaviors. Third, the sender of the mobile messages, Dr Chobi, was a physician at a hospital and viewed as a creditable source of information in our formative research [12]. Fourth, our theory-driven and evidence-based approach for intervention development allowed us to tailor our intervention for our target population. Fifth, we included both voice and text messages in our mHealth program. Voice messages allowed our information to be understood by those who could not read, and text messages allowed for sharing mobile message content with others.
The lower diarrhea prevalence observed with delivery of the CHoBI7 mHealth program is comparable to recent findings from the Bangladesh WASH Benefits study site [16]. The WASH Benefits study is a large-scale WASH and nutrition RCT, including modules on water treatment, handwashing with soap, safe child feces disposal, and provision of a double-pit pour-flush improved latrine. At the Bangladesh site, these interventions were delivered through an average of 6 home visits monthly. The combined WASH arm in the Bangladesh WASH Benefits trial that received all of these WASH interventions had a diarrhea PR of 0.69 (95% CI: .53–.90) compared to the control arm [16], similar to the PR of 0.69 (95% CI: .58–.82) found in the mHealth with 2 home visits arm of our trial. Our findings are also comparable to a recent meta-analysis of WASH interventions, which estimated a relative risk of 0.67 (95% CI: .63–.73) for water treatment interventions and 0.70 (95% CI: .64–.77) for hygiene interventions [17].
The significant association between delivery of our WASH intervention and improvements in stunting for children <2 years is consistent with 2 previous studies conducted in Mali and Ethiopia [18, 19]. In Pickering et al, delivery of a community-led-total-sanitation intervention in Mali resulted in increased linear growth and less stunting in children <5 years of age in the intervention compared to a control arm, with the greatest impact observed for children <2 years of age [19]. In Fenn et al, delivery of a WASH intervention which included education, pit latrines, and clean water sources resulted in significantly improved linear growth in the intervention group compared with a comparison group for children 6–36 months of age [18]. The first 2 years of life are when children are most susceptible to growth faltering [20]. Therefore, this critical window is likely when interventions will have the most impact on improving child growth.
Our study findings are in contrast with the recent WASH Benefits and Sanitation, Hygiene, Infant Nutrition Efficacy Project (SHINE) trials conducted in Bangladesh, Kenya, and Zimbabwe, which found no improvements in linear growth with delivery of WASH interventions including modules on water treatment, handwashing with soap, safe child feces disposal, and the provision of improved latrines [16, 21, 22]. The effectiveness of our intervention in improving child growth is likely attributed to the high-risk population we targeted, which had a household member recently admitted to a health facility for diarrhea, resided mostly in slum areas of Dhaka, and lacked running water in their home. The diarrhea prevalence among children <2 years of age in our study was 25% during the study period compared to 6% in the recent WASH Benefits Bangladesh trial [16]. The higher rate of enteric infections within our study population likely provided more room for improvement in child growth. No previous study, to our knowledge, has assessed the relationship between WASH intervention delivery and child growth for this high-risk population with a family member that recently came to the hospital for diarrhea. In addition, our study was conducted in an urban setting compared to the recent WASH Benefits and SHINE trials, which were both conducted in rural settings. Future intervention studies are needed to establish the reproducibility of this finding, and to evaluate the impact of delivery of the CHoBI7 mHealth program in both urban and rural settings for this high-risk population.
This study has some limitations. First, since all intervention arms received the CHoBI7 mHealth program mobile messages, we do not know the impact of health facility and home visits for intervention delivery alone on diarrhea rates and child growth, nor do we know the impact of the handwashing station and water vessel alone on improving our health outcomes. Future studies should assess the added benefit of mHealth messages to in-person visits alone, and assess the added benefit of the provision of the diarrhea prevention package. Second, we assessed our intervention only among a high-risk population without running water in their home. Future studies should assess the efficacy of this intervention for populations with running water in their household. Third, we conducted our study in an urban area, which limits the generalizability of our findings to rural settings.
This study has several strengths. First is our clinical surveillance of both child and adult diarrhea prevalence. Second is performing structured observation of handwashing with soap practices at multiple time points. Third is the inclusion of the second intervention arm, which allowed us to investigate the added benefit of home visits to the CHoBI7 mHealth program. Fourth is the frequent water quality measurements to assess household stored drinking water quality. Fifth is the 12-month duration of the study period, which allowed us to account for seasonal variations in diarrheal disease and WASH behaviors in our study population.
The CHoBI7 mHealth program significantly lowered pediatric diarrhea and stunting, and resulted in sustained handwashing with soap and improved household stored drinking water quality over a 12-month period. Furthermore, our findings demonstrate that frequent home visits were not needed to facilitate WASH behavior change. We are currently partnering with the Bangladesh Ministry of Health and Family Welfare to develop a scaling plan to deliver the CHoBI7 mHealth program across Bangladesh. Our findings suggest that mHealth presents a promising tool to improve child health and increase WASH behaviors.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Financial support. This research was supported by a United States Agency for International Development (USAID), Development Innovation Ventures grant awarded to Johns Hopkins School of Public Health. We thank USAID for their support. We thank the study participants and the following individuals for their support with the implementation of this study: Professor Abul Khair Mohammad Shamsuzzaman, Professor Be-Nazir Ahmed, Fosiul Alam Nizame, Khobair Hossain, Jahed Masud, Ismat Minhaj Uddin, Rafiqul Islam, Maynul Hasan, SM. Arifur Rahman, Abdullah Al Morshed, Zakir Hossain, Kabir Hossain, Amal Sarker, Abul Bashar Sikder, Abdul Matin, Sadia Afrin Ananya, Lubna Tani, Farhana Ahmed, Tahera Taznen, Marufa Akter, Akhi Sultana, Nasrin Akter, Laki Das, Abdul Karim, Shirin Akter, Khan Ali Afsar and Wasim Ahmed Asif. We also thank hospital staff for their support. icddr,b acknowledges the governments of Bangladesh, Canada, Sweden, and United Kingdom for providing core/unrestricted support.
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. GBD 2016 Diarrhoeal Disease Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis 2018; 18:1211–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. George CM, Hasan K, Monira S, et al. A prospective cohort study comparing household contact and water Vibrio cholerae isolates in households of cholera patients in rural Bangladesh. PLoS Negl Trop Dis 2018; 12:e0006641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. George CM, Ahmed S, Talukder KA, et al. Shigella infections in household contacts of pediatric shigellosis patients in rural Bangladesh. Emerg Infect Dis 2015; 21:2006–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Weil AA, Khan AI, Chowdhury F, et al. Clinical outcomes in household contacts of patients with cholera in Bangladesh. Clin Infect Dis 2009; 49:1473–9. doi: 10.1086/644779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burrowes V, Perin J, Monira S, et al. Risk factors for household transmission of vibrio cholerae in Dhaka, Bangladesh (CHoBI7 Trial). Am J Trop Med Hyg 2017; 96:1382–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Figueroa ME, Kincaid DL. Social, cultural and behavioral correlates of household water treatment and storage. Household water treatment and safe storage. Geneva, Switzerland: World Health Organization, 2007. [Google Scholar]
- 7. George CM, Monira S, Sack DA, et al. Randomized controlled trial of hospital-based hygiene and water treatment intervention (CHoBI7) to reduce cholera. Emerg Infect Dis 2016; 22:233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. George CM, Jung DS, Saif-Ur-Rahman KM, et al. Sustained uptake of a hospital-based handwashing with soap and water treatment intervention (cholera-hospital-based intervention for 7 days [CHoBI7]): a randomized controlled trial. Am J Trop Med Hyg 2016; 94:428–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med 2013; 10:e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Information and communication technologies (ICT). Key ICT indicators for developed and developing countries and the world (totals and penetration rates). 2017. Available at: https://www.itu.int/en/ITU-D/Statistics/Pages/stat/default.aspx. Accessed 28 September 2018.
- 11. Bangladesh Telecommunication Regulatory Commission. Current news and notice board. 2019. Available at: http://www.btrc.gov.bd/content/mobile-phone-subscribers-bangladesh-february-2019. Accessed February 2019. [Google Scholar]
- 12. George CM, Zohura F, Teman A, et al. Formative research for the design of a scalable water, sanitation, and hygiene mobile health program: CHoBI7 mobile health program. BMC Public Health 2019; 19:1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Onis M, Onyango AW. WHO child growth standards. Lancet 2008; 371:204. [DOI] [PubMed] [Google Scholar]
- 14. Islam MS, Siddika A, Khan MN, et al. Microbiological analysis of tube-well water in a rural area of Bangladesh. Appl Environ Microbiol 2001; 67:3328–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. World Health Organization. Guidelines for drinking-water quality. Geneva, Switzerland:WHO, 2011. [Google Scholar]
- 16. Luby SP, Rahman M, Arnold BF, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: a cluster randomised controlled trial. Lancet Glob Health 2018; 6:e302–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wolf J, Hunter PR, Freeman MC, et al. Impact of drinking water, sanitation and handwashing with soap on childhood diarrhoeal disease: updated meta-analysis and meta-regression. Trop Med Int Health 2018; 23:508–25. [DOI] [PubMed] [Google Scholar]
- 18. Fenn B, Bulti AT, Nduna T, Duffield A, Watson F. An evaluation of an operations research project to reduce childhood stunting in a food-insecure area in Ethiopia. Public Health Nutr 2012; 15:1746–54. [DOI] [PubMed] [Google Scholar]
- 19. Pickering AJ, Djebbari H, Lopez C, Coulibaly M, Alzua ML. Effect of a community-led sanitation intervention on child diarrhoea and child growth in rural Mali: a cluster-randomised controlled trial. Lancet Glob Health 2015; 3:e701–11. [DOI] [PubMed] [Google Scholar]
- 20. Victora CG, de Onis M, Hallal PC, Blössner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 2010; 125:e473–80. [DOI] [PubMed] [Google Scholar]
- 21. Null C, Stewart CP, Pickering AJ, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: a cluster-randomised controlled trial. Lancet Glob Health 2018; 6:e316–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Humphrey JH, Mbuya MNN, Ntozini R, et al. Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial Team . Independent and combined effects of improved water, sanitation, and hygiene, and improved complementary feeding, on child stunting and anaemia in rural Zimbabwe: a cluster-randomised trial. Lancet Glob Health 2019; 7:e132–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.