Abstract
Objectives The present study examines the effect of median household income on mid- and long-term outcomes in a posterior fossa brain tumor resection population.
Design This is a retrospective regression analysis.
Setting The study conducted at a single, multihospital, urban academic medical center.
Participants A total of 283 consecutive posterior fossa brain tumor cases, excluding cerebellar pontine angle tumors, over a 6-year period (June 09, 2013–April 26, 2019) was included in this analysis.
Main Outcome Measures Outcomes studied included 90-day readmission, 90-day emergency department evaluation, 90-day return to surgery, reoperation within 90 days after index admission, reoperation throughout the entire follow-up period, mortality within 90 days, and mortality throughout the entire follow-up period. Univariate analysis was conducted for the whole population and between the lowest (Q1) and highest (Q4) socioeconomic quartiles. Stepwise regression was conducted to identify confounding variables.
Results Lower socioeconomic status was found to be correlated with increased mortality within 90 postoperative days and throughout the entire follow-up period. Similarly, analysis between the lowest and highest household income quartiles (Q1 vs. Q4) demonstrated Q4 to have significantly decreased mortality during total follow-up and a decreasing but not significant difference in 90-day mortality. No significant difference in morbidity was observed.
Conclusion This study suggests that lower household income is associated with increased mortality in both the 90-day window and total follow-up period. It is possible that there is an opportunity for health care providers to use socioeconomic status to proactively identify high-risk patients and provide additional resources in the postoperative setting.
Keywords: posterior fossa tumor, outcome disparities, socioeconomic status, readmissions
Introduction
Physicians and public health specialists are increasingly interested in the effect of social determinants of health (SDOH) on the provision of quality care in the American health care system. As defined by the World Health Organization (WHO), SDOH encompasses “the conditions in which people are born, grow, live, work, and age (which) are shaped by the distribution of money, power, and resources at global, national, and local levels.” 1 Such conditions include but are not limited to occupation, race, gender, neighborhood conditions, level of education, and income. 2 An overwhelming body of literature points to race, gender, and ethnicity among other SDOH as significant contributors to disparities in care. 3 4 5 6 7 As such, eliminating disparities in medical care has the potential to improve quality of care, while potentially decreasing cost by reducing adverse outcomes and providing a more equitable patient experience.
Disparities are reflected at multiple levels within the health care system, affecting access to care, provider of care, and outcomes of care once access has been attained. Within the realm of surgery, the effects of inequities have manifested in the form of delayed surgical intervention, 8 9 poor hospital characteristics, 3 4 10 11 12 and increased morbidity and mortality. 3 4 13 14 15 16 17 18
Unfortunately, despite clear negative impact, the processes underlying economic inequalities are poorly understood. To date, investigations into the role of economics on care have centered primarily on the issue of access to care. 19 20 21 22 23 24 Further research into the presence of disparities on outcomes “once access has been attained” is crucial for improving care protocols at the provider and hospital levels. Recently, studies in the Netherlands and Italy, where universal coverage provides a system of more equal access, show that low socioeconomic status (SES) correlates with an increased risk of poor outcome. 23 25 26 There remains a need to examine such relationships in contexts where barriers to access exist, such as the United States.
Additionally, literature on the effect of household economics in neurosurgical populations is sparse. In a previous study, the authors of the present paper demonstrated that in patients of a heterogeneous brain tumor population, low income correlated with increased mortality at short- and long-term follow-ups. 27 However, studies investigating the influence of economics on outcomes in specific neurosurgical procedures are necessary to guide practice and improve patient care. 3 28 29 To that end, the present study examines the relationship between economic background and postoperative outcomes in a cohort of patients undergoing posterior fossa tumor resection. Posterior fossa brain tumor resection is noteworthy due to the unique profile of complications that can occur in this highly sensitive region. Such complications include but are not limited to compression and posterior fossa syndrome, cranial nerve palsies, swallowing difficulty, aphasia, weakness, ataxia, brain stem distortion, cerebrospinal fluid (CSF) leak, pseudomeningocele formation, and death. Studies have demonstrated that the incidence of morbidity and mortality following posterior fossa surgery is greater than in supratentorial tumor resections. 30 As such, understanding the drivers of such complications is of paramount importance. The study employs univariate and stepwise regression to mediate confounding covariates and other SDOH which are known to impact outcomes, to better understand the effect of economic disparity after access to care has been obtained.
Methods
Sample Selection
In this institutional review board (IRB)-approved study, 283 consecutive patients undergoing posterior fossa tumor resection, excluding cerebellar pontine angle (CPA) tumors, at a multihospital, 1,659 bed university health system over 6 years (June 07, 2013–April 29, 2019) were enrolled. A waiver of informed consent was granted by the IRB as this study was considered to be of minimal risk to patients. Key data were acquired using the EpiLog tool, a nonproprietary data acquisition system created by the senior author on the present paper. 26 It was built and layered on top of the existing electronic health record (EHR) architecture to facilitate charting, workflow, quality improvement, and cost-reduction initiatives.
Data Collection
Patient and outcome data for this study were extracted from EpiLog and pushed into defined spreadsheets. Patient characteristics including median household income (MHI), age, gender, race, American Society of Anesthesiologists (ASA) score, smoking status, body mass index (BMI), Charlson's comorbidity index (CCI) and underlying covariates, duration of surgery, total surgical cost, history of prior resection, and level of education were recorded ( Table 1 ). When household income and level of education were not directly available from the EHR, data were obtained by cross referencing zip code and patient demographic characteristics with the 2012 to 2016 U.S. Census Bureau 5-year American Community report. 31 Outcomes assessed were 90-day readmission, 90-day emergency department (ED) evaluation, 90-day unanticipated return to surgery, and mortality within 90 postoperative days. Additionally, mortality and return to surgery throughout the entire follow-up period were assessed.
Table 1. Patient demographics and baseline characteristics.
| Variable | Median household income Q1 ( n = 70) | Median household income Q4 ( n = 69) | Standardized difference |
|---|---|---|---|
| Age (y) Mean (SD) |
58.16 (13.46) | 52.42 (15.76) | −0.3914 |
| Length of stay (h) Mean, (SD) |
263.49 (202.27) | 165.13 (155.85) | −0.5447 |
| Gender, n (%) | −0.217 | ||
| Female | 31 (44.29) | 38 (55.07) | |
| Male | 39 (56.31) | 32 (44.93) | |
| Total cost (USD) Mean (SD) |
2,505.44 (1,622.84) | 3,092.22 (3,278.82) | 0.2268 |
| Duration of surgery (min) Mean, (SD) |
245.22 (123.07) | 225.65 (90.26) | −0.1813 |
| CCI score Mean (SD) Myocardial infarction Congestive heart failure Peripheral vascular disease Transient ischemic attack Dementia Chronic obstructive pulmonary disorder Connective tissue disease Peptic ulcer disease liver disease Diabetes Hemiplegia Chronic kidney disease Solid tumor Leukemia Lymphoma AIDS |
5.93 (3.85) | 4.55 (3.73) | −0.3636 |
| Number of surgical intervention within 90 days prior to surgery n (%) |
0.3822 | ||
| 0 | 61 (87.14) | 67 (97.10) | |
| 1 | 8 (11.43) | 2 (2.90) | |
| 2 | 1 (1.43) | 0 (0) | |
| Number of lifetime surgical intervention prior to surgery n (%) |
0.204 | ||
| 0 | 63 (90.00) | 65 (94.20) | |
| 1 | 6 (8.57) | 4 (5.80) | |
| 2 | 1 (1.43) | 0 (0) | |
|
BMI (kg/m
2
)
Mean (SD) |
26.75 (6.80) | 26.44 (5.96) | −0.0484 |
| ASA grade n (%) |
0.3221 | ||
| 1 | 0 (0) | 0 (0) | |
| 2 | 14 (20.00) | 23 (33.33) | |
| 3 | 52 (74.29) | 44 (63.77) | |
| 4 | 4 (5.71) | 2 (2.90) | |
| Tobacco use (within past 12 months) n (%) |
0.4617 | ||
| Yes | 16 (22.86) | 5 (7.25) | |
| No | 45 (64.29) | 56 (81.16) | |
| Unknown | 9 (12.86) | 8 (11.59) | |
| Race n (%) |
1.0544 | ||
| Asian | 1 (1.43) | 6 (8.70) | |
| Black | 27 (38.57) | 2 (2.90) | |
| White | 35 (50.00) | 52 (75.36) | |
| HLB | 1 (1.43) | 0 (0) | |
| HLW | 2 (2.86) | 3 (4.35) | |
| Unknown | 1 (1.43) | 2 (2.90) | |
| Other | 3 (4.29) | 4 (5.80) |
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index; CCI, Charlson's comorbidity index; HLB, Hispanic/Latino-Black; HLW, Hispanic/Latino-White; Q1, lowest socioeconomic quartile; Q4, highest socioeconomic quartile; SD, standard deviation; USD, U.S. dollar.
Statistical Analysis
Univariate analysis was performed with respect to MHI, with significance set as p < 0.05. Patients were then divided into quartiles based on MHI, and an additional univariate analysis was conducted between the lowest (Q1) and highest (Q4) socioeconomic quartiles, with a significance set as p < 0.05. Stepwise regression was conducted to identify confounding variables.
Results
Patient Characteristics
The sample included all consecutive patients undergoing posterior fossa tumor resection, excluding CPA tumors, over the course of six calendar years ( n = 283). Four patients with missing values and one patient with a BMI less than 10 kg/m 2 were excluded from analysis. For the resulting patient cohort, mean age was 54.7 years. In this cohort, 11.5% of the studied patients used tobacco within the 12 months prior to surgery. Mean length of stay was 8.4 days and gender of the cohort was 54% female ( Fig. 1 ; Table 1 ).
Fig. 1.
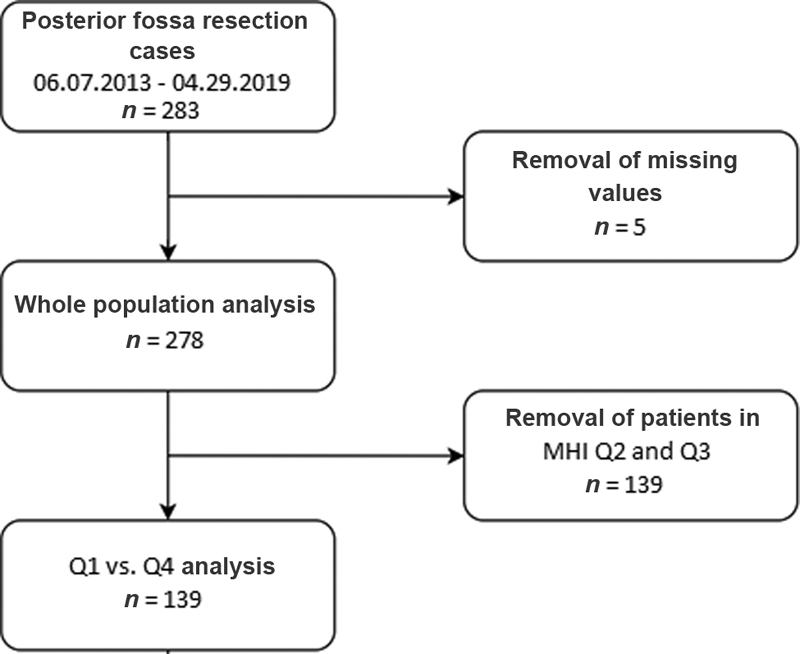
Patient selection flow-chart. MHI, median household income.
Patient Outcomes
Mortality
Whole population univariate analysis demonstrated lower SES to be correlated with increased mortality within 90 postoperative days ( p = 0.03, odds ratio [OR] = 0.65, 95% confidence interval [CI]: 0.44–0.96) and throughout the entire follow-up period ( p < 0.01, OR = 0.68, 95% CI: 0.52–0.90). Similarly, analysis between the lowest and highest socioeconomic quartiles (Q1 vs. Q4) demonstrated the highest quartile to have significantly decreased mortality during total follow-up (20.29 vs. 37.14%, p = 0.03, OR = 0.43, 95% CI: 0.20–0.92) and a decreasing but not significant difference in 90-day mortality (10.14 vs. 20.00%, p = 0.11, OR = 0.45, 95% CI: 0.17–1.12; Figs. 2 and 3; Table 2 ).
Fig. 2.
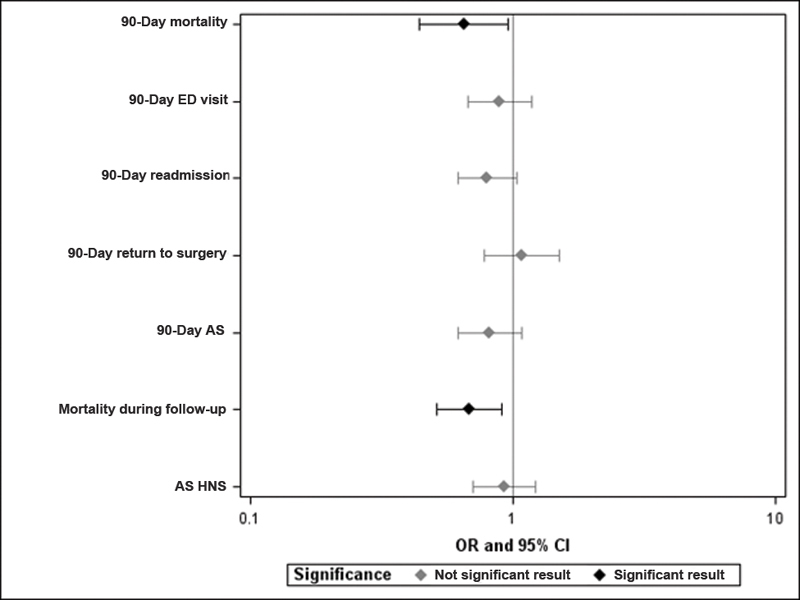
Odds ratios for adverse outcome with increasing household income. Error bars denote 95% confidence interval. CI, confidence interval; ED, emergency department; OR, odds ratio.
Fig. 3.
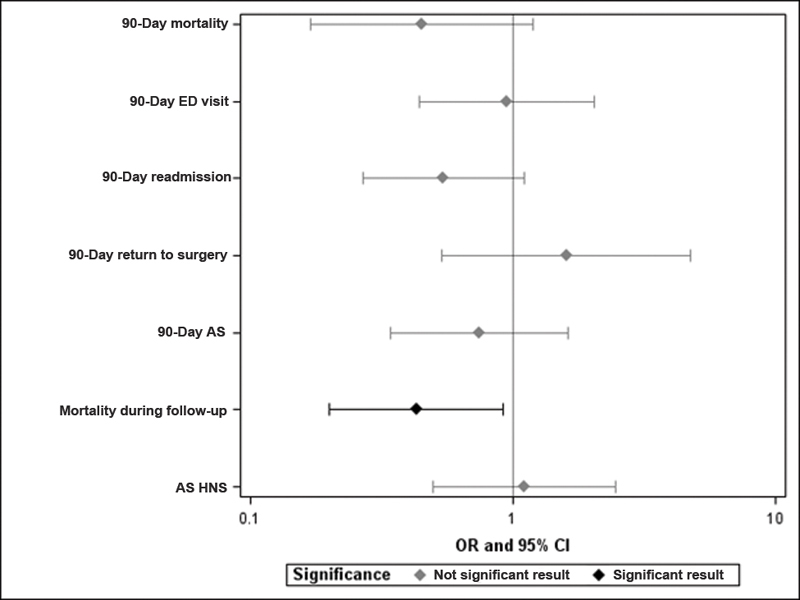
Odds ratios of adverse outcome for patients in the high household income quartile (Q4) relative to patients with in the low household income quartile (Q1). Error bars denote 95% confidence interval. CI, confidence interval; ED, emergency department; OR, odds ratio.
Table 2. Patient outcomes and complications.
| Patient groups | ||
|---|---|---|
| Outcome/complication | MHI Q4 n (%) |
MHI Q1 n (%) |
| 90-day mortality | 14 (20.00) | 7 (10.14) |
| p = 0.1048 | ||
| OR = 0.4516 (CI: 0.1701–1.1992) | ||
| Mortality during follow-up | 26 (37.14) | 14 (20.29) |
| p = 0.0282 | ||
| OR = 0.4308 (CI: 0.2012–0.9221) | ||
| 90-day readmission | 30 (42.86) | 20 (28.99) |
| p = 0.0884 | ||
| OR = 0.5442 (CI: 0.2693–1.0995) | ||
| 90-day ED evaluation | 18 (25.71) | 17 (24.64) |
| p = 0.8838 | ||
| OR = 0.9444 (CI: 0.4389–2.0321) | ||
| 90-day reoperation | 9 (13.04) | 6 (8.57) |
| p = 0.3955 | ||
| OR = 0.6250 (CI: 0.2098–1.8615) | ||
| Return to surgery during follow-up | 16 (23.19) | 15 (21.43) |
| p = 0.8032 | ||
| OR = 0.9034 (CI: 0.4063–2.0088) | ||
Abbreviations: CI, confidence interval; ED, emergency department; MHI, median household income; OR, odds ratio; Q1, lowest socioeconomic quartile; Q4, highest socioeconomic quartile.
Morbidity
In the whole population univariate analysis, no significant difference was found with regards to 90-day readmission ( p = 0.08, OR = 0.80, 95% CI: 0.62–1.03), 90-day ED evaluation ( p = 0.42, OR = 0.89, 95% CI: 0.67–1.18), 90-day return to surgery ( p = 0.64, OR = 1.08, 95% CI: 0.78–1.51), or return to surgery throughout the entire follow-up period ( p = 0.60, OR = 0.93, 95% CI: 0.71–1.22). Similarly, no significant differences were found between Q1 and Q4 quartiles in 90-day readmission (28.99 vs. 42.86%, p = 0.08, OR = 0.54, 95% CI:0.27–1.10), 90-day ED evaluation (24.64 vs. 25.71%, p = 0.88, OR = 0.94, 95% CI:0.44–2.03), 90-day return to surgery (8.57 vs. 13.04%, p = 0.40, OR = 0.63, 95% CI:0.21–1.86), or return to surgery throughout the entire follow-up period (21.43 vs. 23.19%, p = 0.80, OR = 0.90, 95% CI:0.41–2.01).
Stepwise Regression
The 90-day readmission and ED evaluation are significantly predicted by history of surgery within prior 90 days. Return to surgery within 90 days is associated with duration of surgery, BMI, and ASA grade. Mortality within 90 days is associated with duration of surgery and ASA grade. Mortality during the entire follow-up period is associated with CCI score, history of surgery within prior 90 days, total cost, and ASA grade. Return to surgery throughout the entire follow-up period is associated with duration of surgery.
Discussion
The posterior fossa, home to critical structures, such as the brainstem, cerebellum, and cranial nerves, is highly sensitive to manipulation and compression. As such, surgical interventions carry high risks for complications leading to significant morbidity and mortality. 32 Intra- and postoperative complications include hematoma, cerebral edema, posterior fossa syndrome, cranial nerve palsies, respiratory distress, pseudomeningocele formation, and hydrocephalus necessitating CSF diversion, among others. 33 Furthermore, Cochrane et al reported aggravated deficits in 41% of children presenting with worsening ataxia, cranial nerve palsies, mutism, apnea, and seizures. 33 Similarly, adults undergoing posterior fossa tumor surgery are at risk for damage to the brain stem, cerebellum, and cranial nerves housed in the compartment, leading to significant morbidity and mortality. 30 32 As such, identification and elimination of factors that contribute to adverse outcomes is paramount to improving quality of care for patients undergoing posterior fossa tumor resection.
This study sought to investigate the influence of household income on mid- and long-term outcomes in the posterior fossa tumor population. Univariate analysis of 278 consecutive patients demonstrated significantly increased risk of mortality within 90 days and during the entire follow-up period for patients of lower SES. Further, univariate analysis between the lowest and highest socioeconomic quartiles demonstrated greater risk of mortality during total follow-up for the lowest quartile. No significant difference in morbidity was found.
The findings presented in this study suggest a significant imperative to address socioeconomic disparities in neurosurgical care. It is unique in that it evaluates the role of SES after care has been established. Notably, long-term mortality was found to be significantly associated with patient comorbidities; however, a significant difference in mortality remained after comorbidities were controlled for. Furthermore, comorbidities were not found to be associated with a difference in 90-day mortality. These results suggest that, after controlling for the effect of patient characteristics, disparity may be driven by distinct socioeconomic barriers to care. Such barriers include difficulty, making it to follow-up appointments due to employment status or lack of transportation and lack of in-home postoperative assistance among other factors. 34
While population-level interventions are beyond the scope of surgical practice, there are many provider- and hospital-level interventions which may improve prognosis following surgery for the most vulnerable group of patients. To date, several health systems have experimented with programs to target high-risk patients with additional resources following surgery to facilitate the recovery process and enable effective follow-up. 35 36 37 With increased focus on value-based medicine, SES may serve as a powerful metric for predicting adverse outcomes, responding proactively, and eliminating avoidable complications.
This study contributes to the growing body of literature on the influence of SES on outcomes while mediating for confounding covariates. This is particularly important when studying SDOH, given the complex interactions between various factors. The covariates investigated in this study were based on supporting literature indicating the relationship between each characteristic and patient outcome. Smoking status, BMI, and CCI score have been shown to independently predict morbidity following surgery in numerous studies. 38 39 40 41 42 Furthermore, duration of surgery has been shown to correlate with greater risk of complications. 43 44 In a study by Dial et al, ASA score was associated with increased length of stay and 90-day readmission. 45 Similarly, the impact of race on postoperative outcomes is largely detailed in the literature. 15 16 46 47 48
Limitations
There are several limitations to this study. One limitation is that this study is retrospective, therefore potential sampling bias and data recording inaccuracies may exist. Furthermore, the study assesses for readmissions and ED evaluation based on EHR data from the university hospital system in which the study was conducted, assuming that this system would be the recipient of all such events. As such, there is a potential for underreporting of true readmission and ED evaluation rates. Nonetheless, this would likely be consistent across patients of multiple income-levels and therefore should not significantly affect the internal validity of the study. Further, all patients are queried during postoperative visits as to visits with other health care providers and events, with an average follow-up time of 619 days, which would capture the relevant endpoints. Second, as with all retrospective studies, the influence of each covariate could not be completely controlled for despite being incorporated into the model by stepwise regression. Notably, mortality during the entire follow-up period is associated with CCI score, history of surgery within 90 days prior to the index intervention, total cost, and ASA grade. Furthermore, mortality within 90 postoperative days is associated with duration of surgery and ASA grade. Future studies prospectively analyzing these outcomes in a larger, matched population is required to further validate our findings and rule out potential confounding variables.
Further research should seek to investigate the underlying mechanisms of the effect of SES on outcomes, to more accurately target patients with efficient interventions to improve patient outcomes in the postoperative period. Moreover, expanding on the present findings in other procedure types is necessary to guide changes in a large scale, heterogeneous neurosurgery practice.
Conclusion
The present study responds to the growing interest among providers and population health experts in understanding the role of socioeconomics in medical and surgical care. The results demonstrate that SES significantly predicts risk of mortality in the 90-day postoperative window and throughout the entire follow-up period following posterior fossa tumor resection. The findings suggest that mitigating for disparities in SES may be an important avenue for reducing complications and improving outcomes in a neurosurgical setting. Additionally, the study emphasizes the need to further investigate the forces, other than access, which drive socioeconomic disparities in outcomes and calls for effective interventions to support vulnerable patients following surgery.
Footnotes
Conflict of Interest None declared.
References
- 1.Marmot M, Friel S, Bell R, Houweling T A, Taylor S.Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health Lancet 2008372(9650):1661–1669. [DOI] [PubMed] [Google Scholar]
- 2.Catalyst N.Social determinants of health (SDOH). NEJM Catal 2017. Accessed November 16, 2019 at:https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0312
- 3.Curry W T, Jr., Carter B S, Barker F G., IIRacial, ethnic, and socioeconomic disparities in patient outcomes after craniotomy for tumor in adult patients in the United States, 1988-2004 Neurosurgery 20106603427–437., discussion 437–438 [DOI] [PubMed] [Google Scholar]
- 4.Haider A H, Scott V K, Rehman K A. Racial disparities in surgical care and outcomes in the United States: a comprehensive review of patient, provider, and systemic factors. J Am Coll Surg. 2013;216(03):482–9.2E13. doi: 10.1016/j.jamcollsurg.2012.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bowman K, Telem D A, Hernandez-Rosa J, Stein N, Williams R, Divino C M. Impact of race and socioeconomic status on presentation and management of ventral hernias. Arch Surg. 2010;145(08):776–780. doi: 10.1001/archsurg.2010.141. [DOI] [PubMed] [Google Scholar]
- 6.Hofmann L J, Lee S, Waddell B, Davis K G. Effect of race on colon cancer treatment and outcomes in the department of defense healthcare system. Dis Colon Rectum. 2010;53(01):9–15. doi: 10.1007/DCR.0b013e3181bdcdb2. [DOI] [PubMed] [Google Scholar]
- 7.Schoenfeld A J, Sieg R N, Li G, Bader J O, Belmont P J, Jr., Bono C M. Outcomes after spine surgery among racial/ethnic minorities: a meta-analysis of the literature. Spine J. 2011;11(05):381–388. doi: 10.1016/j.spinee.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Lee S L, Shekherdimian S, Chiu V Y, Sydorak R M. Perforated appendicitis in children: equal access to care eliminates racial and socioeconomic disparities. J Pediatr Surg. 2010;45(06):1203–1207. doi: 10.1016/j.jpedsurg.2010.02.089. [DOI] [PubMed] [Google Scholar]
- 9.Meagher A D, Beadles C A, Doorey J, Charles A G. Racial and ethnic disparities in discharge to rehabilitation following traumatic brain injury. J Neurosurg. 2015;122(03):595–601. doi: 10.3171/2014.10.JNS14187. [DOI] [PubMed] [Google Scholar]
- 10.Lucas F L, Stukel T A, Morris A M, Siewers A E, Birkmeyer J D. Race and surgical mortality in the United States. Ann Surg. 2006;243(02):281–286. doi: 10.1097/01.sla.0000197560.92456.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nathan H, Frederick W, Choti M A, Schulick R D, Pawlik T M. Racial disparity in surgical mortality after major hepatectomy. J Am Coll Surg. 2008;207(03):312–319. doi: 10.1016/j.jamcollsurg.2008.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breslin T M, Morris A M, Gu N. Hospital factors and racial disparities in mortality after surgery for breast and colon cancer. J Clin Oncol. 2009;27(24):3945–3950. doi: 10.1200/JCO.2008.20.8546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoover E L. There is no scientific rationale for race-based research. J Natl Med Assoc. 2007;99(06):690–692. [PMC free article] [PubMed] [Google Scholar]
- 14.Kim D H, Daskalakis C, Lee A N. Racial disparity in the relationship between hospital volume and mortality among patients undergoing coronary artery bypass grafting. Ann Surg. 2008;248(05):886–892. doi: 10.1097/SLA.0b013e318189b1bc. [DOI] [PubMed] [Google Scholar]
- 15.Lemaire A, Cook C, Tackett S, Mendes D M, Shortell C K. The impact of race and insurance type on the outcome of endovascular abdominal aortic aneurysm (AAA) repair. J Vasc Surg. 2008;47(06):1172–1180. doi: 10.1016/j.jvs.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 16.Alosh H, Riley L H, III, Skolasky R L. Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality: an examination of United States trends from 1992 to 2005. Spine. 2009;34(18):1956–1962. doi: 10.1097/BRS.0b013e3181ab930e. [DOI] [PubMed] [Google Scholar]
- 17.Kim J, Artinyan A, Mailey B. An interaction of race and ethnicity with socioeconomic status in rectal cancer outcomes. Ann Surg. 2011;253(04):647–654. doi: 10.1097/SLA.0b013e3182111102. [DOI] [PubMed] [Google Scholar]
- 18.Bennett K M, Scarborough J E, Pappas T N, Kepler T B.Patient socioeconomic status is an independent predictor of operative mortality Ann Surg 201025203552–557., discussion 557–558 [DOI] [PubMed] [Google Scholar]
- 19.Rubinger L, Chan C, Andrade D. Socioeconomic status influences time to surgery and surgical outcome in pediatric epilepsy surgery. Epilepsy Behav. 2016;55:133–138. doi: 10.1016/j.yebeh.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 20.Lapar D J, Bhamidipati C M, Walters D M. Primary payer status affects outcomes for cardiac valve operations. J Am Coll Surg. 2011;212(05):759–767. doi: 10.1016/j.jamcollsurg.2010.12.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Du X L, Liu C-C. Racial/Ethnic disparities in socioeconomic status, diagnosis, treatment and survival among medicare-insured men and women with head and neck cancer. J Health Care Poor Underserved. 2010;21(03):913–930. doi: 10.1353/hpu.0.0331. [DOI] [PubMed] [Google Scholar]
- 22.Manuel J I. Racial/ethnic and gender disparities in health care use and access. Health Serv Res. 2018;53(03):1407–1429. doi: 10.1111/1475-6773.12705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barone A P, Fusco D, Colais P. Effects of socioeconomic position on 30-day mortality and wait for surgery after hip fracture. Int J Qual Health Care. 2009;21(06):379–386. doi: 10.1093/intqhc/mzp046. [DOI] [PubMed] [Google Scholar]
- 24.Birkmeyer N J, Gu N, Baser O, Morris A M, Birkmeyer J D. Socioeconomic status and surgical mortality in the elderly. Med Care. 2008;46(09):893–899. doi: 10.1097/MLR.0b013e31817925b0. [DOI] [PubMed] [Google Scholar]
- 25.Agabiti N, Cesaroni G, Picciotto S et al. The association of socioeconomic disadvantage with postoperative complications after major elective cardiovascular surgery. J Epidemiol Community Health. 2008;62(10):882–889. doi: 10.1136/jech.2007.067470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ultee K HJ, Tjeertes E KM, Bastos Gonçalves F. The relation between household income and surgical outcome in the Dutch setting of equal access to and provision of healthcare. PLoS One. 2018;13(01):e0191464. doi: 10.1371/journal.pone.0191464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glauser G, Dimentberg R, Shultz K, McClintock S D, Malhotra N R.Survival disparity based on household income in 1,970 patients following brain cancer surgery World Neurosurg 2020(e-pub ahead of print) 10.1016/j.wneu.2020.07.016 [DOI] [PubMed] [Google Scholar]
- 28.Pollom E L, Fujimoto D K, Han S S, Harris J P, Tharin S A, Soltys S G. Newly diagnosed glioblastoma: adverse socioeconomic factors correlate with delay in radiotherapy initiation and worse overall survival. J Radiat Res (Tokyo) 2018;59 01:i11–i18. doi: 10.1093/jrr/rrx103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shin J Y, Yoon J K, Diaz A Z. Influence of insurance status and income in anaplastic astrocytoma: an analysis of 4325 patients. J Neurooncol. 2017;132(01):89–98. doi: 10.1007/s11060-016-2339-y. [DOI] [PubMed] [Google Scholar]
- 30.Dubey A, Sung W-S, Shaya M. Complications of posterior cranial fossa surgery--an institutional experience of 500 patients. Surg Neurol. 2009;72(04):369–375. doi: 10.1016/j.surneu.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Census Bureau. B19013 median household income in the past 12 months (in 2016 inflation-adjusted dollars): American Community Survey Tables: 2012 -- 2016 (5-Year Estimates) (ACS16_5yr). Accessed July 14, 2020 at:https://www.socialexplorer.com/data/ACS2016_5yr/metadata/?ds=ACS16_5yr&table=B19013H
- 32.Goodrich J T. New York, NY: Springer; 2015. History of posterior fossa tumor surgery; pp. 3–60. [Google Scholar]
- 33.Cochrane D D, Gustavsson B, Poskitt K P, Steinbok P, Kestle J R. The surgical and natural morbidity of aggressive resection for posterior fossa tumors in childhood. Pediatr Neurosurg. 1994;20(01):19–29. doi: 10.1159/000120761. [DOI] [PubMed] [Google Scholar]
- 34.Billings J, Zeitel L, Lukomnik J, Carey T S, Blank A E, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12(01):162–173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 35.Silow-Carroll S, Edwards J N, Lashbrook A.Reducing hospital readmissions: lessons from top-performing hospitalsAccessed July 14, 2020 at:https://www.commonwealthfund.org/publications/case-study/2011/apr/reducing-hospital-readmissions-lessons-top-performing-hospitals
- 36.Ryan J G, Fedders M, Jennings T, Vittoria I, Yanes M. Clinical outcomes and incremental costs from a medication adherence pilot intervention targeting low-income patients with diabetes at risk of cost-related medication nonadherence. Clin Ther. 2014;36(12):1991–2002. doi: 10.1016/j.clinthera.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 37.Feinberg A T, Hess A, Passaretti M, Coolbaugh S, Lee T H.Prescribing food as a specialty drug. NEJM Catal 20184(02. Accessed November 18, 2020 at:https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0212
- 38.Turan A, Mascha E J, Roberman D. Smoking and perioperative outcomes. Anesthesiology. 2011;114(04):837–846. doi: 10.1097/ALN.0b013e318210f560. [DOI] [PubMed] [Google Scholar]
- 39.Grossman R, Mukherjee D, Chang D C. Preoperative charlson comorbidity score predicts postoperative outcomes among older intracranial meningioma patients. World Neurosurg. 2011;75(02):279–285. doi: 10.1016/j.wneu.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 40.Rueth N M, Parsons H M, Habermann E B. Surgical treatment of lung cancer: predicting postoperative morbidity in the elderly population. J Thorac Cardiovasc Surg. 2012;143(06):1314–1323. doi: 10.1016/j.jtcvs.2011.09.072. [DOI] [PubMed] [Google Scholar]
- 41.Smits A, Lopes A, Das N. Surgical morbidity and clinical outcomes in ovarian cancer - the role of obesity. BJOG. 2016;123(02):300–308. doi: 10.1111/1471-0528.13585. [DOI] [PubMed] [Google Scholar]
- 42.Wilson J R, Tetreault L A, Schroeder G. Impact of elevated body mass index and obesity on long-term surgical outcomes for patients with degenerative cervical myelopathy: analysis of a combined prospective dataset. Spine. 2017;42(03):195–201. doi: 10.1097/BRS.0000000000001859. [DOI] [PubMed] [Google Scholar]
- 43.Chu D, Bakaeen F G, Wang X L, LeMaire S A, Coselli J S, Huh J. Does the duration of surgery affect outcomes in patients undergoing coronary artery bypass grafting? Am J Surg. 2008;196(05):652–656. doi: 10.1016/j.amjsurg.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 44.Kim J Y, Khavanin N, Rambachan A. Surgical duration and risk of venous thromboembolism. JAMA Surg. 2015;150(02):110–117. doi: 10.1001/jamasurg.2014.1841. [DOI] [PubMed] [Google Scholar]
- 45.Dial B L, Esposito V R, Danilkowicz R. Factors associated with extended length of stay and 90-day readmission rates following ACDF. Global Spine J. 2020;10(03):252–260. doi: 10.1177/2192568219843111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.LaPar D J, Bhamidipati C M, Harris D A. Gender, race, and socioeconomic status affects outcomes after lung cancer resections in the United States. Ann Thorac Surg. 2011;92(02):434–439. doi: 10.1016/j.athoracsur.2011.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martsolf G R, Barrett M L, Weiss A J. Impact of race/ethnicity and socioeconomic status on risk-adjusted hospital readmission rates following hip and knee arthroplasty. J Bone Joint Surg Am. 2016;98(16):1385–1391. doi: 10.2106/JBJS.15.00884. [DOI] [PubMed] [Google Scholar]
- 48.Seicean A, Seicean S, Neuhauser D, Benzel E C, Weil R J. The influence of race on short-term outcomes after laminectomy and/or fusion spine surgery. Spine. 2017;42(01):34–41. doi: 10.1097/BRS.0000000000001657. [DOI] [PubMed] [Google Scholar]


