Abstract
The disruptions of the coronavirus pandemic have enabled new opportunities for telehealth expansion within movement disorders. However, inadequate internet infrastructure has, unfortunately, led to fragmented implementation and may worsen disparities in some areas. In this Correspondence, we report on geographic and racial/ethnic disparities in access to our center's comprehensive care clinic for people with Parkinson's disease. While both in-person and virtual versions of the clinic enjoyed high patient satisfaction, we discovered that participation by Black/African-American individuals was cut in half when we shifted to a virtual delivery format in April 2020. We outline potential barriers in access using a socio-ecological model.
Keywords: Parkinson disease, Telehealth, Health disparities, Access to care, Interdisciplinary care
Telemedicine in movement disorders can increase access to subspecialty care, monitor patient symptoms and treatment response, and provide family support in times of crisis [1]. Catalyzed by the coronavirus pandemic, the use of both synchronous and asynchronous forms of telemedicine has expanded in the last two years [2]. While virtual visits allowed many people with Parkinson disease (PwP) to remain connected with their healthcare teams, the rapid deployment of a virtual care as a result of the pandemic, and the lack of supporting infrastructure, may worsen existing disparities in access to care [3,4]. Here, we report on our center's experience with telemedicine implementation of a comprehensive interdisciplinary clinic for PwP, including unexpected benefits and challenges in access.
The Duke Movement Disorders Center is a designated Parkinson's Foundation Center of Excellence, located in central North Carolina, with a catchment area spanning the entire state and an annual PwP panel of about 2000 individuals across six fellowship-trained movement disorders neurologists. In July 2019, we implemented an interdisciplinary clinic for PwP. Participants undergo standardized evaluations by physical, occupational, and speech therapists who specialize in the care of PwP, a social worker, and a clinical pharmacist. Following an interdisciplinary team meeting, the patient and care partner (if present) meet with their movement disorders neurologist to review assessments and devise a comprehensive treatment plan. We conducted the clinic in person from July 2019–March 2020. After a brief pause to reorganize in response to the pandemic, we re-opened the clinic in virtual format from April 2020–July 2021, with scheduling flexibility over an assigned week to minimize screen fatigue for participants.
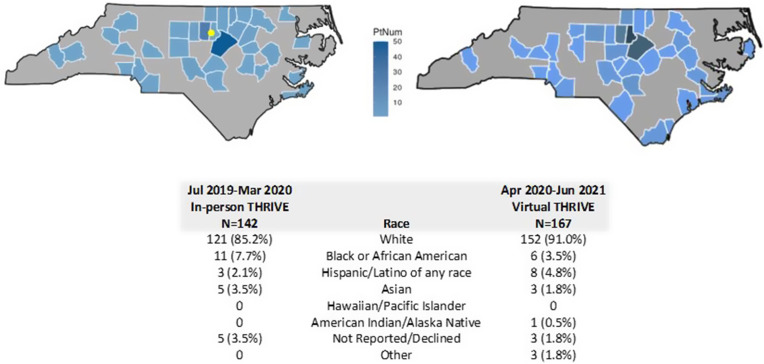
As demonstrated in Fig. 1 , the geographic and racial/ethnic mixture of patients seen in the clinic changed after the shift to a virtual model. Prior to the pandemic, approximately half of patients seen in the comprehensive clinic were located within a 1-h drive from our Center. The most common reason for late cancellation was the 6-h appointment duration, which necessitated PwP living farther away to arrive the night before and stay locally. While virtual implementation expanded geographic reach, it also unmasked significant loss of access for Black PwP (7.7% in-person vs 3.5% virtually; Z = −1.6, p = 0.05). Changes in visits for other racial/ethnic groups were not statistically significant. The most common reason for late cancellation for the virtual comprehensive clinic was cost of care and/or lack of insurance coverage for telehealth services by physical, occupational, or speech therapy. Analysis of these barriers and other outcomes is underway, including patient-reported Self-Efficacy for Management of Chronic Disease [5], health utilization, and documented adherence to quality metrics for PwP.
Fig. 1.
Home locations and racial/ethnic features of PwP seen in the comprehensive care clinic at Duke Movement Disorders Center, in-person (left) and virtual (right). Clinic location marked with yellow dot. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Sociodemographic disparities in telemedicine access exist across multiple specialties [3]; possible explanations range from individual factors such as lack of familiarity with online technology to community or policy factors including fragmented insurance coverage for telehealth services or limited internet infrastructure in rural areas. Overcoming these barriers will require not only creative thought on the part of individual clinicians but also structural changes in the practice of movement disorders in the United States. This letter describes our single center's experience; comparative data from other regions or countries will be helpful in evaluating the impact of different strategies to bridge the digital divide. For instance, asynchronous “store-and-forward” assessments can lessen the need for high-bandwidth two-way streaming video services. Alternatively, a “hub-and-spoke” model, wherein patients travel to a local health center or community space for a consultation with a remotely-located specialist, could provide patients with additional, on-the-ground technical support [4] as well as promote academic-community partnerships. These partnerships could further ensure that specialist recommendations are able to be implemented at the local level.
These models, and others, will require a reconsideration of how we define, deliver, and fund healthcare in the 21st century. Telemedicine carries great promise for the care of PwP, but as our and others’ experience demonstrates, we must ensure that expanded access does not leave behind vulnerable patients.
Author roles
SM: 1B, 1C, 2A, 2B, 2C, 3A, 3BKM: 1A, 1B, 1C, 2C, 3B.
Funding
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002553. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Ethical compliance statement
This study was approved by the Duke University Institutional Review Board (Pro00105281). Written consent was obtained from all participants prior to research activities. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Declaration of competing interest
SM receives research support from the Michael J Fox Foundation (MJFF) and Cerevel Therapeutics, is a paid consultant to Deep Brain Innovations, LLC, is a study site investigator for a study sponsored by Neuraly Rho, and is a study site sub-investigator for a study sponsored by Biogen.
KM will be serving as a site principal investigator for a Medtronic sponsored clinical trial and currently is PI on a trial sponsored by Deep Brain Innovations. He has consulted for Boston Scientific.
References
- 1.Spear K.L., Auinger P., Simone R., Dorsey E.R., Francis J. Patient views on telemedicine for Parkinson disease. J. Parkinsons Dis. 2019;9:401–404. doi: 10.3233/JPD-181557. [DOI] [PubMed] [Google Scholar]
- 2.Hassan A., Mari Z., Gatto E.M., Cardozo A., Youn J., Okubadejo N., Bajwa J.A., Shalash A., Fujioka S., Aldaajani Z., Cubo E. International telemedicine study group, global survey on telemedicine utilization for movement disorders during the COVID-19 pandemic. Mov. Disord. 2020;35:1701–1711. doi: 10.1002/mds.28284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ortega G., Rodriguez J.A., Maurer L.R., Witt E.E., Perez N., Reich A., Bates D.W. Telemedicine, COVID-19, and disparities: policy implications. Health Pol. Technol. 2020;9:368–371. doi: 10.1016/j.hlpt.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dorsey E.R. The new platforms of health care. NPJ Digit Med. 2021;4:112. doi: 10.1038/s41746-021-00478-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ritter P.L., Lorig K. The English and Spanish Self-Efficacy to Manage Chronic Disease Scale measures were validated using multiple studies. J. Clin. Epidemiol. 2014;67:1265–1273. doi: 10.1016/j.jclinepi.2014.06.009. [DOI] [PubMed] [Google Scholar]