Abstract
Purpose
Triceps tendon avulsion (TTA) is an uncommon injury, and there are no classifications or treatment guidelines available. This study aims to describe a clinicoradiological classification and treatment algorithm for traumatic TTA in adults. The functional outcome of surgical repair has been evaluated too.
Methods
A retrospective analysis of adult patients with traumatic TTA treated in our institution between January 2012 and December 2017 was done. We only included complete TTA injuries. Children below 15 years, with open injuries, associated fractures, or partial TTA were excluded. The data were obtained from hospital records. The intraoperative findings were correlated with the clinicoradiological presentation for classifying TTA. The functional outcome was analyzed using the Mayo Elbow Performance index and Hospital for Special Surgery elbow score. ANOVA test was used to assess the statistical significance.
Results
There were 15 patients included, 11 males and 4 females. The mean age was (31.5 ± 9.15) years, and the mean follow-up was (22.4 ± 8.4) months. Fall on outstretched hand was the mode of injury. In 6 patients, diagnosis was missed on the initial visit. TTA were classified as Type I: palpable soft-tissue defect without bony mass; Type II: palpable soft-tissue defect with a wafer-thin/comminuted bony fragment on X-ray; Type III: palpable soft-tissue defect with a bony mass and a large bony fragment on X-ray without extension to the articular surface; and Type IV: an olecranon fracture with less than 25% of the articular surface. An algorithm for treatment was recommended, i.e. transosseous suture repair/suture anchor for Type I, transosseous suture repair for Type II, and tension band wiring or steel wire sutures for Types III and IV. All the patients achieved good to excellent outcome: the mean Mayo Elbow Performance index was 100 and Hospital for Special Surgery score was 98.26 ± 2.60 on final follow-up.
Conclusion
Our clinicoradiological classification and treatment algorithm for TTAs is simple. Surgical treatment results in excellent functions of the elbow. Since it is a single-center study involving a very small number of cases, a multicenter study with a larger number of patients is required for external validation of our classification and treatment recommendations.
Keywords: Wounds and injuries, Triceps tendon avulsion, Injuries around elbow, Classification of triceps avulsion, Treatment algorithm
Introduction
Isolated traumatic triceps tendon avulsion (TTA) is the least reported among all the tendon injuries in the literature.1 Triceps avulsions are often high energy injuries. The mechanism of injury is either by a direct blow to the posterior elbow or indirectly by a violent contraction of the triceps tendon. Contraction of the tendon against flexion is common in fall injuries on the outstretched hand.2 Comorbid conditions like diabetes, enthesopathy, calcific tendinitis, chronic renal insufficiency, rheumatoid arthritis, systemic lupus erythematosus, Marfan's syndrome, osteogenesis imperfecta, local steroid injection, and hyperparathyroidism predispose this injury.2,3 Local steroid injections are a risk factor.4
TTA can be partial or complete and can occur at various anatomical levels. This injury is often associated with bony avulsion of the olecranon and sometimes poses a diagnostic challenge because of the innocuous presentation in partial ruptures.5 An intact lateral expansion and a functional anconeus can result in preserved active elbow extension. Patients present with painful active elbow extension after TTA injury. Local tenderness at the tip of the olecranon and a palpable gap over the triceps tendon are the common clinical signs.6 The flake sign in X-ray films is pathognomic. It is the avulsed footprint from the olecranon.5, 6, 7 Pure intra-substance ruptures of the tendon are more difficult to diagnose and often require an ultrasound scan or MRI for confirmation.6, 7, 8
There are no definitive treatment guidelines for the management of TTA. Partial triceps tendon tears can be managed either conservatively or surgically. Complete ruptures need surgical management.8 Surgical repair of the avulsed tendon has proven to give universally good results irrespective of the technique. Methods used for repair are tension band wiring, transosseous suture repair, and suture anchor technique. There is no consensus among surgeons on the best method of repair.5,8 The treatment decision, in a majority of reported literature, was made after the radiological confirmation of a complete injury by MRI.
Classifications are useful for disease characterization, communication, treatment design, and research purposes. A good classification needs to be simple, easy to identify, and having very low inter or intraobserver variability. To the best of our knowledge, there are no reliable clinicoradiological methods in the diagnosis and treatment of traumatic TTA. This may be due to the rarity of this injury. There is a lack of consensus regarding the surgical methods of repair used. The available literature includes several isolated reports and case series without a proper recommendation. Our objective is to retrospectively analyze the clinical and radiological profile of adult patients with traumatic TTA and to describe a clinicoradiological classification for this injury, and further propose a treatment algorithm based on our classification. We think this will allow uniformity in the assessment and management of this rare entity. We also want to share the functional outcome of our patients.
Methods
After obtaining the institutional research committee approval we conducted this retrospective cohort study on patients with TTAs between 2012 and 2017. A case of traumatic TTA was defined as a patient having pain, swelling, and tenderness locally with a palpable defect in the triceps tendon with or without a palpable bony mass after an injury. An active extension of the elbow was not possible against gravity. The diagnosis was made based on clinical and radiological findings (X-ray or ultrasound scan). An X-ray may show a detached bony mass in the lateral view. An ultrasound scan demonstrates a tear in the tendon. In doubtful cases, MRI was done for confirmation. A minimum of 6 months follow-up was necessary for inclusion. Patients with open injuries, prior injuries around the elbow, associated fractures around the elbow, and children below the age of 15 years were excluded. Those patients with partial injury of tendon were also excluded.
All procedures were done after obtaining informed consent. Antibiotic prophylaxis using 1 g cefuroxime was given 30 min before surgery. The antibiotic was continued for 24 h after surgery. The patient was positioned in the lateral decubitus position. The procedure was done under a supraclavicular block. No tourniquet was used. A 10 cm posterior incision was made. The ruptured portion of the triceps tendon was identified. It was dissected free of paratendinous tissues to reduce tension during the repair. The technique used for repair is based on preoperative planning and intraoperative findings. The repair was done in the extended position of the elbow joint. The whole procedure was completed within 1 h.
After the procedure, all patients were given a long arm slab until suture removal. Active flexion exercises and passive extension exercises were started after the removal of the slab. The elbow was protected in an arm pouch. Complete flexion was obtained by 6 weeks. Regular unprotected activities were allowed after 12 weeks. The patients who underwent tension band wiring/stainless steel suture underwent implant removal at one-year follow-up.
The intraoperative finding was retrospectively correlated with the clinicoradiological presentation. The details and the contact numbers of the patients were retrieved from the prospectively maintained hospital database and the treatment and follow-up notes were reviewed. The functional outcome was analyzed using validated scores such as the Mayo Elbow Performance index and Hospital for Special Surgery (HSS) elbow score.3,9 Statistical analysis was done using ANOVA test to find out any significant difference of mean score among different types of TTA.
Results
A total of 18 cases of TTA were identified. One case was excluded because it was following a cut injury. Two cases of partial injury with the patients able to extend the elbow against gravity were also excluded. Finally, 15 patients met the inclusion criteria (Appendix 1).
There were 11 males and 4 females. The mean age was (31.5 ± 9.15) years (17–52 years). The mode of injury was an indirect injury: all patients sustained the TTA due to fall on an outstretched hand. In 9 patients diagnosis was made on the first visit. In the other 6 patients, the diagnosis was missed at the first visit and later confirmed within a week. The dominant upper limb was involved in 80% of cases. Two patients had pure tendinous avulsion, which was diagnosed by ultrasound scan and confirmed by MRI (Fig. 1A). In 11 patients diagnosis was confirmed only with X-rays (Fig. 1B–D).
Fig. 1.
Radiological findings in patients with triceps tendon injury. (A) Type I injury--MRI scan showing triceps tendon footprint avulsion (arrow) without bony involvement; (B) Type II injury – an X-ray image showing wafer-thin bony fragment (arrow); (C) Type II injury showing comminuted bone fragments (arrow); (D) Type III injury – a single large bony fragment without articular extension (arrow).
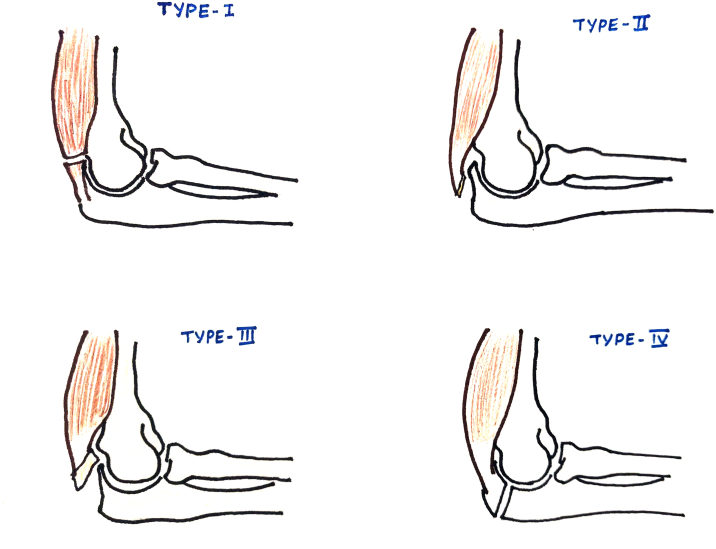
Patients were followed up to an average period of (22.4 ± 8.2) months. Based on the clinical features and radiological findings, a clinicoradiological classification of traumatic TTA was made. The salient features of each type and the number of patients in each group are shown in Table 1 and Fig. 2.
Table 1.
Clinicoradiological classification of total triceps tendon avulsion, proposed treatment method, and the number of patients in each type.
| Classification of triceps tendon avulsions | Clinico radiological presentation | Proposed treatment method | No. of patients |
|---|---|---|---|
| Type I |
|
Transosseous suture repair/suture anchor | 4 |
| Type II |
|
Transosseous suture repair | 7 |
| Type III |
|
Tension band wiring | 4 |
| Type IV |
|
Tension band wiring/plating | 0 |
Fig. 2.
Sketch of triceps tendon avulsion classification.
The intraoperative findings correlated with the preoperative clinicoradiological features were used for the classification of the injury. In 4 cases a very few fibers of the triceps tendon were still inserted onto the olecranon with no bony injury. An ultrasound scan or MRI scan is required for confirmation of diagnosis. The 4 cases were included in clinicoradiological Type I (Fig. 3A). In 2 of them, the repair was done using No. 2 Fiber Wire® (Arthrex) in the form of a Krakow stitch tied through a transverse tunnel drilled in the olecranon (Fig. 3B). The remaining 2 were repaired by utilizing the Krakow stitch secured to 2.5 mm titanium suture anchors (2 in numbers) inserted at the footprint (Fig. 4).
Fig. 3.
(A) Intraoperative photograph showing Type I triceps tendon avulsion without bony injury; (B) Intraoperative photograph demonstrating transosseous tunnel repair.
Fig. 4.
Postoperative radiograph showing triceps avulsion injury repaired by suture anchor technique.
There were 7 patients with Type II injury. Among them, 2 had a complete avulsion of the tendon with a wafer-thin bone attached to it. One patient had complete avulsion with comminuted bony fragments noted intraoperatively. The other 5 patients had partial avulsion with wafer-thin bony fragments noted intraoperatively. For all the Type II patients (7/15), the avulsed fragment was deemed too weak to support tension band fixation, and repair was done by using the similar technique described earlier using fiber wire. The ends of the suture were pulled through a transverse bone tunnel in the olecranon and tied with the elbow in extension.
The remaining 4 patients belonged to Type III. They had a complete tear with a large single bony defect noted intraoperatively, not extending to the articular surface. Due to the large avulsed bone fragment, fixation was done by a routine tension band fixation using K-wires and 18 gauge stainless steel wire (Fig. 5). However, removal of the implants at a second sitting was required, compared to other techniques that do not necessitate implant removal.
Fig. 5.
Postoperative radiograph showing a Type III triceps tendon avulsion treated by a tension band fixation using K-wires and 18 gauge stainless steel wire.
A Type IV variety is also possible even though we do not have any such case in our group. It is an avulsion fracture of the olecranon with less than 25% involvement of the articular area. In a true sense, it is not an avulsion injury of the triceps tendon as there is articular surface involvement.
The Mayo elbow performance (MEP) index and HSS scores measured at the follow-up evaluation showed excellent outcomes of surgical repair in all the patients irrespective of the repair technique used. The mean MEP index was 100 and HSS scores were 98.26 ± 2.60 (Table 2). There was no significant difference in mean HSS scores among different Types (I–III). The F-value obtained was 2.61, whereas the critical value corresponding to a 5% level of significance is 3.89. A similar comparison between the type of repair and the MEP index showed no significant association. The F-value obtained was 0.087 whereas the critical value was 3.89.
Table 2.
The final MEP index, HSS score, and duration of follow-up of each patient with the type of lesion and treatment method used.
| Type of TTA | Type of repair | Total follow-up (months) | MEP index | HSS score |
|---|---|---|---|---|
| III | TBW | 33 | 100 | 100 |
| III | TBW | 28 | 100 | 95 |
| III | TBW | 33 | 100 | 100 |
| III | TBW | 9 | 100 | 100 |
| II | Trans-osseous | 24 | 100 | 100 |
| I | Trans-osseous | 26 | 100 | 93 |
| I | Suture-Anchor | 32 | 100 | 100 |
| II | Trans-osseous | 30 | 100 | 100 |
| II | Trans-osseous | 24 | 100 | 95 |
| II | Trans-osseous | 11 | 100 | 100 |
| II | Trans-osseous | 20 | 100 | 100 |
| II | Trans-osseous | 16 | 100 | 100 |
| I | Trans-osseous | 18 | 100 | 95 |
| I | Suture anchor | 10 | 100 | 96 |
| II | Trans-osseous | 22 | 100 | 100 |
| Mean | 22.4 ± 8.2 | 100 | 98.26 ± 2.60 |
TBW: tension band wiring; MEP index: Mayo elbow performance index; HSS score: hospital for special surgery elbow score.
All patients had a complete range of motion at the final follow- up with full power of elbow extension. There were no re-ruptures reported in the study. One patient developed painful bursitis and infection at the olecranon due to prominent hardware and was managed by removal of the protruding K-wires. The follow-up X-ray for this patient showed an un-united avulsed fragment; the overall elbow function scores were comparable to the other cases. One patient managed with suture anchor fixation demonstrated pull out of the anchors in the follow-up X-ray at 6 weeks although the patient was clinically asymptomatic (Fig. 6).
Fig. 6.
Complications. (A) A patient treated using a suture anchor technique presented with a pull-out in the postoperative period. He had a full range of elbow movement (upper row). (B) (lower row) Radiograph showing K-wire removal following bursitis with follow-up showing the full range of movements of the elbow.
Discussion
In this study, we tried to correlate the clinicoradiological features of traumatic TTA with intraoperative findings for proposing a classification and treatment algorithm for it. We were able to suggest a simple and easy use classification. There are 4 types of possible injuries. The fourth one is an olecranon fracture. We also proposed a treatment algorithm for each type. From our experience of 15 cases, we found out that irrespective of the surgical techniques used for traumatic TTA, excellent functional outcomes can be obtained.
Traumatic TTA is a rare injury. The prevalence is about 3.8%.1,2 The diagnosis of this injury is often delayed. The paucity of clinical findings and more or less preserved elbow function are the reasons for the delay. A high index of suspicion is necessary for its diagnosis. There is a lack of consensus on surgical methods. Most of the available literature is based on the isolated reports and case series.
In a cadaveric study, it has been found that the triceps tendon is attached to the olecranon through a deep and superficial and deep part. There is a plain of cleavage between these two parts which continued to discrete insertion sites at the footprint on the olecranon. The superficial part originates from the long and lateral heads of the triceps and the deep part from the medial head. The superficial part is attached to the olecranon in a "W" shaped pattern with medial "V" more distal to the lateral one. The mean distance of triceps tendon attachment from the olecranon tip is about 1.1 cm.10 The type I Mayo or type A Schatzker class of olecranon fracture is a triceps tendon avulsion injury.11 We have included such injuries into type IV injuries in our classification where less than 25% of the articular surface of the olecranon is involved or the fracture line is within 1 cm from the tip of the olecranon.
We classify the TTA clinico-radiologically as Type I: palpable soft-tissues defect without bony mass and no bony fragment evident on the X-ray (an ultrasound scan or MRI scan is required for confirmation); Type II: Palpable soft-tissue defect with or without a palpable bony mass with a wafer-thin/comminuted bony fragment on the X-ray; Type III: Palpable soft-tissue defect with a bony mass and a large bony fragment on the X-ray which does not extend to the articular surface; and Type IV: An avulsion injury of the olecranon with less than 25% of the articular surface (Fig. 2). Cadaveric studies had shown that the triceps tendon is attached to the olecranon through a deep and superficial part. The mean distance of attachment of the triceps tendon from the tip of the olecranon is about 1.1 cm. The triceps injury with larger bony fragments extending into the articular surface cannot be differentiated from an olecranon fracture and hence have not been included in this study.
The injury is common in males. The third to fifth decade is the commonest age group.12,13 We found that the average age of our patient (31.5 years) was lower compared to the results (47.5 years) of a recent systematic review.5 This difference is probably because we included only traumatic cases. There are reports of intraarticular arthroscopic examination in TTA injuries where there is an extension of fractures into the joint.2 This variety is the one that we included in the Type IV classification. We have no Type IV injuries in the present series. Lack of proper clinical signs is an important factor in delayed diagnosis especially in partial injuries with preservation of active extension of the elbow. A palpable defect in the triceps tendon was found in 80% of patients in a previous study.5,6 We have not included any patients with partial rupture. We observed a greater degree of loss of function of the elbow in complete rupture with a palpable bony mass. So we think the differentiation of cases with and without palpable bony mass is important. The majority of cases belonged to the first category. Partial ruptures are often missed on X-ray and thus ultrasonography or MRI is required to make a diagnosis.14,15 However, in the present study, all cases were picked up by X-ray except for 4 which were picked up by ultrasonography. Ultrasonography is as effective as MRI in diagnosing partial and complete tears. There was a delay of about a week in the diagnosis of 6 patients in this study. Yeh et al.16 reported a similar case of delayed diagnosis of triceps tendon rupture.
Reports demonstrate that a triceps injury may get overlooked in up to 45% of patients. This emphasizes the need for a high index of suspicion and re-evaluation at the earliest. Neglected or under-diagnosed injury can develop poor functional outcomes. Hence a classification system becomes useful in making the clinical approach more systematic.
Partial ruptures of the triceps tendon recover well with rest and physiotherapy. Some patients may have a residual weakness that is clinically insignificant.8,17 Surgical repair of acute tears has been reported to be associated with a better and earlier functional recovery.8 Anatomical repair of acute injuries are associated with good outcome.18 In our series, the decision for a surgical repair was made only if the patient was unable to perform an active elbow extension.
Surgical repair of the triceps tendon can be achieved by various means such as tension band wiring of the osseous fragment, tendon whipstitch sutures passed through a bone tunnel in the olecranon, suture anchors, etc.8,10,13,17 There is no consensus on the best technique owing to the rarity of this injury and the heterogeneity in the repair techniques in the literature. Although there have been numerous small case series on the outcome of surgical repair of TTA, very few have studied function based on standardized outcome measures.7 There is a lack of literature evidence regarding the superiority of one technique over others or regarding the rehabilitation of these injuries.19 The rehabilitation protocol includes early active elbow flexion and passive extension using a dynamic elbow splint.20 In a review of 184 cases of acute TTA treated either by transosseous fixation or suture anchoring, there was a higher rate of re-rupture, reoperation rate, and longer released from medical care in patients treated with a transosseous technique.21 Yet in another report, primary repair of acute and chronic TTA yielded satisfactory results in the majority of patients with low re-rupture rate.22 Age, surgical technique, the extent of the tear, and the mechanism of injury were not associated with adverse patient outcomes.23 In the present study, irrespective of the techniques employed, excellent functional results were found in all the 12 patients at follow-up by the MEP index and the HSS elbow score following open surgical repair. A study by Bava et al.7 on the outcome of suture anchor repair of the triceps tendon showed excellent outcomes.
Many complications like infection, ulnar nerve neuropathy, arthrofibrosis, flexion contracture, hardware irritation, and failure of repair can occur following surgical repair of this injury.24 We had a patient with a suture anchor technique who later developed a pull out of the suture anchor although clinically silent. Similar reports of suture anchor pull out and re-ruptures were reported in a series by Neumann et al.3 Van Riet et al.6 in their series of 23 cases of repair using bone tunnels demonstrated good functional outcomes. Similar results were obtained in the 7 patients in the present study treated by the same technique. Few reports are demonstrating good outcomes with the Krakow 4 strand method.16 In our study, fairly good objective outcomes were obtained in the patients treated with the conventional Krakow 2 strand method. Although few reports demonstrate better biomechanics with bone tunnel technique when compared with transosseous technique, there are a few reports which showed no significant difference in the biomechanics of various techniques. We suggest a possible algorithm of adopting a transosseous suture/suture anchor for Type I, transosseous suture for Type II, and tension band wiring or steel wire sutures for Type II. However, large prospective studies are needed to further validate this classification and its clinical utility.
This study is not without limitations. This is a single-center study involving a small cohort with a short-term follow-up. This was a retrospective series and the comparison of the outcomes of different surgical techniques could not be carried out as all patients had fairly good outcomes irrespective of the technique. Due to the rarity of injury, we are not able to assess how good is our classification in terms of communication, and observer variability, and research purpose. The role of conservative management also could not be evaluated as only patients who underwent surgical repair were included in the study. The elderly patients who are not good candidates for surgery or with low activity demands can be treated by conservative methods.
In conclusion, TTAs are rare and require a high index of clinical suspicion for early diagnosis. The clinicoradiological classification and treatment algorithm is simple and useful for the management of traumatic complete TTAs. Surgical treatment of this injury results in excellent functions of the elbow irrespective of the surgical techniques. Since it is a single-center study involving a very small number of cases, we think a multicenter study with a larger number of patients is required for external validation of our classification and treatment recommendations.
Funding
Nil.
Ethical statement
This study has been approved by the institutional research committee (GMCKKD/RP2017/IEC/106).
Declaration of competing interest
The authors declare no competing interest for this manuscript.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Koplas M.C., Schneider E., Sundaram M. Prevalence of triceps tendon tears on MRI of the elbow and clinical correlation. Skeletal Radiol. 2011;40:587–594. doi: 10.1007/s00256-010-1043-9. [DOI] [PubMed] [Google Scholar]
- 2.Athwal G.S., McGill R.J., Rispoli D.M. Isolated avulsion of the medial head of the triceps tendon: an anatomic study and arthroscopic repair in 2 cases. Arthroscopy. 2009;25:983–988. doi: 10.1016/j.arthro.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 3.Neumann H., Schulz A.P., Breer S. Traumatic rupture of the distal triceps tendon (a series of 7 cases) Open Orthop J. 2015;9:536–541. doi: 10.2174/1874325001509010536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stannard J.P., Bucknell A.L. Rupture of the triceps tendon associated with steroid injections. Am J Sports Med. 1993;21:482–485. doi: 10.1177/036354659302100327. [DOI] [PubMed] [Google Scholar]
- 5.Shuttlewood K., Beazley J., Smith C.D. Distal triceps injuries (including snapping triceps): a systematic review of the literature. World J Orthoped. 2017;8:507–513. doi: 10.5312/wjo.v8.i6.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Riet R.P., Morrey B.F., Ho E. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am. 2003;85:1961–1967. doi: 10.2106/00004623-200310000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Bava E.D., Barber F.A., Lund E.R. Clinical outcome after suture anchor repair for complete traumatic rupture of the distal triceps tendon. Arthroscopy. 2012;28:1058–1063. doi: 10.1016/j.arthro.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 8.Marinello P.G., Peers S., Sraj S. A treatment algorithm for the management of distal triceps ruptures. Tech Hand Up Extrem Surg. 2015;19:73–80. doi: 10.1097/BTH.0000000000000082. [DOI] [PubMed] [Google Scholar]
- 9.Safran M.R., Graham S.M. Distal biceps tendon ruptures incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;40:275–283. [PubMed] [Google Scholar]
- 10.Barco R., Sánchez P., Morrey M.E. The distal triceps tendon insertional anatomy-implications for surgery. JSES Open Access. 2017;1:98–103. doi: 10.1016/j.jses.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benetton C.A., Cesa G., El-Kouba Junior G. Agreement of olecranon fractures before and after the exposure to four classification systems. J Shoulder Elbow Surg. 2015;24:358–363. doi: 10.1016/j.jse.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 12.Finstein J.L., Cohen S.B., Dodson C.C. Triceps tendon ruptures requiring surgical repair in national football league players. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115601021. 2325967115601021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tagliafico A., Gandolfo N., Michaud J. Ultrasound demonstration of distal triceps tendon tears. Eur J Radiol. 2012;81:1207–1210. doi: 10.1016/j.ejrad.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Meena U.K., Sharma A.K., Behera P. Triceps tendon avulsion in an army recruit: a case report. J Trauma Treat. 2015;4:255. doi: 10.4172/21671222.1000255. [DOI] [Google Scholar]
- 15.Tiger E., Mayer D.P., Glazer R. Complete avulsion of the triceps tendon: MRI diagnosis. Comput Med Imag Graph. 1993;17:51–54. doi: 10.1016/0895-6111(93)90074-w. [DOI] [PubMed] [Google Scholar]
- 16.Yeh P.C., Stephens K.T., Solovyova O. The distal triceps tendon footprint and a biomechanical analysis of 3 repair techniques. Am J Sports Med. 2010;38:1025–1033. doi: 10.1177/0363546509358319. [DOI] [PubMed] [Google Scholar]
- 17.Morrey B.F., An K.N., Chao E.Y.S. In: The Elbow and its Disorders. second ed. Morrey B.F., editor. WB Saunders Co; Philadelphia, PA: 1993. Functional evaluation of the elbow; p. 95. [Google Scholar]
- 18.Vidal A.F., Drakos M.C., Allen A.A. Biceps tendon and triceps tendon injuries. Clin Sports Med. 2004;23:707–722. doi: 10.1016/j.csm.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 19.Blackmore S.M., Jander R.M., Culp R.W. Management of distal biceps and triceps ruptures. J Hand Ther. 2006;19:154–168. doi: 10.1197/j.jht.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 20.Greer M.A., Miklos-Essenberg M.E. Early mobilization using dynamic splinting with acute triceps tendon avulsion. J Hand Ther. 2005;18:365–371. doi: 10.1197/j.jht.2005.04.004. quiz 371. [DOI] [PubMed] [Google Scholar]
- 21.Mirzayan R., Acevedo D.C., Sodl J.F. Operative management of acute triceps tendon ruptures: review of 184 cases. Am J Sports Med. 2018;46:1451–1458. doi: 10.1177/0363546518757426. [DOI] [PubMed] [Google Scholar]
- 22.Giannicola G., Bullitta G., Rotini R. Results of primary repair of distal triceps tendon ruptures in a general population: a multicentre study. Bone Joint Lett J. 2018;100-B:610–616. doi: 10.1302/0301-620X.100B5.BJJ-2017-1057.R2. [DOI] [PubMed] [Google Scholar]
- 23.Waterman B.R., Dean R.S., Veera S. Surgical repair of distal triceps tendon injuries: short-term to midterm clinical outcomes and risk factors for perioperative complications. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119839998. 2325967119839998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steffes M., Tayne S., Osmani F. Triceps repair and restoration of triceps footprint with anchorless suture fixation. Tech Hand Up Extrem Surg. 2018;22:89–93. doi: 10.1097/BTH.0000000000000196. [DOI] [PubMed] [Google Scholar]