Abstract
Purpose
The use of tourniquet in orthopedic surgery facilitates operation by establishing a bloodless surgical field. However, many complications following the use of tourniquets have been reported. Tourniquet pain is the most common complication. This study aimed to find the actual incidence of pain associated with tourniquet use in orthopedic surgery and the various factors.
Methods
It is a prospective observational study conducted on 132 consecutive cases. Patients aged 18-70 years with musculoskeletal problems of the forearm and leg requiring surgery were included in the study. Patients with open injuries or contraindications such as diabetes mellitus, compromised circulatory states, neurological deficit, compartment syndrome and unable to give informed consent were excluded. The parameters assessed included duration of tourniquet use, tourniquet pressure, type of anesthesia, any interval release of the tourniquet and reapplication after a reperfusion period, whether upper or lower limb surgery, severity of tourniquet pain, timing of tourniquet release and complications. Chi-square and non-parametric Mann-Whitney U test were used for data analysis.
Results
In upper limb surgeries, if duration of surgery was less than 60 min, 14 (51.8%) cases experienced tourniquet pain and 13 (48.1%) had no pain, and if duration of surgery was more than 60 min, 24 (60.0%) had pain and 16 (40.0%) experienced no pain. In lower limb surgeries if duration of surgery was less than 60 min, 2 (7.7%) experienced pain and 24 (92.3%) had no pain, and if duration of surgery was more than 60 min, 14 (35.8%) experienced pain and 25 (64.8%) had no pain. Degree of tourniquet pain increases with the duration of surgery. Statistically, there was significant association between tourniquet inflation time and tourniquet pain in both upper and lower limbs (p = 0.034 and 0.024, respectively)
Conclusion
Incidence of tourniquet pain was in direct proportion to the duration of tourniquet use and was higher in cases with regional anesthesia. Other risk factors assessed including tourniquet pressure, upper or lower limb surgery, tourniquet release time and interval had no significant contribution to the incidence or severity of tourniquet pain.
Keywords: Tourniquet pain, Pneumatic tourniquet, Bloodless field, Orthopedic surgery, Complications, Pain intensity
Introduction
The word tourniquet coined by Jean Louis Petit, is derived from the French word “tourner” which means “to turn”. The use of tourniquet in limb surgery facilitates operation by reliably establishing a bloodless surgical field with a high level of safety.1
The U.S. Food and Drug Administration has classified pneumatic tourniquet as class-I medical devices and the complications following its use has been reduced by improvements in technology along with appropriate precautions. However, a variety of cases suffered vascular or neurological damage following the use of tourniquets have been reported.1,2,3 Complications arising from tourniquet use can be systemic, which include cardiovascular effects, metabolic effects, thermal effects, drug kinetics and reperfusion syndrome or local which include tourniquet pain, cutaneous effects, direct vascular injury, neurological complications, tissue ischemia, edema and micro-vascular congestion. Tourniquet pain is described as a poorly localized, dull, tight, aching sensation at the site of tourniquet application. Tourniquet pain is a cause of concern for both anesthesiologists and orthopedic surgeons. The clinical syndrome of tourniquet pain consists of several components and is not just due to the pain and pressure under the tourniquet.2,3
The purpose of this study was to find the actual incidence of pain associated with tourniquet use in limb surgeries and the various factors contributing to them.
Methods
Study design and settings
It is a prospective observational study undertaken following an approval from Institutional Ethics Committee, with a convenient sampling of 132 consecutive cases operated in the department of orthopedic surgery with pneumatic tourniquet for the need of a bloodless surgical field from November 2017 to October 2019, a period over 2 years. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Inclusion and exclusion
Patients aged 18-70 years with musculoskeletal problems of the upper or lower extremities requiring surgery were included in the study. All these patients were explained pre-operatively regarding the use of tourniquet and its associated possible complications. An informed consent was taken after that.
Patients with open injuries or contraindications such as diabetes mellitus, compromised circulatory states (such as peripheral vascular disease, sickle cell disease, etc.), neurological deficit, compartment syndrome or unable to give an informed consent were excluded.
Study population
A total of 132 cases operated with pneumatic tourniquet for the need of a bloodless surgical field over a period of 2 years were included in this study. Majority of the patients fell in the age group of 31-40 years (n = 39, 29.5%) followed by the age group of 41-50 years (n = 36, 27.3%). Out of 132 patients, 50 (37.9%) were women and 82 (62.1%) were men. There were 67 cases involved upper extremity and 65 involved lower extremity. Both groups of patients (upper and lower extremity) had similar gender proportions and age distribution.
Methodology
All patients meeting the inclusion criteria underwent thorough pre-operative evaluation. General condition of the patient and associated medical conditions were assessed and fitness for appropriate anesthesia was taken. Pre-operative blood pressure in supine position was noted.
Pneumatic tourniquet system was used for all the patients in this study. Cylindrical non-tapered standard cuff for upper limb and lower limb were used. Adequate padding was applied over the extremity. Appropriate tourniquet cuff was applied with adequate padding and the limb was exsanguinated by elevating to 90° for 2 min. Tourniquet pressure was set by adding 75–125 mmHg above systolic pressure for upper limb and 150–200 mmHg above systolic pressure for lower limb. However, in normotensive patients an arbitrary of 250 mmHg for upper limb and 350 mmHg for lower limb were set.
The parameters assessed included duration of tourniquet use, tourniquet pressure, type of anesthesia, any interval release of tourniquet and reapplication after a reperfusion period, whether upper or lower limb surgery, severity of tourniquet pain, timing of tourniquet release and other complications including blood loss.
Tourniquet pain was assessed using 11-point numerical rating scale, the visual analogue scale and 4-point categorical verbal rating scale. Pain was assessed at 6 h, 24 h and 5 days following the surgery. Pain ratings were given by the patients and entered by the same observer.
Statistical analysis
Data analysis was performed using proportions, Chi-square test and non-parametric Mann-Whitney U test. A statistical package SPSS Version 17.0 was used for data analysis. A p < 0.05 was considered as statistically significant.
Results
Type of anesthesia and tourniquet pain
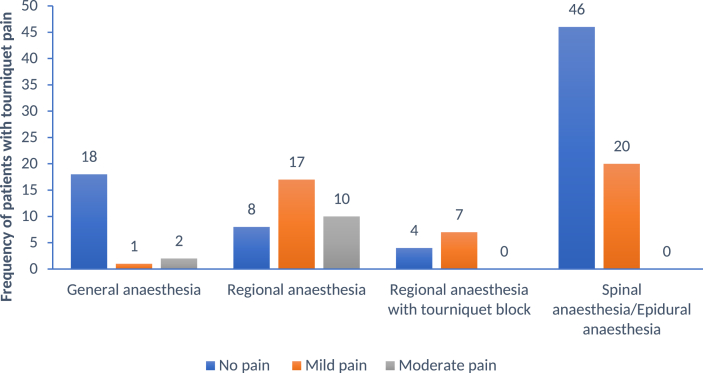
The type of anesthesia administered to the patient was analyzed. In the upper extremity, general anesthesia was administered for 21 patients, brachial block for a total of 37 (11 were also given tourniquet block) and local anesthesia for 9 (tourniquet block for 4). All the 65 patients of lower extremity in this study were given spinal anesthesia or a combination of epidural and spinal anesthesia. The incidence of pain was higher in patients with regional anesthesia. Detailed data are shown in Fig. 1.
Fig. 1.
Frequency of patients with tourniquet pain based on type of anaesthesia.
Duration of inflation and limb surgeries relationship for tourniquet pain
Tourniquet inflation ranged from 17 min to 140 min for the upper extremity with the mean duration of 70.14 min, standard deviation of 36.64 and a median of 70 min. For the lower extremity, the range was 25–140 min, standard deviation of 27.45 min and a median of 70 min.
Tourniquet pain was assessed separately for upper extremity and lower extremity surgeries. Each group was divided further into two sub-groups based on the duration of surgery (more than 60 min and less than 60 min).
In upper extremity group, patients whose duration of surgery was less than 60 min (n = 27), 48.1% (n = 13) experienced mild tourniquet pain, 3.7% (n = 1) experienced moderate tourniquet pain and 48.1% (n = 13) experienced no pain at all. In patients whose duration of surgery was more than 60 min (n = 40), 35.0% (n = 14) experienced mild tourniquet pain, 25.0% (n = 10) experienced moderate tourniquet pain and 40.0% (n = 16) experienced no pain at all (Table 1).
Table 1.
Association between duration of surgery and degree of tourniquet pain in 67 patients with upper limb surgeries, n (%).
| Duration of surgery | Degree of pain |
||
|---|---|---|---|
| Mild | Moderate | No pain | |
| <60 min (n = 27) | 13 (48.1) | 1 (3.7) | 13 (48.1) |
| >60 min (n = 40) | 14 (35.0) | 10 (25.0) | 16 (40.0) |
| Total | 27 (40.3) | 11 (16.4) | 29 (43.3) |
Fisher's exact test p = 0.024 that is statistically significant.
In lower extremity group, patients whose duration of surgery was less than 60 min (n = 26), 7.7% experienced mild tourniquet pain, none of them experienced moderate tourniquet pain and 92.3% experienced no pain at all. In patients whose duration of surgery was more than 60 min (n = 39), 33.3% (n = 13) experienced mild tourniquet pain, 2.6% (n = 1) experienced moderate tourniquet pain and 64.1% (n = 25) experienced no pain at all (Table 2). There were no neurological or vascular complications noted in this study.
Table 2.
Association between duration of surgery and degree of tourniquet pain in 67 patients with lower limb surgeries, n (%).
| Duration of surgery | Degree of pain |
||
|---|---|---|---|
| Mild | Moderate | No pain | |
| <60 min (n = 26) | 2 (7.7) | 0 (0) | 24 (92.3) |
| >60 min (n = 26) | 2 (7.7) | 0 (0) | 24 (92.3) |
| Total | 13 (33.3) | 1 (2.6) | 25 (64.1) |
Fisher's exact test p = 0.034 that is statistically significant.
Blood loss following tourniquet deflation was calculated and average loss was around 60 mL. There was no statistical significance (p = 0.026) in postoperative blood loss and timing of tourniquet deflation.
The mean pressure in the upper extremity was 230.67 mmHg and in the lower extremity the mean pressure was 331.38 mmHg. Mean tourniquet inflation duration 70.14 min for the upper extremity and 70 min for the lower extremity.
Discussion
Tourniquet has become an essential part of orthopedic surgeries involving the extremities for the sake of a bloodless surgical field. Tourniquet pain is possibly associated with complications following tourniquet use. Overall, complications following the use of tourniquets are less frequent if applied under supervision of experienced personnel with proper inflation pressures and duration of tourniquet use. Providing adequate analgesia by blocks, regional techniques or local anesthetic drugs, opioids or analgesics help in reducing the complications associated with tourniquet use.3,4
Tourniquet cuff inflation has been a matter of debate over the years. In our study the mean pressure in the upper extremity was 230.67 mmHg with the range 200-250 mmHg and in the lower extremity the mean pressure was 331.38 mmHg with the range 260-360 mmHg. The range of pressures was similar to those in previous studies.
Tourniquet inflation duration ranged 7-140 min for the upper extremity with the mean being 70.14 min. For the lower extremity, the range was 25-140 min.
Tourniquet pain is described as a poorly localized, dull, tight, aching sensation at the site of tourniquet application. Incidence varies from 53% to 67% in various studies.
Pain associated with tourniquet use was firstly studied in 1952 and a number of mechanisms have been explained for its cause.5, 6, 7 The exact etiology is unclear, but it is thought to be due to a cutaneous neural mechanism. The pain is thought to be mediated by the unmyelinated, slow conducting C fibers that are usually inhibited by the A-delta fibers. The A-delta fibers are blocked by mechanical compression after about 30 min, while the C fibers continue to function. Tourniquet compression leads to release of prostaglandins by the injured cells. These prostaglandins increase pain perception by sensitizing and exciting pain receptors. Also, limb ischemia causes central sensitization via N-methyl D-aspartate receptor activation due to repeated nociceptive afferent input from the affected limb.
Præstegaard et al.8 did a systematic review and meta analysis regarding the tourniquet use in lower limb surgery and stated that there was no statistically significant difference in the postoperative complications and pain in tourniquet group and no tourniquet group in lower limb fracture surgery.
In our study there was significant association between tourniquet inflation time and tourniquet pain in both upper and lower limbs (p= 0.034 and 0.024, respectively). Also, recovery occurred within a few minutes after deflation in most of the patients.8,9
There are other studies in the literature showing increased incidence of pain and swelling following the use of tourniquet in lower limb surgeries with increased postoperative opioid consumption.9,10 Also the incidence and severity of pain was seen with prolonged and increased pressure usage.11,12
In our study, for upper limb surgeries, if duration of surgery was less than 60 min, 51.8% experienced tourniquet pain whereas if duration of surgery was more than 60 min, 60% experienced tourniquet pain. In contrast to those with lower limb surgeries if duration of surgery was less than 60 min, 7.7% experienced tourniquet pain and if duration of surgery was more than 60 min, 35.8% experienced tourniquet pain. It seems to be contrasting results of tourniquet release on postoperative blood loss and other complications. In our study, there was no statistical significance (p = 0.026) in postoperative blood loss and timing of tourniquet deflation. Limitations of our study includes the smaller sample size and less number of parameters studied.
The most common complication following tourniquet use noted was tourniquet pain. Incidence and intensity of tourniquet pain was directly proportional to the duration of tourniquet use. Thus minimizing the duration of tourniquet use is recommended.
Another important finding observed in our study was frequency and intensity of tourniquet pain were higher in cases in which regional anesthesia was used. Hence tourniquet blocks and other pain-relieving modalities are recommended wherever regional anesthesia is used. There were no neurological or vascular complications seen.
Funding
Nil.
Ethical statement
This study complies with all the relevant national regulations, institutional policies and was performed in accordance with the tenets of the Helsinki Declaration and has been approved by our institutional ethics committee. Informed consent has been obtained from all individuals included in this study.
Declaration of competing interest
Authors state that no conflict of interest.
Acknowledgements
We are grateful for the support from Kasturba Medical College, Mangalore and Manipal Academy of Higher Education, Manipal.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Klenerman L. The tourniquet in surgery. J Bone Joint Surg Br. 1962;44-B:937–943. doi: 10.1302/0301-620X.44B4.937. [DOI] [PubMed] [Google Scholar]
- 2.Hagenouw R.R., Bridenbaugh P.O., Egmond J. Tourniquet pain: a volunteer study. Anesth Analg. 1986;65:1175–1180. [PubMed] [Google Scholar]
- 3.Sharma J.P., Salhotra R. Tourniquets in orthopedic surgery. Indian J Orthop. 2012;46:377–383. doi: 10.4103/0019-5413.98824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saied A., Ayatollahi M.A., Arabnejad F. Tourniquet in surgery of the limbs: a review of history, types and complications. Iran Red Crescent Med J. 2015;17 doi: 10.5812/ircmj.9588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu David, Graham David, Kim Gillies. Effects of tourniquet use on quadriceps function and pain in total knee arthroplasty. Knee Surg Relat Res. 2014;26:207–213. doi: 10.5792/ksrr.2014.26.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Souza Leão M.G., Neta G.P., Coutinho L.I. Comparative analysis of pain in patients who underwent total knee replacement regarding the tourniquet pressure. Rev Bras Orthop. 2016;51:672–679. doi: 10.1016/j.rboe.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omeroğlu H., Uçaner A., Tabak A.Y. The effect of using a tourniquet on the intensity of postoperative pain in forearm fractures: a randomized study in 32 surgically treated patients. Int Orthop. 1998;22:369–373. doi: 10.1007/s002640050280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Præstegaard M., Beisvåg E., Erichsen J.L. Tourniquet use in lower limb fracture surgery: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2019;29:175–181. doi: 10.1007/s00590-018-2282-z. [DOI] [PubMed] [Google Scholar]
- 9.Kumar N., Yadav C., Singh S. Evaluation of pain in bilateral total knee replacement and without tourniquet; a prospective randomized control trial. J Clin Orthop Trauma. 2015;6:85–88. doi: 10.1016/j.jcot.2015.01.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kruse H., Christensen K.P., Møller A.M. Tourniquet use during ankle surgery leads to increased postoperative opioid use. J Clin Anesth. 2015;27:380–384. doi: 10.1016/j.jclinane.2015.03.034. [DOI] [PubMed] [Google Scholar]
- 11.Ömeroğlu H., Günel U., Biçimoğlu A. The relationship between the use of tourniquet and the intensity of postoperative pain in surgically treated malleolar fractures. Foot Ankle Int. 1997;18(12):798–802. doi: 10.1177/107110079701801208. [DOI] [PubMed] [Google Scholar]
- 12.Konrad G., Markmiller M., Lenich A. Tourniquets may increase postoperative swelling and pain after internal fixation of ankle fractures. Clin Orthop Relat Res. 2005;433:189–194. doi: 10.1097/01.blo.0000151849.37260.0a. [DOI] [PubMed] [Google Scholar]