Abstract
Purpose
In the surgical treatment of paediatric forearm fractures, plate-screw and titanium elastic nails are used. During the transformation of ligamento-osseous structures from adolescence form into adult form, more stable fixation is required. The aim of this study was to evaluate the results of locked intramedullary nail fixation in adolescent forearm fractures.
Methods
A retrospective examination was made on 36 adolescent patients who underwent surgery with locked intramedullary nail fixation due to a forearm fracture. The included patients were in the adolescent age group (12–17 years), did not meet conservative follow-up criteria and had unstable fractures (>10° angulation and <50% cortex continuity after plaster casting). Patients were excluded from the study if they were aged >18 years or <12 years, had Gustilo-Anderson type 2/3 open fractures, multi-trauma, history of physeal injuries or could not be contacted during follow-up. Patients’ age, gender, body mass index, affected side, and the pronation and supination values during follow-up were noted. Functional evaluation of the patients was performed with disabilities of the arm, shoulder and hand score and the surgical outcomes were evaluated according to the Price criteria. The time to union, infection during follow-up, re-fracture and vascular nerve damage were also examined. Data were analyzed using SPSS 22 Windows package program software.
Results
The patients comprised 30 males and 6 females (ratio, 5:1) with a mean age of (14.7 ± 2.1) years (range, 12–18 years). According to the Price criteria, the results of 33 patients were excellent, 3 were good and there were no moderate or poor cases. The mean disabilities of the arm, shoulder and hand score was 11.2 ± 6.1 (range, 4–28). The mean time to union was (8.7 ± 2.2) weeks (range, 6–14 weeks), while patients aged >15 years had prolonged time to union ([11.1 ± 1.8] weeks). There were no non-unions, re-fractures or infections. No complications were observed during implant removal. None of the patients had sensorial radial nerve injury or tendon damage.
Conclusion
The locked intramedullary nailing technique, which is minimally invasive and provides biological fixation, was found to be successful and safe in the treatment of adolescent forearm fractures.
Keywords: Adolescent forearm fracture, Intramedullary locked nail, Functional results, Complications
Introduction
Forearm fractures are often seen in children and constitute 6% of all children fractures.1 Diaphyseal forearm fractures can usually be treated with closed reduction and plaster casting. A total of 85% of cases aged <10 years are treated with closed reduction and plaster casting; however, fracture reduction becomes more difficult as the patient's age increases.2,3 Indications for surgical treatment of paediatric forearm fractures include not being able to obtain acceptable alignment with closed manipulation, accompanying neurovascular injury, polytrauma cases, open fractures and unstable fractures (e.g. proximal fractures).4,5 Advanced age and some fracture configurations (such as proximal 1/3 fractures, Monteggia fractures) are risk factors of unstable fractures.6
As the patients get older, ligamento-osseous structures transform into adult form which makes the fracture manipulation more difficult to achieve and reduce the fracture remodelling capability. Therefore, the success of conservative treatment is reduced in older children and surgical treatment options come to the fore. Inappropriate treatment of forearm fractures could lead to malunions and restrict movement at forearm.7 Although there is debate in literature about the age range, it has been reported that patients aged >14 years can be treated as adults. Although there is no gold standard treatment method for patients aged 10–14 years, plate-screw osteosynthesis with titanium elastic screws can be used.8 While plate application is often used in adult, the more minimally invasive and biological fixation method of locking intramedullary nailing is used successfully in forearm fractures owing to recently developed nailing techniques. Özkaya et al.9 compared plate-screw and locking plate applications and reported that similar functional results were obtained. To the best of our knowledge, there have been no reports in literature of the results of locked intramedullary nailing in adolescent patients.
Locking nailing techniques for forearm fractures is developing and these developments yielded successful results and low complication rates in literature. The aim of the current study was to evaluate the results of adolescent forearm fractures surgically treated with locked intramedullary nailing providing stable fixation.
Methods
A retrospective examination was performed on 36 adolescent patients who underwent surgery with intramedullary nail fixation because of forearm fracture between January 2014 and December 2018. The included patients were in the adolescent age group (12–17 years), did not meet conservative follow-up criteria and had unstable fractures (>10° angulation and <50% cortex continuity after plaster casting). Patients were excluded from the study if they were aged >18 years or <12 years, had Gustilo-Anderson type 2 or 3 open fractures, multi-trauma, history of physeal injuries or could not be contacted during follow-up. Patients' age, gender, body mass index and affected side were obtained from hospital registry notes. Functional evaluation of the patients during follow-up was made according to the disabilities of the arm,shoulder and hand (DASH) score and the Price criteria.10,11 The pronation and supination degrees, malalignment, time to union, infection or re-fracture rate were noted. Malalignment was evaluated according to the radial curve index and location. The radial curve point and the radial curve index were calculated by determining the bicipital tubercle, the most medial point of the distal radioulnar joint, and the deepest points on the medial side of the radius shaft, on anterior-posterior radiographs at the final follow-up visit. A radial curve index value > 10 was accepted as pathological.12,13 Patients’ fractures were considered clinically united when there was no pain at the fracture line. And radiological union was considered when callus formation was observed in at least 3 cortices on anterior-posterior and lateral radiographs.14 No union till in the 4th month was defined as delayed union and the absence of callus tissue in the 6th month as non-union.
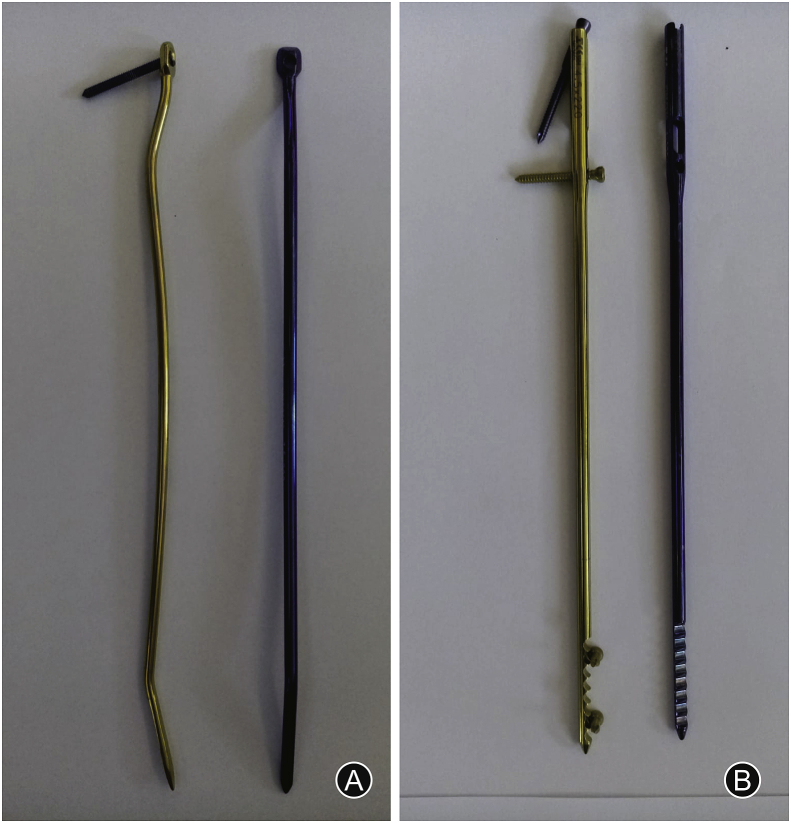
Design of the radius-ulna nails
All the radius and ulna nails used were made from titanium alloys (TST Rakor Tıbbi Aletler San. ve Tic. Ltd. Sti., Istanbul, Turkey). The radius nail is solid and round, with a parabolic shape which angulates 10° toward the anterior in the 3 cm proximal part. There is a distal static locking screw providing stability based on the three-point fixation principle. The distal static locking screw provides locking at a 17° proximal and volar angle (Fig. 1A). This angle prevents orientation of the locking screw toward the distal joint surface of the radius. The same radius intramedullary nails can be used for both right and left forearms. The nails are available in diameters of 3 mm, 3.5 mm and 4 mm and length 18 cm, 19 cm, 20 cm, 21 cm, 22 cm, 23 cm and 25 cm. They are used non-reamed.
Fig. 1.
(A) Distal static locking screw and three-point fixation principle on intramedullary radial nail; (B) Intramedullary ulna nail design: yellow screws proper for adolescent patients.
The proximal 4 cm part of the newly designed locked intramedullary ulna nail is tubular and the distal section is solid. There are different screw position options for both distal and proximal: yellow screws are proper for adolescent patients, blue screw damage proximal ulna physis and should not be used in adolescent patients (Fig. 1B). The proximal diameter of all nails is 6 mm, and the distal section is available in diameters of 3.5 mm, 4 mm, 4.5 mm, 5 mm and 6 mm. There are 22 different options for nail length. The same nail may be used for right- and left-side ulna fractures. The titanium elastic structure allows bending with torsional forces and the distal and proximal locking provides rigid axial and rotational fixation. If needed, compression can be applied. The intramedullary ulna nail has a proximal and distal locking system.
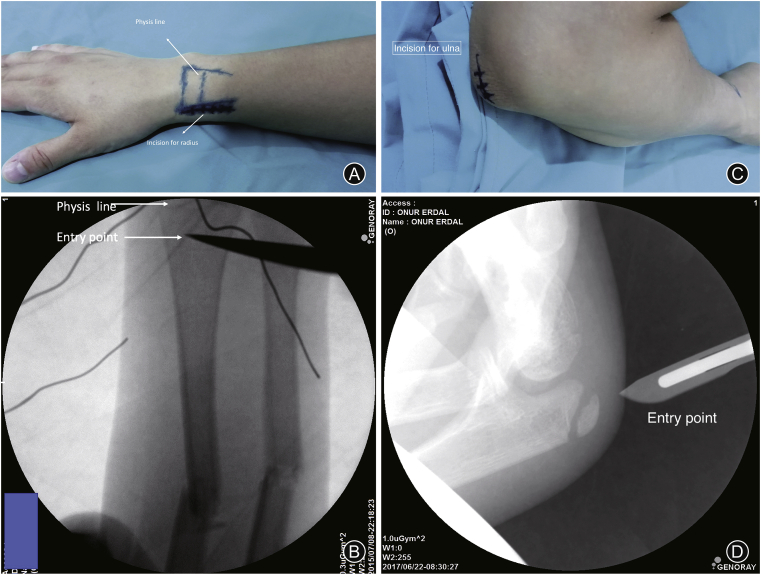
Surgical technique
The surgical procedure is performed in supine position and under tourniquet. Under fluoroscopy guidance, a 2 cm incision was made from the distal radius 1 cm proximal of the physis (Fig. 2A and B). Radial sensory branch and extensor tendons were protected. Entry point was determined 2 cm proximal to the radial styloid and 1 cm proximal to the physis, checked carefully with fluoroscopy. Initially, closed reduction was attempted and when 3 attempts were unsuccessful, the procedure was continued with open reduction, which was performed with a 2 cm mini-incision over the fracture line. The special design of the radius nail implant does not require a proximal fixation. Distal fixation of radius was made based on the 3-point principle and especially after obtaining radial curve. The entry of ulna was performed through the apophysis (Fig. 2C and D). If closed reduction failed 3 times, open reduction was performed with a 2 cm mini-incision over the fracture line. Following fracture reduction, intramedullary ulna nail with appropriate length and size was applied. The screws for the ulna were checked by fluoroscopy to confirm the preservation of physis. In late adolescent patients, fixation was performed with both distal and proximal screws. However, distal and proximal screw fixation are not necessary in early adolescent patients. Otherwise, all adolescent patients did not need compression for ulna. Forearm screws were used in all patients; 3–4 mm screws for the radius and 3.5–4.5 mm screws for the ulna. The nail thicknesses used were the same in 50% of the patients, as 3mm, 3.5mm and 4 mm diameter. No problems were experienced in any patient in respect of intramedullary diameter and length.
Fig. 2.
Surgery technique, incision and entry point for radius and ulna.
Follow-up
All the patients were discharged with a short-arm splint on postoperative day 1. Elbow joint movements and finger movements were started immediately after surgery. Patients were followed with 2-week intervals with anteroposterior and lateral forearm radiographs until achieved radiological union. At the postoperative 2-week visit, the splint and sutures were removed and wrist movements were started. The patients returned to social and school life in the 2nd week, and sports were resumed when the bone union criteria were met. At the 1-year follow-up, the nails were removed. Preoperative images of a 13-year-old male patient, at 3 months after union and after removal of the implants, are shown in Fig. 3.
Fig. 3.
(A) Images of a 13-year-old female patient preoperatively; (B & C) Postoperatively radiographs on day 1; (D & E) In cast and union of the case on 3-month; (F & G) After removal of the implants on 12-month.
Statistical analysis
Data obtained in the study were analyzed using SPSS 22 Windows Package Program software. Values were stated as 95% confidence interval (CI). Data were recorded as percentage, arithmetic mean and standard deviation (SD). Compliance of the variables included in the analysis with normal distribution was analyzed with the Kolmogorov–Smirnov test. Spearman's correlation analysis was used for correlation between parameters. Correlation between pronation, supination and grip strength of the treated and healthy forearms was evaluated with the Mann–Whitney U test. A value of p < 0.05 was considered statistically significant.
Results
The patients comprised 30 males and 6 females (ratio: 5:1) with a mean age of (14.7 ± 2.1) years (range, 12–17 years). The fracture was on the right side in 30 patients, on the left in 6 (R/L:5/1), and on the dominant side in 32 (88.9%) patients. Among the patients, 32 had primer fracture (non-acceptable alignment), 2 had refracture, 2 had reduction loss; and the first application time to hospital was longer than 14 days in 6 patients. Gustilo-Anderson type 1 open fracture was determined in 2 (5.6%) patients. The demographic data are shown in Table 1.
Table 1.
Demographic data of the patients.
| Variables | n (%) |
|---|---|
| Age (mean ± SD) | 14.7 ± 2.1 |
| Early adolescent (<14 years) | 20 (55.6) |
| Late adolescent (>14 years) | 16 (44.4) |
| Gender | |
| Male | 30 (83.3) |
| Female | 6 (16.7) |
| Side | |
| Right | 30 (83.3) |
| Left | 6 (16.7) |
| Follow-up (year) (mean ± SD) | 1.8 ± 0.6 |
| Gustilo-Anderson type 1 open fracture | 2 (5.6) |
| Dominant side | |
| Dominant | 32 (88.9) |
| Non-dominant | 4 (11.1) |
| Etiology | |
| Primer fracture (non-acceptable alignment) | 26 (72.2) |
| Re-fracture | 2 (5.6) |
| Reduction fail | 2 (5.6) |
| First application time to hospital was longer than 14 days | 6 (16.7) |
SD: standard deviation.
Fractures were located proximal in 16.6%, mid-shaft in 66.7% and distal in 16.6% of the patients. The fractures were transverse in 77.8% of patients and non-transverse in 22.2%. Open reduction with a mini incision was applied in 3 (8.3%) patients. The mean radial curve point was located at 71.2% ± 6.4% of radius length. The mean radial curve index was 6.8% ± 1.4%. According to the Price criteria, the results were excellent in 33 patients, and good in 3 patients. The mean supination range of motion was 82.35° (range, 75°-90°), and pronation range of motion was 85.18° (range: 82°-90°) (Table 2). The mean duration of surgery was (48 ± 13) min (range, 40–60 min), and mean fluoroscopy time was (40 ± 18) seconds (range, 30–70 seconds). The mean DASH score was 11.2 ± 3.8 (range, 4–28). No complications were observed during implant removal.
Table 2.
Comparation of pronation and supination values of patients in the healthy and treated forearms, degree.
| Variables | Treated forearm |
Healthy forearm |
p value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Min | Max | Mean | SD | Min | Max | Mean | SD | ||
| Pronation | 84 | 90 | 85.1 | 6.6 | 90 | 95 | 91.1 | 2.1 | 0.182 |
| Supination | 75 | 90 | 82.3 | 7.8 | 85 | 90 | 88.2 | 2.2 | 0.246 |
SD: standard deviation.
The overall mean time to union was (8.7 ± 2.2) weeks (range, 6–14 weeks), (11.1 ± 1.8) weeks for patients aged >15 years, and (11.3 ± 1.8) weeks for patients who had initially treated by a bonesetter. No non-union, refracture, physeal arrest, infection, complication during implant removal, sensory radial nerve damage or tendon rupture were observed (Table 3).
Table 3.
Analyses of radiological and clinic results.
| Variables | Mean | SD |
|---|---|---|
| Union time (weeks) | 8.7 (6–14) | 2.2 |
| DASH score | 11.2 (4–28) | 6.1 |
| Radial point | 6.8 | 1.4 |
| Radial index (%) | 71.2 | 6.4 |
| Fluoroscopy time (seconds) | 48 (30–60) | 13 |
| Surgery time (mins) | 40 (40–70) | 18 |
SD: standard deviation; DASH: disabilities of the arm, shoulder and hand.
Discussion
Adolescence is the time of transition from childhood to adulthood involving biological, psychological, and social changes of an individual. The World Health Organization defines the adolescence as the period from 10 to 19 years of age, with 10–14 years accepted as early adolescence and 15–19 years as late adolescence.15 Differences in fracture mechanism in the adolescent period make conservative treatments more difficult due to reduced capability for remodelling and difficulty in fracture manipulation. Therefore, the criteria for acceptable reduction of paediatric forearm fractures change inpatient aged over 10 years, and after plaster casting, angulation of >10° is surgically evaluated as <50% cortex continuity.
Titanium elastic nail and plate-screw osteosynthesis are among the surgical treatment options for these fractures.16,17 There are some disadvantages of the existing surgical options, especially for the late adolescent age group, such as the inadequacy of the intramedullary titanium elastic nail in terms of stability, and that plate screw applications are invasive and not biological. In this study, the results are presented of the treatment of adolescent forearm fractures with intramedullary locked nail, which is a stable and biological method leading to good results in adults.
The study included a total of 36 patients applied with locked intramedullary nail because of forearm fracture in adolescence. According to the Price criteria, the results were excellent in 33 patients and good in 3, no moderate or poor results were observed. The mean DASH score was determined to be high. No complications, such as infection, non-union, tendon, nerve or vascular damage, were seen in any patient. Thus, this method is presented in literature as a successful surgical treatment with high functional scores and low complication rates.
Surgery is necessary for paediatric forearm fractures that do not meet the reduction criteria and are unstable. Plate-screw osteosynthesis and intramedullary titanium nails are often used in surgical treatment. In addition to successful results from both treatments, studies compared the 2 methods have obtained similar functional results.16,17 In the studies that have presented successful results of titanium elastic nailing, the mean age of the patients was usually 10–11 years old and the upper limit was 14 years. Intramedullary fixation is often used, with the advantages of being a biological fixation method, requiring less tissue dissection and there are better cosmetic results.18,19
Plate-screw fixations come to the fore in paediatric forearm fractures in the age group where the stability of titanium elastic nailing would be insufficient. The current study mostly consisted of the advanced adolescent patients with a mean age of (14.72 ± 2.15) years and an upper limit of 18 years; approximately half the patients were aged over 14 years. The greatest disadvantage of the intramedullary elastic nail is the absence of rotational stability. However, stability is provided by the locking screws located in the proximal and distal parts of the intramedullary nail.
High functional scores have been obtained in adult forearm fractures treated with intramedullary locked nailing.9,20,21 Özkaya et al.9 compared plate-screw synthesis and intramedullary locked nailing in a group of 42 adult patients. Similar functional results were obtained from both surgical methods, but the time to union was noticeably shorter in the intramedullary nailing group.
Köse et al.20 obtained higher patient satisfaction in 18 adult fractures by using the same design of intramedullary locking nail as in the current study. Although there was no intraoperative damage to neurovascular structures, they had late stage extensor tendon damage (extensor pollicis longus) in 1 patient. There are 2 important advantages of the intramedullary nails used in the current study: (1) the surgical technique facilitates the restoration of radial bowing and establishment of fracture reduction with the 3-point principle, and (2) as there is no need for proximal locking, the possibility neurovascular injury, primarily on the posterior interosseous nerve, is reduced. With a 2 cm mini-incision made in the distal radius, the extensor tendons were protected and it was ensured that dorsal sensory branch of the radial nerve was protected, as well, thus possibility of tendon, vascular, or nerve damage was minimized. There was no proximity to neurovascular structures during nailing of ulna. Current surgical implant allows on ulna but there was no requirement for this in any of the adolescent patients in the study. While incompatibility can be expected between the intramedullary diameter and the nail diameter in the adolescent period, the surgical set used in this study was observed to be suitable for adolescent fractures.
Plate screw fixation requires soft tissue dissection and causes periosteal damage. The potential risks in this fixation method are intraoperative neurovascular injury, compartment syndrome, infection, non-union and refracture after plate removal. In previous studies, Sage et al.22 mentioned the risk of intraoperative is nerve damage and Moerman et al.23 stated that nerve palsy was seen in 7%–10% of patients, postoperatively. In a study by Jones et al.24 that compared plate-screw osteosynthesis with intramedullary locking nail, infection was observed at a high rate in the plate-screw fixation group. Of the patients in the current study treated with intramedullary locking nail, no intraoperative vascular, nerve or tendon damage was seen, and postoperatively there were no cases of non-union, refracture, or infection. The implants were removed from all the adolescent patients included in this study. No complications or deformities were observed during removal.
The most significant limitation of this study was the lack of a control group. A comparison of a similar age group applied with plate-screw synthesis in respect of time to union and complications could be of more guidance in treatment. Another limitation of the study was that it was retrospective. Nevertheless, the strong aspect of the study is the application of intramedullary locking nail to a large patient group of adolescents which is presented for the first time in literature.
The locked intramedullary locked nailing technique, which is minimally invasive and provides biological fixation, was found to be successful and safe in the treatment of adolescent forearm fractures. The use of intramedullary locked nail can be recommended in adolescent forearm fracture surgery, where titanium elastic nails could be insufficient.
Funding
Nil.
Ethical statement
The study protocol was approved by the Çankırı State Hospital Review Board and Çankırı Provincial Health Directorate (Date: 08.07.2019, Number: 21392878-799).
Declaration of competing interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Landin L.A. Epidemiology of children's fractures. J Pediatr Orthop B. 1997;6:79–83. doi: 10.1097/01202412-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Creasman C., Zaleske D.J., Ehrlich M.G. Analyzing forearm fractures in children. Clin Orthop Relat Res. 1984;188:40–53. [PubMed] [Google Scholar]
- 3.Zionts L.E., Zalavras C.G., Gerhardt M.B. Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J Pediar Orthop. 2005;25:507–512. doi: 10.1097/01.bpo.0000158005.53671.c4. [DOI] [PubMed] [Google Scholar]
- 4.Truntzer J., Vopat M.L., Kane P.M., Christino M.A., Katarincic J., Vopat B.G. Forearm diaphyseal fractures in the adolescent population: treatment and management. Eur J Orthop Surg Traumatol. 2015;25(2):201–209. doi: 10.1007/s00590-014-1489-x. [DOI] [PubMed] [Google Scholar]
- 5.Larsen E., Vittas D., Trop-Pedersen S. Remodeling of angulated in distal forearm fractures in Children. Clin Orthop Relat Res. 1988;237:190–195. [PubMed] [Google Scholar]
- 6.Younger A.S., Tredwell S.J., Mackenzie W.G. Factors affecting fracture position at cast removal after paediatric forearm fracture. J Pediatr Orthop. 1997;17:332–336. [PubMed] [Google Scholar]
- 7.Daruwalla J.S. A study of radioulnar movements following fractures of the forearm in children. Clin Orthop Relat Res. 1979;139:114–120. [PubMed] [Google Scholar]
- 8.Amstrong P.F., Joughin V.E., Clarke H.M. In: Skeletal Trauma. Grecn N.E., Swiontkowski M.F., editors. W.B. Saunders Co; Philadelphia, PA: 1994. Paediatric fractures of the forearm wrist, and hand; pp. 127–211. [Google Scholar]
- 9.Ozkaya U., Kilic A., Ozdogan U. Comparison between locked intramedullary nailing and plate osteosynthesis in the management of adult forearm fractures. Acta Orthop Traumatol Turcica. 2009;43:14–20. doi: 10.3944/AOTT.2009.014. [DOI] [PubMed] [Google Scholar]
- 10.Hudak P.L., Amadio P.C., Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 11.Price C.T., Scott D.S., Kurzner M.E. Malunited forearm fractures in children. J Pediatr Orthop. 1990;10:705–712. doi: 10.1097/01241398-199011000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Schemitsch E.H., Richards R.R. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am. 1992;74:1068–1078. [PubMed] [Google Scholar]
- 13.Firl M., Wunsch L. Measurement of bowing of the radius. J Bone Joint Surg Br. 2004;86:1047–1049. doi: 10.1302/0301-620x.86b7.14294. [DOI] [PubMed] [Google Scholar]
- 14.Shah A.S., Lesniak B.P., Wolter T.D. Stabilization of adolescent bothbone forearm fractures: a comparison of intramedullary nailing versus open reduction and internal fixation. J Orthop Trauma. 2010;24:440–447. doi: 10.1097/BOT.0b013e3181ca343b. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization . WHO, Department of Child and Adolescent Health and Development, Programme Brochure; Geneva: 1998. The Second Decade: Improving Adolescent Health and Development. [Google Scholar]
- 16.Atay T., Tomruk Ö., Çetin G.N. Süleyman Demirel Üniversitesi Tıp Fakültesi acil servisine başvuran çocuk kırıklarının epidemiyolojik değerlendirmesi. Kocatepe Tıp Dergisi. 2008;9:17–21. [Google Scholar]
- 17.Genç E., Çamurcu İ.Y., Eren E. Comparison of plating and titanium elastic nail fixation for surgical treatment of paediatric both-bone forearm fractures. Acta Med Alanya. 2018;2:64–68. doi: 10.30565/medalanya.364191. [DOI] [Google Scholar]
- 18.Shoemaker S.D., Comstock C.P., Mubarek S.J. Intramedullary Kıshner wire fixation of open or unstable forearm fractures in children. J Pediatr Orthop. 1999;19:329–337. [PubMed] [Google Scholar]
- 19.Yalcinkaya M., Dogan A., Ozkaya V. Clinical results of intramedullary nailing following closed or mini open reduction in paediatric unstable diaphyseal forearm fractures. Acta Orthop Traumatol Turcica. 2010;44:7–13. doi: 10.1097/BOT.0b013e3181ca343b. [DOI] [PubMed] [Google Scholar]
- 20.Köse A., Aydın A., Ezirmik N. Alternative treatment of forearm double fractures: new design intramedullary nail. Arch Orthop Trauma Surg. 2014;134:1387–1396. doi: 10.1007/s00402-014-2058-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bansal H. Intramedullary fixation of forearm fractures with new locked nail. Indian J Orthop. 2011;45:410–416. doi: 10.4103/0019-5413.83760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sage F.P. Medullary fixation of fractures of the forearm. J Bone Joint Surg Am. 1959;41:1489–1516. doi: 10.1007/s00402-014-2058-9. [DOI] [PubMed] [Google Scholar]
- 23.Moerman J., Leneart A., Deconinck D. Intramedullary fixation of forearm fractures in adults. Acta Orthop Belg. 1996;62:34–40. [PubMed] [Google Scholar]
- 24.Jones D.B., Kakar S. Adult diaphyseal forearm fractures: intramedullary nail versus plate fixation. J Hand Surg Am. 2011;36:1216–1219. doi: 10.1016/j.jhsa.2011.03.020. [DOI] [PubMed] [Google Scholar]